Abstract
Study Objectives
The evolution of sleep bruxism manifestations and their co-occurrence with separation anxiety in early childhood remain unclear. Our threefold aim was to: (1) describe developmental sleep bruxism trajectories in early childhood, (2) investigate co-occurrences between trajectories of sleep bruxism and separation anxiety, and (3) determine whether distinct trajectories of separation anxiety increase the risk of presenting sleep bruxism during the first year of elementary school.
Methods
This study is part of the Québec Longitudinal Study of Child Development. Sleep bruxism scores were assessed from age 1.5 to 7 years with the Self-Administered Questionnaire for Mother (n = 1946). Separation anxiety scores were measured from age 1.5 to 6 years with the Interviewer-Completed Computerized Questionnaire (n = 2045).
Results
We identified four sleep bruxism trajectories from age 1.5 to 6 years: High-Increasing sleep bruxism at age 1.5 (14.1%), High-Increasing sleep bruxism at age 4 (18.3%), Low-Persistent sleep bruxism (12.1%), and Never-Persistent sleep bruxism (55.5%); and four separation anxiety trajectories from age 1.5 to 6 years: Low-Persistent separation anxiety (60.2%), High-Increasing separation anxiety (6.9%), High-Decreasing separation anxiety (10.8%), and Low-Increasing separation anxiety (22.1%). Sleep bruxism and separation anxiety trajectories were weakly associated (X2 = 37.84, p < 0.001). Compared with preschoolers belonging to the Low-Persistent separation anxiety trajectory, preschoolers in the High-Increasing separation anxiety trajectory had almost double the risk of presenting sleep bruxism at age 7 (95% CI = 1.25–3.22, p = 0.04).
Conclusion
When separation anxiety issues are detected in early childhood, it would be useful to target sleep bruxism during the first year of elementary school.
Keywords: sleep bruxism, separation anxiety, preschoolers, longitudinal study
Statement of Significance.
Associations between sleep bruxism and child general anxiety have been reported in many studies based on maternal reports and objective assessments. Separation anxiety could also be a risk factor for sleep bruxism. We found that children belonging to a High-Increasing separation anxiety trajectory in the preschool years double their risk of presenting sleep bruxism manifestations at age 7. Once a child is diagnosed with separation anxiety, sleep bruxism assessment by a dentist is recommended.
Introduction
The American Academy of Sleep Medicine defines sleep bruxism as a stereotyped movement disorder occurring during sleep and characterized by tooth clenching and/or grinding as a result of prolonged and involuntary contractions and hyperactivity of the masticatory muscles, usually associated with sleep arousals [1]. Polysomnographic findings have shown that sleep bruxism is a rhythmic or tonic activity of the masseter and temporal muscles that may occur in any sleep stage, although it is more common in stage 1 and 2 non-rapid eye movement sleep and NREM sleep. Sleep bruxism is categorized as a sleep-related movement disorder in the International Classification of Sleep Disorders, Third Edition [2], and reported as the third leading parasomnia in terms of prevalence [3]. The estimated prevalence of sleep bruxism ranges from 15% to 49% in general population children. This wide variation could be explained by the fact that different age periods were investigated with different methodologies [3–9]. As children grow up, sleep bruxism increases [9]. The prevalence of sleep bruxism then decreases in adolescence [3] to 8% in adults [10]. Few prospective studies have investigated sleep bruxism in early childhood, an important period for understanding the complex etiology of this parasomnia. If untreated, sleep bruxism has numerous consequences (e.g. tooth damage, orofacial pain, headache complaint) [11] that could affect children’s quality of life, especially in terms of functional ability and social well-being [12].
In past decades, researchers have explained sleep bruxism etiology as the result of physical abnormalities (e.g. malocclusions, balancing interferences) [7, 13]. Hence, many studies have examined physiological changes to explain sleep bruxism. Maladaptive behaviors, including psychological factors (e.g. stress), have also been proposed in the multifactorial sleep bruxism etiology [14–17]. As suggested by Lavigne and collaborators [11], many dentists concur that sleep bruxism is associated with stress and anxiety [7, 8, 10, 18–20]. Recent physiological studies have investigated this association more objectively. One study found that sleep bruxism activity in children was related to higher perceived psychological stress and salivary cortisol [21], whereas another study [22] found no difference in salivary stress biomarkers between children with and without temporomandibular disorders. However, the latter study included a heterogeneous group of psychophysiological disorders, including sleep bruxism, nail biting, and nonnutritive sucking, which may explain the inconsistent results. Many studies have shown that patients with sleep bruxism had elevated levels of catecholamines in their urine compared to non-bruxers, supporting a relationship between emotional stress and sleep bruxism [23–25].
Separation anxiety is a developmentally appropriate emotional stress reaction when a child aged 12 to 18 months is separated from major attachment figures (typically parents) [26]. As the child grows up, an exaggerated and/or age-inappropriate manifestation of fear or anxiety when anticipating or experiencing separation from major attachment figures is called separation anxiety disorder (SAD) [3]. It was recently found that SAD is far from rare (4% prevalence in population samples [27–29] and 7.6% in pediatric clinical samples [30]), and is not without consequences. Childhood SAD has been identified as a possible gateway to both physical and psychiatric problems such as panic disorders in adolescence and early adulthood [31–33]. Accounting for up to 50% of referrals [32], and with clear implications for prospective physical health [34], SAD is recognized as the most frequently diagnosed anxiety disorder in early childhood. Two studies found that separation anxiety predicted later dyssomnias (e.g. child sleep–wake transition disorders) [9, 35] and other parasomnias (e.g. sleep terrors, somniloquy, enuresis, rhythmic movements, somnambulism) [9, 36]. Petit and colleagues [9] suggested that separation anxiety was associated with sleep bruxism in early childhood.
The underlying mechanisms of covariation between sleep bruxism and separation anxiety remain unexplored. However, studies have shown that children with SAD reported responses to CO2 stimulation similar to those in adults with panic disorder, such as abnormal respiratory measures during exposure to hyperpnea [37, 38]. Abnormal respiratory patterns were also found in sleep bruxers, suggested as another putative mechanism of sleep bruxism etiology [39]. Therefore, abnormal respiratory patterns could act as a bridging element between sleep bruxism and separation anxiety, which are generated by the same underlying neural substrate. In addition, emotional stress associated with separation anxiety could reduce sleep quality, resulting in tooth clenching/grinding/gnashing.
To date, sleep bruxism and separation anxiety have not been investigated concomitantly and longitudinally in general population children. Our research team [40] identified four developmental separation anxiety trajectories from infancy to school entry: Low-Persistent separation anxiety (60.2%), High-Increasing separation anxiety (6.9%), High-Decreasing separation anxiety (10.8%), and Low-Increasing separation anxiety (22.1%). However, after accounting for several factors related to general anxiety, separation anxiety has not yet been established as a significant trigger for sleep bruxism. The present study aimed to fill this gap by investigating co-occurrences between sleep bruxism and separation anxiety trajectories in early childhood. The specific objectives were to (1) describe developmental sleep bruxism trajectories in early childhood (age 1.5 to 6 years), (2) investigate co-occurrences of sleep bruxism and separation anxiety trajectories (age 1.5 to 6 years), and (3) examine whether distinct developmental separation anxiety trajectories increase the risk of sleep bruxism at age 7. Many studies have reported that more girls than girls suffer from anxious manifestations [41]. Therefore, a gender interaction with separation anxiety trajectories was tested (objective 3). Given previous evidence on associations between sleep bruxism and reported child general anxiety [16–20], we hypothesized that children with a High-Increasing separation anxiety trajectory would be at higher risk for later sleep bruxism even after controlling for general anxiety-related factors and other covariates such as child’ sex, child’s age, and socioeconomic status (SES).
Methods
Sample description
This study is part of the Québec Longitudinal Study of Child Development (QLSCD), a large epidemiological study conducted by the Québec Institute of Statistics (Canada). Children were recruited from the Québec Master Birth Registry of the Ministry of Health and Social Services. A randomized three-level stratified survey design was used to obtain a representative sample of children born in 1997 and 1998 in the province of Québec (Canada). The first level was the geographic region of Québec. For the second level, each region was subdivided into areas representing the number of births in the region. Third, the number of children selected per area was proportional to the number of births and the gender ratio for the area. Families living in northern Québec, the Inuit territories, and First Nations reserves were excluded for technical reasons. Of the 2940 children initially selected, 265 were excluded, leaving 2675 who were invited to participate. Of these, 452 families declined to participate. The final longitudinal sample, therefore, comprised 2120 children (born in 1997 or 1998) aged 5.0 ± 0.5 months. Table 1 presents the number of families included at each measurement time. In the initial cohort, most (88.1%) children had a Canadian nonimmigrant mother and 11.9% were first-generation immigrants. The majority were Caucasian (90.8%, including 1.2% Arab), with minorities of Blacks (2.8%), Native Amerindians (0.3%), and Asians (2.2%). Most mothers spoke French as a first language (81.1%), with 9.1% English and 9.8% another language.
Table 1.
Means and frequencies for the variables assessed at each measurement time
| Variables | Measurement time (age in months ± SD) | |||||||
|---|---|---|---|---|---|---|---|---|
| 5 months 5.03 ± 0.46 (n = 2120) | ~1.5 year 16.6 ± 0.6 (n = 2045) | ~2.5 years 28.5 ± 0.5 (n = 1997) | ~3.5 years 40.6 ± 0.6 (n = 1950) | ~4 years 49.5 ± 3.1 (n = 1944) | ~5 years 61.4 ± 3.1 (n = 1759) | ~6 years 73.8 ± 3.1 (n = 1492) | ~7 years 85.8 ± 3.1 (n = 1325) | |
| Trajectory measures | ||||||||
| Separation anxiety, mean (SD) | 2.59 (2.09) | 2.71 (2.40) | 3.25 (2.37) | 2.69 (2.22) | 2.31 (1.73) | 2.07 (1.72) | n.a. | |
| Sleep bruxism, yes (%) | 7.1 | 10.9 | 17.6 | 22.4 | 28.7 | 32.7 | 34.7 | |
| Covariates | ||||||||
| Male gender (%) | 50.9 | |||||||
| Child’s age (at 5 mo), mean (SD) | 5.03 (0.46) | |||||||
| Child general anxiety, mean (SD) | 1.20 (1.40) | |||||||
| Socioeconomic status, mean (SD) | 0.00 (1.00) |
Data are courtesy of the Québec Institute of Statistics. n.a.: non-applicable; mo: age in months; SA was not measured at age 7.
Outcome measures
Data were collected with a questionnaire and an interview in English or French according to the participant’s preference.
Sleep bruxism
Sleep bruxism was defined based on parental reports of audible nighttime sleep bruxism. The Self-Administered Questionnaire for Mother, a paper and pencil questionnaire completed by the mother, was used to collect information on sleep bruxism occurrence from age 1.5 to 7 years. Sleep bruxism was measured by the following question: “Does your child grind his/her teeth during the night?” Responses were rated on a Likert scale (1 = never, 2 = sometimes, 3 = often, and 4 = always). Because this parasomnia does not necessarily occur daily or even weekly, it was considered present for the responses sometimes, often, or always (yes) versus never (no).
Separation anxiety
Four distinct developmental separation anxiety trajectories from infancy to school entry were reused in the present article: Low-Persistent separation anxiety (60.2%), High-Increasing separation anxiety (6.9%), High-Decreasing separation anxiety (10.8%), and Low-Increasing separation anxiety (22.1%), based on separation anxiety scores from age 1.5 to 6 years on the Interviewer-Completed Computerized Questionnaire. This face-to-face structured interview with the mother assesses the child’s social development. Child’s separation anxiety scores were obtained at age 1.5, 2.5, 3.5, 4, 5, and 6 years with three items adapted from the Child Behavior Checklist [42]: “In the past 3 months, how often would you say your child: (1) reacts badly when a parent is away?; (2) does not want to sleep alone?; and (3) clings to adults or is too dependent?” Responses were rated on a Likert scale (0 = never; 1 = sometimes; 2 = often). The means scores were rescaled (10 * (x – min) / (max – min)) to a range of 0 to 10. Internal consistency of these subscales was determined acceptable with ordinal coefficient alpha (0.74–0.78 for “reacts badly when the child is away”; 0.52–0.60 for “does not want to sleep alone”; 0.70–0.77 for “clings to adults or is too dependent”) using polychoric correlations [43]. Cronbach alphas (mean = 0.80) were also consistently high across measurements.
Covariate factors
Child’s sex and child’s age at baseline (5 months) were included as covariates. SES was calculated according to the method described in Desrosiers et al. [44] using a combination of three sources: (1) parents’ occupation, (2) maternal education status, and (3) family income in the past year when the child was 1.5 years old. Child’s general anxiety was assessed when the child was 1.5 years old with four questions answered by the mother on the Interviewer-Completed Computerized Questionnaire: “In the past 3 months, how often would you say your child (1) appears fearful or anxious?; (2) appears worried?; (3) sounds unhappy or sad?; and (4) cries a lot?” Responses were rated on a Likert scale (0 = never; 1 = sometimes; 2 = often). The means scores were rescaled (10 * (x – min) / (max – min)) to a range of 0 to 10. Internal consistency of this subscale (0.64) was determined acceptable with ordinal coefficient alpha using polychoric correlations [43]. Child’s general anxiety at age 1.5 was significantly associated with separation anxiety across age (r = 0.08–0.36, p < 0.01).
Statistical analysis
Frequency analyses were used to determine sleep bruxism prevalence rates and descriptive analyses to determine separation anxiety scores at each age. In order to describe developmental sleep bruxism trajectories in early childhood (age 1.5 to 6 years) (objective 1), semiparametric modeling [45] was used. Trajectory models allowing 2 to 5 trajectories with different slope shapes (intercept (0), linear (1), quadratic (2), and cubic (3)) were estimated and compared using the PROC TRAJ SAS procedure [46]. The maximum Bayesian information criterion (BIC) was used to determine the optimal number and shape of trajectories that best fit the data. Individual children were then assigned to specific sleep bruxism trajectories (calculated with a binary logit model) based on the highest probability of belonging. To judge the adequacy of the sleep bruxism model, three criteria were used [47]: (1) average group posterior probability (AvePP) should be greater than 0.70, suggesting that individuals are very accurately placed into a trajectory group; (2) odds of correct classification (OCC) of 5 or more are recommended for all groups and; (3) the difference between estimated group probabilities and the proportions (|π-P|) approaches zero, indicating good model fit to the data. A similar procedure was applied to identify groups of children with similar separation anxiety trajectories (but calculated with a censored normal model) [46]. Frequency analyses were used to determine sleep bruxism prevalence rates and descriptive analyses to determine separation anxiety scores at each age.
Chi-square and Cramer’s V tests were used to investigate associations between trajectories of sleep bruxism and separation anxiety (objective 2) using SPSS version 24 [49] with p set at <0.01. The conditional probabilities were estimated with a joint trajectory model [48] to determine associations between the developmental trajectories of the two outcomes.
Logistic regressions were performed to determine whether distinct developmental separation anxiety trajectories increase the risk of presenting sleep bruxism during the first year of elementary school (objective 3). Families with complete data (n = 1325) compared with those not included in the logistic regressions (n = 803) differed on family income, immigrant status, maternal education, and family type (calculated effect sizes are small). However, to ensure the validity of the data, missing data were handled with full information maximum likelihood (FIML), which uses maximum likelihood to estimate model parameters using all available raw data [50, 51]. Model 1 contains covariates such as child’s sex, child’s age at 5 months, SES, and child’s general anxiety at age 1.5 years as well as separation anxiety trajectories. Model 2a includes all the variables from Model 1 and the sleep bruxism trajectories. Model 2b includes all the variables from Model 1 and the initial measure of sleep bruxism at age 1.5. An interaction term between child’s sex and separation anxiety trajectories was also tested. All analyses were run in Mplus version 8.1, 1998–2018 [52].
Ethical aspects
The ethics review committee of the Québec Institute of Statistics, which was responsible for data collection, approved this study. Before participating in the study, all families received detailed information by mail on the study aims and procedures, and all signed an informed consent form at each measurement time.
Results
Changes in sleep bruxism and separation anxiety in early childhood
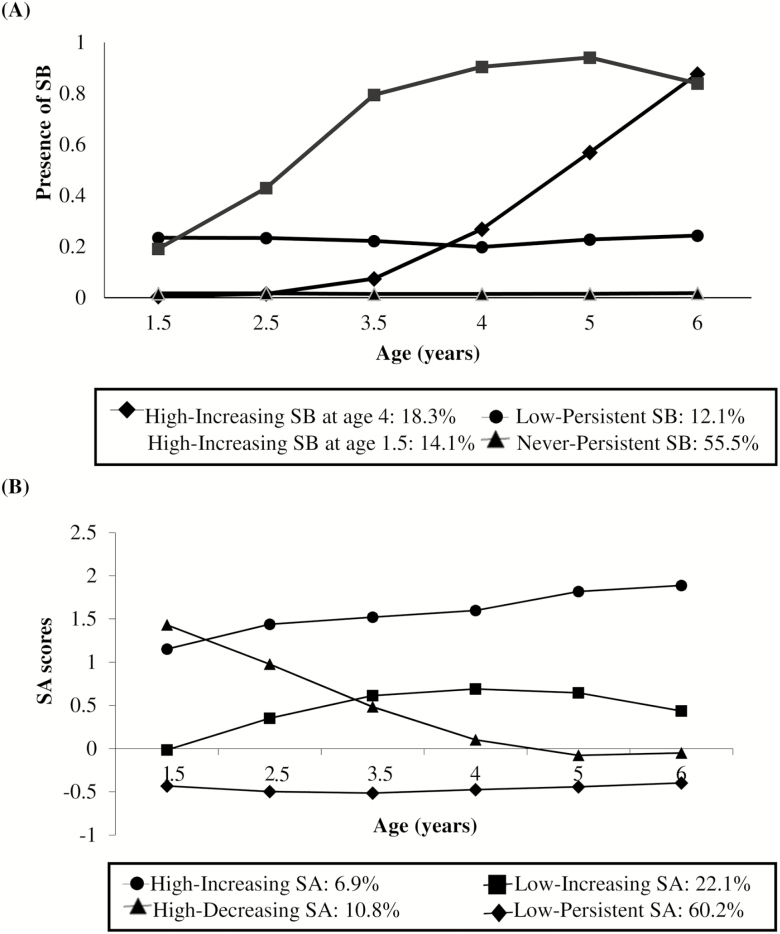
Table 1 presents the prevalence rates for sleep bruxism from age 1.5 to 7 and the separation anxiety scores from age 1.5 to 6. Based on maternal reports, the sleep bruxism prevalence rates varied from 7.1% to 34.7% (from age 1.5 to 7). Figure 1A shows four sleep bruxism trajectories that showed the best fit to the parent-rated sleep bruxism scores from age 1.5 (Time 2) to 6 (Time 7), thus providing the most parsimonious and useful model [53] (BIC = −3726.01, n = 1840) with the following profile: 1 (linear slope), 0 (constant slope), 0 (constant slope), and 3 (cubic slope). The most common trajectory, Never-Persistent sleep bruxism (n = 1021 (55.5%), AvePP = 0.89, OCC = 6.97, |π-P| = 0.019), showed a constant pattern of no sleep bruxism manifestations throughout early childhood. The Low-Persistent sleep bruxism trajectory (n = 223 (12.1%), AvePP = 0.58, OCC = 9.26, |π-P| = 0.009) showed a constant pattern of low sleep bruxism manifestations throughout early childhood. Two trajectories showed noticeable changes with time. First, the High-Increasing sleep bruxism at age 4 trajectory (n = 337 (18.3%), AvePP = 0.72, OCC = 11.95, |π-P| = 0.006) included children with initially low SB manifestations that increased steadily from age 4. Second, the High-Increasing sleep bruxism at age 1.5 trajectory (n = 259 (14.1%), AvePP = 0.92, OCC = 61.17, |π-P| = 0.017) showed a clear pattern of high sleep bruxism manifestations that increased steadily up to age 5.
Figure 1.
Data courtesy of the Québec Institute of Statistics. (A) SB trajectories identified from age 1.5 to 6 years. (B) SA trajectories identified from age 1.5 to 6 years. Note that Panel B was previously published in J Child Psychol Psychiatr; Battaglia et al. [40].
Figure 1B (previously published [40]) shows the four identified separation anxiety trajectories that best fit the data (BIC = −13942.45, n = 1933), with the following profile: 2 (quadratic slope), 2 (quadratic slope), 3 (cubic slope), and 1 (linear slope). The most populous group was the Low-Persistent separation anxiety trajectory (n = 1163, 60.2%), followed by three smaller groups with distinct separation anxiety developmental paths: High-Increasing separation anxiety (n = 134, 6.9%), High-Decreasing separation anxiety (n = 209, 10.8%), and Low-Increasing separation anxiety (n = 427, 22.1%).
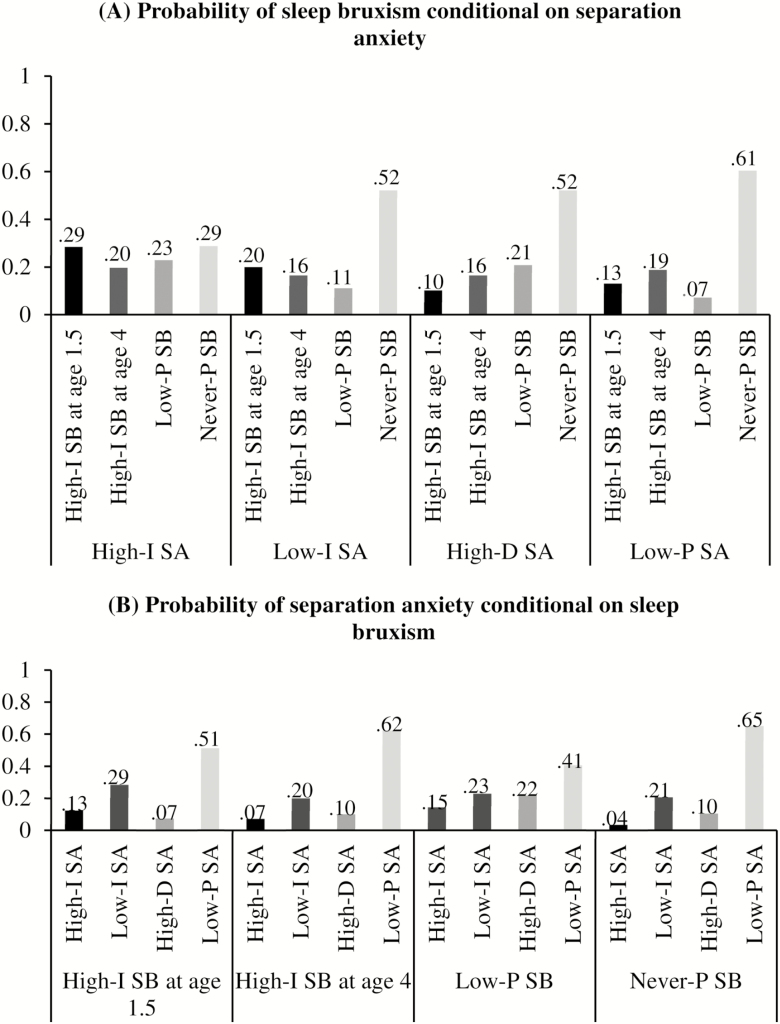
As seen in Table 2, the sleep bruxism and separation anxiety trajectories are weakly associated (X2 = 37.84, Cramer’s V = 0.08, p < 0.001). Figure 2A shows the probability of membership in each sleep bruxism trajectory conditional on membership in each separation anxiety trajectory. Children in the High-Increasing separation anxiety trajectory had .29 probability of membership in the High-Increasing sleep bruxism at age 1.5 trajectory, whereas children in the Low-Persistent separation anxiety trajectory had .13 probability of membership in the High-Increasing sleep bruxism at age 1.5 trajectory. In contrast, children in the High-Increasing separation anxiety trajectory had 0.29 probability of membership in the Never-Persistent sleep bruxism trajectory and children in the Low-Persistent separation anxiety trajectory had 0.61 probability of membership in the Never-Persistent sleep bruxism trajectory. Figure 2B shows the membership probability for each separation anxiety trajectory conditional on membership in each sleep bruxism trajectory. Children belonging to the High-Increasing sleep bruxism at age 1.5 trajectory had 0.13 probability of membership in the High-Increasing separation anxiety trajectory, whereas children in the Never-Persistent sleep bruxism trajectory had 0.04 probability of membership in the High-Increasing separation anxiety trajectory.
Table 2.
Co-occurrence between separation anxiety and sleep bruxism trajectories from age 1.5 to 6 years (n = 1834)
| High-Increasing sleep bruxism at age 4 (n = 337) | High-Increasing sleep bruxism at age 1.5 (n = 258) | Low-Persistent sleep bruxism (n = 223) | Never-Persistent sleep bruxism (n = 1016) | |
|---|---|---|---|---|
| High-Increasing SA (n = 119) | 25 (1.4%) | 30 (1.6%) | 20 (1.1%) | 44 (2.4%) |
| Low-Increasing SA (n = 404) | 65 (3.5%) | 68 (3.7%) | 50 (2.7%) | 221 (12.1%) |
| High-Decreasing SA (n = 191) | 36 (2.0%) | 20 (1.1%) | 35 (1.9%) | 100 (5.5%) |
| Low-Persistent SA (n = 1120) | 211 (11.5%) | 140 (7.6%) | 118 (6.4%) | 651 (35.5%) |
Data are courtesy of the Québec Institute of Statistics. SA: separation anxiety. Chi-squared test was used (X2 = 37.84, Cramer’s V = 0.08, p < 0.001).
Figure 2.
Data courtesy of the Québec Institute of Statistics. (A) The probability of membership in each sleep bruxism trajectory conditional on membership in each separation anxiety trajectory group. (B) The probability of membership in each separation anxiety trajectory conditional on membership in each sleep bruxism trajectory group. Because the probabilities are conditional on membership in a given trajectory, the four columns sum to 1.
Factors associated with sleep bruxism occurrence at age 7
Table 3 presents three logistic regression models that predict sleep bruxism at age 7. No significant interactions between child’s sex and separation anxiety trajectories were found. Therefore, the interaction term was excluded from the three models. Compared with children in the Low-Persistent separation trajectory, Model 1 shows that children in the High-Increasing separation anxiety trajectory had about twice the risk of presenting sleep bruxism at age 7 (OR = 2.23, 95% CI = 1.39–3.56, p = 0.02). After controlling for sleep bruxism trajectories, Model 2a shows that the separation anxiety trajectories were no longer significantly associated with sleep bruxism at age 7, whereas the sleep bruxism trajectories were strongly associated with sleep bruxism at age 7. Thus, children in the High-Increasing sleep bruxism at age 4 trajectory or the High-Increasing sleep bruxism at age 1.5 trajectory had 21 to 30 times the risk of sleep bruxism at age 7 compared to children in the Never-Persistent sleep bruxism trajectory. However, compared to children in the Low-Persistent separation anxiety trajectory, Model 2b shows that children in the High-Increasing separation anxiety trajectory still had about twice the risk of presenting sleep bruxism at age 7, even after controlling for the same variables as in Model 1 and the initial sleep bruxism measure at age 1.5 (OR = 2.01, 95% CI = 1.25–3.22, p = 0.04). No significant effect was found for child’s sex, child’s age at baseline (5 months), SES at age 1.5, or general anxiety at age 1.5.
Table 3.
Logistic regression models to predict sleep bruxism at age 7
| Odds ratio (95% CI) | p | |
|---|---|---|
| Model 1 (n = 1283) | ||
| Covariates | ||
| Male gender, female (ref) | 1.26 (0.99–1.58) | 0.09 |
| Child’s age at baseline (5 months) | 1.20 (0.92–1.56) | 0.23 |
| Socioeconomic status at 1.5 years | 1.10 (0.97–1.25) | 0.17 |
| General anxiety scores at 1.5 years | 0.98 (0.90–1.07) | 0.63 |
| Separation anxiety trajectories a | ||
| High-Increasing separation anxiety | 2.23 (1.39–3.56) | 0.02 |
| High-Decreasing separation anxiety | 1.23 (0.83–1.84) | 0.35 |
| Low-Increasing separation anxiety | 1.24 (0.92–1.67) | 0.20 |
| Model 2a (n = 1283) | ||
| Covariates | ||
| Male gender, female (ref) | 1.14 (0.85–1.54) | 0.41 |
| Child’s age at baseline (5 months) | 1.11 (0.80–1.56) | 0.55 |
| Socioeconomic status at 1.5 years | 1.06 (0.90–1.25) | 0.48 |
| General anxiety scores at 1.5 years | 1.00 (0.89–1.11) | 0.94 |
| Sleep bruxism trajectoriesb | ||
| High-Increasing sleep bruxism at 4 years | 21.01 (14.57–30.30) | <0.001 |
| High-Increasing sleep bruxism at 1.5 years | 30.36 (19.62–46.98) | <0.001 |
| Low-Persistent sleep bruxism | 2.73 (1.76–4.23) | 0.005 |
| Separation anxiety trajectories a | ||
| High-Increasing separation anxiety | 1.26 (0.64–2.50) | 0.55 |
| High-Decreasing separation anxiety | 1.31 (0.79–2.17) | 0.36 |
| Low-Increasing separation anxiety | 1.10 (0.76–1.59) | 0.63 |
| Model 2b (n = 1306) | ||
| Covariates | ||
| Male gender, female (ref) | 1.22 (0.97–1.54) | 0.12 |
| Child aged 5 months | 1.17 (0.91–1.52) | 0.26 |
| Socioeconomic status at 1.5 years | 1.10 (0.97–1.25) | 0.15 |
| General anxiety scores at 1.5 years | 0.98 (0.90–1.06) | 0.57 |
| Sleep bruxism at 1.5 years | 1.75 (1.13–2.70) | 0.05 |
| Separation anxiety trajectories a | ||
| High-Increasing separation anxiety | 2.01 (1.25–3.22) | 0.04* |
| High-Decreasing separation anxiety | 1.13 (0.76–1.69) | 0.56 |
| Low-Increasing separation anxiety | 1.19 (0.89–1.60) | 0.28 |
For each model, all covariates were considered simultaneously. No significant interactions between child’s sex and separation anxiety trajectories were found. Therefore, the interaction term was not included in the three models. Data are courtesy of the Québec Institute of Statistics. 95% CI: 95% confidence interval.
aCompared with the Low-persistent separation anxiety trajectory.
bCompared with the Never-persistent bruxism trajectory.
*p < 0.05.
Discussion
The first objective of this paper was to describe developmental sleep bruxism trajectories during early childhood in a nonclinical population. We found two progressions of sleep bruxism in early childhood. First, 14.1% of the children showed increasing sleep bruxism manifestations from age 1.5 to 5 years. Second, another 18.3% showed increasing sleep bruxism manifestations from age 4 to 6. Future studies should investigate these two sleep bruxism progressions further to better understand the etiology in association with other parasomnias. The high prevalence of these sleep bruxism trajectories (approximately 32.4%) highlights the importance of understanding how sleep bruxism unfolds in the preschool and early school years [54].
The second objective was to investigate associations between sleep bruxism trajectories and separation anxiety trajectories. A previous study [9] obtained associations between separation anxiety and sleep bruxism. In the present longitudinal study, a weak co-occurrence between trajectories of separation anxiety and sleep bruxism was found. These results indicate that children belonging to the High-Increasing separation anxiety trajectory had greater probability of membership in the High-Increasing sleep bruxism at age 1.5 compared to children in the Low-Persistent separation anxiety trajectory. In contrast, children in the High-Increasing separation anxiety trajectory had lower probability of membership in the Never-Persistent sleep bruxism trajectory compared to children in the Low-Persistent separation anxiety trajectory. Considering that studies have identified abnormal respiratory patterns in both conditions (separation anxiety and sleep bruxism) [37–39], future studies should test whether a common neural substrate that underlies abnormal respiratory patterns could explain the association between these two conditions. Given that children with SAD have reported hypersensitivity to CO2 [37, 38], a condition that is associated with specific biological markers [55], it would be informative to test these biological markers in sleep bruxism.
The third objective was to examine whether distinct developmental separation anxiety trajectories increase the risk of presenting sleep bruxism during the first year of elementary school. Sleep bruxism etiology is a combination of pathophysiological and psychological factors [11]. Other studies [9, 56] have determined that the prevalence of sleep bruxism during preschool years did not differ significantly between girls and boys. We found that sleep bruxism trajectories were strongly associated with sleep bruxism at age 7, suggesting a persistent association. Not surprisingly, this association is so strong that separation anxiety trajectories are no longer significantly associated with sleep bruxism at age 7. Interestingly, after controlling for the initial measure of sleep bruxism at age 1.5, child’s sex, child’s age at baseline (5 months), SES, and child’s general anxiety at age 1.5, children belonging to the High-Increasing separation anxiety trajectory had about twice the risk of sleep bruxism at age 7 compared to children belonging to the Low-Persistent separation anxiety trajectory. This result underlines the importance of assessing separation anxiety to help target the underlying mechanisms of sleep bruxism manifestations. Age 7 years coincides with the first year of elementary school, a major, daily event involving separation that may strengthen the association between sleep bruxism and separation anxiety. This result also highlights the need to consider separation anxiety as a risk factor, along with other psychological aspects associated with sleep bruxism in children [57–59].
Limitations and strengths
The first limitation is that our study design did not allow determining causal relationships. Second, we used maternal self-reports, such that mothers could have underreported or overreported sleep bruxism and separation anxiety scores. Future longitudinal studies could gain more insight by gathering teacher reports of separation anxiety and by including objective measures of sleep bruxism such as polysomnographic and audio-video recordings. Furthermore, because our population was mainly Caucasian, which is hardly representative of the wider population, our results should be replicated in other population samples. Unfortunately, although facial pain is a potential covariate factor that could be associated with anxiety [60], it was not measured in the present study and should be considered in future studies. Despite these limitations, useful prospective and longitudinal data on reported sleep bruxism and separation anxiety were collected from a large population sample throughout early childhood.
Conclusion
Psychiatrists and family psychotherapists who detect separation anxiety in young children could recommend that parents provide their child with regular dental checkups to detect and monitor signs of sleep bruxism. A better understanding of separation anxiety as a risk factor in sleep bruxism etiology could improve psychological treatment approaches for children suffering from sleep bruxism. Future studies should explore whether different types of anxieties and worries (e.g. panic disorders) may be associated with different bruxing subtypes (e.g. daytime vs. nocturnal). An innovative research avenue would be to explore whether psychological treatment for separation anxiety can reduce the intensity of sleep bruxism manifestations in children.
Funding
This study was funded by the Ministère de la Santé et des Services sociaux (Québec City, Québec, Canada), the Canadian Institutes of Health Research (Ottawa, Ontario, Canada), the Social Sciences and Humanities Research Council of Canada (Ottawa, Ontario, Canada), the Fonds de recherche du Québec – Société et culture (Québec City, Québec, Canada), the Fonds québécois de la recherche sur la nature et les technologies (Québec City, Québec, Canada), and the Fonds de recherche du Québec – Santé (Québec City, Québec, Canada).
Conflict of interest statement. None declared.
Acknowledgments
We thank the children and families whose ongoing participation made this study possible. We acknowledge the considerable contribution of the coordinators of the Québec Longitudinal Study of Child Development and the Québec Institute of Statistics, as well as the tireless work of all the interviewers who met with the mothers and children in this study. We are grateful to Hélène Paradis and Bei Feng for their invaluable statistical expertise on the sleep bruxism and separation anxiety trajectories and the joint trajectories. The second author (director) had full access to all the study data, and takes responsibility for the data integrity and accuracy.
References
- 1. American Academy of Sleep Medicine. International Classification of Sleep Disorders. 2nd Ed. Diagnostic and Coding Manual. Westchester, IL: American Academy of Sleep Medicine; 2005. [Google Scholar]
- 2. Sateia MJ. International classification of sleep disorders-third edition: highlights and modifications. Chest. 2014;146(5):1387–1394. [DOI] [PubMed] [Google Scholar]
- 3. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.Arlington, VA: American Psychiatric Association; 2013. [Google Scholar]
- 4. Laberge L, et al. Development of parasomnias from childhood to early adolescence. Pediatrics. 2000;106(1 Pt 1):67–74. [DOI] [PubMed] [Google Scholar]
- 5. Lam MH, et al. A community study of sleep bruxism in Hong Kong children: association with comorbid sleep disorders and neurobehavioral consequences. Sleep Med. 2011;12(7):641–645. [DOI] [PubMed] [Google Scholar]
- 6. Machado E, et al. Prevalence of sleep bruxism in children: a systematic review. Dental Press J Orthod. 2014;19(6):54–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Serra-Negra JM, et al. Relationship between tasks performed, personality traits, and sleep bruxism in Brazilian school children–a population-based cross-sectional study. PLoS One. 2013;8(11):e80075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Manfredini D, et al. Prevalence of sleep bruxism in children: a systematic review of the literature. J Oral Rehabil. 2013;40(8):631–642. [DOI] [PubMed] [Google Scholar]
- 9. Petit D, et al. Dyssomnias and parasomnias in early childhood. Pediatrics. 2007;119(5):e1016–e1025. [DOI] [PubMed] [Google Scholar]
- 10. Kato T, et al. Age is associated with self-reported sleep bruxism, independently of tooth loss. Sleep Breath. 2012;16(4):1159–1165. [DOI] [PubMed] [Google Scholar]
- 11. Lavigne GJ, et al. Bruxism physiology and pathology: an overview for clinicians. J Oral Rehabil. 2008;35(7):476–494. [DOI] [PubMed] [Google Scholar]
- 12. Carvalho ABM, et al. Bruxism and quality of life in schoolchildren aged 11 to 14. Cien Saude Colet. 2015;20(11): 3385–3393. [DOI] [PubMed] [Google Scholar]
- 13. Pingitore G, et al. The social and psychologic factors of bruxism. J Prosthet Dent. 1991;65(3):443–446. [DOI] [PubMed] [Google Scholar]
- 14. Castelo PM, et al. Quality of life evaluation of children with sleep bruxism. BMC Oral Health. 2010;10:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Montaldo L, et al. Association between exposure to secondhand smoke and sleep bruxism in children: a randomised control study. Tob Control. 2012;21(4):392–395. [DOI] [PubMed] [Google Scholar]
- 16. Serra-Negra JM, et al. Influence of psychosocial factors on the development of sleep bruxism among children. Int J Paediatr Dent. 2009;19(5):309–317. [DOI] [PubMed] [Google Scholar]
- 17. Serra-Negra JM, et al. Association among stress, personality traits, and sleep bruxism in children. Pediatr Dent. 2012;34(2):e30–e34. [PubMed] [Google Scholar]
- 18. Gungormus Z, et al. Evaluation of the relationship between anxiety and depression and bruxism. J Int Med Res. 2009;37(2):547–550. [DOI] [PubMed] [Google Scholar]
- 19. Bader G, et al. Sleep bruxism; an overview of an oromandibular sleep movement disorder. REVIEW ARTICLE. Sleep Med Rev. 2000;4(1):27–43. [DOI] [PubMed] [Google Scholar]
- 20. Oliveira MT, et al. Sleep bruxism and anxiety level in children. Braz Oral Res. 2015;29(1):1–5. [DOI] [PubMed] [Google Scholar]
- 21. Castelo PM, et al. Awakening salivary cortisol levels of children with sleep bruxism. Clin Biochem. 2012;45(9):651–654. [DOI] [PubMed] [Google Scholar]
- 22. Kobayashi FY, et al. Salivary stress biomarkers and anxiety symptoms in children with and without temporomandibular disorders. Braz Oral Res. 2017;31:e78. [DOI] [PubMed] [Google Scholar]
- 23. Clark GT, et al. Nocturnal masseter muscle activity and urinary catecholamine levels in bruxers. J Dent Res. 1980;59(10):1571–1576. [DOI] [PubMed] [Google Scholar]
- 24. Mascaro MB, et al. Alternative pathways for catecholamine action in oral motor control. Neurosci Lett. 2005;386(1):34–39. [DOI] [PubMed] [Google Scholar]
- 25. Vanderas AP, et al. Urinary catecholamine levels and bruxism in children. J Oral Rehabil. 1999;26(2):103–110. [DOI] [PubMed] [Google Scholar]
- 26. Beesdo K, et al. Anxiety and anxiety disorders in children and adolescents: developmental issues and implications for DSM-V. Psychiatr Clin North Am. 2009;32(3):483–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Carpenter KLH, et al. Quantifying risk for anxiety disorders in preschool children: a machine learning approach. PLoS One. 2016;11(11):e0165524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kessler RC, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):768. [DOI] [PubMed] [Google Scholar]
- 29. Shear K, et al. Prevalence and correlates of estimated DSM-IV child and adult separation anxiety disorder in the National Comorbidity Survey Replication. Am J Psychiatry. 2006;163(6):1074–1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ginsburg GS, et al. Naturalistic follow-up of youths treated for pediatric anxiety disorders. JAMA Psychiatry. 2014;71(3):310–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Battaglia M, et al. Early childhood trajectories of separation anxiety: bearing on mental health, academic achievement, and physical health from mid-childhood to preadolescence. Depress Anxiety. 2017;34(10):918–927. [DOI] [PubMed] [Google Scholar]
- 32. Bandelow B, et al. Separation anxiety and actual separation experiences during childhood in patients with panic disorder. Can J Psychiatry. 2011;46(10):948–952. [DOI] [PubMed] [Google Scholar]
- 33. Copeland WE, et al. Longitudinal patterns of anxiety from childhood to adulthood: the Great Smoky Mountains Study. J Am Acad Child Adolesc Psychiatry. 2014;53(1):21–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Cartwright-Hatton S, et al. Anxiety in a neglected population: prevalence of anxiety disorders in pre-adolescent children. Clin Psychol Rev. 2006;26(7):817–833. [DOI] [PubMed] [Google Scholar]
- 35. Scher A. Maternal separation anxiety as a regulator of infants’ sleep. J Child Psychol Psychiatry. 2008;49(6):618–625. [DOI] [PubMed] [Google Scholar]
- 36. Archbold KH, et al. Symptoms of sleep disturbances among children at two general pediatric clinics. J Pediatr. 2002;140(1):97–102. [DOI] [PubMed] [Google Scholar]
- 37. Pine DS, et al. Differential carbon dioxide sensitivity in childhood anxiety disorders and nonill comparison group. Arch Gen Psychiatry. 2000;57(10):960–967. [DOI] [PubMed] [Google Scholar]
- 38. Battalglia M, et al. A genetically informed study of the association between childhood separation anxiety, sensitivity to CO(2), panic disorder, and the effect of childhood parental loss. Arch Gen Psychiatry. 2009;66(1):64–71. [DOI] [PubMed] [Google Scholar]
- 39. Lavigne GJ, et al. Sleep Bruxism. Principles and Practice of Sleep Medicine, 4th ed.Philadelphia, PA: Elsevier Saunders; 2005:946–959. [Google Scholar]
- 40. Battaglia M, et al. Distinct trajectories of separation anxiety in the preschool years: persistence at school entry and early-life associated factors. J Child Psychol Psychiatry. 2016;57(1):39–46. [DOI] [PubMed] [Google Scholar]
- 41. Hodes GE, et al. Sex differences in vulnerability and resilience to stress across the life span. Biol Psychiatry. 2019;86(6):421–432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Achenbach TM. Child Behavior Checklist. Burlington, VT: Department of Psychiatry, University of Vermont; 1991. [Google Scholar]
- 43. Zumbo BD, et al. Ordinal versions of coefficients alpha and theta for Likert rating scales. J Mod Appl Stat Methods. 2007;6(1):4. [Google Scholar]
- 44. Desrosiers H, et al. Aspects conceptuels et opérationnels, section II – Les données et les variables dérivées. In: Étude longitudinale du développement des enfants du Québec (ÉLDEQ 1998–2002). Québec, Canada: Institut de la statistique du Québec; 2001;1(12):146. [Google Scholar]
- 45. Nagin DS. Analyzing developmental trajectories: a semiparametric, group-based approach. Psychol Methods. 4(2):139–157. [DOI] [PubMed] [Google Scholar]
- 46. Jones BL, et al. An SAS procedure based on mixture models for estimating developmental trajectories. Sociolo Methods Res. 2001;29(3):374–393. [Google Scholar]
- 47. Niyonkuru C, et al. Group-based trajectory analysis applications for prognostic biomarker model development in severe TBI: a practical example. J Neurotrauma. 2013;30(11):938–945. [DOI] [PubMed] [Google Scholar]
- 48. Jones BL, et al. Advances in group-based trajectory modeling and an SAS procedure for estimating them. Sociol Methods Res. 2007;35(4):542–571. [Google Scholar]
- 49. SPSS Inc. SPSS Base 24.0 for Windows User’s Guide. Chicago, IL: SPSS Inc; 2016. [Google Scholar]
- 50. Arbuckle JL. Full information estimation in the presence of incomplete data. In: Marcoulides GA, Schumacker RE, eds. Advanced Structural Equation Modeling: Issues and Techniques. Mahwah, NJ: Lawrence Erlbaum Associates, Inc.; 1996:243–277. [Google Scholar]
- 51. Wothke W. Longitudinal and multigroup modeling with missing data. In: Modeling Longitudinal and Multilevel Data: Practical Issues, Applied Approaches, and Specific Examples. Mahwah, NJ: Lawrence Erlbaum Associates Publishers; 2000:219–281. [Google Scholar]
- 52. Muthén LK, Muthén BO.. Mplus User’s Guide. 8th Edition Los Angeles, CA: Muthén & Muthén; 1998–2018. [Google Scholar]
- 53. Nagin DS, et al. Group-based trajectory modeling in clinical research. Annu Rev Clin Psychol. 2010;6:109–138. [DOI] [PubMed] [Google Scholar]
- 54. de Alencar NA, et al. Sleep bruxism and anxiety impacts in quality of life related to oral health of brazilian children and their families. J Clin Pediatr Dent. 2017;41(3): 179–185. [DOI] [PubMed] [Google Scholar]
- 55. Battaglia M, et al. The 35% CO2 challenge in panic disorder: optimization by receiver operating characteristic (ROC) analysis. J Psychiatr Res. 1995;29(2):111–119. [DOI] [PubMed] [Google Scholar]
- 56. Kim DS, et al. Sleep problems in children and adolescents at pediatric clinics. Korean J Pediatr. 2017;60(5):158–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Ferreira-Bacci Ado V, et al. Behavioral problems and emotional stress in children with bruxism. Braz Dent J. 2012;23(3):246–251. [DOI] [PubMed] [Google Scholar]
- 58. Goettems ML, et al. Influence of maternal psychological traits on sleep bruxism in children. Int J Paediatr Dent. 2017;27(6):469–475. [DOI] [PubMed] [Google Scholar]
- 59. Kampe T, et al. Personality traits in a group of subjects with long-standing bruxing behaviour. J Oral Rehabil. 1997;24(8):588–593. [DOI] [PubMed] [Google Scholar]
- 60. Svensson P, et al. Relationships between craniofacial pain and bruxism. J Oral Rehabil. 2008;35(7):524–547. [DOI] [PubMed] [Google Scholar]