Introduction
In December 2019, the outbreak of Severe Acute Respiratory Syndrome coronavirus 2 (SARS CoV2) which is the cause of coronavirus disease 19 (COVID-19) has begun in Wuhan, China's Hubei province [1]. The clinical presentations of the novel infection in general population are considered to be fever, dry cough, fatigue, nausea [2]. Patients with underlying diseases and co-morbidities may end up to acute respiratory distress syndrome, and eventually death [3]. The diagnosis of the disease is based on clinical features of the disease, laboratory abnormalities including elevated C-reactive protein, lymphopenia and elevated lactate dehydrogenase which would be confirmed by reverse transcriptase polymerase chain reaction (RT-PCR) test [4]. In this regard, the role of medical imaging, especially chest x-ray and chest computed tomography (CT) scan, is crystal clear [5].
The main chest CT findings in patients with COVID-19 are bilateral ground-glass opacities, consolidations, and septal thickenings [6]. Previous studies have also mentioned that COVID-19 patients could have the CT characteristic features of architectural distortion in a peripheral distribution, ground glass pulmonary nodules and discrete nodules, and multifocal organizing pneumonia [5].
Immunocompromised patients commonly present atypical presentations of viral diseases [7]. For instances, herpes simplex virus and cytomegalovirus had led to esophageal symptoms in patients with human immunodeficiency virus (infection) [8]. Furthermore, previous investigations have reported that viral infection could result pulmonary nodules in immunocompromised patients [9]. Considering the SARS CoV-2, a prior investigation has noticed that the infection in immunocompromised patients may cause gastrointestinal symptoms including nausea, vomiting, and diarrhea [10]. Conversely to the fact that these patients are more susceptible to the infections, there is limited information regarding the features of COVID-19 in immunocompromised population (Figs. 1 and 2).
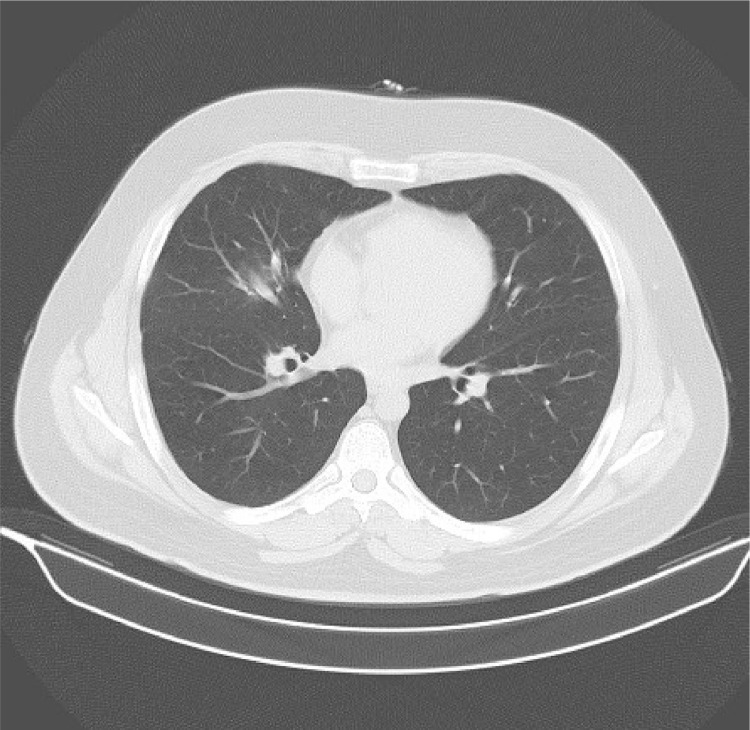
Fig. 1.
A: plain PA chest X-ray reveals a small pulmonary nodule in right lower lobe. B: spiral chest CT scan axial section at level of pulmonary veins demonstrates a 29×27 mm solid nodule with faint peripheral halo of ground glass density.
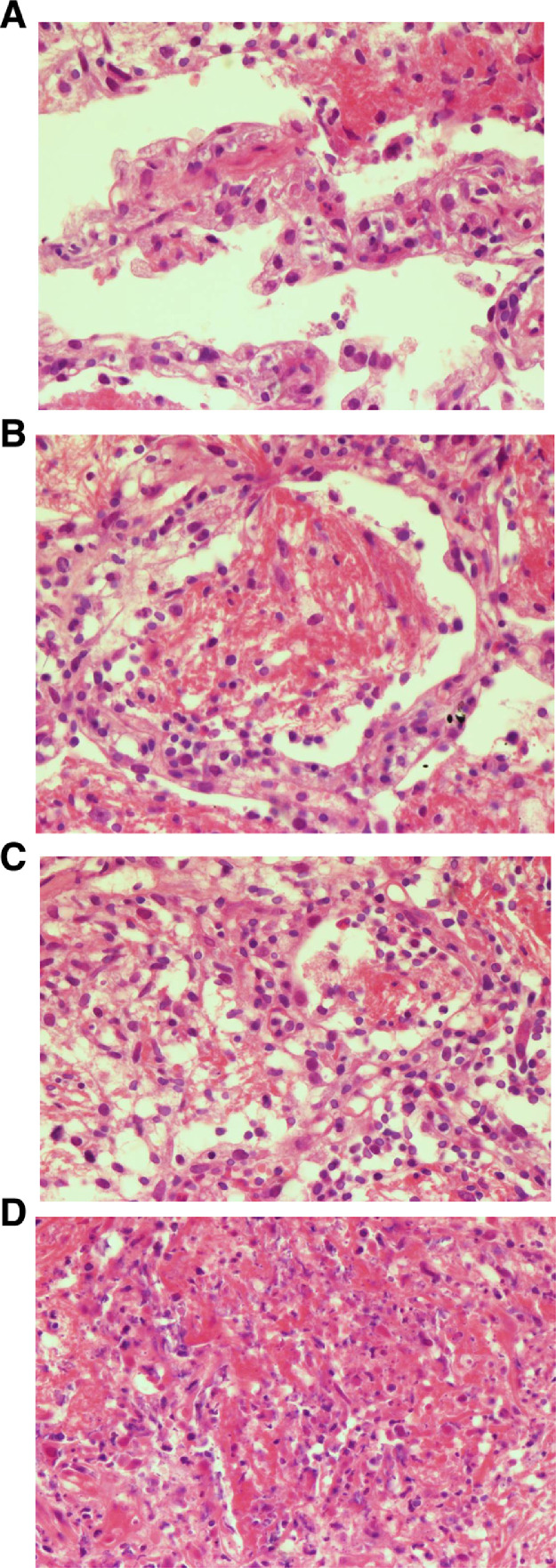
Fig. 2.
Microscopic examination from peripheral border to the center of the lesion show, A: Alveolar wall edema, congestion, infiltration of lymphocytes, neutrophiles and eosinophils and fibrin material deposition, B: Alveolar spaces filled by fibrinoid material deposition admixed with mixed inflammatory cells infiltration, C: Early alveolar destruction with infiltration of inflammatory cells and fibrinoid material deposition, D: Complete destruction of alveolar spaces with necrosis.
Here we report a case of kidney transplant recipient who receives immunosuppressive regimen who was infected with SARS CoV-2. The patient presented the disease as a solitary pulmonary nodule, raising the suspicion of metastases of renal cell carcinoma (RCC). Percutaneous biopsy was done for the patient and the specimen was sent for further evaluation, which diagnosed COVID-19.
Case report
The patient is a 37-year-old man who received live-related renal transplantation for bilateral nephrectomy due to RCC last year, after 3 years of hemodialysis. He is a known case of Von Hippel-Lindau who developed bilateral RCC about 4 years ago and underwent subsequent bilateral nephrectomy. He is on immunosuppressive regimen for a year, since renal transplantation. His medications are as followed: Tacrolimus (1 mg twice a day, orally), Mycophenolate Sodium (500 mg twice a day, orally) and Prednisolone (5 mg daily, orally). On May 1, 2020, he referred to his doctor with mild dyspnea. On physical examination the patient was febrile (38.4°C) and was complaining of shortness of breath. Initial laboratory data were remarkable for mild leukopenia (WBC: 3.5 × 109/L with 19% lymphocytes) and elevated CRP. The subsequently performed chest CT scan revealed a 29 × 27 mm ill-defined solid pulmonary nodule with faint peripheral halo located in superior aspect of the right lower lobe. Despite the suspicion for COVID-19 infection, the primary RT-PCR of the nasopharynx sample was falsely negative. Hence the patient was referred to our center for percutaneous pulmonary nodule biopsy under guide of CT scan. The histopathologic findings revealed alveolar wall edema and congestion. Infiltration of lymphocytes, neutrophils, and eosinophils along with fibrin material deposition. No sign of malignancy was seen. Afterwards, the repeated RT-PCR result was positive for COVID-19 infection. The patient was discharged with conservative treatment and immunosuppressant adjustments. In 2 weeks follow-up CT scan, decrease in size of the nodule was evident alongside the clinical improvement (Fig. 3)
Fig. 3.
Axial section of spiral chest CT scan at level of left atrium in 2 weeks’ follow-up. Significant resolution of the pulmonary nodule is noted leaving a patch of ground glass opacity in superior aspect of right lower lobe.
Discussion
Chronic immunosuppression in transplant recipient population is an important risk factor for development of serious viral infections [11]. Earlier studies have mentioned that the previously known corona viruses including sever acute respiratory syndrome (SARS-CoV) and Middle East respiratory syndrome (MERS-CoV) may result in several complications in solid organ transplant recipients [[12],[13]]. These complications are progressive respiratory symptoms, acute renal failure in kidney recipient patients [13]. Furthermore, influenza infections are more severe and lethal in immunocompromised patients [14].
The first reported renal transplant recipient infected with COVID-19 pneumonia was a 52-year-old man from Wuhan, China, whom clinical and para clinical characteristics were similar to those of nontransplanted patients [15]. Another study also mentioned the same conclusion, as it has found that the clinical, laboratory and radiological characteristics of COVID-19 in immunocompromised patients are similar to the normal population [11]. The dominant chest CT features of these immunocompromised patients are typical multiple patchy ground glass densities, multifocal patchy opacities, and consolidation of subsegmental areas, in both lungs [16], [17], [18].
The CT halo sign has been typically seen in fungal infections, vasculitis, organizing pneumonia, and viral infections [19]. The most common cause of CT halo sign in immunocompromised and immunocompetent patients are pulmonary aspergillosis and malignancy [[20],[21]]. Solid nodules with a peripheral halo of ground glass are reported in a range of 0%-26% in COVID-19 patients and are considered as an atypical imaging presentation so far [22], [23], [24], [25], [26].
Here we report a case of kidney transplant recipient, on immunosuppressive regimen who has presented with a single pulmonary nodule. The patient had done nephrectomy 4 years ago, and received the kidney transplantation 1 year ago. To the best of our knowledge, this is the first report, that presents an immunocompromised patient who shows the COVID-19 as a single pulmonary nodule with peripheral halo.
The results of the real-time RT-PCR test for COVID-19 should be interpreted cautiously, and in cases with negative RT-PCR who shows has the clinical features, several tests should be done [27]. In such cases of negative initial RT-PCR, chest CT scan has a comparable diagnostic performance [28]. In our patient, a case of previous RCC, the negative results of the initial RT-PCR assessment and the atypical imaging presentation, misled the physician and resulted in suspicion for metastasis rather than COVID-19 pulmonary involvement.
We suggest that during the SARS CoV-2 pandemic, the patients who has pulmonary nodule with peripheral halo should be evaluated regarding the COVID-19. However, more investigations with higher study population are needed in this regard for a comprehensive conclusion. On the other hand, the imaging characteristics of COVID-19 in immunocompromised patients and solid organ recipients may differ from the general population and are yet to be investigated.
Ethical Considerations
All experiments were performed according to the Institutional Review Board (IR.sums.med.rec.1395.s125) guidelines that approved by the ethics committee of Shiraz University of Medical Sciences.
Footnotes
Conflict of Interest: The authors declare that there is no conflict of interest regarding the publication of this paper.
Funding: The authors received no financial support for the research and authorship.
Acknowledgments: This research was supported by Research Committee of Shiraz University of Medical Sciences.
References
- 1.Bernheim A., Mei X., Huang M. Chest CT findings in coronavirus disease-19 (COVID-19): relationship to duration of infection. Radiology. 2020;295(3) doi: 10.1148/radiol.2020200463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lovato A., de Filippis C. Clinical presentation of COVID-19: a systematic review focusing on upper airway symptoms. Ear Nose Throat J. 2020 doi: 10.1177/0145561320920762. [DOI] [PubMed] [Google Scholar]
- 3.Huang C., Wang Y., Li X. et al., “Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fu L., Wang B., Yuan T. Clinical characteristics of coronavirus disease 2019 (COVID-19) in China: a systematic review and meta-analysis. J Infect. 2020;80(6):656–665. doi: 10.1016/j.jinf.2020.03.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ai T., Yang Z., Hou H. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 2020 doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu J., Wu X., Zeng W. Chest CT findings in patients with coronavirus disease 2019 and its relationship with clinical features. Investigat Radiol. 2020;55(5):257. doi: 10.1097/RLI.0000000000000670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Krones E., Högenauer C. Diarrhea in the immunocompromised patient. Gastroenterol Clin. 2012;41(3):677–701. doi: 10.1016/j.gtc.2012.06.009. [DOI] [PubMed] [Google Scholar]
- 8.Bonacini M., Young T., Laine L. The causes of esophageal symptoms in human immunodeficiency virus infection: a prospective study of 110 patients. Arch Int Med. 1991;151(8):1567–1572. [PubMed] [Google Scholar]
- 9.Franquet T., Müller N.L., Giménez A. Infectious pulmonary nodules in immunocompromised patients: usefulness of computed tomography in predicting their etiology. J Comput Assist Tomograph. 2003;27(4) doi: 10.1097/00004728-200307000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Guillen E., Pineiro G.J., Revuelta I. Case report of COVID-19 in a kidney transplant recipient: does immunosuppression alter the clinical presentation? Am J Transplant. 2020;20(7):1875–1878. doi: 10.1111/ajt.15874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhu L., Gong N., Liu B. Coronavirus disease 2019 pneumonia in immunosuppressed renal transplant recipients: a summary of 10 confirmed cases in Wuhan, China. Eur Urol. 2020;77(6):748–754. doi: 10.1016/j.eururo.2020.03.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kumar D., Tellier R., Draker R., Levy G., Humar A. Severe Acute Respiratory Syndrome (SARS) in a liver transplant recipient and guidelines for donor SARS screening. Am J Transplant. 2003;3(8):977–981. doi: 10.1034/j.1600-6143.2003.00197.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.AlGhamdi M., Mushtaq F., Awn N., Shalhoub S. MERS CoV infection in two renal transplant recipients: case report. Am J Transpl. 2015;15(4):1101–1104. doi: 10.1111/ajt.13085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.D’Antiga L. Coronaviruses and Immunosuppressed Patients: The Facts During the Third Epidemic. Liver Transpl. 2020;26(6):832–834. doi: 10.1002/lt.25756. [DOI] [PubMed] [Google Scholar]
- 15.Zhu L., Xu X., Ma K. Successful recovery of COVID-19 pneumonia in a renal transplant recipient with long-term immunosuppression. Am J Transplant. 2020;20(7):1859–1863. doi: 10.1111/ajt.15869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abrishami A., Samavat S., Behnam B. Clinical course, imaging features, and outcomes of COVID-19 in kidney transplant recipients. Eur Urol. 2020 doi: 10.1016/j.eururo.2020.04.064. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nair V., Jandovitz N., Hirsch J.S. COVID‐19 in kidney transplant recipients. Am J Transpl. 2020;20(7):1819–1825. doi: 10.1111/ajt.15967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Siddiqi H., Mehra M. COVID-19 illness in native and immunosuppressed states: A clinical-therapeutic staging proposal. J Heart Lung Transplant. 2020;39(5):405–407. doi: 10.1016/j.healun.2020.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee Y.R., Choi Y.W., Lee K.J. CT halo sign: the spectrum of pulmonary diseases. Br J Radiol. 2005;78(933):862–865. doi: 10.1259/bjr/77712845. [DOI] [PubMed] [Google Scholar]
- 20.Alves G.R., Marchiori E., Irion K. The halo sign: HRCT findings in 85 patients. J Bras Pneumol. 2016;42(6):435–439. doi: 10.1590/S1806-37562015000000029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ray A., Mittal A., Vyas S. "CT Halo sign - a systematic review and meta analysis. Eur Respir J. 2019;54(suppl 63):PA4819. [Google Scholar]
- 22.Ye Z., Zhang Y., Wang Y., Huang Z., Song B. Chest CT manifestations of new coronavirus disease 2019 (COVID-19): a pictorial review. Eur Radiol. 2020 doi: 10.1007/s00330-020-06801-0. . In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.S. Haseli, N. Khalili, M. Bakhshayeshkaram, M. Sanei-Taheri, and Y. Moharramzad, “Lobar distribution of COVID-19 pneumonia based on chest computed tomography findings; a retrospective study,” 2020, vol. 8, no. 1, 2020. [PMC free article] [PubMed]
- 24.Lomoro P., Verde F., Zerboni F. COVID-19 pneumonia manifestations at the admission on chest ultrasound, radiographs, and CT: single-center study and comprehensive radiologic literature review. Eur J Radiol Open. 2020;7 doi: 10.1016/j.ejro.2020.100231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bernheim A., Mei X., Huang M. Chest CT findings in coronavirus disease-19 (COVID-19): relationship to duration of infection. Radiology. 2020;295(3) doi: 10.1148/radiol.2020200463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hu Q., Guan H., Sun Z. Early CT features and temporal lung changes in COVID-19 pneumonia in Wuhan, China. Eur J Radiol. 2020;128 doi: 10.1016/j.ejrad.2020.109017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tahamtan A., Ardebili A. Real-time RT-PCR in COVID-19 detection: issues affecting the results. Expert Rev Mol Diagn. 2020;20(5):453–454. doi: 10.1080/14737159.2020.1757437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.He J.L., Luo L., Luo Z.D. Diagnostic performance between CT and initial real-time RT-PCR for clinically suspected 2019 coronavirus disease (COVID-19) patients outside Wuhan, China. Respir Med. 2020;168 doi: 10.1016/j.rmed.2020.105980. [DOI] [PMC free article] [PubMed] [Google Scholar]