Abstract
Background:
Despite the frequent occurrence of interhospital transfers in emergency general surgery (EGS), rates of transfer of complications are undescribed. Improved understanding of hospital transfer patterns has a multitude of implications, including quality measurement. The objective of this study was to describe individual hospital transfer rates of mortal encounters.
Materials and methods:
A retrospective review was undertaken from 2013 to 2015 of the Maryland Health Services Cost Review Commission database. Two groups of EGS encounters were identified: encounters with death following transfer and encounters with death without transfer. The percentage of mortal encounters transferred was defined as the percentage of EGS hospital encounters with mortality initially presenting to a hospital transferred to another hospital before death at the receiving hospital.
Results:
Overall, 370,242 total EGS encounters were included, with 17,003 (4.6%) of the total EGS encounters with mortality. Encounters with death without transfer encompassed 15,604 (91.8%) of mortal EGS encounters and encounters with death following transfer 1399 (8.2%). EGS disease categories of esophageal varices or perforation, necrotizing fasciitis, enterocutaneous fistula, and pancreatitis had over 10% of these total mortal encounters with death following transfer. For individual hospitals, percentage of mortal encounters transferred ranged from 0.8% to 35.2%. The percentage of mortal encounters transferred was inversely correlated with annual EGS hospital volume for all state hospitals (P < 0.001, r = −0.57).
Conclusions:
Broad variability in individual hospital practices exists for mortality transferred to other institutions. Application of this knowledge of percentage of mortal encounters transferred includes consideration in hospital quality metrics.
Keywords: Emergency general surgery, Interhospital transfer
Introduction
Emergency general surgery (EGS) has only recently been defined as a subspecialty in acute care surgery.1 EGS patients utilize a substantial portion of overall hospital resources, with 26% of hospital patient encounters carrying an EGS diagnosis.2,3 Over 10% of EGS patients require intensive care unit admission and costs of caring for EGS pat are greater than for trauma, sepsis, myocardial infarction, and respiratory failure.2,4
Interhospital transfers in EGS are common, with 7% of EGS patients admitted to National Surgical Quality Improvement Project (NSQIP) hospitals having undergone interhospital transfer. EGS patients undergoing interhospital transfer unsurprisingly have higher medical comorbidities, in-hospital complications, length of stay (LOS), reoperations, and mortality rates.5
After patients undergo interhospital transfer, complications are attributed to the receiving hospital rather than the sending hospital. Despite frequent interhospital transfers in EGS, individual hospital rates of transferring complications to other institutions are unknown. Patients should always be transferred if higher-level resources are needed. However, transferring complications between individual institutions has the potential to skew quality metrics and may reflect funneling of complex, high-risk patients to higher resource centers.
The primary aim of this study was to describe individual hospital percentages of mortal encounters transferred to other institutions. Secondary aims included describing patterns by EGS disease, hospital volume, and severity of illness. We hypothesized that individual hospital percentages of mortal encounters transferred would be constant.
Materials and methods
We obtained approval from the University of Maryland Institutional Review Board (IRB). EGS encounters were identified using American Association for the Surgery of Trauma (AAST) International Classification of Diseases, ninth Edition (ICD-9) EGS codes.1 ICD-9 codes were used to create disease categories for common EGS diseases (Supplement 1).
Health Services Cost Review Commission database
The Maryland State Health Services Cost Review Commission (HSCRC) is an ideal database to investigate interhospital transfers. The Maryland health care system is unique as it is the only state with state-determined reimbursements.6 The HSCRC database comprises all Maryland hospital encounters,7 allowing description of statewide trends. This contrasts with other large administrative databases, such as the National Inpatient Sample, the NSQIP data set, or Medicare claims data. These other databases represent a sample of encounters, preventing comparison of transfer rates between individual hospitals.5,8,9
The HSCRC database has multiple markers of illness severity. The severity of illness (SOI) score uses All Payer Related (APR) Diagnosis-Related Groups (DRG), a Center for Medicaid and Medicare Services measure to determine payment, which includes disease severity.10 SOI is stratified into minor, moderate, major, and extreme. The risk of mortality (ROM) is based on APR-DRG codes but also incorporates other patient diagnoses and surgical procedures,10 and is stratified same as SOI from minor to extreme.
Encounter selection
Using HSCRC data from 2013 to 2015, we selected encounters with at least one EGS ICD-9 diagnosis code. Encounters were excluded if the encounter was missing key data points, represented intrahospital transfer, was an encounter before interhospital transfer, or occurred in the last quarter of 2015 when the change to ICD-10 had occurred. Encounters were excluded if patient age was less than 20 y. Age 20 y and less was chosen because only age ranges were available. Encounters were excluded if they did not result in mortality. Using admission and discharge locations, remaining encounters were divided into two groups of patients initially presenting to an institution: encounters with death following transfer or encounters with death without transfer. Encounters transferred from out-of-state are included in the database.
Encounter linkage
Encounters with death following transfer represented the first hospital visit before interhospital transfer. Encounters with death following transfer were identified from the second (receiving) hospital encounter and linked to the first (sending) hospital using an HSCRC database variable identifying the origin hospital. This allowed mortality occurring at the second hospital to be attributed to the first hospital where the patient had initially presented. Encounters with death without transfer represented encounters where medical care was provided in total at a single hospital without interhospital transfer.
Variable definitions
The percentage of mortal encounters transferred was defined as the percentage of encounters with death following transfer out of all encounters with mortality initially presenting to a hospital. For example, at an individual institution, if 30 encounters with mortality were transferred to another hospital and 70 encounters with mortality were not transferred to another hospital out of these 100 total encounters, the percentage of mortal encounters transferred would be 30%. Annual EGS hospital volume was measured, with high-volume hospitals considered the 15 top hospitals for annual EGS hospital volume, and low-volume hospitals considered the bottom 15 hospitals for annual EGS hospital volume. Mortality was defined as occurring during the hospital encounter and represents all-cause mortality (not mortality due to EGS disease states specifically). The HSCRC database does not specify cause of mortality.
Statistical analysis
Statistical analysis was performed using SAS software, version 9.4 of the SAS system for Windows 7 operating system. (Copyright 2014, SAS Institute Inc, SAS and all other SAS Institute Inc product or service names are registered trademarks or trademarks of SAS Institute Inc, Cary, NC). Univariate analysis described frequencies, ranges, and median values. Chi-squared, Fisher’s exact, and Wilcoxon rank-sum testing compared encounters with death following transfer and encounters with death without transfer. Pearson’s correlation analysis was performed between annual EGS hospital volume and percentage of mortal encounters transferred. Owing to the large sample size, statistical significance was set at P < 0.001.
Results
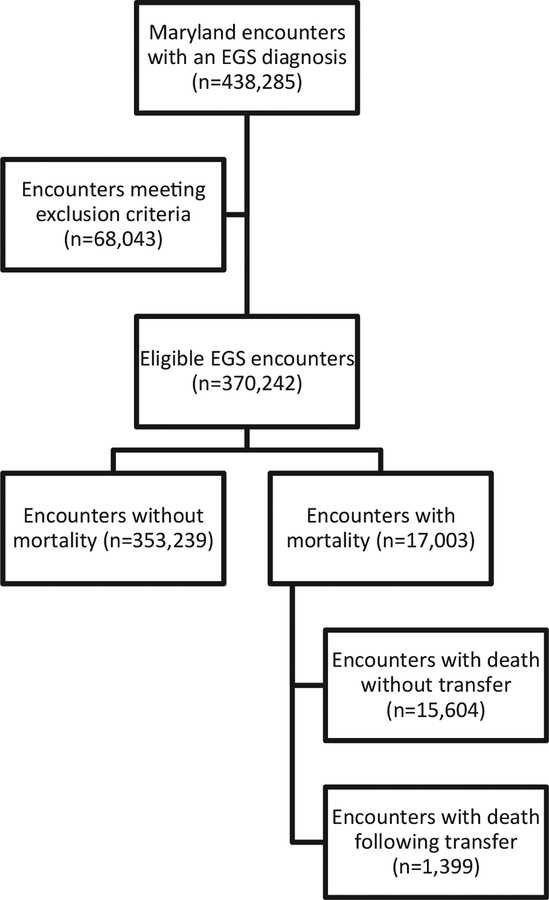
A total of 370,242 total EGS encounters occurred at 45 hospitals in Maryland. Of these total EGS encounters, 17,003/370,242 (4.6%) had a mortality and 353,239/370,242 (95.4%) did not have a mortality. Of the 17,003 EGS encounters with a mortality, 15,604/17,003 (91.8%) were encounters with death without transfer and 1399/17,003 (8.2%) were encounters with death following transfer (Fig. 1). Transfers were primarily to level 1 trauma centers (Fig. 2). There were no transfers from out-of-state with mortality.
Fig. 1 –
Flow diagram for group creation.
Fig. 2 –
Distribution of encounters with death following transfer stratified by trauma center status.
Demographic variables had significant differences for encounters with death following transfer and encounters with death without transfer. Encounters with death following transfer more often had extreme ROM and less often had major, moderate, or minor ROM compared with NT encounters (P < 0.001). Similarly, encounters with death following transfer more often had extreme SOI and less often had major or moderate SOI than encounters with death without transfer (P < 0.001). Encounters with death following transfer had a significantly longer LOS (9 d versus 5 d, P < 0.001) and intensive care unit LOS (7 d versus 4d, P < 0.001) compared to encounters with death without transfer. Median hospital charges were also significantly higher in encounters with death following transfer compared to encounters with death without transfer ($52,176.66 versus $19,968.30, P < 0.001) (Table).
Table –
Demographic variables and outcomes stratified by transfer status.
| Total EGS encounters with mortality (n = 17,003) | Encounters with death without transfer (n = 15,604) | Encounters with death following transfer (n = 1399) | P-value | |
|---|---|---|---|---|
| Age, no. (%) | ||||
| 20–44 y | 883/17,003 (5.2%) | 748/15,604 (4.8%) | 135/1399 (9.7%) | <0.001 |
| 45–64 y | 4527/17,003 (26.6%) | 3979/15,604 (25.5%) | 548/1399 (39.2%) | |
| 65 y and older | 11,593/17,003 (68.2%) | 10,877/15,604 (69.7%) | 716/1399 (51.2%) | |
| Sex, no. (%) | ||||
| Male | 8718/17,003 (51.3%) | 7946/15,604 (50.9%) | 772/1399 (55.2%) | 0.002 |
| Female | 8285/17,003 (48.7%) | 7658/15,604 (49.1%) | 627/1399 (44.8%) | |
| Race, no. (%) | ||||
| Caucasian | 9.694/17,003 (57.0%) | 8877/15,604 (56.9%) | 817/1399 (58.4%) | 0.19 |
| African American | 5043/17,003 (29.7%) | 4622/15,604 (29.6%) | 421/1399 (30.1%) | |
| Hispanic | 299/17,003 (1.8%) | 282/15,604 (1.8%) | 17/1399 (1.2%) | |
| Asian/Pacific Islander | 328/17,003 (1.9%) | 308/15,604 (2.0%) | 20/1399 (1.4%) | |
| Other/unknown | 1639/17,003 (9.6%) | 1515/15,604 (9.7%) | 124/1399 (8.9%) | |
| Patient insurance, no. (%) | ||||
| Commercial | 2574/17,003 (15.1%) | 2273/15,604 (14.6%) | 201/1399 (21.5%) | <0.001 |
| Public (Medicare/Medicaid) | 13,579/17,003 (79.9%) | 12,528/15,604 (80.3%) | 1051/1399 (75.1%) | |
| Self-pay/charity | 368/17,003 (2.2%) | 348/15,604 (2.2%) | 20/1399 (1.4%) | |
| Other/unknown | 482/17,003 (2.8%) | 455/15,604 (2.9%) | 27/1399 (1.9%) | |
| SOI, no. (%) | ||||
| Minor | 83/17,003 (0.5%) | 75/15,604 (0.5%) | 8/1399 (0.6%) | <0.001 |
| Moderate | 646/17,003 (3.8%) | 611/15,604 (3.9%) | 35/1399 (2.5%) | |
| Major | 5469/17,003 (32.2%) | 5147/15,604 (33.0%) | 322/1399 (23.0%) | |
| Extreme | 10,805/17,003 (63.6%) | 9771/15,604 (62.2%) | 1034/1399 (73.9%) | |
| ROM, no. (%) | ||||
| Minor | 154/17,003 (0.9%) | 145/15,604 (0.9%) | 9/1399 (0.6%) | <0.001 |
| Moderate | 1194/17,003 (7.0%) | 1103/15,604 (7.1%) | 91/1399 (6.5%) | |
| Major | 5089/17,003 (29.9%) | 4756/15,604 (30.5%) | 342/1399 (24.5%) | |
| Extreme | 10,557/17,003 (62.1%) | 9600/15,604 (61.5%) | 957/1399 (68.4%) | |
| ICU admission, no. (%) | ||||
| Yes | 6538/17,003 (38.5%) | 5705/15,604 (36.6%) | 833/1399 (59.5%) | <0.001 |
| No | 10,465/17,003 (61.6%) | 9899/15,604 (63.4%) | 566/1399 (40.5%) | |
| ICU LOS, median (IQR) | 4 d (1–10) | 4 d (1–9) | 7 d (3–15) | <0.001 |
| LOS, median (IQR) | 5 d (2–12) | 5 d (2–11) | 9 d (3–19) | <0.001 |
| Total hospital charges, median (IQR) | $21,494.05 (9559.61–48,324.45) | $19,968.30 (9078.30–44,373.33) | $52,176.66 (23,973.55–108,918.60) | <0.001 |
| Hospital of origin, no. (%) | ||||
| Trauma center | 5163/17,003 (30.4%) | 4893/15,604 (31.6%) | 270/1399 (19.3%) | <0.001 |
| Nontrauma center | 11,840/17,003 (69.6%) | 10,711/15,604 (68.6%) | 1129/1399 (80.7%) | |
ICU = intensive care unit.
The percentage of encounters with death following transfer out of the total number of mortal encounters for common EGS diseases was next examined (Fig. 3). Encounters with diagnosis codes for esophageal varices, necrotizing fasciitis, enterocutaneous fistula, pancreatitis, and esophageal perforation had greater than 10% of total mortal encounters for those individual EGS diseases with death following transfer.
Fig. 3 –
Percentages of encounters with mortality following transfer and encounters with mortality without transfer stratified by common emergency general surgery (EGS) diseases.
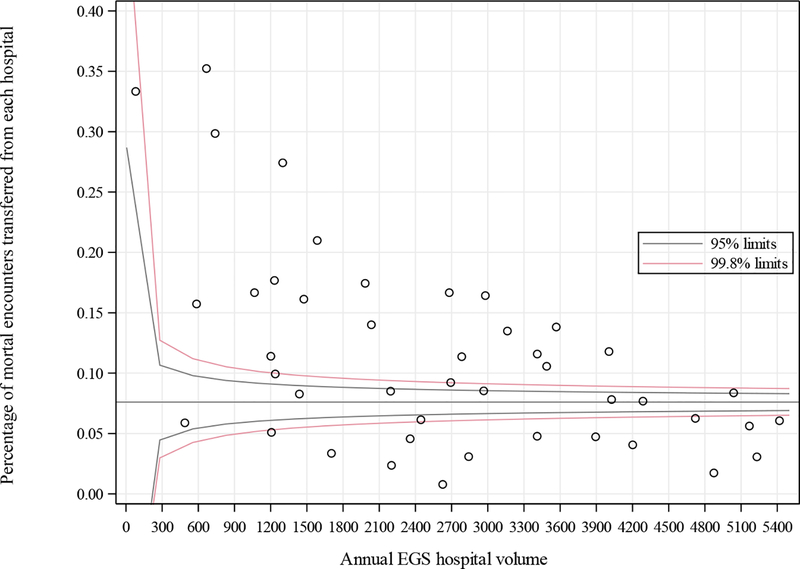
The percentage of mortal encounters transferred was calculated for individual hospitals. The percentage of mortal encounters transferred ranged from 0.8% to 35.2% of mortality initially presenting to each individual hospital (Fig. 4). For high-volume hospitals, the percentage of mortal encounters transferred ranged from 2.1% to 13.9%, and for low-volume hospitals, the percentage of mortal encounters transferred ranged from 3.4% to 35.2%. The percentage of mortal encounters transferred was inversely correlated with sending annual EGS hospital volume for all state hospitals (P < 0.001, r = −0.57) and for high-volume hospitals (P = 0.002, r = −0.73), but not for low-volume hospitals (P = 0.07, r = −0.47).
Fig. 4 –
Funnel plot comparing the percentage of mortal encounters transferred from each hospital with annual EGS hospital volume. (Color version of figure is available online.)
Discussion
Approximately 1 out of 10 EGS encounters in Maryland with mortality undergo interhospital transfer, making this an infrequent but nonnegligible occurrence. When patients undergo interhospital transfer, complications undergo interhospital transfer with them. These complications are attributed to the receiving hospital if they occur after transfer. This study is the first description of rates mortality transferred away from hospitals.
Use of interhospital transfers is becoming universal. Standardization in transfer practices has made interhospital transfer safer even for the critically ill.11 However, the percentages of mortal encounters transferred for individual hospitals were not constant. Some hospitals reported almost no transfers of mortal encounters away from their institution. Other hospitals transferred away 1 out of every 3 EGS patients who died after initially presenting to their institution. The range for percentages of mortal encounters transferred is broad.
Despite the variability in the percentage of mortal encounters transferred, patterns of percentages of mortal encounters transferred seemed to be appropriate for the Maryland state medical system. Mortal encounters were more likely to be transferred from low-volume hospitals and less likely to be transferred from high-volume hospitals. This pattern persisted even for high-volume hospitals only, which likely reflects continued specialization of resources even among the busiest centers. Interestingly, the pattern that mortal encounters were more likely to be transferred from lower volume centers did not persist within the lowest volume centers. This has multiple potential explanations, including variations in providers experience and comfort at lower volume centers, variations in hospital cultures, differing patient populations, and variability of resources even within lower volume centers.
However, the exact reasons for interhospital transfers in this data set are unknown. Factors which we could examine included age, race, payer source, and severity of illness. Determining which of these factors are clinically significant given the size of the data set is difficult even if many of these factors are statistically significant.
Overall, it did not seem that payer status influenced the decision to transfer, without a noticeable tendency to retain patients with commercial insurance and transfer patients with self-pay or charity care. Certainly, it would be concerning if patients less likely to provide full payment were more likely to be transferred. Payer status still may not tell the whole story of the financial implications of transfer, as patients with a longer real or potential hospital stay could be resource intensive regardless of payer status.
Although the association between SOI and ROM with transfer status is statistically significant, SOI and ROM do not appear to influence interhospital transfer. Patients with the highest SOI and ROM more commonly underwent interhospital transfer, but not all patients with death following transfer had the highest SOI or ROM level. This suggests that either patients are transferred for reasons other than critical illness (i.e., specialized surgical care, interventional radiology, etc.) or that the SOI and ROM quality measurements do not fully capture the complexity and illness of these patients.
Race was not associated with interhospital transfer status, which is reassuring. Race has been associated with transfer status in critically ill patients, with African American and Hispanic patients less likely to undergo interhospital transfer.12 Similarly elderly age did not seem to be a driver of transfer status, with those ages 65 y and greater less likely to undergo transfer.
EGS disease, however, likely influences decision for interhospital transfer. Many EGS diseases had overall similar rates of encounters with death following transfer (such as chol-edocholithiasis, intestinal obstruction, gastric ulcer, ventral hernia, or appendicitis). Conversely, those EGS diseases we see in clinical practice which often require the resources of a referral hospital (such as necrotizing fasciitis, esophageal varices and perforation, enterocutaneous fistula, and pancreatitis) more commonly had death following transfer.
However, physiology, while not directly measured in the HSCRC database, likely plays a role in the transfer of mortal encounters. One would expect that most cases of appendicitis, hernia, intestinal obstruction, and so on could be managed in most any hospital with general surgery coverage. The similar rates of encounters with death following transfer for these conditions suggest that patient physiology may be driving the decision for interhospital transfer rather than EGS disease for these encounters.
Multiple variables that are not represented in the HSCRC database likely influence the decision for interhospital transfer. Body mass index may play a role in transfer, and our institution does receive transfers of patients felt too obese for care at other institutions. Similarly, patient comorbidities undoubtedly drive the decision for interhospital transfer, and our institution also commonly receives transfers of patients felt too medically complex for care at other institutions. However, differentiating congestive heart failure able to be managed at a referring institution and congestive heart failure requiring a tertiary facility for management is difficult in large databases.
Even with appropriate system-level interhospital transfer patterns in EGS, there are some further important applications to the variability seen in the percentage of mortal encounters transferred. Although interhospital transfer is undoubtedly beneficial for EGS patients by providing more appropriate resources for patient care at receiving hospitals,13 the reality for physicians and hospitals is that outcomes are tracked. The variable rates of percentages of mortal encounters transferred seen in this manuscript could influence calculation of quality metrics or pay-for-performance reimbursement.14,15 For example, a high percentage of mortal encounters transferred may falsely improve a hospital’s quality metrics when high-risk patients are transferred away, while low percentages of mortal encounters transferred may harm a hospital’s quality metrics in comparison to other, high-transfer institutions. A concern is then there is incentive for tertiary centers to deny interhospital transfers if patients will likely do poorly or for centers to transfer away patients who will likely do poorly. Assuring fair representation for all institutions is then paramount to assure optimal patient care.16,17 The HSCRC has identified this issue and created cost adjustments for sending institutions,18 but much work is still needed.
This manuscript provides an initial system-wide description of percentages of mortal encounters transferred in EGS, which was previously not described. It raises questions about whether we are appropriately applying quality metrics. This study is not meant to delineate which patients should undergo interhospital transfer or appropriate ranges for percentages of mortal encounters transferred, but rather raise the potential issue of transfers of reportable mortality in our modern health care system.
An appropriate rate of mortality transferred is not likely a static number. Much as hospital resources play a role in the decision for interhospital transfer, hospital resources also would influence what an appropriate rate of transfer would be. Lower resource institutions should transfer more mortality, and higher resource institutions should transfer less if any. Patients in whom mortality might be avoided through care at a higher resource institution should undergo interhospital transfer. Potential for mortality within a patient encounter will not be the single driver of interhospital transfers, and hospitals will not only transfer patients at imminent risk of death. Patients requiring the specialized services of a tertiary center will still benefit from undergoing interhospital transfer, even if they are not high risk for mortality.
Limitations include that given the admission and discharge locations in the HSCRC database used to define the encounters with death following transfer and encounters with death without transfer, we could not account for greater than one interhospital transfer, which is seen.8 Cause of death is not delineated in the data set; all-cause mortality was used in this study but EGS-specific mortality would be the ideal outcome for evaluation. Similarly, available hospital resources were inferred from annual EGS hospital volume and not directly measured. Surgeon experience was also not measured and likely plays a role in decision for interhospital transfer.
Conclusion
The burden of transfer of mortal encounters in EGS was previously undescribed. Broad variability exists in the percentage of mortal encounters transferred from individual hospitals, although the overall frequency of encounters with death following transfer amid the total EGS encounters for the state is low. Encounters with death following transfer appear to occur without reference to race, elderly age, payer status, or severity of illness and occur appropriately from low-volume hospitals to high-volume hospitals. However, the data do suggest that physiology, while not directly measured in this administrative database, may play a key role in transfer of mortal encounters in addition to EGS disease complexity. While tertiary facilities have increased resources to manage complex EGS diseases and critically ill patients, application of the variability seen in percentages of mortal encounters transferred may need consideration in quality metric measurement.
Supplementary Material
Acknowledgment
The authors would like to thank Gordon Smith for his assistance with this project.
There was no funding specifically used for this project.
Disclosure
M.L. received grant support from NHTSA and Maryland Department of Health and Mental Hygiene. A.V.H. was training under the T32 training grant T32 AG00262. J.A. received AHRQ grant K01HS024560. B.B. received grant support from National Institutes of Health, Department of Defense. J.D. receives consultancy from Acuity-KCI and Acute Innovations. The other authors declared no conflicts of interest.
Footnotes
Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jss.2019.05.040.
The meeting was presented at the 89th Annual Pacific Coast Surgical Association, Napa, California, February 17, 2018.
REFERENCES
- 1.Shafi S, Aboutanos MB, Agarwal S Jr, et al. Emergency general surgery: definition and estimated burden of disease. J Trauma Acute Care Surg. 2013;74:1092–1097. [DOI] [PubMed] [Google Scholar]
- 2.Narayan M, Tesoriero R, Bruns BR, Klyushnenkova EN, Chen H, Diaz JJ. Acute care surgery: defining mortality in emergency general surgery in the state of Maryland. J Am Coll Surg. 2015;220:762–770. [DOI] [PubMed] [Google Scholar]
- 3.Bruns BR, Tesoriero R, Narayan M, et al. Emergency general surgery: defining burden of disease in the state of Maryland. Am Surg. 2015;81:829–834. [PubMed] [Google Scholar]
- 4.Ogola GO, Gale SC, Haider A, Shafi S. The financial burden of emergency general surgery: National estimates 2010 to 2060. J Trauma Acute Care Surg. 2015;79:444–448. [DOI] [PubMed] [Google Scholar]
- 5.Lucas DJ, Ejaz A, Haut ER, Spolverato G, Haider AH, Pawlik TM. Interhospital transfer and adverse outcomes after general surgery: implications for pay for performance. J Am Coll Surg. 2014;218:393–400. [DOI] [PubMed] [Google Scholar]
- 6.Kastor JA, Adashi EY. Maryland’s hospital cost review commission at 40: a model for the country. JAMA. 2011;306:1137–1138. [DOI] [PubMed] [Google Scholar]
- 7.HSCRC overview. Available at: http://www.hscrc.state.md.us/aboutHSCRC.cfm. Accessed March 15, 2016.
- 8.Iwashyna TJ, Christie JD, Moody J, Kahn JM, Asch DA. The structure of critical care transfer networks. Med Care. 2009;47:787–793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kindermann DR, Mutter RL, Houchens RL, Barrett ML, Pines JM. Emergency department transfers and transfer relationships in United States hospitals. Acad Emerg Med. 2015;22:157–165. [DOI] [PubMed] [Google Scholar]
- 10.Averill R, Goldfield N, Hughes J, et al. All patient refined diagnosis related groups. 2003. Available at: https://www.hcup-us.ahrq.gov/db/nation/nis/APR-DRGsV20MethodologyOverviewandBibliography.pdf. Accessed March 15, 2016.
- 11.Warren J, Fromm RE Jr, Orr RA, Rotello LC, Horst HM, American College of Critical Care Medicine. Guidelines for the inter- and intrahospital transport of critically ill patients. Crit Care Med. 2004;32:256–262. [DOI] [PubMed] [Google Scholar]
- 12.Tyler PD, Stone DJ, Geisler BP, McLennan S, Celi LA, Rush B. Racial and geographic disparities in interhospital ICU transfers. Crit Care Med. 2018;46:e76–e80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Santry HP, Janjua S, Chang Y, Petrovick L, Velmahos GC. Interhospital transfers of acute care surgery patients: should care for nontraumatic surgical emergencies be regionalized? World J Surg. 2011;35:2660–2667. [DOI] [PubMed] [Google Scholar]
- 14.Rosenberg AL, Hofer TP, Strachan C, Watts CM, Hayward RA. Accepting critically ill transfer patients: adverse effect on a referral center’s outcome and benchmark measures. Ann Intern Med. 2003;138:882–890. [DOI] [PubMed] [Google Scholar]
- 15.Combes A, Luyt CE, Trouillet JL, Chastre J, Gibert C. Adverse effect on a referral intensive care unit’s performance of accepting patients transferred from another intensive care unit. Crit Care Med. 2005;33:705–710. [DOI] [PubMed] [Google Scholar]
- 16.Ban KA, Cohen ME, Ko CY, et al. Evaluation of the ProPublica surgeon scorecard “adjusted complication rate” measure specifications. Ann Surg. 2016;264: 566–574. [DOI] [PubMed] [Google Scholar]
- 17.Bilimoria KY, Barnard C. The new CMS hospital quality star ratings: the stars are not aligned. JAMA. 2016;316: 1761–1762. [DOI] [PubMed] [Google Scholar]
- 18.Transfer cases payment adjustment under global revenue and total patient revenue models. 2015. Available at: http://www.hscrc.state.md.us/Documents/global-budgets/adj/Transfer-Cases-Description-20150902.pdf. Accessed March 30, 2018.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.