Abstract
Objectives: Existing evidence supports the use of certain Chinese medicine (CM) interventions for symptom management among palliative cancer patients. However, evidence-based service recommendations tailored to the local context are needed for CM planning and implementation. In response, we aimed to establish consensus on CM clinical service recommendations for cancer palliative care among Hong Kong experts. Methods: Seven CM interventions showing statistically significant favorable results in existing systematic reviews (SRs) and overviews of SRs were subjected to a GRADE-ADOLOPMENT–based 2-round Delphi survey. Twelve Hong Kong experts in cancer palliative care, including conventionally trained physicians, CM practitioners, and nurses (n = 4 from each category), were invited to participate. Use of the Evidence to Decision framework within the GRADE-ADOLOPMENT approach enabled experts to consider aspects of problem priority, benefits, harms, equity, acceptability, and feasibility when making CM recommendations in cancer palliative care. Results: Three evidence-based CM interventions reached positive consensus as service recommendations, namely: (1) acupuncture for reducing fatigue among palliative cancer patients; (2) acupressure for reducing fatigue among palliative cancer patients; and (3) moxibustion for reducing nausea and vomiting among patients receiving chemotherapy. Median rating of recommendation ranged from 2.5 to 3.0 (interquartile range = 0.00-1.00) on a 4-point Likert-type scale, and the percentage agreement ranged from 83.4% to 91.7%. Conclusions: The GRADE-ADOLOPMENT approach facilitates a consensus-based process of reaching 3 evidence-based CM recommendations for cancer palliative care. Future studies may develop tailored strategies to implement these recommendations in the Hong Kong health system.
Keywords: palliative care, traditional Chinese medicine, Chinese herbal drugs, acupuncture, GRADE approach, neoplasms, Delphi technique
Introduction
Echoing recommendations from the World Health Organization (WHO) on integrating traditional and complementary medicine into national health systems in an evidence-based manner,1 there is a need to develop evidence-based clinical service recommendations for traditional and complementary medicine services. Existing systematic reviews (SRs) and overviews of SRs identify certain Chinese medicine (CM) interventions, inclusive of Chinese herbal medicine (CHM) and acupuncture and related therapies, as effective in managing cancer-related symptoms, such as fatigue, nausea, and vomiting, among palliative cancer patients.2-6 The palliative care version of the US National Comprehensive Cancer Network (NCCN) clinical practice guidelines in oncology7,8 has already recommended acupuncture for reducing cancer pain and cancer-related fatigue.
Since multiple stakeholders may have different perspectives and concerns regarding the implementation of these evidence-based CM service recommendations, it is important to bridge the gap between clinical evidence, health care experts’ experience, as well as patients’ values in decision making.9,10 The GRADE-ADOLOPMENT approach is a methodology that combines the advantages of adoption, adaptation, and de novo development of recommendations among an expert panel based on Grading of Recommendations Assessment, Development and Evaluation (GRADE), as well as the associated Evidence to Decision (EtD) framework.11
As a core component of the approach, the EtD framework is applied for the following purposes:
Providing experts with a concise summary of the best available evidence about each criterion, namely, problem priority, benefits, harms, equity, acceptability, and feasibility
Allowing experts to consider these criteria in a comprehensive manner on whether an intervention should be recommended
Structuring and documenting experts’ justifications on how each criterion described above would influence the direction, strength, and implementability of the recommendations11-13
The GRADE-ADOLOPMENT approach successfully guided the development of recommendations and guidelines in Canada14 and Australia,15 and Saudi Arabia.16 This approach has high adaptability for facilitating the formulation of health service recommendations in different health systems with distinct governance, financing, and service delivery models.
Cancer is a major cause of disease burden in Hong Kong. According to the Hong Kong Hospital Authority, there were 31 468 new cancer cases and 14 209 cancer deaths in 2016.17 Among local cancer patients, 68.9% received palliative care in publicly funded health care setting in 2015.18 A 2009 survey reported that over 50% of Hong Kong cancer patients receiving conventional treatments also concurrently utilized CM services with the expectation of reducing side effects of conventional treatments, limiting tumor progression, and improving their quality of life.19 Nearly 90% of these patients also supported the government to integrate CM and biomedicine (BM) in cancer treatment within the Hong Kong health system.19
Under the influence of colonial history, CM is commonly used as a complement to BM, with the later occupying a dominant position in the health system.20 According to previous Hong Kong surveys, physicians and nurses held mixed attitudes toward the value of CM.21,22 Interprofessional collaboration is inevitable if CM services are to be integrated into the Hong Kong health system.23 Therefore, acceptance and endorsement from physicians and nurses are considered essential in the successful implementation of CM service recommendations in Hong Kong.24 In line with international experiences,25 physicians and nurses should be regarded as key stakeholders in the formulation of CM service recommendations.
Numerous factors are hindering the transition from parallel to integrative practice model.26 A previous SR showed that an unverified perception on the lack of high-quality evidence supporting effectiveness and safety of CM was a common rhetorical tool employed among physicians to oppose collaboration with CM practitioners (CMPs).25 One of the suggested solutions to change physicians’ opposition toward collaboration with CMPs was to implement existing CM modalities supported with sufficient evidence, and to design interprofessional collaboration plans accordingly.25
To translate evidence-based CM modalities into integrative practice, the current study aimed to establish consensus on evidence-based CM clinical service recommendations for cancer palliative care among Hong Kong experts using the EtD framework approach.
Methods
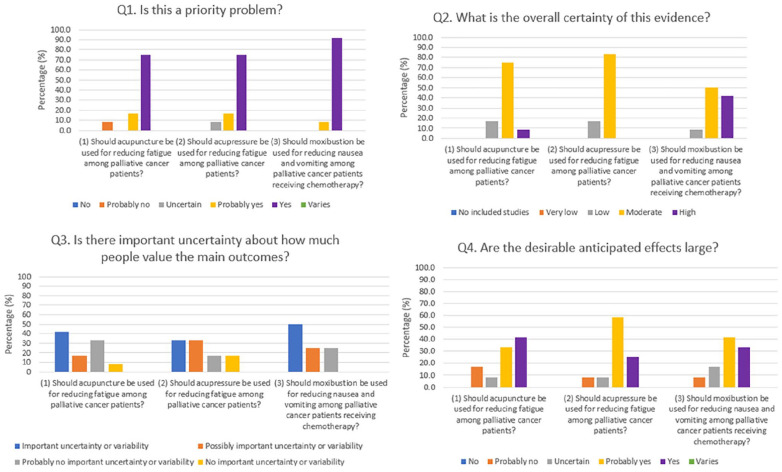
This Delphi survey is reported in accordance to the standard for Conducting and Reporting of Delphi Studies (CREDES).27 Ethical approval was obtained from the Survey and Behavioural Research Ethics Committee, The Chinese University of Hong Kong (Reference No. 023-17). The workflow of the study and details are presented in Figure 1.
Figure 1.
Workflow of developing Chinese medicine clinical service recommendations for cancer palliative care.
Abbreviations: Acupuncture, acupuncture and related therapies; CHM, Chinese herbal medicine; CM, Chinese medicine; CMPs; Chinese medicine practitioners; EtD, Evidence to Decision; Overviews, overviews of systematic reviews; SRs, systematic reviews.
*Evidence profiles includes number of studies; number of participants; effects of binary and continuous outcomes along with their corresponding 95% confidence intervals and P values; and quality of evidence.
^EtD frameworks consider the following criteria: problem priority, benefits, harms, equity, acceptability, and feasibility.
Part 1: Preparation of Evidence Profiles and EtD Frameworks of CM Interventions for Cancer Palliative Care
Three overviews of SRs and 2 SRs2-6 on CM interventions for cancer palliative care published in late 2015 and early 2016 were selected for this part. They were selected as they had critically appraised and summarized the most up-to-date clinical evidence on CHM, as well as acupuncture and related therapies, for cancer palliative care at the time of our study. In these rigorous syntheses,2-6 methodological quality of 74 included SRs was evaluated using the AMSTAR instrument,28 while risk of bias of 88 included randomized controlled trials (RCTs) were assessed with the Cochrane risk of bias tool.29 Strengths and limitations on the synthesized evidence were also highlighted by the original authors.2-6
By identifying statistically significant favorable results from these synthesis,2-6 our study focused on a total of 7 CM interventions. Results of these interventions were displayed in 7 evidence profiles, which presented in a consistent format: number of studies; number of participants; effects of binary and continuous outcomes including their corresponding 95% confidence intervals (CIs) and P values; and quality of evidence.30,31 Quality of evidence was assessed by the Clinical and Health Intervention Meta-analysis Evidence RAting System (CHIMERAS; Appendix 1, Supplementary material, available online).32 The rating was conducted by the investigators, and the Delphi experts were not required to rate evidence quality. Evidence profiles of the 7 CM interventions are shown in Appendix 2 (Supplementary material, available online).
EtD frameworks of the 7 evidence-based CM interventions were then prepared. These frameworks facilitated Delphi experts’ decision-making process, moving from results presented in evidence profiles to recommendations, through explicit consideration of the following criteria: deemed priority of the problem, benefits, harms, equity, acceptability, and feasibility of CM interventions.33 In this structured approach, experts were invited to consider the criteria mentioned above thoroughly,10,12 and subsequently, each expert was invited to provide a rating on whether a specific CM intervention should be recommended in the Hong Kong health system. Rating of recommendations was assessed on a 4-point Likert-type scale, ranging from “recommend against this option” (ie, strongly disagree with the proposed CM intervention), “suggest not this option” (ie, disagree with the proposed CM intervention), “suggest this option” (ie, agree with the proposed CM intervention), to “recommend this option” (ie, strongly agree with the proposed CM intervention).11,34 Experts were also invited to provide additional qualitative comments on implementation, monitoring, evaluation, and future research possibilities.7,31 EtD frameworks of the 7 CM interventions are shown in Appendix 3 (Supplementary material, available online).
Part 2: Sampling of Experts
Purposive sampling is a technique widely used to identify individuals who are especially knowledgeable about, or experienced with, a phenomenon of interest.35 In the purposive sampling of this study, we selected a balanced number of conventionally trained physicians, CMPs, and nurses (4 experts from each of the 3 professions) with at least 1 year of professional experience in cancer palliative care service provision within the Hong Kong health system. Under such maximum variation sampling strategy, experts from different health care disciplines in cancer palliative care were identified to provide unique and diverse insight on CM service recommendations, ensuring balanced perspectives across members in the expert panel.35 Since a smaller sample size would enable higher response rate, total number of experts recruited was limited to 12.36 All participating experts were de-identified to safeguard confidentiality and independence of judgements during the process.
Thirteen potential experts were approached through the investigators’ professional networks. The experts were first contacted via email in July 2018, along with objectives, study details, and written informed consent forms. Online introduction to the Delphi survey procedures was then provided to the 12 experts who returned their signed informed consent. The introductory package included a narrated online presentation of the whole study process, an online video on interpretation of evidence profiles, and an overview of the EtD framework.
Part 3: Round 1 Delphi Survey Data Collection and Data Analysis
The Round 1 Delphi survey package, which included a questionnaire on demographic and professional information, evidence profiles, and EtD frameworks of evidence-based CM interventions prepared in Part 1, was then emailed to the participants. Each expert was invited to complete and return the questionnaire by email.
For each CM intervention, Round 1 median rating of recommendation was calculated alongside interquartile range (IQR) to demonstrate magnitude of disagreement among experts. Median and IQR are preferred as they are less influenced by outliers when compared with mean and standard deviation.36,37 Agreement on the recommendation was expressed in percentage (%). With reference to the agreement standard adopted in previous studies, the consensus cutoff level of this study was set at 75%.38 In other words, an intervention would reach positive consensus as a service recommendation if ≥75% of experts rated “suggest this option” or “recommend this option” on the 4-point Likert-type scale; while negative consensus would be attained when ≥75% rated “suggest not this option” or “recommend against this option.”38 Interventions achieving positive consensus in Round 1 were considered as service recommendations. For interventions without consensus, qualitative comments were summarized and presented for further evaluation in Round 2. Besides, assessment results on each EtD framework criterion were expressed in percentage (%), based on the proportion of experts making a specific rating.
Part 4: Round 2 Delphi Survey Data Collection and Data Analysis
In Round 2, the same panel of experts were asked to reassess CM interventions that neither reached positive nor negative consensus in Round 1. Delphi survey package for this round included the following: (1) experts’ own rating in Round 1; (2) median ratings with IQRs and percentage agreement; (3) anonymous qualitative comments; as well as (4) assessment results on each EtD framework criterion from all other experts. Data collection and analysis similar to Round 1 were then performed. A list of finalized, local experts–endorsed CM clinical service recommendations was generated at the end of Round 2, including all interventions with positive consensus across both rounds.
Results
Participants
Twelve cancer palliative care experts agreed to take part in the 2-round Delphi survey. The response rates of completing both rounds were 100.0%. The expert panel comprised physicians (n = 4), CMPs (n = 4), and nurses (n = 4), with 4 of them belonging to more than 1 profession. One third of the experts worked in public tax funded hospitals (33.3%) and one fourth (25%) in private outpatient settings at the time of the study. Majority of experts (66.7%) had professional experience in cancer palliative care for 7 years or more, while 33.3% had been conducting relevant research for over 15 years (Table 1).
Table 1.
Demographic Data of Participants in the 2-Round Delphi Survey (n = 12).
| Demographics | Values |
|---|---|
| 1. Gender, n (%) | |
| Male | 4 (33.3) |
| Female | 8 (66.7) |
| 2. Age, n (%) | |
| 31-45 | 6 (50.0) |
| 46-60 | 6 (50.0) |
| 3. Profession, n (%) | |
| One profession only | 8 (66.7) |
| Physician only | 4 (33.3) |
| CMP only | 2 (16.7) |
| Nurse only | 2 (16.7) |
| More than one profession | 4 (33.3) |
| CMP and clinical research methodologist | 2 (16.7) |
| Nurse and clinical research methodologist | 2 (16.7) |
| 4. Work setting, n (%) | |
| Academic institutions | 2 (16.7) |
| Public tax funded hospitals | 4 (33.3) |
| Private clinics | 3 (25.0) |
| University clinics | 1 (8.3) |
| Academic institutions and university clinics | 2 (16.7) |
| 5. Years of professional experience in cancer palliative care, n (%) | |
| 1 to 3 years | 1 (8.3) |
| 3 to 5 years | 2 (16.7) |
| 5 to 7 years | 1 (8.3) |
| 7 years or above | 8 (66.7) |
| 6. Years of conducting research, n (%) | |
| Less than 5 years | 2 (16.7) |
| 5 to 9 years | 1 (8.3) |
| 10 to 14 years | 1 (8.3) |
| 15 years or above | 4 (33.3) |
| Not applicable | 4 (33.3) |
Abbreviation: CMP, Chinese medicine practitioner.
Service Recommendations Developed in Round 1 Delphi Survey
Overall Rating Results
Three out of 7 evidence-based CM interventions reached positive consensus as service recommendations in Round 1. Median rating of these 3 recommendations ranged from 2.5 to 3.0 (IQR = 0.00-1.00) on a 4-point Likert-type scale, while the percentage agreement ranged from 83.4% to 91.7% (Table 2). Among the recommendations, quality of evidence assessed by CHIMERAS on (1) acupuncture for reducing fatigue among palliative cancer patients and (2) acupressure for reducing fatigue among palliative cancer patients were moderate; while the quality of evidence on (3) moxibustion for reducing nausea and vomiting among patients receiving chemotherapy was high.
Table 2.
List of Interventions and Agreement Results in the 2-Round Delphi Survey.
| Interventions | Overall quality ranking of the evidence (CHIMERAS) | Delphi round 1 | Delphi round 2 | ||||
|---|---|---|---|---|---|---|---|
| Median (IQR) | Agreement (%) | Consensus (yes/no) | Median (IQR) | Agreement (%) | Consensus (yes/no) | ||
| (1) Should acupuncture be used for reducing fatigue among palliative cancer patients? | Moderate | 3.0 (0.00) | 91.7 | Yes | N/Aa | ||
| (2) Should acupressure be used for reducing fatigue among palliative cancer patients? | Moderate | 2.5 (1.00) | 91.7 | Yes | N/Aa | ||
| (3) Should moxibustion be used for reducing nausea and vomiting among palliative cancer patients receiving chemotherapy? | High | 3.0 (1.00) | 83.3 | Yes | N/Aa | ||
| (4) Should electroacupuncture be added on top of antiemetics for reducing nausea and vomiting among palliative cancer patients? | Moderate | 3.0 (1.00) | 66.7 | No | 3.0 (1.00) | 66.7 | No |
| (5) Should hyperthermia plus Gui-dan-san-zi-san (桂丹三籽散)b be used for reducing pain among palliative cancer patients receiving radiotherapy? | Moderate | 2.0 (1.00) | 33.3 | No | 2.0 (1.00) | 33.3 | No |
| (6) Should Zi-long-jing (紫龍金)c be used for improving quality of life among palliative cancer patients receiving chemotherapy? | High | 2.5 (1.00) | 50.0 | No | 3.0 (1.00) | 58.3 | No |
| (7) Should Ganoderma lucidum (靈芝) extract be used for improving quality of life among palliative cancer patients receiving chemotherapy or radiotherapy? | High | 2.5 (1.00) | 50.0 | No | 2.5 (1.75) | 50.0 | No |
Abbreviations: CHIMERAS, Clinical and Health Intervention Meta-analysis Evidence RAting System; IQR, interquartile range; N/A, not applicable.
Not applicable since the topic has achieved positive consensus in the first round of Delphi survey.
Detailed prescriptions for Gui-dan-san-zi-san (桂丹三籽散): gui zhi桂枝 30 g, bai jie zi 白芥子 30 g, wu zhu yu吳茱萸 30 g, tu si zi菟絲子 30 g.
Detailed prescriptions for Zi-long-jing (紫龍金): 由huang qi 黃芪, dang gui 當歸, bai ying 白英, long kui 龍葵, dan shen 丹參, ban zhi lian 半枝蓮, she mei 蛇莓, yu jin 鬱金等組成, 天津中新藥業集團股份有限公司龍順榕製藥廠生產, 批號 Z20010064.
Rating Results From the Evidence to Decision Framework
Priority of the problem
Over 70% of the experts on the panel agreed that all 3 recommended CM clinical services were “a priority” from their perspectives (Figure 2).
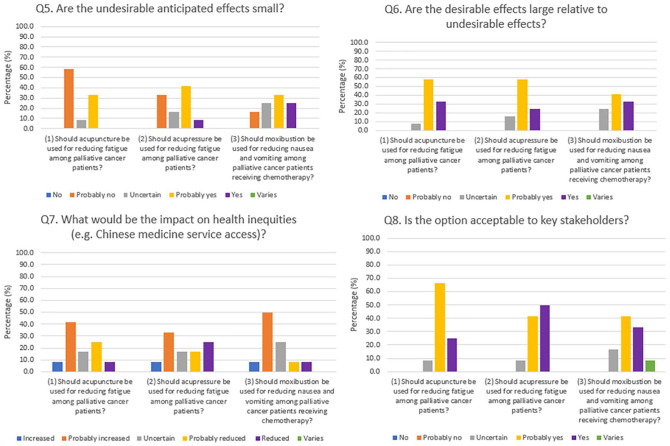
Figure 2.
Evidence to Decision (EtD) framework assessment results on Chinese medicine clinical service recommendations: Q1 to Q4.
Keys. The percentage (%) of the criteria of each EtD framework was expressed based on the proportion of experts making the judgements.
Benefits and harms of the interventions
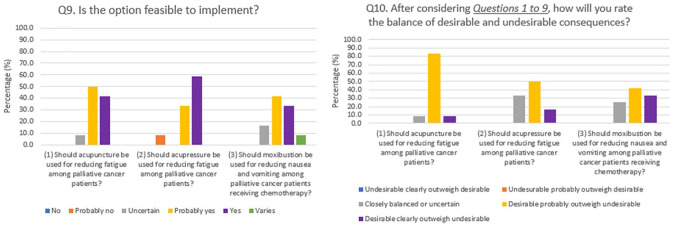
More than 80% agreed that overall certainty of evidence among the 3 recommendations were moderate or high (Figure 2). However, over half of experts believed that there was “important” or “possibly important” uncertainty about how much cancer patients might value the main outcomes (Figure 2). More than 75% regarded desirable anticipated effects of the 3 recommendations were “probably large” or “large.” Over 50% indicated that undesirable anticipated effects of the 3 recommendations, except on acupuncture for reducing fatigue, were “probably small” or “small” (Figures 2 and 3). More than 75% agreed that desirable effects were large or probably large relative to undesirable effects (Figure 3).
Figure 3.
Evidence to Decision (EtD) framework assessment results on Chinese medicine clinical service recommendations: Q5 to Q8.
Keys. The percentage (%) of the criteria of each EtD framework was expressed based on the proportion of experts making the judgements.
Some experts provided qualitative comments on benefits and harms of these 3 recommendations. For (1) acupuncture, one physician believed that it brought less adverse effects than CHM, as the latter might induce herb-drug interactions. However, the physician also suggested that patients receiving chemotherapy were more vulnerable to infection; and therefore, they should avoid receiving acupuncture treatment. For (2) acupressure, one physician pointed out that there was a lack of clinical evidence supporting its use for fatigue. Nonetheless, one CMP and one nurse regarded acupressure as safe and noninvasive under careful administration. For (3) moxibustion, one CMP highlighted that it was a very affordable treatment. As recommended by one physician and one nurse, patients receiving chemotherapy should be monitored for possible burns induced by moxibustion, as this might cause subsequent infections (Table 3).
Table 3.
Qualitative Comments on Chinese Medicine Clinical Service Recommendations.
| Service recommendations | Qualitative comments | |||
|---|---|---|---|---|
| Further comments and justifications | Considerations for implementation | Monitoring and evaluation | Future research possibilities | |
| (1) Should acupuncture be used for reducing fatigue among palliative cancer patients? |
Physician: • Patients receiving chemotherapy may avoid the use of acupuncture because of infection risk • Acupuncture brings less adverse effects when compared with CHM as the later may induce herb-drug interactions CMP and Nurse: • Acupuncture is more acceptable by the public without causing herb-drug interactions when compared with CHM |
Physician: • Fatigue level of patients • Risk of infections CMP: • The use of CHM for supplementing the vital Qi may be considered as an add-on to acupuncture Nurse: • Frequency of acupuncture |
Physician and CMP: • Scales that palliative cancer patients can comprehend should be used for monitoring and evaluation CMP: • Patients’ psychological conditions should be monitored during the intervention Nurse: • Other symptoms, such as edema, insomnia, and anorexia, should be monitored |
Physician and CMP: • Validated patient-reported outcome should be used for future clinical studies CMP: • Large observation studies or multicenter RCT with larger sample size on acupuncture for reducing chronic fatigue among palliative cancer patients should be conducted |
| (2) Should acupressure be used for reducing fatigue among palliative cancer patients? | Physician: • There is not enough study to support the use of acupressure for fatigue CMP: • Acupressure is safe and noninvasive, so it can be widely used in hospital and home setting Nurse: • Acupressure is safe and noninvasive which brings less side effects when compared with acupuncture |
Physician: • Safety issues: patients with low platelet count would have bruising easily, so patients and carers should be well informed and educated before receiving or applying acupressure CMP: • Acupressure on body parts close to the tumor should be carefully administered, particularly among patients with osteoporosis or higher bleeding tendency |
Nurse: • Other symptoms, such as edema and insomnia, should also be monitored |
Physician and CMP: • Validated patient-reported outcome should be used for future clinical studies CMP: • Multicenter RCT with larger sample size on acupressure for reducing chronic fatigue should be conducted |
| (3) Should moxibustion be used for reducing nausea and vomiting among palliative cancer patients receiving chemotherapy? |
Physician and Nurse: • Patients should beware of burn induced by moxibustion. Patients receiving chemotherapy are more vulnerable to infection CMP: • Moxibustion is inexpensive that patients are able to afford the treatment |
Physician: • Patients who are intolerant to 5-HT3 antagonist, which are regarded as the gold standard treatment for post-chemotherapy nausea and vomiting, may use moxibustion as an alternative CMP: • Patients with “excessive heat” syndrome in Chinese medicine diagnosis should avoid the use of moxibustion • Extra facilities for ventilation of smoke particulates during the treatment is required |
CMP: • Regular monitoring on patients’ nausea and vomiting severity are needed |
Physician: • Further studies on exploring the combined effect of moxibustion plus 5-HT3 antagonist for post-chemotherapy nausea and vomiting may be conducted Physician and CMP: • Validated patient-reported outcome should be used for future clinical studies CMP: • Effect of the topical application of CHM on reducing nausea and vomiting among palliative cancer patients should be investigated in future research Nurse: • Mechanism of how moxibustion work should be investigated in future studies |
Abbreviations: CHM, Chinese herbal medicine; CMP, Chinese medicine practitioners; RCTs, randomized controlled trials.
Equity, acceptability, and feasibility of the interventions
More than 40% believed that the 3 recommendations would “increase” or “probably increase” health inequities (Figure 3). However, they provided no qualitative comments on how such inequities might arise, as well as the potential impact of such inequities.
Over 75% recognized that these recommendations were acceptable to key stakeholders, and were feasible to implement in the Hong Kong health system (Figures 3 and 4). To this end, some experts provided the following qualitative comments: (1) 2 CMPs and 1 nurse claimed that acupuncture would be more acceptable by the public as compared with CHM, since the former would not cause harmful herb-drug interactions; (2) 1 CMP suggested that acupressure would be widely used in hospital and home setting because it was safe and noninvasive; and (3) 1 CMP recommended that appropriate ventilation of smoke particulates emitted during moxibustion would be required during service provision. When implementing these 3 recommendations, 2 CMPs, 1 physician, and 1 nurse suggested that close monitoring of patients’ health conditions would be of high importance, given the vulnerability of palliative cancer patients (Table 3).
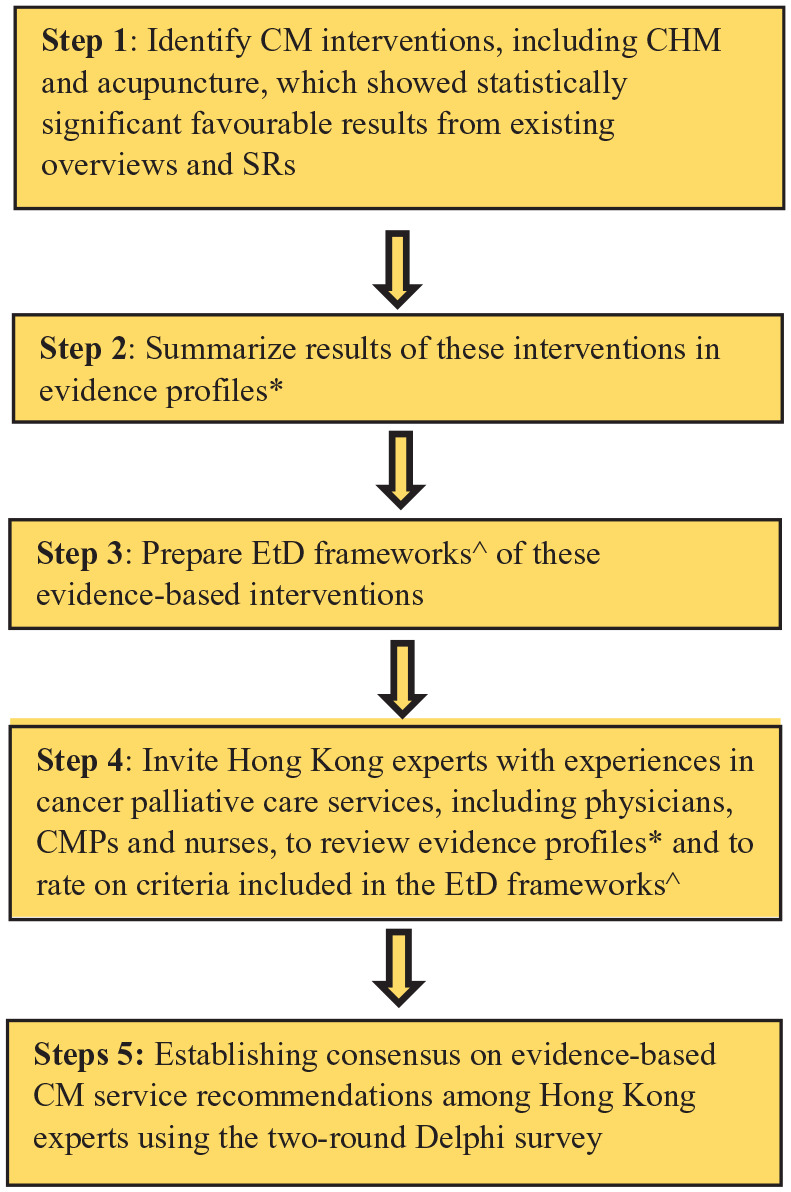
Figure 4.
Evidence to Decision (EtD) framework assessment results on Chinese medicine clinical service recommendations: Q9 to Q10.
Keys. Undesirable, undesirable consequences; desirable, desirable consequences; the percentage (%) of the criteria of each EtD framework was expressed based on the proportion of experts making the judgements.
Balance of consequences
More than 60% agreed that desirable consequences of the 3 recommendations probably or clearly outweighed undesirable consequences (Figure 4). Details of experts’ qualitative comments, including recommendations for future research, are shown in Table 3.
Interventions Without Consensus After the 2-Round Delphi Survey
Overall Rating Results
In the Round 2 Delphi survey, evidence profiles and EtD frameworks of the remaining 4 interventions were reevaluated. None of these interventions reached positive or negative consensus. The median rating ranged from 2.00 to 3.00 (IQR = 1.00-1.75), while the percentage agreement ranged from 33.3% to 66.7% (Table 2).
Quality of evidence assessed by CHIMERAS regarding (1) electroacupuncture plus antiemetics among palliative cancer patients for reducing nausea and vomiting and (2) hyperthermia plus Gui-dan-san-zi-san (桂丹三籽散) among patients receiving radiotherapy for reducing pain were moderate; while the quality of evidence on (3) Zi-long-jing (紫龍金) among patients receiving chemotherapy and (4) Ganoderma lucidum (靈芝) extract among patients receiving chemotherapy or radiotherapy for improving quality of life were high.
Panel experts expressed concerns on the safety of these 4 interventions. For (1) electroacupuncture plus antiemetics, one physician suggested the avoidance of electroacupuncture among patients with pacemaker, artificial joints, and neuropathy. For (2) hyperthermia plus Gui-dan-san-zi-san and (3) Zi-long-jing, safety of applying hyperthermia among patients receiving radiotherapy, as well as potentially harmful herb-drug interactions between Zi-long-jing and chemotherapeutic agents, remained to be main concerns among experts from all disciplines. For (4) Ganoderma lucidum extract, one physician and one nurse expressed concerns on its negative impact on blood cell count, as well as possible negative herb-drug interactions between Ganoderma lucidum and chemotherapeutic agents. Detailed reporting of rating results on the EtD framework criteria and other qualitative comments are presented in Appendix 4 (Supplementary material, available online).
Discussion
Summary of Findings
Three out of 7 evidence-based interventions reached positive consensus as service recommendations. These recommendations were (1) acupuncture for reducing fatigue among palliative cancer patients; (2) acupressure for reducing fatigue among palliative cancer patients; and (3) moxibustion for reducing nausea and vomiting among patients receiving chemotherapy.
Considering Patients’ Values in Developing Future Service Recommendations
Although palliative care ideally should align strongly with patient-centered principles,39 our findings indicated that the experts reported substantial uncertainty about how much patients might value the main outcomes attributable to CM clinical services that failed to reach consensus. This finding was contradictory to the result of a representative survey showing high prevalence of CM service usage in Hong Kong, with 16.5% of the population consulting CMP at least once in a 12-month time frame.40
According to a previous SR of qualitative and quantitative studies, some patients with chronic or serious diseases, including cancer, chose to use CM because of its perceived strength in (1) providing tonic care; (2) individualizing treatment to address various health needs; (3) bringing few adverse effects; (4) guiding for health maintenance and health promotion; and (5) improving health conditions that could not be cured completely by BM.41 However, CM was perceived to be less effective in managing serious diseases and slow in demonstrating treatment effect when compared with BM.41 As patients believed that the co-use of BM and CM would offset weakness of both systems of medicine while retaining their specific strengths, they intended to use BM and CM services simultaneously to address their complex needs in a holistic way.41 On the other hand, both physicians and CMPs agreed that patients should have the right to choose between BM and CM services in a focus group study.23 From the perspective of patient-centered care, our findings suggested that it would be important to address health care professionals’ uncertainty about patients’ value in CM clinical services in the future.
Since patients’ role in clinical decision-making is becoming increasingly recognized,42 future development of evidence-based clinical service recommendations may consider adding patients to the expert panel.43 Besides, experts suggested using validated patient-reported outcomes (PROs) tools to monitor responses to CM treatments. This may help improving health care professionals’ understanding on impact from CM service delivered,44 particularly in enhancing patients’ quality of life and functional performance.
Uncertainty on Adverse Events as a Barrier to Interprofessional Collaboration
Modalities for which consensus was reached in this study were acupuncture and related therapies, with the use of electroacupuncture being rejected by the experts. Despite evidence on the effectiveness of electroacupuncture for reducing nausea and vomiting,3 this intervention was rejected due to physicians’ perceived harm of performing electroacupuncture among patients with cardiac pacemaker45 and neuropathy.46 This may indicate an exaggeration of undesirable effects attributable to electroacupuncture,47 since Delphi result concluded that the use of electroacupuncture should be rejected among all palliative care patients. Such potentially overcautious view implies a need for disseminating evidence on safety of acupuncture treatments among conventionally trained health care professionals, rather than focusing dissemination solely on evidence of efficacy.
Potential interprofessional conflicts over malpractice liability may also be a root cause for deep concerns on CM-related adverse events among the experts. Existing literature suggested a number of strategies for reducing the uncertainty48 among physicians, CMPs, and nurses: (1) determine clinical risk level; (2) document evidence supporting the choice of BM and CM treatments in an appropriate manner; (3) elicit informed consent for patients before carrying out any integrative treatments; (4) closely monitor patients’ health conditions; and (5) improve communications among different professions and arrange for interprofessional consultation if needed.48
However, these strategies for reducing uncertainty may not be applicable for the co-use of CHM and conventional medications in an interprofessional collaborative environment. In our study, concerns over potentially harmful herb-drug interactions49 were repeatedly expressed as a reason for rejecting CHM interventions, even though experts were unable to cite research supporting such concerns. Existing evidence suggested that pharmacokinetic interactions between CHM and chemotherapeutics50 might lead to unpredictable toxicities and even multi-organ failure.51 Building a strong evidence base on the safety of CHM, as well as herb-drug interactions using appropriate observational studies should be regarded as a research priority.
Possible Health Inequities Caused by Implementing the Recommendations
In Hong Kong, fees for CM general consultation service in non–private sector are regulated by the government at a standardized and reasonable level, with provision of subsidies for patients who are in need. Private CM consultation fees are determined by the market without regulation.52 According to the 2019 Thematic Household Survey, a representative survey monitoring health service use among noninstitutionalized Hong Kong population, only 0.5% of the interviewees utilized CM service delivered by non–private sector. Majority (16.0%) consulted CMPs in the private sector.40 Therefore, if the recommended services are implemented, most patients will access them via private CMPs, which would incur much more out-of-pocket expenses. This could be the reason why our experts expressed concerns on widening inequities on CM service access. Policies to reduce financial barriers are needed prior to implementing our current recommendations, for example, through enhancing public-private partnership (PPP).26 PPP can facilitate the contractual relationship between a public agency and a private entity, thus promoting greater private sector participation in the provision of evidence-based CM services for those who cannot afford.53
Tailoring Implementation Strategies to Inform Future Interprofessional Collaboration
While experts were generally positive on the recommendations’ implementability, there is a need to tailor practical strategies for promoting their actual implementation. The design of implementation strategies may follow a 3-step approach described as follows. In Step 1, contextual barriers and facilitators of implementing the recommendations can be identified through conducting qualitative studies guided by the Consolidated Framework for Implementation Research (CFIR).54 In Step 2, assessment results from Step 1 can guide the generation of implementation strategies. These strategies should be tailored to address barriers, and to enhance facilitators of implementation. Implementation strategies catalogues developed by the Expert Recommendations for Implement-ing Change (ERIC) study55 offer a wide range of possible interventions. In Step 3, proposed implementation strategies identified in Step 2 should be finalized via establishing local expert consensus using Delphi techniques, so as to increase stakeholders’ acceptability.56
Strengths and Limitations
A Delphi survey approach based on the GRADE-ADOLOPMENT framework was first applied for developing evidence-based CM clinical service recommendations for cancer palliative care. These evidence-based recommendations have been contextualized to address relationship between BM and CM, as well as features of the Hong Kong health system. The use of EtD framework offered structured recordings of judgements in the process of reaching recommendations among a multidisciplinary panel of experts. This inclusive approach would facilitate interprofessional understanding in the future implementation of these recommendations.
Since this study focused on CHM and acupuncture and related therapies identified from existing overviews of SRs and SRs,2-6 we have omitted other important interventions, such as Tai Chi,57,58 Qigong,57,58 Tuina,58 and cupping.59 Purposive sampling of experts via the investigators’ professional networks might induce researcher bias in the selection process.60 Nevertheless, we believe that the impact of researcher bias would be small, as service recommendations could not be made unless experts across all disciplines arrived at consensus. It is unlikely that researcher bias alone could foster consensus at a high cutoff level of 75% during the Delphi process. Last, our service recommendations were generated without involvement of patients and caregivers. Future Delphi studies should consider adding them to the expert panel, of which the process will empower them in coproducing evidence-based guidelines meaningfully.43
Conclusion
Three evidence-based CM interventions reached positive consensus as service recommendations for cancer palliative care among experts in this GRADE-ADOLOPMENT–based 2-round Delphi survey. To implement these 3 service recommendations in the Hong Kong health system where BM and CM are practiced in a parallel manner, further study is needed for tailoring implementation strategies that address needs of local context, with strong inputs from frontline clinicians across the 2 disciplines.
Supplemental Material
Supplemental material, ServiceGRADE_clean_20200520_v1 for Development of Evidence-Based Chinese Medicine Clinical Service Recommendations for Cancer Palliative Care Using Delphi Approach Based on the Evidence to Decision Framework by Charlene H. L. Wong, Irene X. Y. Wu, Jon Adams, Amie Steel, Jon Wardle, Justin C. Y. Wu, Ting Hung Leung and Vincent C. H. Chung in Integrative Cancer Therapies
Supplemental material, Supplementary_material_20200520 for Development of Evidence-Based Chinese Medicine Clinical Service Recommendations for Cancer Palliative Care Using Delphi Approach Based on the Evidence to Decision Framework by Charlene H. L. Wong, Irene X. Y. Wu, Jon Adams, Amie Steel, Jon Wardle, Justin C. Y. Wu, Ting Hung Leung and Vincent C. H. Chung in Integrative Cancer Therapies
Footnotes
Author Contributions: The following contributed to this work. Study concept and design: CHLW, IXYW, and VCHC. Acquisition of data: CHLW and VCHC. Interpretation of data: CHLW, IXYW, and VCHC. Figures 1 to 4 preparation: CHLW. Tables 1 to 3 preparation: CHLW and IXYW. Appendix 1 to 4 (Supplementary materials) preparation: CHLW. Drafting of the manuscript: CHLW. Critical revision of the manuscript for important intellectual content: IXYW, JA, AS, JW, JCYW, THL, and VCHC. Administrative, technical, or material support: CHLW. All authors reviewed the manuscript, agreed to all the contents, and agreed for the submission.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by the High-level Talents Introduction Plan from Central South University (No. 502045003).
Ethical Approval: Ethical approval was obtained from the Survey and Behavioural Research Ethics Committee, The Chinese University of Hong Kong (Reference No. 023-17).
ORCID iD: Charlene H. L. Wong  https://orcid.org/0000-0003-2623-5855
https://orcid.org/0000-0003-2623-5855
Supplemental Material: Supplemental material for this article is available online.
References
- 1. World Health Organization. WHO Traditional Medicine Strategy: 2014-2023. World Health Organization; 2013. [Google Scholar]
- 2. Chung VCH, Wu X, Lu P, et al. Chinese herbal medicine for symptom management in cancer palliative care: systematic review and meta-analysis. Medicine (Baltimore). 2016;95:e2793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lau CH, Wu X, Chung VC, et al. Acupuncture and related therapies for symptom management in palliative cancer care: systematic review and meta-analysis. Medicine (Baltimore). 2016;95:e2901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wu X, Chung VCH, Lu P, et al. Chinese herbal medicine for improving quality of life among nonsmall cell lung cancer patients: overview of systematic reviews and network meta-analysis. Medicine (Baltimore). 2016;95:e2410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chung VCH, Wu X, Hui EP, et al. Effectiveness of Chinese herbal medicine for cancer palliative care: overview of systematic reviews with meta-analyses. Sci Rep. 2015;5:18111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wu X, Chung VCH, Hui EP, et al. Effectiveness of acupuncture and related therapies for palliative care of cancer: overview of systematic reviews. Sci Rep. 2015;5:16776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Palliative Care. Version 2. Published 2019. Accessed May 10, 2019 https://www.nccn.org/professionals/physician_gls/pdf/palliative.pdf [DOI] [PubMed]
- 8. National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Adult Cancer Pain. Version 1. Published 2019. Accessed February 22, 2019 https://www.nccn.org/professionals/physician_gls/pdf/pain.pdf [DOI] [PubMed]
- 9. Sackett DL, Rosenberg WM, Gray JM, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn’t. BMJ. 1996;312:71-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Neumann I, Brignardello-Petersen R, Wiercioch W, et al. The GRADE evidence-to-decision framework: a report of its testing and application in 15 international guideline panels. Implement Sci. 2015;11:93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Schünemann HJ, Wiercioch W, Brozek J, et al. GRADE Evidence to Decision (EtD) frameworks for adoption, adaptation, and de novo development of trustworthy recommendations: GRADE-ADOLOPMENT. J Clin Epidemiol. 2017;81:101-110. [DOI] [PubMed] [Google Scholar]
- 12. Alonso-Coello P, Oxman AD, Moberg J, et al. GRADE Evidence to Decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 2: clinical practice guidelines. BMJ. 2016;353:i2089. [DOI] [PubMed] [Google Scholar]
- 13. Moberg J, Oxman AD, Rosenbaum S, et al. The GRADE Evidence to Decision (EtD) framework for health system and public health decisions. Health Res Policy Syst. 2018;16:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Tremblay MS, Chaput JP, Adamo KB, et al. Canadian 24-hour movement guidelines for the early years (0–4 years): an integration of physical activity, sedentary behaviour, and sleep. BMC Public Health. 2017;17(suppl 5):874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Okely AD, Ghersi D, Hesketh KD, et al. A collaborative approach to adopting/adapting guidelines—the Australian 24-Hour Movement Guidelines for the early years (birth to 5 years): an integration of physical activity, sedentary behavior, and sleep. BMC Public Health. 2017;17(suppl 5):869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Schunemann H, Mustafa R, Brozek J, et al. Saudi Arabian Handbook for Healthcare Guideline Development Version 1.0. Published 2014. Accessed September 9, 2019 http://www.guidelines-registry.cn/uploadfile/2016/0914/20160914051852300.pdf
- 17. Hong Kong Cancer Registry, Hospital Authority. Overview of Hong Kong cancer statistics of 2016. Published 2016. Accessed February 12, 2019 http://www3.ha.org.hk/cancereg/pdf/overview/Summary%20of%20CanStat%202016.pdf
- 18. Lee VHF, Lam TC, Jing HM, et al. Integrative palliative cancer care in Hong Kong: an overview and an example from the East. Clin Oncol (R Coll Radiol). 2019;31:589-594. [DOI] [PubMed] [Google Scholar]
- 19. Lam YC, Cheng CW, Peng H, et al. Cancer patients’ attitudes towards Chinese medicine: a Hong Kong survey. Chin Med. 2009;4:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Chiu SW, Ko LS, Lee RP. Decolonization and the movement for institutionalization of Chinese medicine in Hong Kong: a political process perspective. Soc Sci Med. 2005;61:1045-1058. [DOI] [PubMed] [Google Scholar]
- 21. Chung VC, Hillier S, Lau CH, et al. Referral to and attitude towards traditional Chinese medicine amongst western medical doctors in postcolonial Hong Kong. Soc Sci Med. 2011;72:247-255. [DOI] [PubMed] [Google Scholar]
- 22. Tzeng YL. A study on the nursing staff’s knowledge, attitude and behaviour and their related factors toward Chinese medicine [in Chinese]. J Nurs (China). 1999;46:57-70. [Google Scholar]
- 23. Chung VC, Ma PH, Lau CH, et al. Developing policy for integrating biomedicine and traditional Chinese medical practice using focus groups and the Delphi technique. Evid Based Complement Alternat Med. 2012;2012:149512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lam TP, Sun KS. Dilemma of integration with Western medicine—views of traditional Chinese medicine practitioners in a predominant Western medical setting. Complement Ther Med. 2013;21:300-305. [DOI] [PubMed] [Google Scholar]
- 25. Chung VC, Ma PH, Hong LC, et al. Organizational determinants of interprofessional collaboration in integrative health care: systematic review of qualitative studies. PLoS One. 2012;7:e50022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Park YL, Canaway R. Integrating traditional and complementary medicine with national healthcare systems for universal health coverage in Asia and the Western Pacific. Health Syst Reform. 2019;5:24-31. [DOI] [PubMed] [Google Scholar]
- 27. Jünger S, Payne SA, Brine J, Radbruch L, Brearley SG. Guidance on Conducting and REporting DElphi Studies (CREDES) in palliative care: recommendations based on a methodological systematic review. Palliat Med. 2017;31:684-706. [DOI] [PubMed] [Google Scholar]
- 28. Shea BJ, Grimshaw JM, Wells GA, et al. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol. 2007;7:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Higgins JPT, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Guyatt GH, Oxman AD, Santesso N, et al. GRADE guidelines: 12. Preparing summary of findings tables—binary outcomes. J Clin Epidemiol. 2013;66:158-172. [DOI] [PubMed] [Google Scholar]
- 31. Guyatt GH, Thorlund K, Oxman AD, et al. GRADE guidelines: 13. Preparing summary of findings tables and evidence profiles—continuous outcomes. J Clin Epidemiol. 2013;66:173-183. [DOI] [PubMed] [Google Scholar]
- 32. Wu XY, Chung VC, Wong CH, et al. CHIMERAS showed better inter-rater reliability and inter-consensus reliability than GRADE in grading quality of evidence: a randomized controlled trial. Eur J Integr Med. 2018;23:116-122. [Google Scholar]
- 33. Alonso-Coello P, Schünemann HJ, Moberg J, et al. GRADE Evidence to Decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 1: introduction. BMJ. 2016;353:i2016. [DOI] [PubMed] [Google Scholar]
- 34. Andrews J, Guyatt G, Oxman AD, et al. GRADE guidelines: 14. Going from evidence to recommendations: the significance and presentation of recommendations. J Clin Epidemiol. 2013;66:719-725. [DOI] [PubMed] [Google Scholar]
- 35. Palinkas LA, Horwitz SM, Green CA, et al. Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Adm Policy Ment Health. 2015;42:533-544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Murphy MK, Black NA, Lamping DL, et al. Consensus development methods, and their use in clinical guideline development. Health Technol Assess. 1998;2:1-88. [PubMed] [Google Scholar]
- 37. Kim TH, White H. On more robust estimation of skewness and kurtosis. Finance Res Lett. 2004;1:56-73. [Google Scholar]
- 38. Diamond IR, Grant RC, Feldman BM, et al. Defining consensus: a systematic review recommends methodologic criteria for reporting of Delphi studies. J Clin Epidemiol. 2014;67:401-409. [DOI] [PubMed] [Google Scholar]
- 39. World Health Organization. WHO definition of palliative care. Published 2019. Accessed April 28, 2019 https://www.who.int/cancer/palliative/definition/en/
- 40. Census and Statistics Department, Hong Kong Special Administrative Region. Thematic Household Survey. Report No. 68. Published November 2019. Accessed January 29, 2020 https://www.statistics.gov.hk/pub/B11302682019XXXXB0100.pdf
- 41. Chung VCH, Ma PHX, Lau CH, et al. Views on traditional Chinese medicine amongst Chinese population: a systematic review of qualitative and quantitative studies. Health Expect. 2014;17:622-636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Elwyn G, Frosch D, Thomson R, et al. Shared decision making: a model for clinical practice. J Gen Intern Med. 2012;27:1361-1367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Armstrong MJ, Mullins CD, Gronseth GS, Gagliardi AR. Impact of patient involvement on clinical practice guideline development: a parallel group study. Implement Sci. 2018;13:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Weldring T, Smith SM. Patient-reported outcomes (PROs) and patient-reported outcome measures (PROMs). Health Serv Insights. 2013;6:61-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Lau EW, Birnie DH, Lemery R, Tang ASL, Green MS. Acupuncture triggering inappropriate ICD shocks. Europace. 2005;7:85-86. [DOI] [PubMed] [Google Scholar]
- 46. White A. A cumulative review of the range and incidence of significant adverse events associated with acupuncture. Acupunct Med. 2004;22:122-133. [DOI] [PubMed] [Google Scholar]
- 47. Chan MWC, Wu XY, Wu JC, Wong SYS, Chung VCH. Safety of acupuncture: overview of systematic reviews. Sci Rep. 2017;7:3369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Cohen MH, Eisenberg DM. Potential physician malpractice liability associated with complementary and integrative medical therapies. Ann Intern Med. 2002;136:596-603. [DOI] [PubMed] [Google Scholar]
- 49. Posadzki P, Watson L, Ernst E. Herb-drug interactions: an overview of systematic reviews. Br J Clin Pharmacol. 2013;75:603-618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Cheng CW, Fan W, Ko SG, Song L, Bian ZX. Evidence-based management of herb-drug interaction in cancer chemotherapy. Explore (NY). 2010;6:324-329. [DOI] [PubMed] [Google Scholar]
- 51. Chiu J, Yau T, Epstein RJ. Complications of traditional Chinese/herbal medicines (TCM)—a guide for perplexed oncologists and other cancer caregivers. Support Care Cancer. 2009;17:231-240. [DOI] [PubMed] [Google Scholar]
- 52. The Government of Hong Kong Special Administrative Region. Press Releases. LCQ3: Development of Chinese Medicine services. Published December 6, 2017. Accessed April 17, 2019 https://www.info.gov.hk/gia/general/201712/06/P2017120600618.htm
- 53. The Government of Hong Kong Special Administrative Region. Serving the community by using the private sector. Policy and practice. Published January 2007. Accessed September 9, 2019 https://www.effo.gov.hk/en/reference/publications/PolicyPractice2007.pdf
- 54. Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Powell BJ, Waltz TJ, Chinman MJ, et al. A refined compilation of implementation strategies: results from the Expert Recommendations for Implementing Change (ERIC) project. Implement Sci. 2015;10:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Holey EA, Feeley JL, Dixon J, Whittaker VJ. An exploration of the use of simple statistics to measure consensus and stability in Delphi studies. BMC Med Res Methodol. 2007;7:52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Zeng Y, Xie X, Cheng ASK. Qigong or tai chi in cancer care: an updated systematic review and meta-analysis. Curr Oncol Rep. 2019;21:48. [DOI] [PubMed] [Google Scholar]
- 58. Tao WW, Jiang H, Tao XM, Jiang P, Sha LY, Sun XC. Effects of acupuncture, Tuina, Tai Chi, Qigong, and traditional Chinese medicine five-element music therapy on symptom management and quality of life for cancer patients: a meta-analysis. J Pain Symptom Manage. 2016;51:728-747. [DOI] [PubMed] [Google Scholar]
- 59. Cao H, Li X, Liu J. An updated review of the efficacy of cupping therapy. PLoS One. 2012;7:e31793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Sharma G. Pros and cons of different sampling techniques. Int J Appl Res. 2017;3:749-752. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, ServiceGRADE_clean_20200520_v1 for Development of Evidence-Based Chinese Medicine Clinical Service Recommendations for Cancer Palliative Care Using Delphi Approach Based on the Evidence to Decision Framework by Charlene H. L. Wong, Irene X. Y. Wu, Jon Adams, Amie Steel, Jon Wardle, Justin C. Y. Wu, Ting Hung Leung and Vincent C. H. Chung in Integrative Cancer Therapies
Supplemental material, Supplementary_material_20200520 for Development of Evidence-Based Chinese Medicine Clinical Service Recommendations for Cancer Palliative Care Using Delphi Approach Based on the Evidence to Decision Framework by Charlene H. L. Wong, Irene X. Y. Wu, Jon Adams, Amie Steel, Jon Wardle, Justin C. Y. Wu, Ting Hung Leung and Vincent C. H. Chung in Integrative Cancer Therapies