Abstract
We describe a 47-year-old female patient with a carotid web and ischemic stroke. A carotid web is a membrane-like shelf of tissue, predominantly affecting the intimal layer of the arterial wall, usually extending from the posterolateral wall of the carotid artery into the lumen, typically at the origin of the internal carotid artery just beyond the bifurcation. It is considered to be an under-recognized etiology of ischemic stroke in young and middle-aged patients. Typically, these patients do not show any coexistent or only few vascular risk factors. Digital subtraction angiography, computer tomography angiography, magnetic resonance angiography, and color-coded duplex sonography are able to identify carotid webs. Therapy strategies include conservative therapy with intake of antiplatelet agents and anticoagulants, or carotid endarterectomy or carotid artery stenting. Optimal therapy strategy remains open. A considerable rate of recurrent cerebrovascular ischemic events has been reported in patients with a symptomatic carotid web and conservative therapy. More data are needed on prevalence, diagnosis, prognosis and therapy of patients with an asymptomatic or a symptomatic carotid web.
Subject Codes: [13] Cerebrovascular Disease/Stroke, [44] Acute Cerebral Infarction, [193] Clinical Studies
Keywords: Neurology, ischemic stroke, stroke management, carotid web
Introduction
Current data indicate that patients with identified stroke etiology and no missed stroke source are receiving the most appropriate prompt secondary prevention in order to decrease short- and long-term disability, morbidity, mortality and recurrence risk. The major pathophysiologic mechanisms, which are recognized as the cause of most ischemic strokes are cardioembolism due to a high-risk cardiac source (such as, for example, atrial fibrillation), large artery atherosclerosis and small vessel disease.1,2 In this case report, we are describing a less frequent stroke etiology.
Case
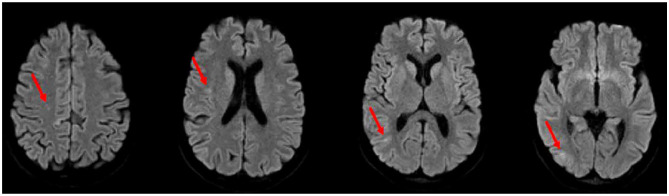
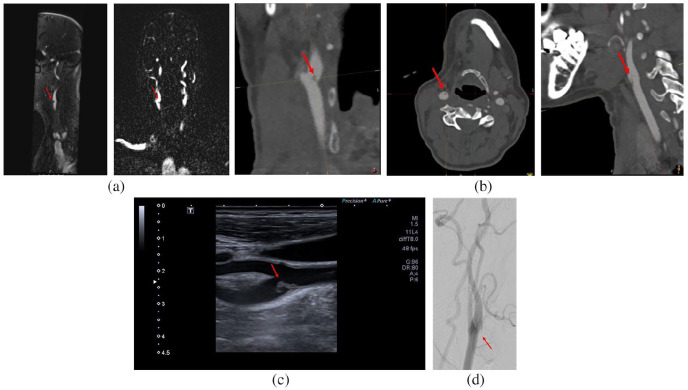
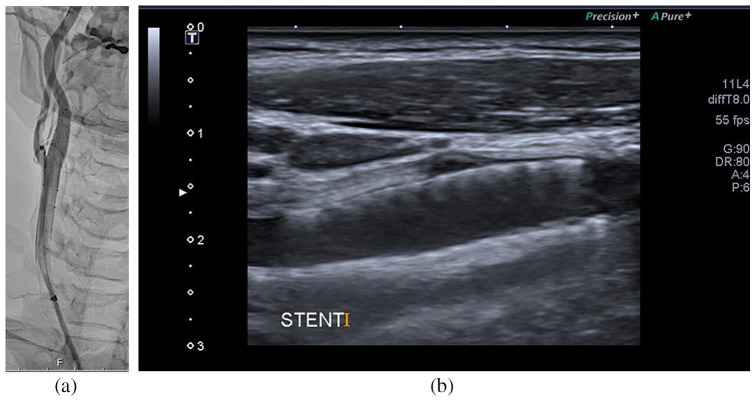
A 47-year-old female patient with neither significant previous medical history nor known vascular risk factors suddenly experienced a short-lasting (few seconds) episode of left-sided sensory disturbance. One hour later, she stumbled while climbing stairs and noted a weak left hand grip. She called the ambulance service. On emergency admission, 83 min after symptom onset, a residual mild paresis of the left arm was seen in neurological examination. Other physical examination detected no abnormalities. Laboratory investigations and electrocardiogram (ECG) were normal. Cerebral magnetic resonance imaging (MRI) and angiography (MRA) (Figure 1) demonstrated several small acute ischemic lesions in the territory of the right middle cerebral artery (MCA) with no visible vessel occlusion (Figure 1). Also, MRA (Figure 2(a)) identified an intraluminal contrast filling defect in the proximal part of the right internal carotid artery (ICA), suspected to be a carotid web. However, an atherosclerotic plaque was not fully excluded at first. A conservative therapy with aspirin 100 mg/d, clopidogrel 75 mg/d, and atorvastatin 80 mg/d was initiated and the patient was hospitalized on our stroke unit. There, transesophageal echocardiography was normal. Computer tomography angiography (CTA) (Figure 2(b)) and color-coded duplex sonography (Figure 2(c)) confirmed the suspected diagnosis of a carotid web in the right ICA. The latter investigation showed an isoechogenic, floating, “question-mark-shaped” lesion extending into the lumen of the right proximal ICA without any hemodynamically significant stenosis. There was an interdisciplinary discussion of the patient at our weekly neurovascular board. Taking the considerable rate of recurrent cerebrovascular ischemic events in patients with a symptomatic carotid web treated conservatively reported in literature and our hospital’s neurointerventionalists’ expertise into account, a digital subtraction angiography (DSA) (Figure 2(d)) was performed and a CGuard stent (7 mm x 30 mm) (Figure 3(a)) was deployed in the right extracranial carotid artery. On the following day, color-coded duplex sonography (Figure 3(b)) showed a fully open stent without any flow or structural abnormalities. On day 4, the patient was discharged home in good health. No recurrent ischemic transient ischemic attack (TIA) or stroke has occurred since (month 12).
Figure 1.
Diffusion-weighted magnetic resonance imaging showing acute ischemic stroke lesions (red arrows) in the right hemisphere.
Figure 2.
Neuroimagings presenting a carotid web (red arrows) in the right proximal internal carotid artery: (a) MR angiography, (b) CT angiography, (c) neurovascular sonography, and (d) digital subtraction angiography.
Figure 3.
Neuroimagings after carotid artery stenting: (a) digital subtraction angiography and (b) neurovascular sonography.
Discussion
The first patient with a carotid web depicted was published by Rainer et al.3 It was a young female patient with a recurrent transient right-sided hemiparesis and a diaphragm-like intraluminal filling defect in the left carotid artery. Different shapes of a carotid web have been described since—weblike, weblike septum, diaphragm, thrombotic carotid megabulb, spur or shell. The current definition of a carotid web is a membrane-like shelf of tissue, usually extending from the posterolateral wall of the carotid artery into the lumen, typically at the origin of the internal carotid artery (ICA) just beyond the bifurcation. Carotid webs predominantly affect the intimal layer of the arterial wall, whereas classic fibromuscular dysplasia is characterized by hyperplasia of fibrous tissue and smooth muscle cells causing media thickening and multifocal “string-of-beads” appearance in DSA.4–7
The exact prevalence of carotid webs in the general population is unclear. It is thought to be a rather rare but likely misdiagnosed and under-recognized condition. In the MR CLEAN trial, 11 (2.5%) carotid webs were found in CTA at the symptomatic and 2 (0.5%) at the asymptomatic side in a subanalysis of patients with intracranial large-vessel occlusion—with fair to good interobserver agreement.4 Several case-control series about patients <60 years of age with cryptogenic ischemic stroke found a 9.4%–37% prevalence of a carotid web ipsilateral to the ischemic stroke associated with variable but potentially considerable stroke severity.5–9 Also, the published data available suggests a higher prevalence in women and in black people.4–11
Pathophysiologically, a carotid web might generate altered hemodynamics with blood flow stagnation and turbulence, possibly triggering thrombus formation and leading to embolism at a relatively early age despite no or only few vascular risk factors.4,6–10
Historically, conventional DSA has been considered to be the “gold standard” technique for carotid artery imaging, having a high temporal and spatial resolution. However, it bears the risk of being invasive and missing a carotid web by using the standard posteroanterior and lateral projections.5
Noninvasive and easier accessible modalities such as conventional CTA, MRA and color-coded duplex sonography may be performed. Color-coded duplex sonography usually demonstrates a carotid web by a shelf-like outgrowth from the arterial wall, potentially causing a hemodynamically significant stenosis. Color-coded duplex sonography has the advantage of being widely available and being routinely performed. However, its quality highly depends on the operator’s experience and skills and carotid webs may be misdiagnosed as an isolated atherosclerotic plaque in some patients.5,8
CTA allows detailed anatomical imaging of the craniocervical vessels with multiplane reconstruction and short acquisition time. It allows good visualization of the vessel wall, differentiation of a carotid web from atherosclerosis. However, CTA lacks information regarding flow dynamics and lesion composition and has the inherited disadvantage of exposure to radiation and iodinated contrast media.4–6,8–10
MRA can be obtained without application of a contrast agent as a time-of-flight-sequence, based on blood flow or as a contrast-enhanced study using gadolinium media. Despite its cost and time-consuming nature, it is an appropriate imaging technique in patients with contraindications for CTA with the additional advantage of clearly depicting areas surrounding arteries. However, data on detection of a carotid web in MRA is limited to date.5,9,12
A recent study has compared DSA, CTA and color-coded duplex sonography in identification of carotid webs. CTA and DSA showed comparable and superior performance as compared to color-coded duplex sonography.13
Due to limited data, best therapy strategy in patients with a carotid web remains open.2,3,5,7–9 Conservative therapy has been proposed and suggested to be effective especially in asymptomatic patients. However, studies have published a considerable rate of recurrent cerebrovascular ischemic events in at least every third to up to every second patient who was treated conservatively.6–8,10 Due to the carotid web’s fibrotic composition, positive remodeling is less likely than in atherosclerotic disease. This might explain potentially little therapy effect and a high recurrence rate if patients with a symptomatic carotid web are treated conservatively with antiplatelet monotherapy or dual therapy. Anticoagulants might be more effective, but data is scarce.5,11
The available data report carotid endarterectomy (CEA) or carotid artery stenting (CAS) in patients with a carotid web to be safe and effective.5–7,8,11
In a recent systematic literature review, follow-up data (median time of 14 months) was reported for 42 (60%) symptomatic patients treated with either CEA or CAS. Neither any complications nor any recurrent event occurred.7
The low risk of complications of CEA or CAS in patients with a carotid web may be related to the fibrotic composition and locally circumscribed pathology as opposed to atherosclerotic disease. In addition, in case of a carotid web, there is no need of highly thromboembolic pre- and post-stenting angioplasty in CAS because the artery lumen is mostly preserved. Also, a benefit of CAS may be the generation of a scaffold for new endothelialization, for endoluminal remodeling.5
Conclusion
To conclude, more data are needed on prevalence, diagnosis, prognosis and therapy of patients with an asymptomatic or a symptomatic carotid web. What is quite unique about our patient is, that we present MRI/MRA, CTA, DSA and neurovascular sonography data. Also, our case report is increasing awareness of a carotid web potentially being the cause of an ischemic stroke and is summarizing available literature.
Acknowledgments
We thank the Bernese stroke team for its contribution.
Footnotes
Declaration of conflicting interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Marina Krasteva has received personal-fee for a stroke research fellowship by the Konstantin and Zenovia Katzarovi foundation. The other co-authors have nothing to disclose directly related with this case report.
Ethical approval: Our institution does not require ethical approval for reporting individual cases or case series.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Written informed consent was obtained from the patient for her anonymized information to be published in this article.
ORCID iD: Mirjam R Heldner  https://orcid.org/0000-0002-3594-2159
https://orcid.org/0000-0002-3594-2159
References
- 1. Norrving B, Barrick J, Davalos A, et al. Action plan for stroke in Europe 2018-2030. Eur Stroke J 2018; 3(4): 309–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2019; 50: e344–e418. [DOI] [PubMed] [Google Scholar]
- 3. Rainer WG, Cramer GG, Newby JP, et al. Fibromuscular hyperplasia of the carotid artery causing positional cerebral ischemia. Ann Surg 1968; 167(3): 444–446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Compagne KCJ, van Es ACGM, Berkhemer OA, et al. Prevalence of carotid web in patients with acute intracranial stroke due to large vessel occlusion. Radiology 2018; 286: 1000–1007. [DOI] [PubMed] [Google Scholar]
- 5. Kim SJ, Nogueira RG, Haussen DC. Current understanding and gaps in research of carotid webs in ischemic strokes: a review. JAMA Neurol 2019; 76: 355–361. [DOI] [PubMed] [Google Scholar]
- 6. Haussen DC, Grossberg JA, Bouslama M, et al. Carotid web (intimal fibromuscular dysplasia) has high stroke recurrence risk and is amenable to stenting. Stroke 2017; 48(11): 3134–3137. [DOI] [PubMed] [Google Scholar]
- 7. Zhang AJ, Dhruv P, Choi P, et al. A systematic literature review of patients with carotid web and acute ischemic stroke. Stroke 2018; 49(12): 2872–2876. [DOI] [PubMed] [Google Scholar]
- 8. Joux J, Chausson N, Jeannin S, et al. Carotid-bulb atypical fibromuscular dysplasia in young Afro-Caribbean patients with stroke. Stroke 2014; 45(12): 3711–3713. [DOI] [PubMed] [Google Scholar]
- 9. Coutinho JM, Derkatch S, Potvin AR, et al. Carotid artery web and ischemic stroke: a case-control study. Neurology 2017; 88: 65–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Choi PM, Singh D, Trivedi A, et al. Carotid webs and recurrent ischemic strokes in the era of CT angiography. AJNR Am J Neuroradiol 2015; 36(11): 2134–2139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Haussen DC, Grossberg JA, Koch S, et al. Multicenter experience with stenting for symptomatic carotid web. Interv Neurol 2018; 7(6): 413–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Boesen ME, Eswaradass PV, Singh D, et al. MR imaging of carotid webs. Neuroradiology 2017; 59(4): 361–365. [DOI] [PubMed] [Google Scholar]
- 13. Madaelil TP, Grossberg JA, Nogueira RG, et al. Multimodality imaging in carotid web. Front Neurol 2019; 10: 220. [DOI] [PMC free article] [PubMed] [Google Scholar]