Abstract
Clostridium difficile infection is a common nosocomial infection in US hospitals, accounting for approximately 12 800 deaths annually in the United States. These infections are often associated with the use of antibiotics, which can alter the gut microbiome and thus render patients susceptible to C difficile infection. C difficile is often spread via fecal oral transmission. Multiple medications have been developed, but recurrence rates reach 60% after treatment. Recent data have shown that zinc supplementation decreases the recurrence of C difficile infection. In this article, we present a case of recurrent C difficile infection with zinc deficiency in which zinc supplementation improved the symptoms and reduced the incidence of recurrence.
Keywords: recurrent Clostridium difficile infection, zinc supplementation, zinc deficiency
Introduction
Clostridium difficile infection is a common cause of nosocomial infections in US hospitals and is the ninth leading cause of death related to gastrointestinal diseases.1 According to the Centers of Disease Control and Prevention, approximately 2.8 million antibiotic-resistant infections occur annually in the United States, and in 2017, 223 900 cases of C difficile infections were reported, from which 12 800 people died.2 C difficile infection results from increased exposure to antibiotics, which alter the natural flora of the intestine. A meta-analysis reported that C difficile infection is most strongly associated with such antibiotics as third-generation cephalosporins, clindamycin, carbapenems, trimethoprim/sulfonamides, and fluoroquinolones.3 In addition to antibiotics, proton pump inhibitors have also played a role in causing C difficile colitis. Infection risk was very high within the first month but can remain high for up to 3 months after antibiotic exposure, and the recurrence rate is 20.9% after initial infection; thereafter, the risk of multiple recurrent infections is higher.4-6 Multiple treatment options, such as metronidazole, vancomycin, nitazoxanide, fidaxomicin, and fecal microbiota transplantation (FMT), have been developed for the treatment of initial and recurrent C difficile infection. Recent emerging data have indicated that zinc deficiency is associated with an increased recurrence of C difficile infection. Zinc is an essential trace element obtained from the diet and is excreted via the gastrointestinal tract. The World Health Organization recommends zinc supplementation in the treatment of acute diarrheal illness.7 In this article, we present an interesting case of recurrent C difficile infection with zinc deficiency, in which zinc supplementation improved the symptoms and reduced the incidence of recurrence.
Case Report
A 52-year-old male with a previous medical history of type 1 diabetes mellitus, s/p renal transplant on tacrolimus and prednisone, recurrent C difficile infection, legal blindness, and left below-knee amputation presented to the emergency department in January 2020 for weakness. On admission, the patient was hypotensive with a systolic blood pressure of 90 mm Hg and acidotic with a bicarbonate level of 12 mEq/L; additionally, he presented with an anion gap of 24 mmol/L, an elevated blood sugar level of 481 mg/dL, a creatinine level of 4.5 mg/dL, and a baseline creatinine of 2.2 mg/dL. The patient was admitted to an intensive care unit under the impression of hypovolemia and diabetic ketoacidosis. The patient was started on intravenous fluids and an insulin drip and exhibited improvements within 48 hours. His vital signs were stable, with a systolic blood pressure >110 mm Hg, a bicarbonate level of 20 mEq/L, a closed anion gap, and normal sugar level. The insulin drip was then switched to long-acting Lantus. During this admission, the patient had diarrhea and was tested positive for C difficile infection, with no recent history of antibiotic use. As noted above, the patient had a history of recurrent C difficile infection.
The patient experienced his first episode of C difficile infection in July 2019 and was treated with vancomycin for 14 days. At the time of this episode, he reported a history of antibiotic use (cefdinir) for a urinary tract infection. After completing the vancomycin course later in September 2019, the patient returned to the hospital with complaints of diarrhea and tested positive for C difficile. At this time, the patient was treated with another long taper of vancomycin. He again returned with similar complaints in January 2020 (the current admission) with recurrent C difficile infection. During the intervals between episodes, the patient never reported a complete relief of diarrhea and reported a weight loss of 30 lbs.
During this admission, given his weight loss, the patient underwent endoscopy and colonoscopy, the results of which were normal (Figures 1 and 2). Random biopsies in the duodenum and stomach revealed mild reactive epithelial changes, and random colon biopsies were normal. Given his nutritional status, his zinc levels were assessed and found to be low, at 36 µg/dL (60-130 µg/dL). The patient refused FMT during this admission; thus, he was treated with long-taper vancomycin and zinc supplementation. The patient improved and was discharged to rehabilitation in a stable condition. The patient received follow-up care in the clinic and reported a relief of symptoms, including diarrhea, after completion of the C difficile treatment, and subsequently, the patient continued to receive zinc supplementation. The patient has not had any further episodes of C difficile infection within the past 3 months.
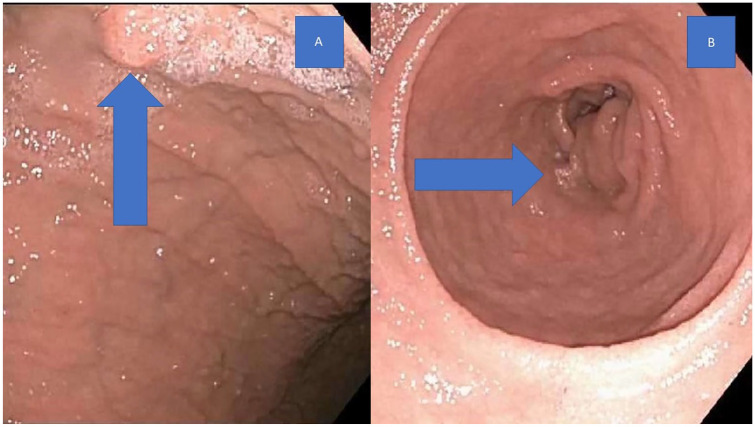
Figure 1.
Gastric polyp (shown by arrow; A). Normal pylorus (shown by arrow; B).
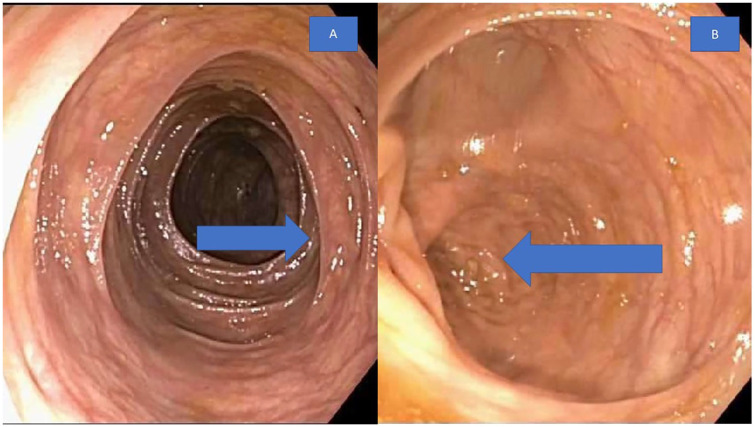
Figure 2.
Normal colonic mucosa (shown by arrow; A). Normal ileocecal valve (shown by arrow; B).
Discussion
Clostridium difficile is a Gram-positive anaerobic spore-forming bacterium that produces enterotoxins. C difficile was first described by Hall and O’Toole in 1935 based on their investigation of bacterial flora in newborns. In 1978, C difficile was isolated in the stool of a pseudomembranous colitis patient.8,9 C difficile produces 2 toxins: toxin A (enterotoxin) and toxin B (cytotoxin). These toxins are glucosyltransferases that inactivate the small GTP-binding protein Rho, which leads to disruption of the cytoskeleton. These toxins exhibit synergistic action with other pro-inflammatory mediators and cytokines and result in inflammation, injury, and cell death.10 In addition to the major toxins, other toxins such as CDT binary toxin, fibronectin-binding protein FbpA, fimbriae, SlpA S-layer, Cwp84 cysteine protease, and Cwp66 and CwpV adhesions are also known to cause inflammation and intestinal injury.11 The gut microbiota generally prevents the colonization of C difficile bacteria; however, when the gut flora is disrupted by antibiotic use, bacteria colonization and infection can result. C difficile is spread through fecal oral transmission via spore formation. The resultant intestinal injury and inflammation lead to varied symptoms, ranging from mild symptoms such as abdominal pain, nausea, vomiting, diarrhea, and melena to severe symptoms such as severe dehydration, hypovolemia and hypoalbuminemia, megacolon, ileus, perforation, and death. This condition also causes deficiencies in trace elements secondary to impaired intestinal absorption and increased losses.12
Zinc is an essential trace element that plays a vital role in maintaining various physiologic and metabolic processes, such as immune functioning, protein synthesis, and DNA synthesis, thus supporting normal growth and development. Zinc also exhibits antioxidant properties, facilitating wound healing.13 In previous works, zinc deficiencies have been well-documented in celiac disease, ulcerative colitis, and Crohn’s disease secondary to malabsorption and inflammation of the intestinal wall.14 Diarrhea caused by zinc deficiency has been reported in infants with hereditary acrodermatitis enteropathica and in adults with total parenteral nutrition.15,16 It is thought that zinc deficiency increases activation of the nitric oxide synthase pathway and intestinal uroguanylin, both of which alter intestinal permeability and thus cause diarrhea.17 This interpretation has been supported by a meta-analysis demonstrating that zinc supplementation reduces the incidence of diarrhea in children.18 In addition, zinc can influence the microbiome in the gut; for example, multiple studies in pigs have reported that high levels of zinc oxide regulate the ileum microbiome in piglets.19,20
The 2 above-mentioned studies support our observation that zinc deficiency caused our patient to experience multiple recurrent C difficile infections and that zinc supplementation improved his symptoms and reduced the recurrence of C difficile. In a retrospective cohort study published in 2018, the authors studied the relationship between zinc deficiency and C difficile recurrence after FMT treatment.21 A total of 80 patients were included in this study, 31 patients with low zinc levels and 59 patients with normal zinc levels. Five of the 31 low-zinc patients (16%) experienced recurrent C difficile infections compared with 3 of the 49 (6%) normal-zinc patients. After the patients in the low-zinc group were treated with zinc supplementation, the rate of C difficile infection decreased to 8% compared with 50% among patients who did not receive supplementation. This study supports prior evidence indicating that zinc deficiency plays an important role in the recurrence of C difficile infection. In contrast, one study in mice found that a high-zinc diet rendered mice susceptible to severe C difficile infection, while normal zinc supplementation had no effect on C difficile infection.22 In addition, it seems that zinc supplementation should only be considered in zinc-deficient individuals, particularly in light of conflicting reports regarding the impact of zinc supplementation on the pathogenesis of C difficile, and in the future studies are necessary to clearly determine the role of zinc in reducing C difficile recurrence rates.
Footnotes
Authors’ Note: Any enquiries regarding supporting data availability of this study should be directed to the corresponding author.
Author Contributions: Article guarantor, literature research, and manuscript preparation: Swetha Parvataneni
Case management, manuscript editing, manuscript revision/review, and final version approval: Swetha Parvataneni and Avinash R. Dasari
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics Approval: Our institution does not require ethics approval for reporting individual cases.
Informed consent: Consent was obtained from the patient for their anonymized information to be published in this article.
ORCID iD: Swetha Parvataneni  https://orcid.org/0000-0002-5932-2237
https://orcid.org/0000-0002-5932-2237
References
- 1. Peery AF, Dellon ES, Lund J, et al. Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology. 2012;143:1179-1187.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Centers for Disease Control and Prevention. Biggest threats and data antibiotic/antimicrobial resistance threats in the United States. Accessed June 26, 2020 https://www.cdc.gov/drugresistance/biggest-threats.html
- 3. Slimings C, Riley TV. Antibiotics and hospital-acquired Clostridium difficile infection: update of systematic review and meta-analysis. J Antimicrob Chemother. 2014;69:881-891. [DOI] [PubMed] [Google Scholar]
- 4. Hensgens MPM, Goorhuis A, Dekkers OM, Kuijper EJ. Time interval of increased risk for Clostridium difficile infection after exposure to antibiotics. J Antimicrob Chemother. 2012;67:742-748. [DOI] [PubMed] [Google Scholar]
- 5. Lessa FC, Mu Y, Bamberg WM, et al. Burden of Clostridium difficile infection in the United States. N Engl J Med. 2015; 372:825-834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Eyre DW, Walker AS, Wyllie D, et al. Predictors of first recurrence of Clostridium difficile infection: implications for initial management. Clin Infect Dis. 2012;55(suppl 2):S77-S87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. World Health Organization. Zinc supplementation in the management of diarrhoea. Published April 2011. Accessed June 26, 2020 http://www.who.int/elena/titles/bbc/zinc_diarrhea/en/
- 8. Hall IC. Intestinal flora in newborn infants. Am J Dis Child. 1935;49:390-402. [Google Scholar]
- 9. Bartlett JG, Moon N, Chang TW, Taylor N, Onderdonk AB. Role of Clostridium difficile in antibiotic-associated pseudomembranous colitis. Gastroenterology. 1978;75:778-782. [PubMed] [Google Scholar]
- 10. Rineh A, Kelso MJ, Vatansever F, Tegos GP, Hamblin MR. Clostridium difficile infection: molecular pathogenesis and novel therapeutics. Expert Rev Anti Infect Ther. 2014;12:131-150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kuehne SA, Cartman ST, Heap JT, Kelly ML, Cockayne A, Minton NP. The role of toxin A and toxin B in Clostridium difficile infection. Nature. 2010;467:711-713. [DOI] [PubMed] [Google Scholar]
- 12. Goudarzi M, Seyedjavadi SS, Goudarzi H, Aghdam EM, Nazeri S. Clostridium difficile infection: epidemiology, pathogenesis, risk factors, and therapeutic options. Scientifica (Cairo). 2014;2014:916826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bhattacharya PT, Misra SR, Hussain M. Nutritional aspects of essential trace elements in oral health and disease: an extensive review. Scientifica (Cairo). 2016;2016:5464373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Skrovanek S, DiGuilio K, Bailey R, et al. Zinc and gastrointestinal disease. World J Gastrointest Pathophysiol. 2014;5:496-513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Barnes PM, Moynahan EJ. Zinc deficiency in acrodermatitis enteropathica: multiple dietary intolerance treated with synthetic diet. Proc R Soc Med. 1973;66:327-329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kay RG, Tasman-Jones C, Pybus J, Whiting R, Black H. A syndrome of acute zinc deficiency during total parenteral alimentation in man. Ann Surg. 1976;183:331-340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Cui L, Blanchard RK, Cousins RJ. The permissive effect of zinc deficiency on uroguanylin and inducible nitric oxide synthase gene upregulation in rat intestine induced by interleukin 1alpha is rapidly reversed by zinc repletion. J Nutr. 2003;133:51-56. [DOI] [PubMed] [Google Scholar]
- 18. Lamberti LM, Walker CLF, Chan KY, Jian WY, Black RE. Oral zinc supplementation for the treatment of acute diarrhea in children: a systematic review and meta-analysis. Nutrients. 2013;5:4715-4740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Pieper R, Vahjen W, Neumann K, Van Kessel AG, Zentek J. Dose-dependent effects of dietary zinc oxide on bacterial communities and metabolic profiles in the ileum of weaned pigs. J Anim Physiol Anim Nutr (Berl). 2012;96:825-833. [DOI] [PubMed] [Google Scholar]
- 20. Vahjen W, Pieper R, Zentek J. Increased dietary zinc oxide changes the bacterial core and enterobacterial composition in the ileum of piglets. J Anim Sci. 2011;89:2430-2439. [DOI] [PubMed] [Google Scholar]
- 21. Niccum BA, Stein DJ, Behm BW, Hays RA. Zinc deficiency and the recurrence of Clostridium difficile infection after fecal microbiota transplant: a retrospective cohort study. J Nutr Metab. 2018;2018:9682975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Zackular JP, Moore JL, Jordan AT, et al. Dietary zinc alters the microbiota and decreases resistance to Clostridium difficile infection. Nat Med. 2016;22:1330-1334. [DOI] [PMC free article] [PubMed] [Google Scholar]