Abstract
The 2019 novel coronavirus pneumonia (COVID-19) is an ongoing global pandemic with a worldwide death toll of over 416,000 as of June 10, 2020. Although the first documented cases in Wuhan, China were patients with severe respiratory symptoms including cough, fever, fatigue, and shortness of breath, the disease process can also be asymptomatic. In this case report, an asymptomatic 63-year-old male with Lynch syndrome undergoing a routine staging fluorodeoxyglucose positron-emission tomography/computed tomography was found to have typical radiologic features of COVID-19 with marked pulmonary FDG uptake and was subsequently diagnosed via reverse-transcription polymerase chain reaction. Many studies have described the appearance of COVID-19 on chest radiography and CT with the most common imaging features being bilateral, peripheral, and basilar predominant ground glass opacities and consolidation. Although these findings are typically nonspecific for an atypical lung infection, early recognition of COVID-19 in the setting of a global pandemic (even in the asymptomatic patient) is critical in order to limit the spread of disease.
Keywords: COVID-19, Coronavirus, FDG PET/CT
Case Summary
An asymptomatic 63-year-old Vietnamese male with a history of Lynch syndrome and colon, liver, and thyroid cancer presented to our nuclear medicine suite in early April 2020 for routine staging fluorodeoxyglucose positron-emission tomography/computed tomography (FDG PET/CT) extending from the skull base to the mid thighs. Patient was status post remote thyroidectomy and radioactive iodine therapy for papillary thyroid cancer and right hemicolectomy with neoadjuvant chemotherapy in 2019 for colon adenocarcinoma. He had also undergone segment VI hepatectomy for hepatocellular carcinoma secondary to hepatitis C.
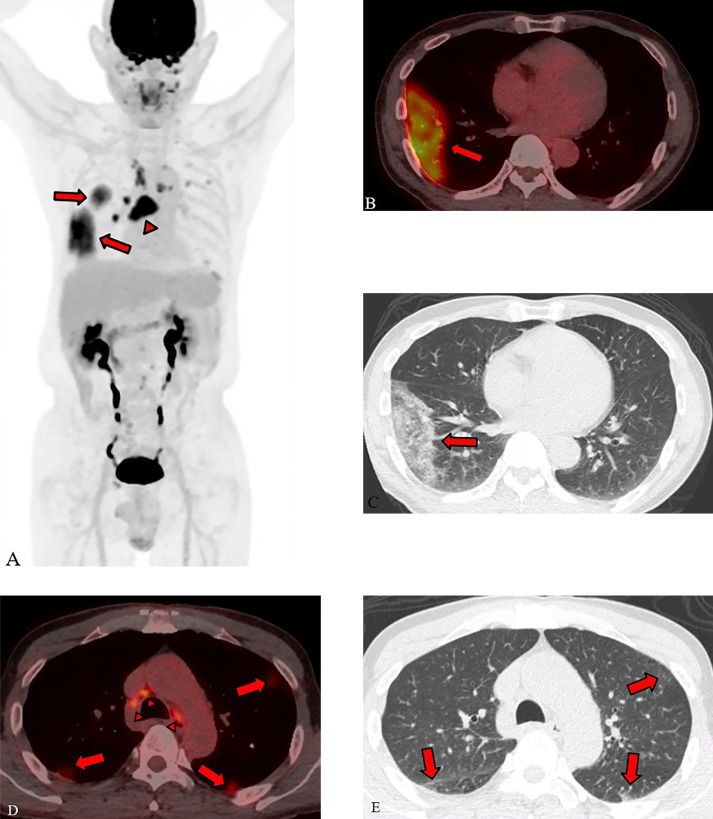
The most recent cancer staging imaging performed four months prior (contrast enhanced CT of the chest, abdomen, and pelvis) described 2 small abdominal lymph nodes suspicious for recurrent colon cancer but was otherwise negative. Notably, the lungs at that time were clear. FDG PET/CT demonstrated multifocal, peripheral ground glass opacities throughout the lungs with right lower lobe predominance. All ground glass opacities, some of which were very faint on the attenuation correction CT, demonstrated markedly increased FDG uptake. The maximum standardized uptake value (SUV) was 9.5 in the right lower lobe. The radiologic appearance of the parenchymal lung disease was typical for COVID-19 and the ordering provider and the nuclear medicine technicians working with the patient were alerted. There was also increased FDG uptake within numerous cervical and thoracic lymph nodes with SUV max of 9.6 in a subcarinal nodal conglomerate (Fig. 1). Given the similar FDG uptake of the lymph nodes compared to the ground glass lung opacities, hypermetabolic lymph nodes were favored to represent reactive nodes secondary to COVID-19 lung involvement rather than new, metastatic disease.
Fig. 1.
(A) PET maximum intensity projection (MIP) image demonstrates two hypermetabolic areas in the right lung (arrows) with an SUV max of 9.5 in the right lower lobe. There are also hypermetabolic mediastinal and hilar lymph nodes (arrowhead) with an SUV max of 9.6 in a subcarinal nodal conglomerate. Axial images (B, low dose CT; C, PET/CT fusion) demonstrate a large area of peripheral ground glass in the right lower lobe (arrow) with associated increased FDG uptake. Additional axial PET/CT fusion image (D) shows hypermetabolic mediastinal lymph nodes (arrowheads) as well as areas of increased FDG uptake in the periphery of both lungs (arrows), corresponding to subtle areas of parenchymal ground glass opacities on axial CT (E).
FDG PET/CT also showed a long segment of small bowel in the mid-abdomen with mildly increased FDG uptake (SUV max of 4.7). The 2 lymph nodes in the lower abdomen (described on prior cancer staging CT) had slightly decreased in size, but also showed mildly increased FDG uptake with SUV max of 2.9. These findings are of uncertain significance, but were described as possible gastrointestinal manifestations of COVID-19. Reevaluation of these areas on repeat FDG PET/CT (and correlation with CEA levels) in 3 to 6 months after resolution of lung disease was recommended.
The following day, patient underwent testing for COVID-19 via nasopharyngeal swab and the hospital's lab-developed SARS-CoV-2 (COVID-19) qualitative PCR was positive. The patient was alerted of these results by the laboratory and discussed its implication with his provider at the international medicine clinic. Patient denied any symptoms including cough, fever, or shortness of breath. He was not employed and lives alone. Patient was advised to self-isolate.
At the time of this patient's FDG PET/CT, most elective examinations (particularly exams for patients with flu-like symptoms or with serious pre-existing health conditions) were being rescheduled per a temporary hospital policy. All patients entering the hospital were screened at the entrances for symptoms of COVID-19 and, if symptomatic, would be provided with a surgical mask and placed in an isolation room. In this specific case, our patient was asymptomatic, but chose to wear a surgical mask as a precaution. Unless patients were known to have COVID-19, imaging suites were sanitized using standard cleaning procedures using quaternary ammonium/alcohol impregnated wipes. If an infected patient was imaged, the imaging room would be closed for one hour following the exam and cleaned via a high-efficiency particulate air (HEPA) filter. Each day, all radiologists and nuclear medicine technicians were provided with standard 3-layer disposable surgical masks for continuous use throughout the day, particularly during direct patient care. Employees exposed to COVID-19 were required to return to work if they were asymptomatic and attest to their daily health and lack of relevant symptoms. No reverse-transcription polymerase chain reaction (RT-PCR) tests were performed for asymptomatic employees. Although COVID-19 was not confirmed in our patient until after imaging was complete and the patient was discharged, the diagnosis was suspected based on his imaging and the nuclear medicine technicians were informed of their possible exposure that day and advised to undergo daily self-screening (Fig. 1).
Discussion
In late December 2019, a novel coronavirus (COVID-19) was discovered in a cluster of patients with severe lower respiratory tract infections in Wuhan, Hubei Province, China. Symptoms were typical of severe pneumonia including cough, fever, fatigue, and shortness of breath [1]. China reported this outbreak to the World Health Organization on December 31, 2019 and cases of COVID-19 within and outside of China began to exponentially increase in the following weeks and months [2]. As of June 10, 2020, COVID-19 has spread to 213 countries and infected over 7.4 million people. The global death toll currently exceeds 400,000 and World Health Organization classified COVID-19 as a public health emergency of international concern on January 30, 2020 and a worldwide pandemic on March 11, 2020. The first known case in the United States was confirmed in Washington state on January 20, 2020 [3]. COVID-19 has since spread to all 50 states with over 2 million confirmed cases in the United States and over 115,000 deaths [4].
Clinical manifestations of COVID-19 are variable ranging from no symptoms to critical illness including respiratory failure, septic shock, and multiorgan dysfunction. Most patients with COVID-19 (approximately 80%) experience mild respiratory symptoms typical of other viral infections including, but not limited to cough, fever, headache, dyspnea, and fatigue [5]. Elderly and patients of any age with severe underlying health conditions are at increased risk of serious respiratory illness including acute respiratory distress syndrome and death. In addition to pulmonary symptoms, gastrointestinal symptoms including diarrhea, nausea, vomiting, and abdominal pain have been reported in approximately 5% of infected patients [6]. Additionally, SARS-CoV-2 RNA has been identified in anal/rectal swabs and stool specimens in COVID-19 patients even after upper respiratory tract infection had cleared, and respiratory samples were negative [7,8]. Given the potential for gastrointestinal involvement in COVID-19 patients, we suggested that the increased FDG uptake within our patient's gastrointestinal system (specifically within a single long segment of small bowel and 2 abdominal lymph nodes) could be related to extra-pulmonary manifestations of COVID-19.
Importantly, it has been postulated that a substantial percentage of patients infected with COVID-19 are asymptomatic with estimates ranging from 18% to 33% [9,10]. Even though human-to-human transmission occurs primarily through droplets generated by coughing and sneezing, transmission can also occur before onset of symptoms and via asymptomatic carriers. The droplets spread from the respiratory tract can travel up to 6 feet and remain viable on some surfaces for several days [2,11]. For this reason, worldwide public health measures such as quarantine, self-isolation, and social distancing in all populations, including those without symptoms, have been mandated in order to contain and slow the spread of disease.
The diagnosis of COVID-19 is currently made from nasopharyngeal or oropharyngeal swabs with RT-PCR, real‐time RT-PCR, and reverse transcription loop‐mediated isothermal amplification [12]. In early January 2020, the University of Washington virology department began developing an RT-PCR test for COVID-19. The Food and Drug Administration granted University of Washington emergency authorization for patient testing on February 29, 2020 [13,14]. Our patient was diagnosed with COVID-19 with this test the day after his FDG PET/CT was obtained in early April 2020.
Chest CT features with increased specificity for COVID-19 include bilateral, peripheral ground glass opacities with or without consolidation or intralobular septal thickening (“crazy paving”). Atypical findings include isolated consolidation without ground glass, discrete pulmonary nodules, lung cavitation, and smooth interlobular septal thickening with pleural effusion [15]. A few recent publications also describe the incidental detection of COVID-19 on routine staging FDG PET/CT. Like any infectious of inflammatory process, the areas of affected lung demonstrate increased FDG uptake. A recent article published in the Journal of Nuclear Medicine described 6 of 65 patients undoing routine FDG PET/CT who showed unexpected findings of pneumonia on the CT portion of the exam with corresponding areas FDG-uptake on PET. Of these 6 patients, 5 were diagnosed with COVID-19 by RT-PCR. All patients in this cohort were asymptomatic [16].
Currently, there are no validated anti-viral medications or other specific therapies targeted toward the treatment of COVID-19. Management of this disease is symptomatic and, more importantly, focused on public health measures which slow the spread of disease, an epidemiolocal concept referred to as “flattening the curve.” Without such measures such as quarantine, social distancing policies, and self-isolation, a large influx of new COVID-19 positive cases in a short amount of time would overwhelm the global healthcare system, exceeding the number of available hospital beds, healthcare staff, and/or mechanical ventilators. Consequently, there would be an exponential increase in the number of deaths both directly and indirectly related to COVID-19 [17]. Therefore, early recognition of patients with COVID-19 (radiologic or otherwise) is critical in order to isolate these cases and prevent additional infection.
References
- 1.Kooraki S, Hosseiny M, Myers L, Gholamrezanezhad A. Coronavirus (COVID-19) outbreak: what the department of radiology should know. J Am Coll Radiol. 2020;17(4):447–451. doi: 10.1016/j.jacr.2020.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Singhal T. A review of coronavirus disease-2019 (COVID-19) Indian J Pediatr. 2020;87(4):281–286. doi: 10.1007/s12098-020-03263-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Holshue ML, DeBolt C, Lindquist S, Lofy K, Wiesman J, Bruce H. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382(10):929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Coronvirus disease 2019 (COVID-19): cases, data, and surveillance. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/index.htmlAccessed June 10, 2020.
- 5.Thomas-Rüddel D, Winning J, Dickmann P, Ouart D, Kortgen A, Janssens U. Coronavirus disease 2019 (COVID-19): update for anesthesiologists and intensivists March 2020 [published online ahead of print, 2020 Mar 24] Anaesthesist. 2020:1–10. doi: 10.1007/s00101-020-00760-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wong S, Lui R, Sung J. "Covid-19 and the digestive system. J Gastroenterol Hepatol. 2020;35(5):744–748. doi: 10.1111/jgh.15047. [DOI] [PubMed] [Google Scholar]
- 7.Tang A, Tong ZD, Wang HL, Dai YX, Li KF, Liu JN. Detection of novel coronavirus by RT-PCR in stool specimen from asymptomatic child, China. Emerg Infect Dis. 2020;26 doi: 10.3201/eid2606.200301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhang W, Du RH, Li B, Zheng XS, Yang XL, Hu B. Molecular and serological investigation of 2019-nCoV infected patients: implication of multiple shedding routes. Emerg Microbes Infect. 2020;9:386–389. doi: 10.1080/22221751.2020.1729071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mizumoto K, Kagaya K, Zarebski A, Chowell G. Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the Diamond Princess cruise ship, Yokohama, Japan, 2020. Euro Surveill. 2020;25(10) doi: 10.2807/1560-7917.ES.2020.25.10.2000180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nishiura H, Kobayashi T, Suzuki A, S-Mok Jung, Hayashi K, Kinoshita R. Estimation of the asymptomatic ratio of novel coronavirus infections (COVID-19) Int J Infect Dis. 2020 doi: 10.1016/j.ijid.2020.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kampf G, Todt D, Pfaender S, Steinmann E. Persistence of coronaviruses on inanimate surfaces and its inactivation with biocidal agents. J Hosp Infect. 2020;104(3):246–251. doi: 10.1016/j.jhin.2020.06.001. pii: S0195–6701(20)30046–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhai P, Ding Y, Wu X, Long J, Zhong Y, Yiming L. The epidemiology, diagnosis and treatment of COVID-19. Int J Antimicrob Agents. 2020 doi: 10.1016/j.ijantimicag.2020.105955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mossa-Basha M, Medverd J, Linnau K, Lynch B, Wener K. Policies and guidelines for COVID-19 preparedness: experiences from the University of Washington. Radiology. 2020:201326. doi: 10.1148/radiol.2019201326. [DOI] [PubMed] [Google Scholar]
- 14.Green Sara. UW medicine gets green light to test for coronavirus. Seattle Times. 2020 www.seattletimes.com/seattle-news/health/with-seattle-on-the-front-lines-of-covid-19-epidemic-university-of-washington-lab-given-emergency-approval-to-test-for-coronavirus/ [Google Scholar]
- 15.Simpson S, Kay F, Abbara S, Bhalla S, Chung J, Chung M. Radiological society of north america expert consensus statement on reporting chest CT findings related to COVID-19. Endorsed by the Society of Thoracic Radiology, the American College of Radiology, and RSNA. Radiology. 2020;2(2) doi: 10.1097/RTI.0000000000000524. e200152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Albano D, Bertagna F, Bertoli M, Bosio G, Lucchini S, Motta F. Incidental findings suggestive of COVID-19 in asymptomatic patients undergoing nuclear medicine procedures in a high prevalence region. J Nucl Med. 2020;61(5):632–636. doi: 10.2967/jnumed.120.246256. [DOI] [PubMed] [Google Scholar]
- 17.Kakodkar P, Kaka N, Baig MN. A comprehensive literature review on the clinical presentation, and management of the pandemic coronavirus disease 2019 (COVID-19) Cureus. 2020;12(4):e7560. doi: 10.7759/cureus.7560. Published 2020 Apr 6. [DOI] [PMC free article] [PubMed] [Google Scholar]