Abstract
The COVID-19 pandemic is spreading at unprecedented pace among the Middle East and neighboring countries. This region is geographically, economically, politically, culturally and religiously a very sensitive area, which impose unique challenges for effective control of this epidemic. These challenges include compromised healthcare systems, prolonged regional conflicts and humanitarian crises, suboptimal levels of transparency and cooperation, and frequent religious gatherings. These factors are interrelated and collectively determine the response to the pandemic in this region. Here, we in-depth emphasize these challenges and take a glimpse of possible solutions towards mitigating the spread of COVID-19.
Keywords: COVID-19, Middle East, Challenges
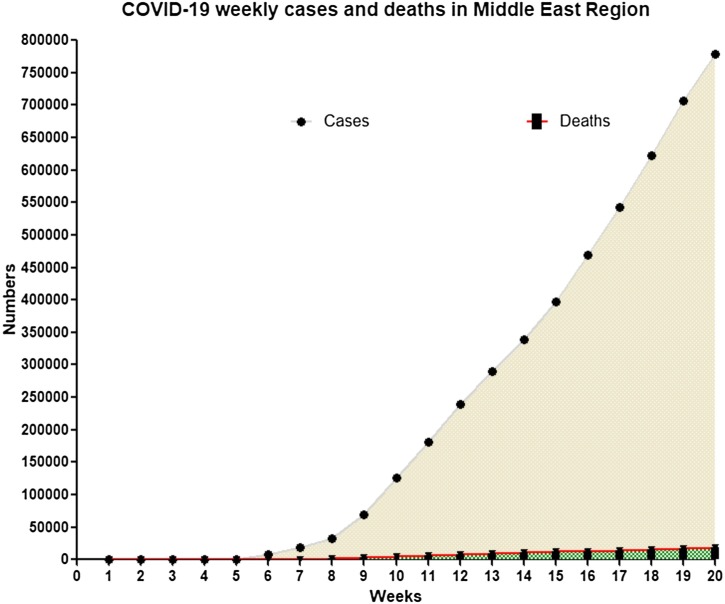
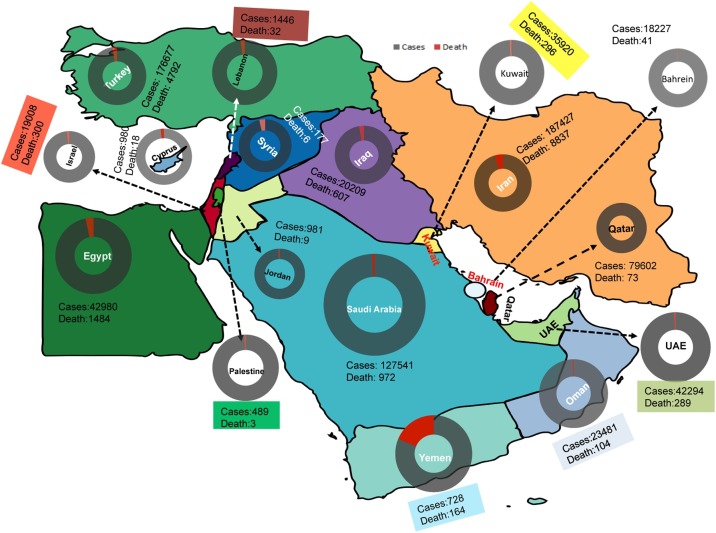
Having not forgotten the panic of the Middle East Respiratory Syndrome coronavirus (MERS-CoV), its new counterpart severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the causative agent of coronavirus disease 2019 (COVID-19), has landed in the Middle East. At June 14, 2020, there were 778,147 cases and 18,027 deaths of COVID-19 recorded across the Middle East. Although the case number was low cases in the early days of the outbreak, it has speeded at unprecedented pace later on and affecting all the Middle East countries (Fig. 1 ). This could reflect the levels of preparedness and response plans implemented locally in Middle East countries. The Middle East lies at the juncture of Eurasia and Africa, and constitutes an important pillar in shaping modern civilizations and religions. It is geographically, economically, politically, culturally and religiously a very sensitive area. Unfortunately, the whole region has been the center for wars and conflicts over the past years. These complexities have immense impact on breading, responding and mitigating epidemics [1]. Of note, Iran is the early epicenter with the highest number of confirmed COVID-19 cases and deaths in the Middle East region, followed by Turkey, Saudi Arab, Qatar and Egypt (Fig. 2 ). Given the rapid spread of COVID-19, we aim to emphasize the unique challenges of containing the epidemic in this region and to take a glimpse of possible solutions.
Fig. 1.
COVID-19 average weekly cases and deaths in Middle East Region.
Fig. 2.
Total number of confirmed COVID-19 cases and deaths from 29/01/2020 to 14/06/2020 in different countries of the Middle East region.
The imbalanced and weakened healthcare systems
Healthcare systems within the Middle East constitute a high degree of variability with regards to accessibility, capacity, and quality among different countries. The Persian Gulf region acquires significant wealth from the oil industry and has developed their healthcare systems [2]. Within these countries, there is a two-tiered healthcare system structure with public and private streams of financing and service delivery. WHO has highlighted the crucial role of early detection of COVID-19 cases to interrupt the spread, whereas the required expertise and diagnostic capacity could differ tremendously among different healthcare providers [3]. Thus, it is essential for the authorities to ensure equal and rapid access to diagnosis and treatment of COVID-19 regardless of nationalities, ethnicities, religions and beliefs.
The healthcare systems in non-oil-producing countries are largely underdeveloped and were further weakened due to prolonged conflicts and wars. Violent attacks on healthcare facilities and health workers during conflicts destroy essential health services that are most needed during the time [4]. The Syrian conflict has been marked by frequent and intense attacks against healthcare facilities [5]. The ongoing Yemen war has led to only 45% of the total healthcare facilities to be functional. A lesson learnt from the conflicts in the Democratic Republic of the Congo is that frequently attacking health care workers and Ebola treatment centers has gravely exacerbated the Ebola outbreaks [6].
The geopolitical context in Palestine results in limited freedom of movement and economic stability causing major challenges for healthcare system maintenance [7]. In Iran, although the healthcare system has been developed, economic sanctions jeopardize social determinants of health and access to medication and healthcare [8]. The rapid growing number of COVID-19 cases in Iran is threating the overwhelmed healthcare system but sanctions further limit the access to emergency medical supplies. Rapid and adequate access to healthcare is essential for controlling the epidemic but also for minimizing severe patient outcomes [9].
Risk of large epidemics in humanitarian crises
Besides weakening healthcare systems, wars and conflicts in the Middle East have also led to large-scale humanitarian crises. Because of the Syrian Civil War, 13.5 out of 22 million Syrian citizens require humanitarian assistance. Of these, five million have been placed in refugee camps established in Turkey, Lebanon, Jordan, Egypt and other countries [10]. The conditions in Yemen have continuously deteriorated since violence broke out in early 2015. Over four million people have been forced to flee their homes, and more than 80% of the population (24 million) is in need of humanitarian assistance [11]. Since 2016, Yemen has experienced a large-scale cholera epidemic, affecting more than 1.2 million cases and over 2500 deaths [12].
Emerging evidence indicates that SARS-CoV-2 is very contagious [13]. Conflicts-driven population migration will likely increase the risk of SARS-CoV-2 transmission. Human-to-human transmission mainly occurs via droplets or close contacts [14]. Thus the high population density in refugee camps and a lack of sanitation and hygiene are prone to widespread of the virus [15]. A subset of COVID-19 patients develop diarrhea and shed viruses into feces [16,17]. This has major implications pointing to possible fecal-oral transmission [18]. Thus, it is recommended to closely monitor whether this route of transmission may occur in refugee camps where have poor water, sanitation and hygiene services. Efforts must be made to minimize the risks of provoking large-scale COVID-19 epidemics in the settings of humanitarian crisis.
Levels of transparency, communication and cooperation
Recalling the important communication lessons from the previous SARS outbreak, transparent communication is key to an effective response to COVID-19 outbreak. Because of cultural, ethnical and religious differences, non-inclusive governments and humanitarian crises, the levels of transparent communication are clearly suboptimal in this region [19].
Two factors are of concern as obstacles for transparent communication and cooperation, including religion and ethnicity oriented diversification and conflicts. Several major religions have their own origins in the Middle East, including Judaism, Christianity and Islam. Arabs constitute the majority of ethnic population followed by Persian, Turk, Azeri’s, Kurds, Jews, Copts, Greek Cypriots, Assyrians and Iraqi Turkmen. These differences have primarily inflamed the instability and conflict of the region. Even within the Islamic countries, the conflict in Yemen between Saudi-backed Sunni and Iran-backed Shia sects has caused the most horrific humanitarian disaster in modern history. Moreover, the governments are also not transparent enough with their people because of the political and religious hierarchies and prioritization in the Middle East countries. In fact, SARS-CoV-2 does not discriminate nationalities, ethnicities and religions. Transparent communication and joint efforts are at the core of effective measures for controlling the ongoing COVID-19 epidemic.
Religious mass gatherings impose risk of super spreading events
Mass gatherings defined by WHO are planned or spontaneous events that gather substantial numbers of attendees, and these events are associated with major public health challenges [20]. This is particularly relevant to the potential superspreading of SARS-CoV-2. The outbreak in China coincided with a massive population movement, because of the Chinese Lunar New Year holiday [21]. A massive annual potluck banquet for 40,000 families held in Wuhan in the middle of January was suspected as an exacerbation of the outbreak in the epicenter. Analysis of nine gatherings for meal or holiday visit has indicated that superspreading events tend to occur during these close contacts [22]. During a religious gathering, a superspreader event that a Church attendee infected nearly 40 people has occurred in Korea and substantially triggered public panic.
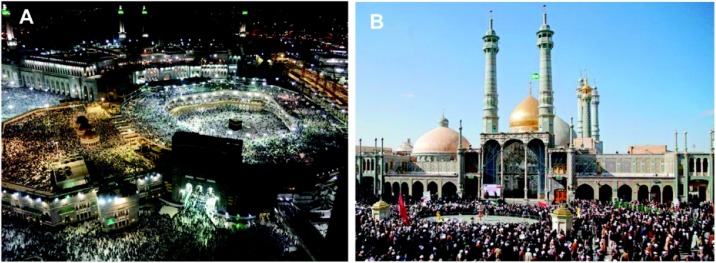
In Islam, there are the five-times-daily ritual prayers and a congregational prayer on every Friday in mosques, where large number of worshipers gathers. Of more concerns are the large-scale pilgrimages. Saudi Arabia continuously receives many millions of Umrah pilgrims and 2–3 million Hajj pilgrims at a special season of each year from over 180 countries (Fig. 3 A). Respiratory infections are the most common illness among pilgrims, and the associated mortality rate during Hajj has been reported as 2.4% [23]. In Iran, the early COVID-19 cases were recorded in Qom (Fig. 3B), a city that attracts millions of pilgrims from countries including Lebanon, Iraq, Bahrain, Yemen, Kuwait and Pakistan. Many of the initial COVID-19 cases in the Middle East and neighboring countries are related to the travel history to Qom or other cities of Iran, and most of them are pilgrims.
Fig. 3.
Mass gatherings in Islam. (A). Pilgrims at the Great Mosque of Mecca, in Saudi Arabia. The ritual of Tawaf walking seven times counterclockwise around the Kaaba, a building at the center of the Great Mosque of Mecca, is performed by all the Umrah and Hajj pilgrims. (B). the city Qom in Iran is considered holy by Shia Muslims. It attracts around twenty million pilgrims every year.
As pilgrims concentrating on religious rituals, there are close contacts among worshipers and insufficient self-protective measures, and therefore amplify the risk of transmission and potential super spreading of SARS-CoV-2 [24]. The governments of Saudi Arabia, Iran and Iraq are taking heavy measures on regulating the attendance of congregational prayers and pilgrimages to mitigate the risks. In this respect, we recommend the authorities to actively communicate with religion scholars and leaders of the religious communities to facilitate decision-making and policy implementation.
Conclusion
Facing the spread of COVID-19 in the Middle East, there are major challenges to contain this epidemic. These include compromised healthcare systems, prolonged regional conflicts and humanitarian crises, suboptimal levels of transparency and cooperation, and frequent religious gatherings. These factors are interrelated and collectively determine the response to the epidemic in this region. There is no simple solution, but to leverage the communication and cooperation between political leaders, healthcare authorities, religion scholars and the general public is certainly important. Immediate efforts should be dedicated to possibly lift economic sanctions and to end violence and conflict. For more effective response to the epidemic, we call to establish an independent and neutral international working group specifically dedicating to COVID-19, with particular focus on areas with conflicts and humanitarian crises. This new organization should work closely with all United Nations agencies, all the humanitarian organizations, and the local healthcare authorities with support of the international community. Finally, we shall unite and ensure commitment from all parties to contain the epidemic, as there are no physical or virtual borders for SARS-CoV-2 to cross.
Funding
The work was supported by the Ministry of Education of China for an Innovative Research Team in University grant (No. IRT_17R88; to Z.M.).
Competing interests
None declared.
Ethical approval
Not required.
References
- 1.Gele A.A., Bjune G.A. Armed conflicts have an impact on the spread of tuberculosis: the case of the Somali Regional State of Ethiopia. Confl Health. 2010;4:1. doi: 10.1186/1752-1505-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Parkash J., Younis M.Z., Ward W. Healthcare for the ageing populations of countries of Middle East and North Africa. Ageing Int. 2015;40:3–12. [Google Scholar]
- 3.Reusken C., Broberg E.K., Haagmans B. Laboratory readiness and response for novel coronavirus (2019-nCoV) in expert laboratories in 30 EU/EEA countries, January 2020. Euro Surveill. 2020;25 doi: 10.2807/1560-7917.ES.2020.25.6.2000082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Haar R.J., Risko C.B., Singh S., Rayes D., Albaik A., Alnajar M. Determining the scope of attacks on health in four governorates of Syria in 2016: results of a field surveillance program. PLoS Med. 2018;15 doi: 10.1371/journal.pmed.1002559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ri S., Blair A.H., Kim C.J., Haar R.J. Attacks on healthcare facilities as an indicator of violence against civilians in Syria: an exploratory analysis of open-source data. PLoS One. 2019;14 doi: 10.1371/journal.pone.0217905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wells C.R., Pandey A., Ndeffo Mbah M.L., Gaüzère B.A., Malvy D., Singer B.H. The exacerbation of Ebola outbreaks by conflict in the Democratic Republic of the Congo. Proc Natl Acad Sci U S A. 2019;116:24366–24372. doi: 10.1073/pnas.1913980116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nabaa H.A., Shelleh N. Barriers preventing Palestinian women from having a mammogram: a qualitative study. Lancet. 2018;391(Suppl 2):S16. doi: 10.1016/S0140-6736(18)30382-9. [DOI] [PubMed] [Google Scholar]
- 8.Aloosh M., Salavati A., Aloosh A. Economic sanctions threaten population health: the case of Iran. Public Health. 2019;169:10–13. doi: 10.1016/j.puhe.2019.01.006. [DOI] [PubMed] [Google Scholar]
- 9.Ji Y., Ma Z., Peppelenbosch M.P., Pan Q. Potential association between COVID-19 mortality and health-care resource availability. Lancet Glob Health. 2020;8:E480. doi: 10.1016/S2214-109X(20)30068-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.El Arnaout N., Rutherford S., Zreik T., Nabulsi D., Yassin N., Saleh S. Assessment of the health needs of Syrian refugees in Lebanon and Syria’s neighboring countries. Confl Health. 2019;13:31. doi: 10.1186/s13031-019-0211-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Al-Khateeb A.A. A call for urgent, organised medical missions in Yemen. Lancet. 2016;388:1877–1878. doi: 10.1016/S0140-6736(16)31805-0. [DOI] [PubMed] [Google Scholar]
- 12.Federspiel F., Ali M. The cholera outbreak in Yemen: lessons learned and way forward. BMC Public Health. 2018;18:1338. doi: 10.1186/s12889-018-6227-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen T.M., Rui J., Wang Q.P., Zhao Z.Y., Cui J.A., Yin L. A mathematical model for simulating the phase-based transmissibility of a novel coronavirus. Infect Dis Poverty. 2020;9:24. doi: 10.1186/s40249-020-00640-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li X., Zai J., Wang X., Li Y. Potential of large “first generation” human-to-human transmission of 2019-nCoV. J Med Virol. 2020;92:448–454. doi: 10.1002/jmv.25693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Peng X., Xu X., Li Y., Cheng L., Zhou X., Ren B. Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci. 2020;12:9. doi: 10.1038/s41368-020-0075-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guan W.J., Ni Z.Y., Hu Y., Liang W.H., Ou C.Q., He J.X. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Young B.E., Ong S.W.X., Kalimuddin S., Low J.G., Tan S.Y., Loh J. Epidemiologic features and clinical course of patients infected with SARS-CoV-2 in Singapore. JAMA. 2020;232(15):1488–1494. doi: 10.1001/jama.2020.3204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yeo C., Kaushal S., Yeo D. Enteric involvement of coronaviruses: is faecal-oral transmission of SARS-CoV-2 possible? Lancet Gastroenterol Hepatol. 2020;5:335–337. doi: 10.1016/S2468-1253(20)30048-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Batniji R., Khatib L., Cammett M., Sweet J., Basu S., Jamal A. Governance and health in the Arab world. Lancet. 2014;383:343–355. doi: 10.1016/S0140-6736(13)62185-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Memish Z.A., Steffen R., White P., Dar O., Azhar E., Sharma A. Mass gatherings medicine: public health issues arising from mass gathering religious and sporting events. Lancet. 2019;393:2073–2084. doi: 10.1016/S0140-6736(19)30501-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen S., Yang J., Yang W., Wang C., Barnighausen T. COVID-19 control in China during mass population movements at New Year. Lancet. 2020;395:764–766. doi: 10.1016/S0140-6736(20)30421-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu Y., Eggo R.M., Kucharski A.J. Secondary attack rate and superspreading events for SARS-CoV-2. Lancet. 2020;395 doi: 10.1016/S0140-6736(20)30462-1. S0140-6736(20)30462-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shirah B.H., Zafar S.H., Alferaidi O.A., Sabir A.M.M. Mass gathering medicine (Hajj Pilgrimage in Saudi Arabia): the clinical pattern of pneumonia among pilgrims during Hajj. J Infect Public Health. 2017;10:277–286. doi: 10.1016/j.jiph.2016.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ebrahim S.H., Memish Z.A. COVID-19: preparing for superspreader potential among Umrah pilgrims to Saudi Arabia. Lancet. 2020;395 doi: 10.1016/S0140-6736(20)30466-9. S0140-6736(20)30466-9. [DOI] [PMC free article] [PubMed] [Google Scholar]