Abstract
Introduction:
Adolescents require a range of scientifically accurate sexual and reproductive health information and services. Adolescent reproductive health services (ARHSs) are an integral part of adolescent health and it is pertinent that adolescents know about them to be able to benefit from them. This study was to assess the awareness and utilization of adolescents in Oyo State about ARHSs.
Materials and Methods:
A descriptive cross-sectional study carried out among in-school adolescents where 225 respondents each were selected for the rural and urban groups using a multi-stage sampling technique. Data were collected using a semi-structured questionnaire, and analysis was performed with SPSS version 22.
Results:
A total of 225 rural and 225 urban respondents participated in this study, with a mean age of 14.3 ± 1.93 and 13.9 ± 2.03 for rural and urban respondents, respectively. Few of the respondents (59, 13.1%) were aware of the existence of ARHS, of which, 34 (57.6%) were of the urban respondents and 25 (42.4%) were from the rural respondents. Only 36 (7.8%) of respondents had ever utilized ARHS with 22 (61.1%) from urban communities. The major reason why almost half of 207 (49.6%) of the adolescents had never been to a facility rendering ARHS before was that they did not know where to go, which was higher among the rural respondents.
Conclusions:
Awareness of ARHSs was lower among rural respondents, leading to poor utilization of such service. It is, therefore, recommended that more youth-friendly environments should be made available and accessible to adolescents, especially in rural areas (114, 53.3%).
Keywords: Adolescent, reproductive health, rural, urban
INTRODUCTION
Adolescents constitute about 20% of the world population.1 An estimate done in a study puts the adolescent's population globally at 1.2 billion with 85% of them living in the developing countries.2 According to the World Health Organization, adolescence is the period of transition from childhood to adulthood and this begins with the onset of puberty. Their age ranges between 10 and 19 years. During this period, the adolescent develops the secondary sexual features with further progression to reproductive and sexual maturity.1 Physical development is not the only form of development during adolescence; they also undergo emotional, psychological, and intellectual development.2
The risks of sexual abuse and other forms of sexual violence are high during adolescence. As a result of this, adolescents have special health needs and they require special reproductive health (RH) attention.3 This includes RH information; sexual abuse counseling, sexuality and reproduction; harmful reproductive health practices; human immunodeficiency virus (HIV) and AIDS; maternal health; sexually transmitted infections (STIs); gender issues; cervical/breast cancer and family planning services.3
Despite the large population of adolescents, their health needs have neither been well researched nor adequately addressed; their RH needs, especially are not well understood and are underestimated. Research shows that adolescents indulge in premarital sex more frequently at an early age,4,5 the incidence of pregnancies among them is rising,6 most of them face the risk of induced abortions under unsafe conditions7 and contracting STIs including HIV.8,9 Adolescents can protect themselves against sexually transmitted diseases and unwanted pregnancy when they have access to private and confidential services, they care for their RH and take advantage of other opportunities that will contribute to their lifelong well-being.10
The study of awareness, as well as utilization of adolescent reproductive health service (ARHS), among adolescents, is pertinent to the design and implementation of the necessary intervention in Nigeria. Studies have been carried out on RH service among adolescents in the urban area, but very few studies compared the awareness as well as the utilization of ARHS in both areas. Thus, this study is needed to provide information to policymakers, adolescent leaders and organizations to guide the development of effective, comprehensive sexuality intervention programs for rural and urban adolescents in Nigeria.
MATERIALS AND METHODS
The study was done in Oyo State. Oyo State is one of the states that make up the Federal Republic of Nigeria. There are 33 local government areas (LGAs) in the state and these local governments (LGs) are mainly divided into urban, semi-urban, and rural LGs. Oyo State has 325 general and private hospitals and 374 maternity clinics (108). Other important facilities include dispensaries, health centers, etc.
Study design
The study was a cross-sectional study, comparative in design, carried out in two rural and two urban LGAs in Oyo State, Nigeria, between March and June 2016.
Study population
The study population included adolescents aged 10–19 years attending public and private day secondary schools in urban and rural communities of Oyo State.
Inclusion criteria
Adolescents attending public and private day secondary schools in urban and rural communities in Oyo-State were included.
Exclusion criteria
Married in-school adolescents were exempted from this study.
Sample size calculation
The sample size was calculated using the formula for comparing two groups. The assumptions of 95% confidence level, 5% error margin, and 10% nonresponse rate were used to determine the sample size. Accordingly, 225 respondents each were chosen from rural and urban communities, making the total sample size of 450.
Sampling and data collection procedure
A multistage sampling technique was used.
First stage: Selection of local governments
Using the grouping of 33 LGAs in Oyo State into 12 rural, 9 semi-urban and 12 urban LGAs by the LG commission in Oyo State (based on population, Ibadan North East and Ogbomoso North LGs were the urban LG selected while the rural LG selected were Olorunsogo and Surulere LG using balloting technique.
Second stage: Selection of schools
All secondary schools in Oyo State were stratified into private and public secondary schools. The lists of all public and private secondary day schools in the selected four LGAs were obtained from the respective Local Government Inspectors of Education. Two public schools and two private schools were selected from the four LGAs using simple random sampling (simple balloting). The four rural schools were United Missionary Christian Association Model College (private), Orile-Igbon Community Secondary School (public), Zoe Secondary School (private) and Ogunbode Memorial Secondary School (public), while urban schools selected were Soun High School (public), Aduke Groups of Schools (private), Excellence Private School (private), and Army Barracks Secondary School (public). The number of respondents chosen from each school was proportionally selected by dividing the number of pupils in the school divided by the total number of students in the eight schools multiplied by the calculated sample size.
Third stage: Determination of desired sample size per school
The desired sample size was selected using stratified random sampling with the proportional allocation of students from the different classes in the selected secondary schools; stratification was done according to the classes (junior secondary school 1 to senior secondary school 3). Sixty respondents were proportionally allocated to the different arms of each of the selected schools. This was achieved by dividing the total number of students that are in the class by the total number in the school and multiplying it by the desired number of respondents in that school (60) as shown below:
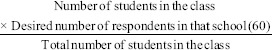
Number of respondents selected in each class in the selected schools.
Fourth stage: Selection of respondents
The respondents were chosen using systematic sampling technique (with the sampling fraction calculated based on the number of students present in the class and the number of respondents to be selected) with the aid of the teacher's class register. First, respondents from each class were selected by simple random technique using the class register, and subsequent respondents selected using sampling fraction (systematic sampling).
RESULTS
There were slightly more males (246, 54.7%) than females (204, 45.3%) [Table 1]. Most of the respondents were from the Yoruba ethnic group (413, 91.8%), and were Christians (330, 73.3%). The mean age of the urban respondents was 13.9 ± 2.03 years and that of the rural respondents was 14.3 ± 1.93 years. There were more of the middle age adolescents in rural areas and more of the early and middle adolescents in urban areas.
Table 1.
Sociodemographic profile of the respondents
| Sociodemographic characteristics | Frequency (%) |
Statistics | ||
|---|---|---|---|---|
| Rural (n=225) | Urban (n=225) | Total (n=450) | ||
| Age in groups (years) | ||||
| 10-13 | 76 (33.8) | 88 (39.1) | 164 (36.4) | t=2.44, df=2, P=0.302 |
| 14-17 | 144 (64.0) | 129 (57.3) | 273 (60.7) | |
| 18-19 | 5 (2.2) | 8 (3.6) | 13 (2.9) | |
| Mean age | 14.3±1.93 | 13.9±2.03 | 14.06±2.02 | |
| Class | ||||
| JSS 1-3 | 112 ( 49.8) | 113 (50.2) | 225 (50.0) | χ 2=0.009*, df=1, P=0.925 |
| SSS 1-3 | 113 (50.2) | 112 (49.8) | 225 (50.0) | |
| Gender | ||||
| Male | 131 (58.2) | 115 (51.1) | 246 (54.7) | χ 2=2.296, df=1, P=0.130 |
| Female | 94 (41.8) | 110 (48.9) | 204 (45.3) | |
| Religion | ||||
| Christianity | 166 (73.8) | 164 (72.9) | 330 (73.3) | χ 2=2.012, df=2, P=0.366 |
| Islam | 59 (26.2) | 59 (26.1) | 118 (26.2) | |
| Traditional | 0 (0.0) | 2 (100.0) | 2 (0.5) | |
| Ethnicity | ||||
| Yoruba | 204 (90.7) | 209 (92.9) | 413 (91.8) | χ 2=4.541, df=3, P=0.209 |
| Hausa/Fulani | 10 (4.4) | 3 (1.3) | 13 (1.3) | |
| Igbo | 6 (2.7) | 9 (4.0) | 9 (4.0) | |
| Others | 5 (2.2) | 4 (1.8) | 4 (1.8) | |
| Custodian | ||||
| Both parents | 173 (76.9) | 183 (81.3) | 356 (79.1) | χ2=1.349, df=2, P=1.349 |
| Single parent | 35 (15.6) | 28 (12.4) | 63 (14.0) | |
| Others | 17 (7.5) | 14 (6.3) | 31 (6.9) | |
*Statistically significant.JSS – Junior Secondary School; SSS – Senior Secondary School
Awareness of respondents about reproductive health services
A majority of the respondents, 200 (88.9%) [Table 2] of the rural and 191 (84.9%) of the urban were not aware of ARHSs, whereas 25 (11.1%) of the rural and 34 (15.1%) were aware. The mass media (radio and television) was the main source of information for 36 (42.6%) of the respondents, followed by parents, schools, then health professionals.
Table 2.
Respondents’ awareness and source of information about reproductive health services
| Frequency (%) |
Statistics | |||
|---|---|---|---|---|
| Rural (n=225) | Urban (n=225) | Total (n=450) | ||
| Awareness about ARHS | ||||
| Yes | 25 (11.1) | 34 (15.1) | 59 (13.1) | χ 2=1.580, df=1, P=0.209 |
| No | 200 (88.9) | 191 (84.9) | 391 (86.9) | |
| Total | 225 (100.0) | 225 (100.0) | 450 (100.0) | |
| Sources of information on ARHS** | ||||
| Mass media (television, radio) | 4 (16.0) | 9 (26.5) | 36 (42.6) | 0.338 |
| Parents | 10 (40.0) | 7 (20.6) | 17 (20.6) | 0.104 |
| School | 4 (16.0) | 10 (29.4) | 14 (23.7) | 0.231 |
| Friend | 3 (12.0) | 8 (23.5) | 11 (18.6) | 0.261 |
| Youth friendly club | 4 (16.0) | 6 (17.6) | 10 (16.9) | 0.868 |
| Internet*** | 1 (4.0) | 9 (26.5) | 10 (16.9) | 0.023* |
| Doctor/nurse | 7 (28.0) | 10 (29.4) | 17 (28.8) | 0.906 |
| Workshop | 4 (16.0) | 9 (26.5) | 13 (22.0) | 0.338 |
*Statistically significant, **Multiple responses allowed, ***Fischer exact. ARHS – Adolescent reproductive health service
Thirteen (52%) and 30 (88.2%) [Table 3] of the rural and urban respondents in both groups knew that counseling services are rendered in ARHS. This difference in their awareness on the type of services rendered in ARHS was statistically significant (P = 0.002). The difference in the knowledge of adolescents about RH was also statistically significant among the two groups (P = 0.035).
Table 3.
Respondents’ awareness about services rendered in an adolescent reproductive health facility
| Variables | Frequency (Percentage) |
χ2 | df | P | ||
|---|---|---|---|---|---|---|
| Rural (n=25) | Urban (n=34) | Total (n=59) | ||||
| Services rendered in ARHS**(n=59) | ||||||
| Counseling | 13 (52.0) | 30 (88.2) | 43 (72.9) | 9.571 | 1 | 0.002* |
| HIV testing | 14 (56.0) | 26 (76.5) | 40 (67.8) | 2.765 | 1 | 0.096 |
| Information on ARH | 10 (40.0) | 23 (69.6) | 33 (55.9) | 4.468 | 1 | 0.035* |
| Pregnancy test | 12 (48.0) | 21 (61.8) | 33 (55.9) | 1.107 | 1 | 0.293 |
| Recreation | 12 (48.0) | 20 (58.8) | 32 (54.2) | 0.680 | 1 | 0.410 |
| Breast examination | 14 (56.0) | 17 (50.0) | 31 (52.5) | 0.208 | 1 | 0.648 |
| STI treatment | 13 (52.0) | 18 (52.9) | 31 (52.5) | 0.005 | 1 | 0.943 |
| Treatment of common ailment | 10 (40.0) | 18 (52.9) | 28 (47.5) | 0.968 | 1 | 0.325 |
| Family planning | 8 (32.0) | 19 (55.9) | 27 (45.8) | 3.311 | 1 | 0.069 |
| Immunization | 8 (32.0) | 15 (44.1) | 23 (39.0) | 0.889 | 1 | 0.346 |
*Statistically Significant, **Multiple response allowed. ARH – Adolescent reproductive health; HIV – Human Immunodeficiency Virus; ARHS – Adolescent reproductive health service
Thirteen (5.8%) and 22 (9.8%) [Table 4] of rural and urban respondents had ever utilized ARHS while and 212 (94.6%) and 203 (90.2%) of rural and urban, respectively, had never been to ARHS. The difference between the utilization of ARHS of both groups was not statistically significant (P = 0.113).
Table 4.
Utilization of adolescent reproductive health service center
| Variables | Frequency (%) |
Statistics | ||
|---|---|---|---|---|
| Rural (n=225) | Urban (n=225) | Total (n=450) | ||
| Ever visited adolescent reproductive service centre | ||||
| Yes | 14 (5.8) | 22 (9.8) | 36 (7.8) | χ 2=2.509, df=1, P=0.113 |
| No | 211 (94.6) | 203 (90.2) | 414 (92.2) | |
The main reason given by rural respondents (114, 53.3%) and urban respondents (93, 45.8%) [Table 5] for not have accessed ARHS before was that they did not know where to go, which however was not statistically significant (P = 0.128). Furthermore, a greater proportion of urban respondents (76, 37.4%) chose that the reason why they had not been to a service center was that they do not need the service, the difference of which was statistically significant (P = 0.003).
Table 5.
Respondents reasons for not accessing reproductive health service
| Reasons for not utilizing service** | Frequency (Percentage) |
χ2 | Df | P | ||
|---|---|---|---|---|---|---|
| Rural (n=211) | Urban (n=203) | Total (n=414) | ||||
| I didn’t know where to go | 114 (53.3) | 93 (45.8) | 207 (49.6) | 2.318 | 1 | 0.128 |
| I do not need the service | 51 (23.8) | 76 (37.4) | 127 (30.5) | 9.106 | 1 | 0.003* |
| I don’t have money | 15 (7.0) | 10 (4.9) | 25 (6.0) | 0.802 | 1 | 0.370 |
| Clinic too far | 25 (11.7) | 20 (9.9) | 45 (10.8) | 0.362 | 1 | 0.547 |
| I don’t have the chance | 27 (12.6) | 23 (11.3) | 50 (12.0) | 0.163 | 1 | 0.686 |
| May et familiar face/staff | 17 (7.9) | 9 (4.4) | 26 (6.2) | 2.196 | 1 | 0.138 |
| My parent refused | 23 (10.7) | 20 (9.9) | 43 (10.3) | 0.090 | 1 | 0.764 |
| Time of service not convenient | 15 (7.0) | 10 (4.9) | 25 (6.0) | 0.802 | 1 | 0.370 |
| Fear of being seen by parent | 13 (6.1) | 10 (4.9) | 23 (5.5) | 0.276 | 1 | 0.599 |
| Embarrassed at needing service | 14 (6.5) | 8 (3.9) | 22 (5.3) | 0.410 | 1 | 0.235 |
| Provider may be judgmental | 3 (1.4) | 3 (1.5) | 6 (1.4) | 0.004 | 1 | 0.948 |
*Statistically significant. **Multiple responses allowed
More adolescents within the age range 14 and 7 had utilized adolescent health service at one time or the other and most were males. A majority of those who had utilized ARHS were Christians (22, 70.2%) and most of them live with their parents (24, 77.2%).
DISCUSSION
The utilization of adolescent RH is strongly determined by the level of awareness.11 In this study, the level of awareness about ARHS was very low; only about one-tenth of respondents were aware of ARHS. This low level of adolescents' awareness about RH service has been reported in Sri Lanka12 and also among secondary school students in a Nigerian study.13 However, it contradicts that found in Ghana, where adolescents have a high awareness of ARHS.14 This may be because adolescent health service is well structured in Ghana compared with the situation in Nigeria, where ARHS is still being advocated to be incorporated into the existing health services most of which are not yet actualized. Furthermore, unlike a study done by Paudel et al. in Nepal, where parents and the Internet were the main sources of ARHSs,15 the common source found out in this study was the mass media and health personnel. This was, however, consistent with studies done in Ethiopia16 and in another state in Nigeria,17 where health professionals and the mass media were the major source of information. Furthermore, more of the urban respondents got to know about ARHS, from the Internet compared with their rural counterparts. This difference may be a result of more accessibility of adolescents to internet services in the urban areas.
Furthermore, more of the urban respondents knew counseling and information on RH issue to be rendered in an ARHS center than the rural respondents, the difference of which was statistically significant. The difference could be linked with the exposure of the urban dwellers to both mass and social media. Exposure to most of these channels increases the knowledge of adolescents in various spheres of life, sexual and RH inclusive.3
Utilization of ARHS was found to be unsatisfactory in this study, as only about one-tenth of respondents had ever used RH services, two-third of which were from the urban area. This is corroborated with a similar study in Sri Lanka, where none of the adolescents had ever accessed an adolescent RH facility.12 This is, however, different from the study done in Ethiopia, where about four-fifth of respondents had utilized Family Planning and Voluntary Counseling and Testing services respectively before.18 A likely reason for this could be because issues that pertain to ARHS in Nigeria is still viewed as a myth or taboo. Young people are not expected to express their sexual needs openly. Therefore, they resort into keeping to themselves in issue that relates to their sexuality. This may, however, be to their disadvantage as they miss vital information and counseling about sexual and RH as a result of this.
More adolescents within the ages of 14–17 years utilized ARHS more than other age groups [Table 6]. This is in tandem with another study done in Ethopia19 This corroborates the fact that as adolescents advance in age, they become more explorative in relation to their development, RH issues inclusive.20 Furthermore, the younger age groups may feel they are too young to explore RH services; hence, the reason why most of them had never utilized any.
Table 6.
Association between socio-demographic characteristics of respondents and utilization of ARHS
| Variables | Utilization |
Statistics | ||
|---|---|---|---|---|
| Yes | No | Total | ||
| Age | ||||
| 10-13 | 5 (26.3) | 149 (32.9) | 164 (36.4) | χ 2=13.067, df=2, P=0.001 |
| 14-17 | 23 (57.9) | 240 (62.8) | 273 (60.7) | |
| 18-19 | 5 (15.8) | 5 (4.3) | 13 (3.9) | |
| Sex | ||||
| Male | 22 (73.7) | 204 (49.7) | 246 (54.7) | χ 2=11.772, df=1, P=0.001 |
| Female | 11 (26.8) | 189 (50.3) | 204 (45.3) | |
| Religion | ||||
| Islam | 10 (28.1) | 314 (27.5) | 330 (73.3) | χ 2=3.591, df=3, P=0.309 |
| Christianity | 22 (70.2) | 78 (71.9) | 118 (26.2) | |
| Traditional | 1 (1.8) | 1 (0.2) | 2 (0.5) | |
| Who respondent live with | ||||
| Both parents | 24 (77.2) | 312 (77.4) | 356 (77.4) | χ 2=0.040, df=2, P=0.980 |
| Single | 7 (15.8) | 54 (16.2) | 63 (16.2) | |
| Others | 2 (7.0) | 27 (6.4) | 31 (6.4) | |
ARHS – Adolescent reproductive health service
The major reason given by half of the respondents, with a higher proportion of adolescents from rural communities, for not using an ARHS facility was because they did not know where to go. This finding is consistent with the study done in the Southern part of Nigeria, about the adequacy of adolescent healthcare where it was found that the nonavailability of RH service facilities prevents youth from utilizing sexual and RH service.21 This actually is a pointer to the paucity of facilities that provide youth-friendly services in the rural areas of the country.
CONCLUSIONS AND RECOMMENDATIONS
This study shows that the level of awareness of adolescents about the existence of an ARHS was very low, with more adolescents from rural communities less aware compared to their urban counterparts. Furthermore, only a few respondents had been to an ARHS, most of which were from the urban communities and the major reason why most of the respondents had assessed ARHS before was that they did not know where to go. Therefore, it is recommended that awareness of the availability of ARHS services should be intensified among adolescents, especially in rural areas. Furthermore, adolescent RH should be incorporated into the school curriculum and hence that they can be exposed to safe and correct information as regards their RH at an early age. Furthermore, it is recommended that ARHS be incorporated into the existing health facility and an enabling environment should be provided for the adolescents to assess such without discrimination.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Aji J, Aji MO, Ifeadike CO, Emelumadu OF, Ubajaka C, Nwabueze SA, et al. Adolescent sexual behaviour and practices in Nigeria: A twelve year review. Afrimedic. 2013;4:10. [Google Scholar]
- 2.World Health Organization. Adolescent Health and Development. [Last accessed on 2017 July 12]. Available from: http://www.searo.who.int/en/section13/section1245_4980.htm .
- 3.Mmari K, Blum RW. Risk and protective factors that affect adolescent reproductive health in developing countries: A structured literature review. Glob Public Health. 2009;4:350–66. doi: 10.1080/17441690701664418. [DOI] [PubMed] [Google Scholar]
- 4.Chauhan S, Joshi B. Determinants of youth sexual behavior: Program implications for India. East J Med. 2011;16:113–21. [Google Scholar]
- 5.Baynesan F, Feldman B, Shtarkshall R. Trends of abortion rates among young Ethiopian immigrants in Israel aged 16-24 years during the period 1995-2005. Harefuah. 2011;150:175–9, 203. [PubMed] [Google Scholar]
- 6.Khanal P. Adolescents knowledge and perception of sexual and reproductive health and services-a study from Nepal. Int Perspect Sex Reprod Health. 2016;1:12–3. [Google Scholar]
- 7.Bendavid E, Avila P, Miller G. United States aid policy and induced abortion in sub-Saharan Africa. Bull World Health Organ. 2011;89:873–80C. doi: 10.2471/BLT.11.091660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.American Academy of Paediatrics. STI in Adolescents. Red Book Online. Available from: http://www.aapredbook.aappublications.org/cgi/content/full./2009/1/2.8.0 .
- 9.Center for Disease Control. Sexual Risk Behaviours, HIV, STD, and Teen Pregnancy Prevention. [Last accessed on 2017 Apr 06]. Available from: http://www.cdc.gov/healthyYouth/sexualbehaviours/
- 10.Kennedy EC, Bulu S, Harris J, Humphreys D, Malverus J, Gray NJ. Be kind to young people so they feel at home: A qualitative study of adolescents' and service providers' perceptions of youth-friendly sexual and reproductive health services in Vanuatu. BMC Health Serv Res. 2013;13:455. doi: 10.1186/1472-6963-13-455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Worku A, Abebe M. Utilization of youth reproductive health services and associated factors among high school students in Bahir Dar, Amhara regional state. Ethiopia. 2014;4:69–75. [Google Scholar]
- 12.Agampodi SB, Agampodi TC, Ukd P. Adolescents perception of reproductive health care services in Sri Lanka. BMC Health Serv Res. 2008;8:98. doi: 10.1186/1472-6963-8-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Olugbenga-Bello AI, Adebimpe OW, Abodunrin OL. Sexual risk behaviour among in-school adolescents in public secondary schools in a Southwestern City in Nigeria. Int J Health Res. 2009;2:243–52. [Google Scholar]
- 14.Jonathan MD, Afua A, Seth CW. Knowledge about sexual and reproductive health services and practice of what is known among Ghanaian youth, a mixed method approach. Adv Sex Med. 2016;6:1–13. [Google Scholar]
- 15.Paudel R, Upadhyaya T, Pahari DP. People's perspective on access to health care services in a rural district of Nepal. JNMA J Nepal Med Assoc. 2012;52:20–4. [PubMed] [Google Scholar]
- 16.Abajobir AA, Seme A. Reproductive health knowledge and services utilization among rural adolescents in East Gojjam zone, Ethiopia: A community-based cross-sectional study. BMC Health Serv Res. 2014;14:138. doi: 10.1186/1472-6963-14-138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Franklin A, Obafemi S, Olumide A, Oluwatosin O. Sexual and reproductive health knowledge and service utilization among in-school rural adolescents in Nigeria. J AIDS Clin Res. 2016;2:576. [Google Scholar]
- 18.Feleke SA, Koye DN, Demssie AF, Mengesha ZB. Reproductive health service utilization and associated factors among adolescents (15-19 years old) in Gondar town, Northwest Ethiopia. BMC Health Serv Res. 2013;13:294. doi: 10.1186/1472-6963-13-294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Binu W, Marama T, Gerbaba M, Sinaga M. Sexual and reproductive health services utilization and associated factors among secondary school students in Nekemte town, Ethiopia. Reprod Health. 2018;15:64. doi: 10.1186/s12978-018-0501-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hindin MJ, Fatusi AO. Adolescent sexual and reproductive health in developing countries: An overview of trends and interventions. Int Perspect Sex Reprod Health. 2009;35:58–62. doi: 10.1363/ipsrh.35.058.09. [DOI] [PubMed] [Google Scholar]
- 21.Ekong I. Adequacy of adolescent health care services available for adolescent girls in a Southern Nigerian environment. Int Res J Med Biomed Sci. 2016;1:23–8. [Google Scholar]


