Abstract
Background
Nausea and vomiting in pregnancy is usually called ‘morning sickness’. This is felt by sufferers to trivialise the condition. Symptoms have been described as occurring both before and after noon, but daily symptom patterns have not been clearly described and statistically modelled to enable the term ‘morning sickness’ to be accurately analysed.
Aim
To describe the daily variation in nausea and vomiting symptoms during early pregnancy in a group of sufferers.
Design and setting
A prospective cohort study of females recruited from 15 May 2014 to 17 February 2017 by Swiss Precision Diagnostics (SPD) Development Company Limited, which was researching hormone levels in early pregnancy and extended its study to include the description of pregnancy symptoms.
Method
Daily symptom diaries of nausea and vomiting were kept by females who were trying to conceive. They also provided daily urine samples, which when analysed enabled the date of ovulation to be determined. Data from 256 females who conceived during the first month of the study are included in this article. Daily symptom patterns and changes in daily patterns by week of pregnancy were modelled. Functional data analysis was used to produce estimated symptom probability functions.
Results
There was a peak probability of nausea in the morning, a lower but sustained probability of nausea throughout the day, and a slight peak in the evening. Vomiting had a defined peak incidence in the morning.
Conclusion
Referring to nausea and vomiting in pregnancy as simply ‘morning sickness’ is inaccurate, simplistic, and therefore unhelpful.
Keywords: cohort studies, early pregnancy symptoms, morning sickness, nausea and vomiting in pregnancy, pregnancy, pregnancy sickness
INTRODUCTION
Nausea and vomiting have been known to be early signs of pregnancy for several thousand years.1 The phrase ‘morning sickness’ has been in widespread use for around 200 years to describe nausea and vomiting.2 The use of the term is felt by many females, who have suffered from it, to trivialise the condition.3 This is especially felt by females who have experienced severe symptoms.3
Though nausea and vomiting in pregnancy (NVP) is now rarely life threatening, it can have a profound effect on the quality of females’ lives. Severe NVP can cause feelings of depression,4 difficulties between partners,4 less effective parenting,5 and concern for the health of the unborn child.4 Some females have such severe NVP that they are less likely to have another child,4 or they consider termination of subsequent pregnancies.6 In some females the condition is so intolerable, or poorly managed, that they actually elect to have a termination of the current pregnancy, even if it was very much wanted.6
The condition also has significant economic impact. It has been recently estimated that the annual costs of managing nausea and vomiting in pregnancy to the NHS in England and Wales are around GBP 62 million.7 There is also an economic impact through time lost in paid work by females suffering from the condition. In one study, around 35% of females in paid work lost time from the condition, causing an estimated loss of 8.6 million hours of paid work per year.8
Several studies have reported that females say that the symptoms of nausea and vomiting occur before and after noon,8 and in severe cases can go on throughout the waking hours,9 but the daily symptom patterns have not been clearly described. In spite of this the widespread use of the phrase ‘morning sickness’ persists.
In this article the authors have used a dataset of daily NVP symptom diaries kept by 256 females who were trying to conceive and were participating in a cohort study. The dataset also recorded demographic details of the females, their date of last menstrual period (LMP), date of ovulation, and daily human chorionic gonadotropin (hCG) urine levels.
Dating a pregnancy from the day of ovulation10 is a much more accurate way of describing the onset of pregnancy than the usual method of using the day of the LMP. Therefore, this study also uses time from the day of ovulation to date the onset of pregnancy.
In this study daily symptom patterns, as well as daily and weekly variation, have been modelled to provide a better understanding of the symptom patterns of NVP to further understand whether the term ‘morning sickness’ is valid.
METHOD
This prospective cohort study was conducted by Swiss Precision Diagnostics (SPD) Development Company Limited, a company that focuses on home diagnostic testing such as pregnancy testing, ovulation testing, and fertility monitoring under the Clearblue brand. The study was originally designed to investigate hormone levels in early pregnancy but was extended to include the study of pregnancy symptoms. Recruitment for the study was through advertising on the company’s website and the study was open for recruitment from 12 May 2014 to 25 November 2016. The first participant was recruited on 15 May 2014 and the final participant of the cohort reported here completed the study on 17 February 2017. Each participant was interviewed and only included in the study if they met the inclusion criteria: aged ≥18 years, seeking to become pregnant, and having regular menstrual periods. Exclusion criteria were medical conditions that contraindicate pregnancy, known infertility or having treatment for infertility, or females who were currently pregnant.
How this fits in
| Nausea and vomiting in pregnancy (NVP) is often termed ‘morning sickness’ but sufferers feel the term ‘morning sickness’ trivialises the condition. Though it has been previously reported that NVP symptoms can occur both before and after noon, the daily symptom pattern has not been well described. This study used statistical modelling to describe the weekly symptom pattern in a representative cohort of 256 females. Morning sickness does not adequately describe the symptom pattern and the term should no longer be used. |
Initially, 1443 females who were planning to become pregnant were recruited to the study. Of these females, 1073 did not achieve pregnancy in a 1-month period, and 82 females had pregnancy losses. Out of the remaining 288, who successfully conceived, 32 dropped out of the study. Hence, the study population includes 256 females.
Participants were recruited preconception, and began the study on day 1 of their next menstrual cycle. On enrolment to the study, participants provided their demographical and menstrual cycle information and previous pregnancy-related medical history. Throughout the study they provided information about their symptoms by completing a daily diary and also provided a daily urine sample, which provided hormone levels. Luteinising hormone (LH) was measured (AutoDELFIA, Perkin Elmer) in order to determine the day of LH surge, which precedes ovulation by approximately 1 day.11,12 Day of ovulation provides the most accurate method for determining pregnancy duration.13 hCG was measured (AutoDELFIA, Perkin Elmer) in late luteal phase and throughout early pregnancy in order to identify viable pregnancy and early pregnancy loss.
Females recorded whether they had experienced each of nausea and vomiting for each hour in the day in their symptom diaries. They started their pregnancy diaries once they had notified the researchers of a positive pregnancy test and were instructed to finish completing the diaries at day 60 of the pregnancy, measured from LMP (date of last menstrual period). If a female did not achieve pregnancy, they were instructed to collect urine samples and complete the symptom diaries only up to day 7 of their next cycle. Of the participants, 194 also responded to a follow-up questionnaire on the outcome of their pregnancy, including the sex and weight of their baby/babies, the type of delivery, and information about any complications during delivery.
Statistical methods
The anonymised dataset was transferred to the Department of Statistics at the University of Warwick and examined by the second and third authors using R Studio statistical software.
Daily symptom patterns and changes in daily patterns by week of pregnancy were modelled. Functional data analysis was used to produce estimated symptom probability functions using a Fourier basis system with 23 basis functions. The roughness penalty method was used to smooth discrete data with an integrated squared second derivative roughness penalty. After this, principle component analysis was used to investigate the main deviations of an individual’s symptom patterns from the mean pattern.14
RESULTS
The study population had a mean age of 30.4 years, which precisely corresponds to the mean age of mothers in England and Wales in 2016, according to the Office for National Statistics’ latest publication on the subject.15 The youngest participant was aged 18 years and the oldest 43 years.
The mean body mass index (BMI) of the whole study population was 27.02 kg/m2. Almost all (95%) of the females were white and 90% of them were European. The study population does not reflect a broad range of ethnicities or races.
There was a high level of education in the population, with 68% of females having an education level of A levels or higher (Table 1). More than half of the females (60%) had previously had children. One participant had already had seven live births. Almost half of the cohort had previously suffered ≥1 miscarriages. Before conceiving and during this study, the participants had been trying to conceive for a mean of 8.42 months, median 5 months (data not shown).
Table 1.
Demographic characteristics of female participants, N = 256
| Characteristics | Nausea symptom, n (%) |
|---|---|
| Age, years | |
| ≤25 | 35 (13.7) |
| 26–30 | 97 (37.9) |
| ≥31 | 124 (48.4) |
|
| |
| BMI,a kg/m2 | |
| ≤25 | 119 (46.7) |
| 26–30 | 63 (24.7) |
| ≥31 | 73 (28.6) |
|
| |
| Smoking status | |
| Previous and current | 100 (39.1) |
| Never | 156 (60.9) |
|
| |
| Live births, n | |
| 0 | 103 (40.2) |
| 1 | 105 (41.0) |
| >1 | 48 (18.8) |
|
| |
| Miscarriages, n | |
| 0 | 145 (56.6) |
| 1 | 68 (26.6) |
| >1 | 43 (16.8) |
|
| |
| Education level | |
| GCSE or no qualifications | 82 (32.0) |
| A levels | 65 (25.4) |
| Higher | 109 (42.6) |
For BMI, n = 255 as one result was missing. BMI = body mass index.
Symptom diaries
A total of 7584 daily diaries were completed with a mean of 30 diaries per participant. The mean start day of the diaries was day 30 of pregnancy measured from LMP and day 13 measured from ovulation. One-sixth (44, 17.2%) of the 256 participants stopped filling in diaries before day 60 from LMP. For the following analysis, start of pregnancy was measured from ovulation and not LMP as it is a more accurate measurement.7 Table 2 shows the number of participants who completed diaries in each week. Week 4 had the highest completion rate with 99.2% of participants. Weeks 2 to 7 are the only weeks in which symptoms could be reliably reviewed because weeks 1 and 8 had few participants. Recordings were only made up to week 8 of pregnancy from ovulation; therefore, only symptoms in early pregnancy were considered.
Table 2.
Proportion of completed symptom diaries in each week of pregnancy, dated from ovulation
| Week from ovulation | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| Participants, n | 2 | 195 | 249 | 254 | 242 | 225 | 141 | 7 |
| Proportion of sample population, % | 0.8 | 76.2 | 97.3 | 99.2 | 94.5 | 87.9 | 55.1 | 2.7 |
A participant was said to have symptoms if they had experienced at least 1 hour of nausea or vomiting during the days they completed diaries. Out of the 256 participants who completed diaries, 15 (5.9%) had no symptoms, 89 (34.8%) had nausea only, 150 (58.6%) had both symptoms, and 2 (0.8%) had only vomiting with no nausea. This brought the symptom prevalence to 94.2% of participants, much higher than found in previous studies (data not shown).
Participants who experienced nausea had symptoms a mean of 3.4 (median 2.7) hours per day, with 23% averaging ≤5 hours per day. Only 17 of the 152 (11.2%) females who experienced vomiting did so during >1 hour per day. The mean day of symptom onset was day 34 measured from LMP and day 18 from ovulation, which is in week 3 of pregnancy (measured from ovulation) (data not shown).
Daily symptom patterns
Despite the term ‘morning sickness’, data showed at least one participant experienced both nausea and vomiting in all hours of the day except between 23.00 hours and 24.00 hours for nausea, and 23.00 hours and 1.00 am for vomiting.
The most common hour for participants to experience nausea and vomiting was between 9.00 am and 10.00 am with 82% experiencing nausea in this hour, and 29% experiencing vomiting. In each hour of the day between 7.00 am and 10.00 pm, >60% of participants experienced nausea and >13% experienced vomiting. In general, vomiting is most common between the hours of 7.00 am and 1.00 pm but nausea is highly likely throughout the whole daytime, not just the morning. Though these statistics are not individual symptom patterns they show there is a very large proportion of females who have symptoms throughout the whole day (Figure 1).
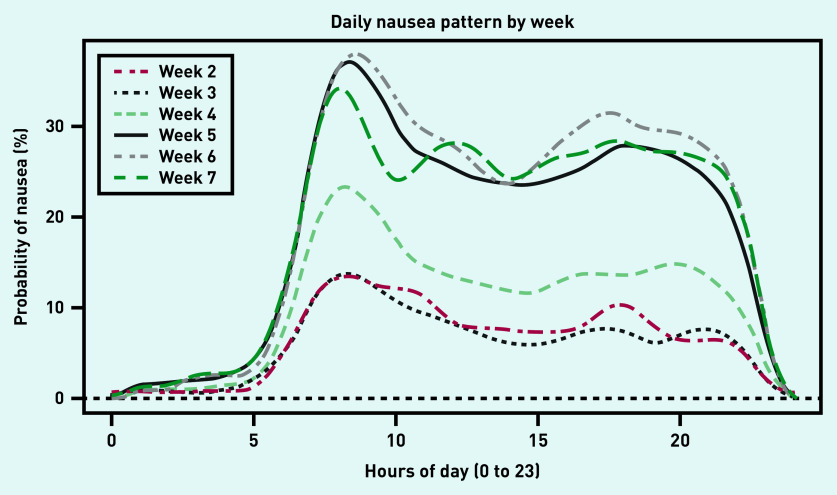
Figure 1.
Estimated probability functions for nausea by week of pregnancy (from ovulation).
In order to investigate daily pattern changes by week, the percentage of nausea and vomiting experienced for each hour of the day for each week was calculated for the participants collectively. Weeks 2 to 7 were considered in the calculation, as at least 141 females recorded a diary (Table 2). Data from all participants who completed diaries in each week were included. The probability functions shown in Figures 1 and 2 were estimated using functional data analysis. Figure 1 shows the estimated probability of nausea throughout the day for each week of pregnancy as measured from ovulation. There is a similar pattern in each week of pregnancy, with a peak of probability of nausea in the morning then a lower but sustained probability of nausea throughout the day with a slight peak in the evening.
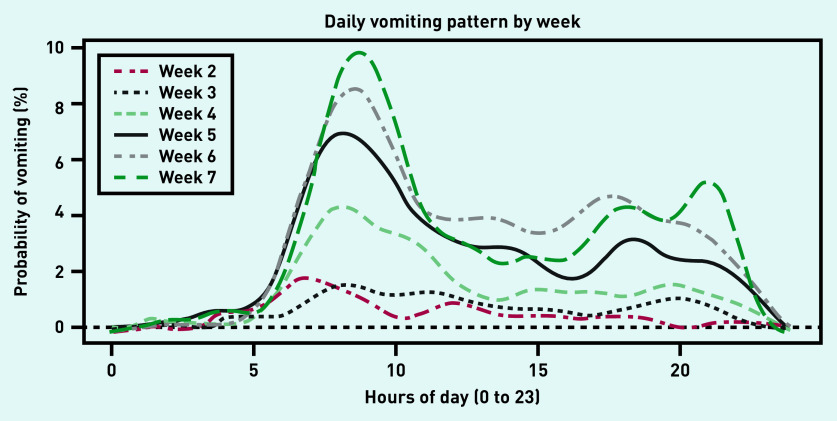
Figure 2.
Estimated probability functions for vomiting by week of pregnancy (from ovulation).
The general probability of nausea throughout the day is different between weeks of pregnancy. Weeks 2 and 3 have the lowest likelihood of nausea, with an increase in week 4, then weeks 5, 6, and 7 have the highest probability of nausea symptoms with similar patterns. Nausea was experienced at all hours in the daytime for all weeks, from 2 to 7, of pregnancy and not confined to the morning. There was a defined peak of probability of vomiting in the morning for each week (Figure 2). The later the week, the higher the probability of vomiting, with the highest probability in week 7, when about 10% of females vomited. Similar to the nausea patterns shown in Figure 1, there was still a sustained probability of vomiting throughout the day until the evening; however, for weeks 2 and 3 the probability of vomiting was very low. The rise in symptom probability in the morning is more defined for vomiting than nausea.
Nausea patterns at an individual level
Although Figure 1 represents the estimated probability of nausea for all participants collectively, it does not necessarily represent an individual participant. At an individual level the most common daily pattern was found to be similar to that of the collective pattern but with a much higher, for example, 50–60%, or lower (<10%) probability of nausea throughout the whole day. This accounted for 67.1% of variation. Some individuals also exhibited a pattern close to the collective pattern but with an increased or decreased probability of nausea in the morning. A small proportion of participants had a peak of symptoms in the middle of the day.
DISCUSSION
Summary
The authors gathered information from a well-described, representative cohort of females who have prospectively collected information on their NVP symptoms from the onset of pregnancy to describe their daily and weekly symptom patterns. For the first time in the literature they have used statistical modelling techniques to accurately describe the variations seen in these symptom patterns.
This article shows that it is not appropriate to call NVP ‘morning sickness’. Presented data describe the daily and weekly pattern of NVP from its early onset in detail. Findings clearly show nausea and vomiting symptoms can occur throughout the day. Vomiting mostly occurs in the mornings. Nausea, which many sufferers describe as the worst aspect of their symptoms,8 can occur throughout 24 hours. The continued use of the term ‘morning sickness’ could imply that symptoms only rarely occur in the afternoon and evening so that sufferers will have significant parts of the day symptom-free and so be able to do housework, paid work, and look after their families for the majority of any 24-hour period. This study shows that this is an incorrect assumption and that symptoms, particularly nausea, can occur at any time of the day.
Strengths and limitations
The strengths of the present study are that it is based on a sizeable cohort of females who are broadly representative of females becoming pregnant in the UK. Data on NVP symptoms were collected prospectively from the onset of pregnancy and the day of ovulation could be pinpointed through the measurement of the LH surge, so the pregnancy could be accurately dated. Statistical methodology has been used to accurately describe daily and weekly symptom patterns for the first time.
Some weaknesses of the study are that the dataset has an under-representation of females from lower socioeconomic (educational) backgrounds, and from black and minority ethnic backgrounds. It was assumed that days without diary entries were days without symptoms.
Females in the study stopped recording NVP symptoms at around week 9 of pregnancy when a number were still experiencing symptoms so that this dataset cannot be used to reliably describe NVP symptom cessation.
As participants were instructed to start collecting NVP data on day 30 following their LMP, there is some heterogeneity in start date relative to day of ovulation. As these results use true pregnancy duration from ovulation, week 4, for example, might be weeks 6 to 9 from LMP.
Comparison with existing literature
The present results confirm and amplify findings from other studies. In their 1993 article Gadsby and Barnie-Adshead report that 92.5% of females with NVP symptoms experienced them both before and after noon.8 In a review of the literature on NVP, a total of 13 articles covering 7904 females were found that describe some information about daily symptom patterns. All describe symptoms occurring both before and after midday.16
Implications for research and practice
The present study further reinforces the idea that calling NVP just ‘morning sickness’ is inaccurate, simplistic, and unhelpful. The authors wonder what further data would be required for the medical profession, media, and general public to stop using the term ‘morning sickness’ and for them to refer to the condition as ‘nausea and vomiting of pregnancy (NVP)' or ‘pregnancy sickness’.
There is a need for further research with patient involvement to confirm the most appropriate terminology to use in describing the condition to a lay audience.
Acknowledgments
The authors would like to thank all the women who took part in this study.
Funding
This study was funded by Swiss Precision Diagnostics (SPD) Development Company Limited. Sarah Johnson is an employee of SPD Development Company Limited, a fully owned subsidiary of SPD GmbH, Geneva; the manufacturer of Clearblue pregnancy and fertility tests (ClinicalTrials.gov trial registration number: NCT01577147).
Ethical approval
The study was approved by SPD Development Company Limited ethics committee on 9 April 2014 (Protocol-0400 Revision 8).
Provenance
Freely submitted; externally peer reviewed.
Competing interests
Sarah Johnson is an employee of SPD Development Company Limited. The other authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.Chadwick J, Mann WN. The medical works of Hippocrates. Oxford: Blackwell Scientific; 1950. [Google Scholar]
- 2.Merriam-Webster Morning sickness. https://www.merriam-webster.com/dictionary/morning%20sickness (accessed 22 Jun 2020).
- 3.Power Z, Thomson AM, Waterman H. Understanding the stigma of hyperemesis gravidarum: qualitative findings from an action research study. Birth. 2010;37(3):237–244. doi: 10.1111/j.1523-536X.2010.00411.x. [DOI] [PubMed] [Google Scholar]
- 4.Mazzotta P, Maltepe C, Navioz Y, et al. Attitudes, management and consequences of nausea and vomiting of pregnancy in the United States and Canada. Int J Gynecol Obstet. 2000;70(3):359–365. doi: 10.1016/s0020-7292(00)00255-1. [DOI] [PubMed] [Google Scholar]
- 5.Smith C, Crowther C, Beilby J, Dandeaux J. The impact of nausea and vomiting on women: a burden of early pregnancy. Aust NZ J Obstet Gynaecol. 2000;40(4):397–401. doi: 10.1111/j.1479-828x.2000.tb01167.x. [DOI] [PubMed] [Google Scholar]
- 6.Mazzotta P, Magee LA, Koren G. The association between abortion and nausea and vomiting of pregnancy. In: Koren G, Bishai R, editors. Nausea and vomiting of pregnancy: state of the art. Toronto: Mortherisk Programme, Hospital for Sick Children; 2000. [Google Scholar]
- 7.Gadsby R, Rawson V, Dziadulewicz E, et al. Nausea and vomiting of pregnancy and resource implications: the NVP Impact study. Br J Gen Pract. 2018 doi: 10.3399/bjgp18X700745. [DOI] [PMC free article] [PubMed]
- 8.Gadsby R, Barnie-Adshead AM, Jagger CA. Prospective study of nausea and vomiting during pregnancy. Br J Gen Pract. 1993;43(371):245–248. [PMC free article] [PubMed] [Google Scholar]
- 9.Gadsby R, Barnie-Adshead T. Severe nausea and vomiting of pregnancy: should it be treated with appropriate pharmacotherapy? Obstet Gynaecol. 2011;13(2):107–111. [Google Scholar]
- 10.Gnoth C, Johnson SR. Strips of hope: accuracy of home pregnancy kits and new developments. Geburtshilfe Frauenheilkd. 2014;74(7):661–669. doi: 10.1055/s-0034-1368589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Johnson S, Weddell S, Godbert S, et al. Development of the first urinary reproductive hormone ranges referenced to independently determined ovulation day. Clin Chem Lab Med. 2015;53(7):1099–1108. doi: 10.1515/cclm-2014-1087. [DOI] [PubMed] [Google Scholar]
- 12.Roos J, Johnson S, Weddell S, et al. Monitoring the menstrual cycle: comparison of urinary and serum reproductive hormones referenced to true ovulation. Eur J Contracept Reprod Health Care. 2015;20(6):438–450. doi: 10.3109/13625187.2015.1048331. [DOI] [PubMed] [Google Scholar]
- 13.Mahendru AA, Wilhem-Benartzi CS, Wilkinson IB, et al. Gestational length assignment based on last menstrual period, first trimester crown-rump length, ovulation, and implantation timing. Arch Gynecol Obstet. 2016;294(4):867–876. doi: 10.1007/s00404-016-4153-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ramsay JO, Hooker G, Graves S. Functional data analysis with R and MATLAB. New York: Springer-Verlag; 2009. [Google Scholar]
- 15.Office for National Statistics Births by parents’ characteristics in England and Wales: 2016–2017. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/livebirths/bulletins/birthsbyparentscharacteristicsinenglandandwales/2016 (accessed 22 Jun 2020).
- 16.Gadsby R, Barnie-Adshead AM. Nausea and vomiting of pregnancy. Clinical information about nausea and vomiting of pregnancy, its relation to various aspects of women's personal and obstetric histories and other significant factors related to nausea and vomiting of pregnancy or hyperemesis gravidarium. A literature review. 2012 https://www.pregnancysicknesssupport.org.uk/documents/NVP-lit-review.pdf (accessed 22 Jun 2020).