Abstract
Emerging adulthood has been described as a difficult stage in life and may be particularly stressful for Hispanic emerging adults who are disproportionately exposed to adversity and chronic sociocultural stressors. To better prevent and treat depressive disorders among Hispanic emerging adults, more research is needed to identify and understand modifiable determinants that can help this population enhance their capacity to offset and recover from adversity and sociocultural stressors. As such, this study aimed to (1) examine the association between resilience and depressive symptoms among Hispanic emerging adults, and (2) examine the extent to which intrapersonal resources (e.g., mindfulness, distress tolerance, emotion regulation strategies) and interpersonal resources (e.g., family cohesion, social support) moderate the association between resilience and depressive symptoms. To examine these aims, 200 Hispanic emerging adults (ages 18-25) from Arizona (n = 99) and Florida (n = 101) completed a cross-sectional survey, and data were analyzed using hierarchical multiple regression and moderation analyses. Findings from the hierarchical multiple regression indicate that higher resilience was associated with lower depressive symptoms. Findings from the moderation analyses indicate that family cohesion, social support, and emotion regulation strategies (e.g., cognitive reappraisal and expressive suppression) functioned as moderators; however, mindfulness and distress tolerance were not significant moderators. Findings from this study add to the limited literature on resilience among Hispanics that have used validated measures of resilience. Furthermore, we advance our understanding of who may benefit most from higher resilience based on levels of intrapersonal and interpersonal resources.
Keywords: reserve capacity, positive adaptation, intrapersonal resources, interpersonal resources, cognitive reappraisal
Introduction
Emerging adulthood is a developmental period that roughly spans the ages of 18-25 years and has been described as a stressful and difficult stage in life because individuals experience transitional life changes that involve striving to develop a personal identity, experiencing greater autonomy, often experiencing high levels of instability, and taking on new and challenging developmental tasks.1,2 Perhaps due to the numerous life changes that occur during this developmental period, emerging adults report a high prevalence of poor mental health. For instance, compared to adolescents and all other adult age groups, emerging adults in the United States (U.S.) report the highest prevalence of elevated depressive symptoms (13.1%).3 Given the present study’s focus on Hispanics, it should be noted that epidemiological surveillance indicates that Hispanics reported a higher prevalence of mild depressive symptoms (26.1%) in comparison to non-Hispanic Whites (21.5%), and a higher prevalence of moderate to severe depressive symptoms (9.4%) compared to non-Hispanic Whites (6.9%).4
One explanation for these ethnic differences in prevalence of depressive symptoms is that, in addition to normative developmental stressors associated with emerging adulthood, Hispanic emerging adults are disproportionately exposed to adversity and chronic sociocultural stressors such as financial hardship with limited upward economic mobility, ethnic discrimination, acculturation stress, and numerous immigration-related stressors that place them at a higher risk of experiencing depressive symptoms and developing a depressive disorder.5–9 Thus, more research is needed to identify and understand modifiable determinants that can help Hispanic emerging adults enhance their capacity to offset and recover from adversity and sociocultural stressors. In doing so, we can inform efforts to prevent and treat depressive disorders among this population. Building on the conceptual framework of the Reserve Capacity Model, in this study we aimed to examine the association between resilience and depressive symptoms among Hispanic emerging adults. To advance our understanding of how resilience may be enhanced by the potentiating influence of other malleable factors, our second aim was to examine the extent to which intrapersonal factors (e.g., mindfulness, distress tolerance, emotion regulation strategies) and interpersonal factors (e.g., family cohesion, social support) moderate the association between resilience and depressive symptoms.
Resilience has been described as the capacity to achieve positive adaptation despite threats to adaptation that include adversity and stressful experiences.10,11 Resilience is a construct relevant to mental health because several research studies have indicated that higher resilience is negatively associated with indicators of poor mental health (e.g., depressive symptoms) and positively associated with indicators of mental health well-being (e.g., positive affect, life satisfaction).12 Research suggests that resilience is protective against depressive symptoms/disorders because it affords individuals the ability to cope more effectively with stress, thus returning to physiological homeostasis, and in turn preventing or reducing symptoms of psychopathology.13,14 Although resilience is considered an important and modifiable construct that can be increased and targeted in prevention and treatment interventions for depression, resilience has been understudied among emerging adults despite their being at high-risk for developing depressive symptoms.13,15
Although there are several validated measures of resilience16, some studies on resilience do not include such measures and instead conceptualize resilience as the absence of pathology despite the presence or history of adversity or stressful events—this line of research often relies on “assets” or “resources” that are considered to be helpful in mitigating the effects of adversity and stressful events.17 Presently, a majority of resilience studies among Hispanics have applied this conceptualization of resilience and have treated cultural constructs such as ethnic identity, familism, and biculturalism as assets and resources.18–21 Studies among Hispanics that have assessed resilience directly with validated measures have been conducted with adolescent and general adult samples, and have found that higher resilience is associated with lower levels of depressive symptoms.22,23 To our knowledge, no prior studies have examined resilience among Hispanic emerging adults using validated measures of the construct. Using validated measures of resilience in research with Hispanics, regardless of age, is essential to advance our understanding of how we can enhance resilience and identify who may benefit most from higher resilience.
The Reserve Capacity Model is a conceptual framework that has been applied to health research with Hispanics and may help advance our understanding of factors that influence the effect of resilience on health and mental health outcomes.24 This framework is built on the premise that individuals from socially disadvantaged groups, including ethnic minorities, experience trauma and chronic stressors more frequently that increase the probability of developing poor health outcomes. However, the association between social disadvantage and poor health outcomes can be broken or weakened with the reserve capacities afforded by resilience. Lastly, this framework proposes that resilience can be enhanced by the presence of certain reserve capacity factors. These include: interpersonal resources (e.g., social support) and intrapersonal resources (e.g., psychological factors such as emotion regulation). In the present study, we examine how intrapersonal factors such as mindfulness, distress tolerance, emotion and regulation strategies, as well as interpersonal factors such as family cohesion and social support, may enhance the effect of resilience in reducing the occurrence or intensity of depressive symptoms. These intrapersonal and interpersonal resources are of particular interest because prior studies have demonstrated that these constructs can be modified with psychosocial interventions that target depressive symptoms.25–29
Mindfulness refers to receptive attention to and awareness of the present moment.30 Presently, research on mindfulness and its effects on resilience is limited; however, one study found that a mindfulness-based intervention increased resilience. The heightened awareness that comes with mindfulness helps individuals engage in more adaptive coping responses to stress and helps them recognize that a particular stressor may be temporary and will not be permanent or long-lasting.31 Research suggests that higher levels of mindfulness are also associated with lower depressive symptoms. Furthermore, mindfulness-based interventions have demonstrated to be efficacious in reducing symptoms of depression, including among Hispanics.27,32
Distress tolerance is the capacity to experience and withstand psychological discomfort such as negative affect and emotions, predisposing individuals with low distress tolerance to experience distress as being unbearable.33 To our knowledge, no prior study has examined the association between distress tolerance and resilience; however, we hypothesize that distress tolerance will enhance the effect of resilience on depressive symptoms. The reason for this hypothesis is that distress tolerance can help individuals actively and successfully cope with situations that are difficult or impossible to change.34 In addition, observational and clinical studies have found higher distress tolerance to be associated with lower levels of depressive symptoms.29
Emotion regulation can be broadly defined as the process to consciously modify one’s reaction to emotions.35,36 In the present study, we examine two strategies of emotion regulation—cognitive reappraisal and expressive suppression. Cognitive reappraisal is typically considered an adaptive emotion regulation strategy that entails reframing one’s thoughts about an event to change its emotional impact.37 Conversely, expressive suppression is typically considered as a maladaptive type of emotion regulation strategy that entails hiding, inhibiting or reducing the outward expression of emotion.38 Generally, cognitive reappraisal has been associated with lower depressive symptoms, whereas expressive suppression is associated with higher depressive symptoms, including among Hispanics.37–39 Research on emotion regulation and resilience suggests that cognitive reappraisal is associated with higher resilience because it may help individuals extract meaning, purpose, and/or strength from adversity or stressful events, and may prevent feeling overwhelmed.40,41 To our knowledge, expressive suppression has not been examined in relation to resilience; however, we hypothesize that it would be associated with lower resilience because prior studies have found that it is associated with less access to social support and adverse physiological responses such as sympathetic arousal and increased vasoconstriction.42,43
Family cohesion is the bond and connectedness that exists among family members.44 Although family cohesion has not been examined in studies that measure resilience directly, we hypothesize that it will enhance resilience because other studies with Hispanics consider familism, a value that emphasizes a strong family orientation, a valued asset within Hispanic cultures.18,45 Among Hispanics, higher family cohesion has been linked with lower depressive symptoms to some extent because it facilitates communication among family members and enhances adaptive family functioning.46,47
Social support is the degree to which members of an individual’s social network serve particular functions such as providing guidance or empathetic understanding.26 Researchers suggest that strong social support can enhance resilience because it increases the likelihood of using problem-focused coping strategies in response to stress.40 Research findings, including studies with Hispanics, have also indicated that stronger social support is associated with lower depressive symptoms because it functions as a buffer that mitigates the adverse effects of stress.26,48,49
Based on the review of the existing literature, the following two hypotheses were proposed. Hypothesis 1, higher levels of resilience will be associated with lower levels of depressive symptoms. Hypothesis 2, higher levels of social support, family cohesion, distress tolerance, cognitive reappraisal, and mindfulness will strengthen the favorable association of resilience on depressive symptoms. By contrast, higher levels of expressive suppression will weaken the association of resilience on depressive symptoms.
Methods
Procedure and Participants
The present analyses used data from a cross-sectional study with a sample of 200 participants from the Project on Health among Emerging Adult Latinos (Project HEAL). Prospective participants were recruited (1) in-person by distributing flyers, (2) by posting flyers with tear-off tabs, (3) through social media, and (4) by emailing an announcement that described the study aims and procedures to organizations and individuals who may have had access to the target sample. It should be noted that, at each study site, most participants who were not current college students were recruited in-person by research personnel with experience in recruiting Hispanic participants for research studies.
Prospective participants interested in the study contacted Project HEAL and a member of the research team screened prospective participants to determine whether they were eligible to enroll in the study. Inclusion criteria for participants included being ages 18 to 25, self-identifying as Hispanic or Latina/o, and currently living in Maricopa County, Arizona or Miami-Dade County, Florida. Participants provided informed consent to participate in the study by using an electronic informed consent form. Data were collected between August 2018 and February 2019 via a confidential online survey using Qualtrics. The survey took approximately 50 minutes to complete and participants were compensated with a $30 electronic Amazon gift card. This study was approved by the Florida International University Institutional Review Board.
Measures
Demographic Questionnaire.
The following sociodemographic variables were assessed in the survey and included in our analyses: age, gender, (0 = male, 1 = female), study site (0 = Florida, 1 = Arizona), partner status (0 = single, 1 = has a partner), nativity (0 = immigrant, 1 = non-immigrant), Hispanic heritage group (0 = non-Mexican heritage, 1 = Mexican heritage), student status (0 = current college student, 1 = not a college student), employment status (0 = unemployed, 1 = employed), and financial strain (1 = has more money than needed, 2 = just enough money for needs, 3 = not enough money to meet needs).
Depressive Symptoms.
Self-reported depressive symptoms were measured with the 10-item Center for Epidemiological Studies Depression Scale (CES-D).50 A sample item from this measure is, “I felt depressed.” Participants responded to items in the measure using a four-point Likert-type scale (0 = rarely or none of the time, 3 = most or all of the time). Higher sum scores are indicative of higher depressive symptomatology. In our sample, Cronbach’s reliability coefficient for the CES-D was α = .84.
Resilience.
Self-reported resilience was measured with the six-item Brief Resilience Scale.51 A sample item from this measure is, “I tend to bounce back quickly after hard times.” Participants responded to items using a five-point Likert-type scale (1 = strongly disagree, 5 = strongly agree) and higher mean scores are indicative of higher levels of resilience. Cronbach’s reliability coefficient for this measure was α = .76.
Mindfulness.
Self-reported mindfulness was measured with the five-item Mindful Attention Awareness Scale.30 A sample item from this measure is, “I find myself doing things without paying attention.” Participants responded to items using a six-point Likert-type scale (1 = almost always, 6 = almost never) and higher mean scores are indicative of higher levels of mindfulness. Cronbach’s reliability coefficient for this measure was α = .92.
Distress Tolerance.
Self-reported emotional distress tolerance was measured with the three-item Distress Tolerance Scale.33 A sample item from this measure is, “I can’t handle feeling distressed or upset.” Participants responded to items using a five-point Likert-type scale (1 = strongly agree, 5 = strongly disagree) and higher mean scores indicate higher levels of distress tolerance. Cronbach’s reliability coefficient for this measure was α = .83.
Emotion Regulation.
The Emotion Regulation Questionnaire was used to measure two strategies of emotion regulation—cognitive reappraisal and expressive suppression.35 A sample item from the six-item cognitive reappraisal subscale is, “I control my emotions by changing the way I think about the situation I’m in.” The expressive suppression subscale consists of four items and a sample item is, “I keep my emotions to myself.” Both subscales use a seven-point Likert-type scale (1 = strongly disagree, 7 = strongly agree). Higher mean scores indicate a higher degree of using each respective strategies of emotion regulation. Cronbach’s reliability coefficients for cognitive reappraisal and expressive suppression in this study were (α = .92) and (α = .84), respectively.
Family Cohesion.
Perceived family cohesion was measured with the corresponding six-item subscale of the Family Relations Scale.44 A sample item from this subscale is, “Family members feel very close to each other.” Participants responded to items using a four-point Likert-type scale (1 = not true at all, 4 = almost always or always true) and higher mean scores indicate higher levels of family cohesion. Cronbach’s reliability coefficient for this measure was α = .90.
Social Support.
Perceived emotional social support was measured with the corresponding four-item subscale of the Medical Outcomes Study Social Support Survey.52 A sample item from this subscale is, “Have someone to turn to for suggestions about how to deal with a personal problem.” Participants responded to items using a five-point Likert-type scale (1 = none of the time, 5 = all of the time) and higher mean scores indicate higher levels of social support. Cronbach’s reliability coefficient for this measure was α = .89.
Statistical Analysis Plan
All analyses were performed using SPSS v25. Descriptive statistics including means, standard deviations were generated for all continuous variables and frequencies and proportions were generated for all categorical variables. Bivariate correlations between study variables were assessed using Pearson correlation coefficients.
Simple main effects of the predictor variables on depressive symptoms were estimated using hierarchical multiple regression (HMR). Predictor variables were entered into the HMR model in a specified order so that each predictor contributed to the explanatory variance of the outcome variable (i.e., depressive symptoms) after controlling for the variance explained by the previous variables.53 Predictor variables were grouped and entered into the HMR model in the following order: (1) demographic variables were entered in the first block, (2) mindfulness, distress tolerance, emotion regulation strategies, family cohesion, and social support were entered in the second block, and (3) resilience was entered in the third and final block to determine the extent to which it uniquely predicted depressive symptoms above and beyond the other predictors.
Using PROCESS v3.2 for SPSS54, moderation analyses were conducted with 50,000 bootstraps to examine the extent to which potential moderating variables influenced the direction and/or strength of the association between resilience and depressive symptoms. PROCESS tested moderation by (1) performing a multiple regression to replicate the variance explained by all the predictor variables included in the HMR model, (2) estimating interaction terms between the focal predictor (e.g., resilience) and respective moderating variables (e.g., social support), and (3) estimating conditional effects for each respective interaction term in relation to depressive symptoms. All moderation analyses controlled for all other variables in the HMR model that were not included in respective interaction terms.
Results
Descriptive Analyses
The mean participant age was 21.30 (SD = 2.09) years and approximately half the sample was composed of women (n = 102, 51.0%) and participants from Arizona (n = 99, 49.5%). Regarding immigrant generations, the sample included first-generation immigrants (n = 60, 30.0%), second-generation individuals (n = 118, 59.0%), and the remainder were third-generation or later (n = 22, 11.0%). The sample also included participants from different Hispanic heritage groups that identified as Mexican (n = 88, 44.0%), Cuban (n = 33, 16.5%), Colombian (n = 24, 12.0%), non-Colombian South American (n = 21, 12.5%), and Central American (n = 20, 10.0%). Frequencies, proportions, means, and standard deviations for all study variables are presented in Table 1. Bivariate correlations for all study variables are presented in Table 2.
Table 1.
Descriptive Statistics for Study Variables (n = 200)
| Variable | |
|---|---|
| n (%) | |
| Gender | |
| Female | 102 (51.0) |
| Male | 98 (49.0) |
| Study Site | |
| Arizona | 99 (49.5) |
| Florida | 101 (50.5) |
| Nativity | |
| Immigrant | 60 (30.0) |
| Non-immigrant | 140 (70.0) |
| Hispanic Heritage | |
| Mexican | 88 (44.0) |
| Non-Mexican | 112 (56.0) |
| Partner Status | |
| Single | 142 (71.0) |
| Has Partner | 58 (29.0) |
| Student Status | |
| Current College Student | 139 (69.5) |
| Not a College Student | 61 (30.5) |
| Employment Status | |
| Employed | 157 (78.5) |
| Unemployed | 43 (21.5) |
| M (SD) | |
| Age | 21.30 (2.09) |
| Financial Strain | 2.30 (.60) |
| Social Support | 4.10 (.91) |
| Family Cohesion | 3.20 (.66) |
| Distress Tolerance | 2.89 (1.08) |
| Cognitive Reappraisal | 5.11 (1.30) |
| Expressive Suppression | 4.17 (1.50) |
| Mindfulness | 3.88 (1.21) |
| Resilience | 3.29 (.74) |
| Depressive Symptoms | 9.75 (6.40) |
Table 2.
Bivariate Correlations for Study Variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | Age | - | ||||||||||||||||
| 2. | Gender | −.05 | - | |||||||||||||||
| 3. | Study Site | .17* | .05 | - | ||||||||||||||
| 4. | Partner Status | .24** | .01 | .07 | - | |||||||||||||
| 5. | Nativity | .08 | .14* | .34** | −.01 | - | ||||||||||||
| 6. | Hispanic Heritage | .23** | .02 | .86** | .06 | .32** | - | |||||||||||
| 7. | Student Status | .30** | −.01 | .02 | .01 | −.11 | .01 | - | ||||||||||
| 8. | Employment Status | .27** | .05 | .40** | .09 | .16* | .37** | .24** | - | |||||||||
| 9. | Financial Strain | −.02 | .10 | .07 | .03 | .02 | .06 | −.19** | .02 | - | ||||||||
| 10. | Social Support | −.01 | .16* | −.03 | .08 | −.12 | .05 | .07 | .09 | −.09 | - | |||||||
| 11. | Family Cohesion | .01 | .05 | .04 | −.01 | −.11 | .02 | .10 | .04 | −.02 | .41** | - | ||||||
| 12. | Distress Tolerance | .05 | −.14 | .08 | .08 | −.14 | .10 | −.03 | −.09 | −.02 | −.02 | −.05 | - | |||||
| 13. | Reappraisal | −.02 | −.08 | −.01 | −.05 | .02 | −.02 | .04 | .02 | −.07 | .16* | .17* | .08 | - | ||||
| 14. | Suppression | .01 | −.17* | .18* | .01 | .02 | .15* | −.08 | .05 | .06 | −.17* | −.11 | .06 | .14 | - | |||
| 15. | Mindfulness | .13 | −.05 | −.10 | .05 | −.20** | −.05 | .34** | .03 | −.14* | .19** | .22** | .22** | .09 | −.12 | - | ||
| 16. | Resilience | .01 | −.18** | −.07 | .02 | −.13 | −.07 | .24** | .08 | −.21** | .19** | .17* | .13 | .21** | −.11 | .28** | - | |
| 17. | Depressive Symptoms | −.15* | .12 | .20** | −.04 | .25** | .18** | −.32** | −.04 | .19** | −.16* | −.21** | −.22** | −.27** | .25** | −.54** | −.44** | - |
p < .05,
p < .01
Hierarchical Multiple Regression
Table 3 presents the regression coefficients from the HMR model. Results indicate that 51.0% of the variance of depressive symptoms was explained by all the predictor variables entered into the HMR model. The first predictor block included demographic variables and explained 20.5% of variability in depressive symptoms, ΔR2 = 20.5, F(9, 190) = 5.44, p < .001. The second block added mindfulness, distress tolerance, emotion regulation strategies, family cohesion, and social support to the HMR model and corresponded with an R2 change of 27.2% [ΔR2 = 27.2, F(6, 184) = 15.94, p < .001]. The third and final block added resilience to the HMR model and corresponded with an R2 change of 3.3% [ΔR2 = 3.3, F(1, 183) = 12.21, p = .001]. Standardized coefficients from the final regression model indicate that distress tolerance (β = −.12, p = .04), cognitive reappraisal (β = −.20, p < .001), expressive suppression (β = .20, p < .001), mindfulness (β = −.34, p < .001), and resilience (β = −.21, p = .001) had statistically significant associations with depressive symptoms.
Table 3.
Hierarchical Multiple Regression Model Predicting Depressive Symptoms
| Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | b | SE | β | b | SE | β | b | SE | β |
| Block 1 | |||||||||
| Age | −.30 | .22 | −.10 | −.25 | .19 | −.08 | −.30 | .18 | −.10 |
| Gender | 1.00 | .84 | .08 | 1.02 | .72 | .08 | .54 | .71 | .04 |
| Study Site | 1.56 | 1.64 | .12 | .56 | 1.40 | .04 | .53 | 1.35 | .04 |
| Partner Status | −.33 | .94 | −.02 | −.09 | .79 | −.01 | −.02 | .76 | −.01 |
| Nativity | 2.22 | .98 | .16* | 1.31 | .84 | .09 | 1.26 | .82 | .09 |
| Hispanic Heritage | .83 | 1.63 | .07 | 1.48 | 1.37 | .12 | 1.37 | 1.33 | .11 |
| Student Status | −3.36 | 1.00 | −.24*** | −1.53 | .86 | −.11 | −1.08 | .85 | −.08 |
| Employment Status | −.88 | 1.15 | −.06 | −1.19 | .96 | −.08 | −.91 | .94 | −.06 |
| Financial Strain | 1.30 | .72 | .12 | .74 | .60 | .07 | .48 | .59 | .05 |
| Block 2 | |||||||||
| Social Support | .20 | .44 | .03 | .34 | .43 | .05 | |||
| Family Cohesion | −.65 | .59 | −.07 | −.53 | .58 | −.05 | |||
| Distress Tolerance | −.80 | .34 | −.13* | −.68 | .33 | −.12* | |||
| Cognitive Reappraisal | −1.14 | .28 | −.23*** | −.99 | .27 | −.20*** | |||
| Expressive Suppression | .93 | .24 | .22*** | .83 | .24 | .20*** | |||
| Mindfulness | −1.90 | .33 | −.36*** | −1.77 | .32 | −.34*** | |||
| Block 3 | |||||||||
| Resilience | −1.79 | .51 | −.21*** | ||||||
Note: b = unstandardized coefficient, SE = standard error, β = standardized coefficient,
p ≤ .05,
≤ .001
ΔR2 = 21.0 for Block 1, ΔR2 change = 26.9 for Block 2, ΔR2 change = 3.3 for Block 3.
Moderation Analyses
A moderation analysis indicated that cognitive reappraisal had a statistically significant interaction with resilience in relation to depressive symptoms (β = .10, p = .05). Conditional effects show that resilience had the strongest association with depressive symptoms at low levels (1 SD below the mean) of cognitive reappraisal (β = −.32, p < .001), followed by the mean level of cognitive reappraisal (β = −.24, p < .001). The conditional effect of resilience on depressive symptoms was not statistically significant at high levels (1 SD above the mean) of cognitive reappraisal. This moderating effect is depicted in Figure 1.
Figure 1.
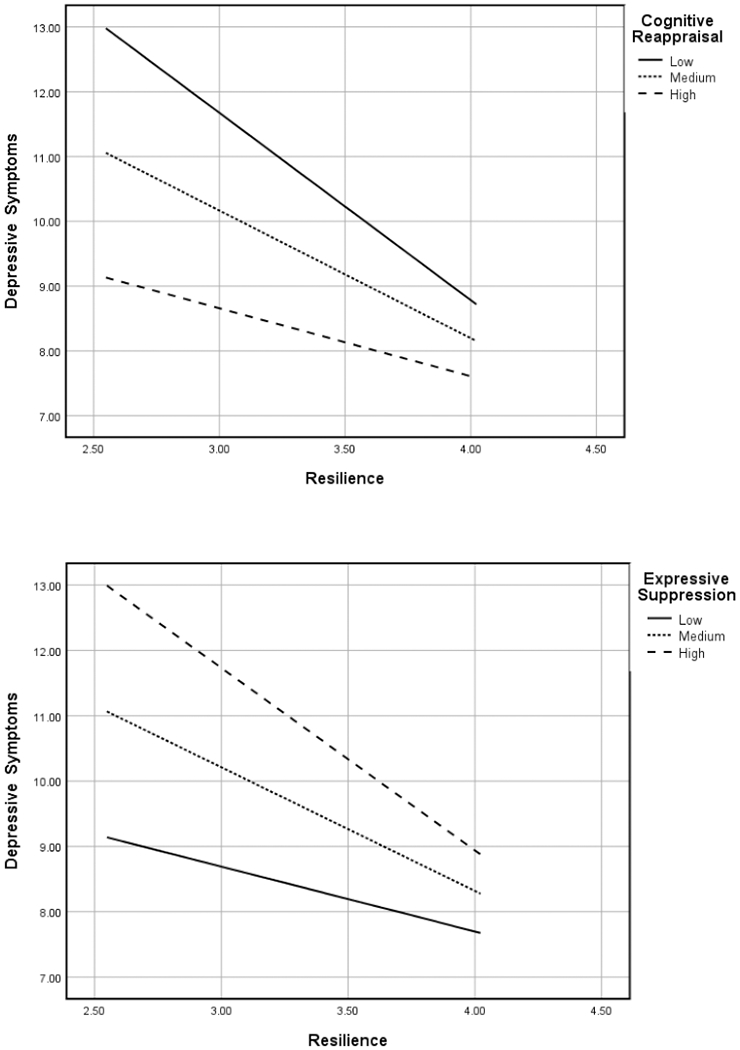
Two-way interactions with emotion regulation strategies, cognitive reappraisal and expressive suppression, moderating the association between resilience and depressive symptoms.
Expressive suppression also functioned as a moderator in the association between resilience and depressive symptoms (β = −.10, p = .03). Conditional effects indicate that resilience had the strongest association with depressive symptoms at high levels (1 SD above the mean) of expressive suppression (β = −.33, p < .001), followed by the mean level of expressive suppression (β = −.22, p < .001). The conditional effect at low levels (1 SD below the mean) of expressive suppression was not statistically significant. This moderating effect is depicted in Figure 1.
Another moderation analysis indicated that family cohesion moderated the association between resilience and depressive symptoms (β = .12, p = .05). Conditional effects show that resilience had the strongest association with depressive symptoms at low levels (1 SD below the mean) of family cohesion (β = −.35, p < .001), followed by the mean level of family cohesion (β = −.25, p < .001). The conditional effect of resilience on depressive symptoms was not statistically significant at high levels (1 SD above the mean) of family cohesion. This moderating effect is depicted in Figure 2.
Figure 2.
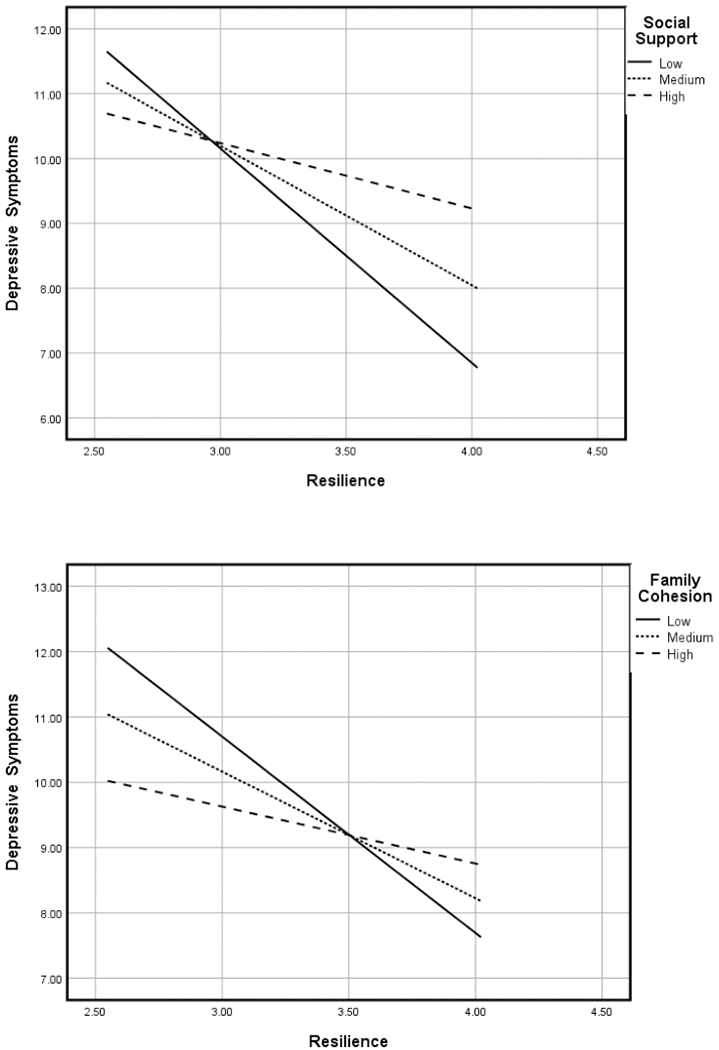
Two-way interactions with interpersonal resources, social support and family cohesion, moderating the association between resilience and depressive symptoms.
Social support also functioned as a moderator between resilience and depressive symptoms (β = .14, p = .02). Conditional effects indicate that resilience had the strongest association with depressive symptoms at low levels (1 SD below the mean) of social support (β = −.41, p < .001), followed by the mean level of social support (β = −.22, p < .001). The conditional effect at high levels (1 SD above the mean) of social support was not statistically significant. This moderating effect is depicted in Figure 2. Lastly, neither mindfulness nor distress tolerance moderated the association between resilience and depressive symptoms.
Discussion
Key findings from the current study can be summarized as follows. The data support our first hypothesis that higher levels of resilience would be associated with lower levels of depressive symptoms. We also found some partial support for our second hypothesis whereby cognitive reappraisal, expressive suppression, family cohesion, and social support moderated the association between resilience and depressive symptoms. However, neither mindfulness nor distress tolerance functioned as moderators.
As noted previously, emerging adulthood can be a difficult developmental stage in life that may be particularly challenging for Hispanic emerging adults. As such it is imperative to identify malleable and protective factors that can equip this population with the capacity to ameliorate the multitude of adverse circumstances and sociocultural stressors. Our study demonstrated that after controlling for key sociodemographic factors and well-established predictors of depressive symptoms, resilience was a key factor associated with lower depressive symptoms. This study adds to the limited literature on resilience among Hispanics that have used validated measures of resilience. Moving forward, rather than operationalizing resilience as the absence of psychopathology, future studies may be strengthened by assessing resilience directly with validated measures and examining if and how cultural resources (e.g., ethnic identity, biculturalism) important to Hispanics may aid in enhancing resilience.
Although familism is considered a pillar of Hispanic culture45, conditional effects indicate that resilience was associated with the steepest decline in depressive symptoms across participants at low levels of family cohesion. One explanation for this finding is that emerging adults may have or perceive lower family cohesion in comparison to adolescents because emerging adults typically experience more autonomy from their parents, might move out of their parent’s home or move to a different community, and consequently spend less time with their family.55 In addition, some literature suggests that emerging adulthood can be a time marked with higher family conflict, particularly among Hispanic emerging adults due to intergenerational cultural differences.56,57 Thus, the conditional effects in this study suggest that increasing levels of resilience may help individuals to compensate for low levels of family cohesion.
Our findings also suggest that resilience may help individuals counteract low levels of social support because resilience was associated with the sharpest decline in depressive symptoms across participants at low levels of social support. From a developmental standpoint, one key factor for this finding may be that it is not uncommon for emerging adults to experience insufficient social support to meet the developmental demands of emerging adulthood.58 One explanation for having or perceiving lower levels of social support is that it may be difficult for many emerging adults to maintain stable sources of social support from friends, family, and a romantic partner, due to developmental changes and transitions in roles and responsibilities that often occur during emerging adulthood.59,60
Expectedly, higher cognitive reappraisal was associated with lower depressive symptoms and thus was adaptive in minimizing the level of depressive symptoms. Conversely, higher expressive suppression was maladaptive, as it increased the level of depressive symptoms. As depicted in Figure 1, the conditional effect of resilience was most favorable at high levels of cognitive reappraisal. Although this condition had the lowest levels of depressive symptoms, this slope was not statistically significant because, as observed across cases, the rate of change in depressive symptoms across participants was low. By contrast, the worst condition was at low levels of cognitive reappraisal, although the slope for this conditional effect was statistically significant because it had the steepest decline in depressive symptoms across levels of resilience. Conversely, the conditional effect of resilience, shown in Figure 1, was most favorable at low levels of expressive suppression. This is expected because expressive suppression is typically considered a maladaptive strategy of emotion regulation. Although this condition had the lowest levels of depressive symptoms this slope was not statistically significant because the rate of change in depressive symptoms across participants was low. The worst condition was at high levels of expressive suppression, whereby the slope for this condition was statistically significant because it had the sharpest decline in depressive symptoms across increasing levels of resilience.
Although emerging adults have a broader and more flexible repertoire of strategies for emotion regulation when compared with adolescents—the capacity to effectively use adaptive emotion regulation strategies may not be fully developed in emerging adulthood.61 For instance, some research suggests that compared to individuals in middle adulthood, emerging adults are less likely to use cognitive reappraisal and more likely to use expressive suppression.61,62 Thus, our conditional effects suggest that higher resilience may help counteract the limited use of adaptive emotion regulation strategies (e.g., cognitive reappraisal), and the more frequent use of maladaptive emotion regulation strategies (e.g., expressive suppression).
Consistent with findings from other studies, higher mindfulness and higher distress tolerance were associated with lower depressive symptoms. Nonetheless, neither mindfulness nor distress tolerance moderated the association between resilience and depressive symptoms. Although the mindfulness measure used in the present study has sound psychometric properties it is a unidimensional measure of this construct and extant literature has described mindfulness as a multifaceted construct.63 Studies that have used multifaceted measures of mindfulness have found that all facets were associated with lower depressive symptoms64; however, few studies have examined mindfulness in relation to resilience and none have used multifaceted measures. Keeping this in mind, it may be the case that only certain facets of mindfulness may operate in interaction with resilience. With regard to distress tolerance, it has been suggested that it is beneficial to examine this construct in response to specific stimuli; thus, one explanation for the null interaction between distress tolerance and resilience may be that this interaction effect may only occur in relation to a specific event (e.g., experiencing ethnic discrimination) that would elicit psychological discomfort.65
The following limitations should be considered when interpreting the findings of this study. First, the present study utilized self-report measures that are susceptible to participant misrepresentation and error. Second, due to the cross-sectional design, the apparent or presumed temporal direction of effect or directional ordering of associations cannot be confirmed. Lastly, generalizability may be limited due to the non-probability sampling technique and sample size adequacy which limits the ability to detect subgroup variations attributable to nativity or different Hispanic heritage groups. Further, most participants were current college students and U.S.-born. Future studies should attempt to recruit more diverse samples that are more representative of the broader Hispanic population living in the United States.
Conclusions
Despite its limitations, the present study makes a meaningful contribution to the field of literature. First, this study is one of a few among Hispanics that used a validated measure of resilience to examine its association with depressive symptoms, and it may be the first to focus on Hispanic emerging adults. Second, the focus on emerging adults is significant because it brings attention to intrapersonal and interpersonal resources that are developing or in transition, yet interact with resilience during this stage of life. Related to this point, the present study lends support to the Reserve Capacity Model and helps advance our understanding of associations among intrapersonal resources, interpersonal resources, and resilience. For instance, we found that all the intrapersonal and interpersonal resources that were examined were correlated with resilience. In addition, we learned that intrapersonal resources such as adaptive emotion regulation strategies (e.g., cognitive reappraisal) and interpersonal resources (e.g., family cohesion and social support) may play key roles in strengthening the inverse association between resilience and depressive symptoms. Findings from our study may have implications for behavioral interventions because, as we continue to learn how to maximize the benefits of resilience, we can translate these findings to improve evidence-based interventions for preventing and reducing depressive symptoms among Hispanic emerging adults.
Acknowledgements:
Preparation of this article was supported by the National Institute on Alcohol Abuse and Alcoholism [K01 AA025992], the National Institute on Minority Health and Health Disparities [U54 MD002266], and the National Institute on Drug Abuse [R03 DA041891]. The authors would like to acknowledge Carlos Estrada, Diana Gutierrez, and Irma Beatriz Vega de Luna for their work in recruiting participants. The content is solely the responsibility of the authors and does not necessarily represent the official view of the National Institutes of Health.
Footnotes
Author Disclosures: All authors declare that they have no conflicts of interest and do not have any financial disclosures to report.
References
- 1.Arnett JJ. Emerging adulthood: A theory of development from the late teens through the twenties. Am Psychol. 2000;55(5):469–480. doi: 10.1037//0003-066X.55.5.469 [DOI] [PubMed] [Google Scholar]
- 2.Arnett JJ, Žukauskienė R, Sugimura K. The new life stage of emerging adulthood at ages 18–29 years: Implications for mental health. Lancet Psychiatry. 2014;1(7):569–576. doi: 10.1016/S2215-0366(14)00080-7 [DOI] [PubMed] [Google Scholar]
- 3.Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: Results from the 2017 National Survey on Drug Use and Health. www.samhsa.gov/data/report/2017-nsduh-annual-national-report. Updated September 12th, 2018 Accessed on November 25th, 2019.
- 4.Pratt LA. Brody DJ. Depression in the U.S. household population, 2009–2012. National Center for Health Statistics—Data Brief 172. www.cdc.gov/nchs/products/databriefs/db172.htm. Updated November 6th, 2015 Accessed November 25th, 2019.
- 5.Cano MA, Castillo LG, Castro Y, de Dios MA, Roncancio AM. Acculturative stress and depressive symptomatology among Mexican and Mexican American students in the U.S.: Examining associations with cultural incongruity and intragroup marginalization. Int J Adv Couns. 2014;36(2):136–149. doi: 10.1007/s10447-013-9196-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cano MA, de Dios MA, Castro Y, Vaughan EL, Castillo LG, Lorenzo-Blanco EI, et al. Alcohol use severity and depressive symptoms among late adolescent Hispanics: Testing associations of acculturation and enculturation in a bicultural transaction model. Addict Behav. 2015;49:78–82. doi: 10.1016/j.addbeh.2015.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.López M, Gonzalez-Barrera A, Krogstad JM. Latinos have become more pessimistic about their place in America. www.pewhispanic.org/2018/10/25/latinos-have-become-more-pessimistic-about-their-place-in-america. Updated October 25th, 2018 Accessed November 25th, 2019.
- 8.Reyes JA, Elias MJ. Fostering social–emotional resilience among Latino youth. Psychol Sch. 2011;48(7):723–737. doi: 10.1002/pits.20580 [DOI] [Google Scholar]
- 9.Shao Z, Richie WD, Bailey RK. Racial and ethnic disparity in major depressive disorder. J Racial Ethn Health Disparities. 2016;3(4):692–705. doi: 10.1007/s40615-015-0188-6 [DOI] [PubMed] [Google Scholar]
- 10.Luthar SS, Cicchetti D, Becker B. The construct of resilience: A critical evaluation and guidelines for future work. Child Dev. 2000;71(3):543–562. doi: 10.1111/1467-8624.00164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Masten AS. Ordinary magic: Resilience processes in development. Am Psychol. 2001;56(3):227–238. doi: 10.1037/0003-066X.56.3.227 [DOI] [PubMed] [Google Scholar]
- 12.Hu T, Zhang D, Wang J. A meta-analysis of the trait resilience and mental health. Pers Individ Differ. 2015;76:18–27. doi: 10.1016/j.paid.2014.11.039 [DOI] [Google Scholar]
- 13.Connor KM, Davidson JR. Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety. 2003;18(2):76–82. doi: 10.1002/da.10113 [DOI] [PubMed] [Google Scholar]
- 14.Feder A, Nestler EJ, Westphal M, Charney DS. Psychobiological mechanisms of resilience ad stress In: Reich JW, Zautra AJ, Hall JS, eds. Handbook of Adult Resilience. New York, NY: Guilford Press; 2010:35–54. [Google Scholar]
- 15.Luecken LJ, Gress JL. Early adversity and resilience in emerging adulthood In: Reich JW, Zautra AJ, Hall JS, eds. Handbook of Adult Resilience. New York, NY: Guilford Press; 2010:238–257. [Google Scholar]
- 16.Windle G, Bennett KM, Noyes J. A methodological review of resilience measurement scales. Health Qual Life Outcomes. 2011;9:8. doi: 10.1186/1477-7525-9-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Prince-Embury S Review of resilience conceptual and assessment issues In: Prince-Embury S, Saklofske DH, eds. Resilience Interventions for Youth in Diverse Populations. New York, NY: Springer; 2014:238–257. [Google Scholar]
- 18.Berger Cardoso J, Thompson SJ. Common themes of resilience among Latino immigrant families: A systematic review of the literature. Fam Soc. 2010;91(3):257–265. doi: 10.1606/1044-3894.4003 [DOI] [Google Scholar]
- 19.Delgado MY, Nair RL, Updegraff KA, Umaña-Taylor AJ. Discrimination, parent–adolescent conflict, and peer intimacy: Examining risk and resilience in Mexican-origin youths’ adjustment trajectories. Child Dev. 2019;90(3):894–910. doi: 10.1111/cdev.12969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Perreira KM, Marchante AN, Schwartz SJ, Isasi CR, Carnethon MR, Corliss HL, et al. Stress and resilience: Key correlates of mental health and substance use in the Hispanic Community Health Study of Latino Youth. J Immigr Minor Health. 2019;21(1):4–13. doi: 10.1007/s10903-018-0724-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Romero AJ, Edwards LM, Fryberg SA, Orduña M. Resilience to discrimination stress across ethnic identity stages of development. J Appl Soc Psychol. 2014;44(1):1–11. doi: 10.1111/jasp.12192 [DOI] [Google Scholar]
- 22.Kim SY, Hou Y, Gonzalez Y. Language brokering and depressive symptoms in Mexican-American adolescents: Parent–child alienation and resilience as moderators. Child Dev. 2017;88(3):867–881. doi: 10.1111/cdev.12620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Morote R, Hjemdal O, Uribe PM, Corveleyn J. Psychometric properties of the Resilience Scale for Adults (RSA) and its relationship with life-stress, anxiety and depression in a Hispanic Latin-American community sample. PloS One. 2017;12(11):e0187954. doi: 10.1371/journal.pone.0187954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gallo LC, Penedo FJ, Espinosa de los Monteros K, Arguelles W. Resiliency in the face of disadvantage: Do Hispanic cultural characteristics protect health outcomes? J Pers. 2009;77(6):1707–1746. doi: 10.1111/j.1467-6494.2009.00598.x [DOI] [PubMed] [Google Scholar]
- 25.Berking M, Ebert D, Cuijpers P, Hofmann SG. Emotion regulation skills training enhances the efficacy of inpatient cognitive behavioral therapy for major depressive disorder: A randomized controlled trial. Psychother Psychosom. 2013;82(4):234–245. doi: 10.1159/000348448 [DOI] [PubMed] [Google Scholar]
- 26.Cohen S Social relationships and health. Am Psychol. 2004;59(8):676–684. doi: 10.1037/0003-066X.59.8.676 [DOI] [PubMed] [Google Scholar]
- 27.Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. J Consult Clin Psychol. 2010;78(2):169–183. doi: 10.1037/a0018555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Perrino T, Pantin H, Huang S, Brincks A, Brown CH, Prado G. Reducing the risk of internalizing symptoms among high-risk Hispanic youth through a family intervention: A randomized controlled trial. Fam Process. 2016;55(1):91–106. 10.1111/famp.12132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Williams AD, Thompson J, Andrews G. The impact of psychological distress tolerance in the treatment of depression. Behav Res Ther. 2013;51:469–475. doi: 10.1016/j.brat.2013.05.005 [DOI] [PubMed] [Google Scholar]
- 30.Osman A, Lamis DA, Bagge CL, Freedenthal S, Barnes SM. The mindful attention awareness scale: Further examination of dimensionality, reliability, and concurrent validity estimates. J Pers Assess. 2016;98(2):189–199. doi: 10.1080/00223891.2015.1095761 [DOI] [PubMed] [Google Scholar]
- 31.Nila K, Holt DV, Ditzen B, Aguilar-Raab C. Mindfulness-based stress reduction (MBSR) enhances distress tolerance and resilience through changes in mindfulness. Ment Health Prev. 2016;4(1):36–41. doi: 10.1016/j.mhp.2016.01.001 [DOI] [Google Scholar]
- 32.Edwards M, Adams EM, Waldo M, Hadfield OD, Biegel GM. Effects of a mindfulness group on Latino adolescent students: Examining levels of perceived stress, mindfulness, self-compassion, and psychological symptoms. Journal for Specialists in Group Work. 2014;39(2):145–163. doi: 10.1080/01933922.2014.891683 [DOI] [Google Scholar]
- 33.Simons JS, Gaher RM. The distress tolerance scale: Development and validation of a self-report measure. Motiv Emot. 2005;29(2):83–102. doi: 10.1007/s11031-005-7955-3 [DOI] [Google Scholar]
- 34.McKay M, Wood JC, Brantley J. The Dialectical Behavior Therapy Skills Workbook: Practical DBT Exercises for Learning Mindfulness, Interpersonal Effectiveness, Emotion Regulation, and Distress Tolerance. Oakland, CA: New Harbinger Publications; 2007. [Google Scholar]
- 35.Gross JJ, John OP. Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. J Pers Soc Psychol. 2003;85:348–362. doi: 10.1037/0022-3514.85.2.348 [DOI] [PubMed] [Google Scholar]
- 36.Thompson RA. Emotion regulation: A theme in search of definition. Monogr Soc Res Child Dev. 1994;59(2–3):25–52. doi: 10.1111/j.1540-5834.1994.tb01276.x [DOI] [PubMed] [Google Scholar]
- 37.Troy AS, Shallcross AJ, Mauss IB. A person-by-situation approach to emotion regulation: Cognitive reappraisal can either help or hurt, depending on the context. Psychol Sci. 2013;24(12):2505–2514. doi: 10.1177/0956797613496434 [DOI] [PubMed] [Google Scholar]
- 38.Cutuli D Cognitive reappraisal and expressive suppression strategies role in the emotion regulation: an overview on their modulatory effects and neural correlates. Front Syst Neurosci. 2014;8:175. doi: 10.3389/fnsys.2014.00175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Juang LP, Moffitt U, Kim SY, Lee RM, Soto JA, Hurley E, et al. Cognitive reappraisal and expressive suppression: Links to racial-ethnic discrimination and adjustment among Latino/a and Asian-heritage college students. J Adolesc. 2016;53:21–33. doi: 10.1016/j.adolescence.2016.08.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Southwick SM, Charney DS. The science of resilience: Implications for the prevention and treatment of depression. Science. 2012;338:79–82. doi: 10.1126/science.1222942 [DOI] [PubMed] [Google Scholar]
- 41.Skodol A The resilient personality In: Reich JW, Zautr AJ, Hall JS, eds. Handbook of Adult Resilience. New York, NY: Guilford Press; 2010:112–125. [Google Scholar]
- 42.Butler EA, Egloff B, Wilhelm FH, Smith NC, Erickson EA, Gross JJ. The social consequences of expressive suppression. Emotion. 2003;3(1):48–67. doi: 10.1037/1528-3542.3.1.48 [DOI] [PubMed] [Google Scholar]
- 43.Peters BJ, Overall NC, Jamieson JP. Physiological and cognitive consequences of suppressing and expressing emotion in dyadic interactions. Int J Psychophysiol. 2014;9:100–107. doi: 10.1016/j.ijpsycho.2014.07.015 [DOI] [PubMed] [Google Scholar]
- 44.Tolan PH, Gorman-Smith D, Huesmann LR, Zelli A. Assessment of family relationship characteristics: A measure to explain risk for antisocial behavior and depression among urban youth. Pyschol Assess. 1997;9(3):212–223. doi: 10.1037/1040-3590.9.3.212 [DOI] [Google Scholar]
- 45.Knight GP, Mazza GL, Carlo G. Trajectories of familism values and the prosocial tendencies of Mexican American adolescents. Dev Psychol. 2018:54:378–384. doi: 10.1037/dev0000436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Baer J Is family cohesion a risk or protective factor during adolescent development? J Marriage Fam. 2002;64(3):668–675. doi: 10.1111/j.1741-3737.2002.00668.x [DOI] [Google Scholar]
- 47.Rivera FI, Guarnaccia PJ, Mulvaney-Day N, Lin JY, Torres M, Alegria M. Family cohesion and its relationship to psychological distress among Latino groups. Hisp J Behav Sci. 2008;30:357–378. doi: 10.1177/0739986308318713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cano MA, Sánchez M, Trepka MJ, Dillon FR, Sheehan DM, Rojas P, et al. Immigration stress and alcohol use severity among recently immigrated Hispanic adults: Examining moderating effects of gender, immigration status, and social support. J Clin Psychol. 2017;73(3):294–307. doi: 10.1002/jclp.22330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Held ML. Correlates of social support among Latino immigrants. J Racial Ethn Health Disparities. 2018;5:422–429. doi: 10.1007/s40615-017-0385-6 [DOI] [PubMed] [Google Scholar]
- 50.Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: Evaluation of a short form of the CES-D. Am J Prev Med. 1994;10(2):77–84. doi: 10.1016/S0749-3797(18)30622-6 [DOI] [PubMed] [Google Scholar]
- 51.Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, Bernard J. The brief resilience scale: Assessing the ability to bounce back. Int J Behav Med. 2008;15(3):194–200. doi: 10.1080/10705500802222972 [DOI] [PubMed] [Google Scholar]
- 52.Moser A, Stuck AE, Silliman RA, Ganz PA, Clough-Gorr KM. The eight-item modified Medical Outcomes Study Social Support Survey: Psychometric evaluation showed excellent performance. J Clin Epidemiol. 2012;65(10):1107–1116. doi: 10.1016/j.jclinepi.2012.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. 3rd ed. Mahwah, NJ: Lawrence Erlbaum Associates, Publishers; 2003. [Google Scholar]
- 54.Hayes AF. Introduction to mediation, moderation, and conditional analysis, second edition: A regression-based approach. New York, NY: The Guilford Press; 2017. [Google Scholar]
- 55.Whiteman SD, McHale SM, Crouter AC. Family relationships from adolescence to early adulthood: Changes in the family system following firstborns’ leaving home. J Res Adolesc. 2011;21(2):461–474. doi: 10.1111/j.1532-7795.2010.00683.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lee RM, Liu HT. Coping with intergenerational family conflict: Comparison of Asian American, Hispanic, and European American college students. J Couns Psychol. 2001;48(4):410–419. doi: 10.1037/0022-0167.48.4.410 [DOI] [Google Scholar]
- 57.Syed M, Mitchell LL. How race and ethnicity shape emerging adulthood In: Arnett JJ, ed. The Oxford Handbook of Emerging Adulthood. New York, NY, US: Oxford University Press; 2015:87.101. [Google Scholar]
- 58.Wang N Emerging adults’ received and desired support from parents: Evidence for optimal received–desired support matching and optimal support surpluses. J Soc Pers Relat. 2019;36(11–12):3448–3470. doi: 10.1177/0265407518822784 [DOI] [Google Scholar]
- 59.Lee CY, Goldstein SE. Loneliness, stress, and social support in young adulthood: Does the source of support matter? J Youth Adolesc. 2016;45(3):568–580. doi: 10.1007/s10964-015-0395-9 [DOI] [PubMed] [Google Scholar]
- 60.Pettit JW, Roberts RE, Lewinsohn PM, Seeley JR, Yaroslavsky I. Developmental relations between perceived social support and depressive symptoms through emerging adulthood: Blood is thicker than water. J Fam Psychol. 2011;25(1):127–136. doi: 10.1037/a0022320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zimmermann P, Iwanski A. Emotion regulation from early adolescence to emerging adulthood and middle adulthood: Age differences, gender differences, and emotion-specific developmental variations. Int J Behav Dev. 2014;38(2):182–194. doi: 10.1177/0165025413515405 [DOI] [Google Scholar]
- 62.John OP, Gross JJ. Healthy and unhealthy emotion regulation: Personality processes, individual differences, and life span development. J Pers. 2004;72:1301–1334. doi: 10.1111/j.1467-6494.2004.00298.x [DOI] [PubMed] [Google Scholar]
- 63.Baer RA, Smith GT, Lykins E, Button D, Krietemeyer J, Sauer S, et al. Construct validity of the Five Facet Mindfulness Questionnaire in meditating and nonmeditating samples. Assessment. 2008;15(3):329–342. doi: 10.1177/1073191107313003 [DOI] [PubMed] [Google Scholar]
- 64.Gu J, Strauss C, Crane C, Barnhofer T, Karl A, Cavanagh K, Kuyken W. Examining the factor structure of the 39-item and 15-item versions of the Five Facet Mindfulness Questionnaire before and after mindfulness-based cognitive therapy for people with recurrent depression. Psychol Assess. 2016;28(7):791–802. doi: 10.1037/pas0000263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Leyro TM, Zvolensky MJ, Bernstein A. Distress tolerance and psychopathological symptoms and disorders: A review of the empirical literature among adults. Pscyhol Bull. 2010;136(4):576–600. doi: 10.1037/a0019712 [DOI] [PMC free article] [PubMed] [Google Scholar]


