Abstract
In late 2019, cases of atypical pneumonia caused by a novel coronavirus called severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) were first reported in Wuhan, China. The disease was officially called coronavirus disease 2019 (COVID-19) and has been declared a pandemic disease by the World Health Organization (WHO). The clinical symptoms may include fever, cough, fatigue, headache, and diarrhea. The radiographic features comprise various presentations, including ground-glass opacities, tiny nodules, and consolidation. However, some atypical pathogens related to community-acquired pneumonia (CAP) may share similar presentations. They may be difficult to distinguish according to the clinical presentation and radiographic findings. Recently, there have been several reports reminding physicians to heed the possibility of co-infection with other pathogens in patients diagnosed with COVID-19. We report a COVID-19 patient co-infected with Mycoplasma pneumoniae who recovered well after combination therapy. We propose that all COVID-19 patients should undergo a meticulous screening routine to ensure that they receive adequate treatments.
In late 2019, several cases of atypical pneumonia were caused by a novel coronavirus called SARS-CoV-2, which was first reported in Wuhan, China. It later spread worldwide in the next few months. COVID-19 was declared a pandemic disease by the World Health Organization (WHO) on March 11, 2020 [1]. The clinical presentations of the disease are diverse and may be asymptomatic, mimic the common cold, involve severe pneumonia, or even deteriorate to acute respiratory distress syndrome (ARDS).
According to recent reports, the initial presentation includes fever, cough, fatigue, headache, and diarrhea [2,3].The radiographic features may also have a wide variety of presentations ranging from ground glass opacities to tiny nodules and consolidation [4]. However, the community-acquired pneumonia (CAP) caused by atypical pathogens may present similarly to COVID-19, and it may be challenging to distinguish them based on symptoms, signs, or radiographic findings. Recently, there have been several reports reminding physicians of the possibility of co-infection with other pathogens in patients with COVID-19 [5,6]. Thus, we report our experience with a COVID-19 patient co-infected with Mycoplasma pneumoniae.
Case presentation
A 61-year-old Taiwanese man presented to the emergency department on March 15th, 2020, with a 2-day history of dry cough and general malaise. The patient had a past history of hypertension, hepatitis B, and hearing impairment. He was afebrile at triage, and his vital signs were within normal limits. The physical examination was unremarkable. He reported a recent trip to Egypt from March 3rd to March 12th, 2020. Another person who went on the trip had tested positive for COVID-19.
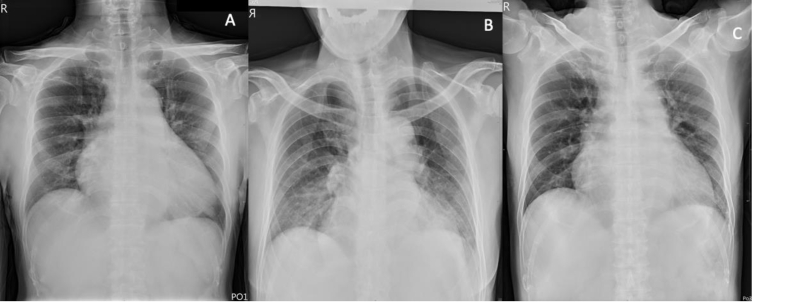
Chest radiography at presentation indicated mildly increased infiltrations in both lungs [Fig. 1A]. Routine laboratory and serology tests were performed, including influenza polymerase chain reaction (PCR), mycoplasma IgG, IgM, PCR and SARS-CoV-2 real-time polymerase chain reaction (RT-PCR) tests. Laboratory results showed only slightly elevated liver transaminases (AST: 80 U/L, ALT: 58 U/L). The RT-PCR results from his nasopharyngeal swab confirmed the presence of SARS-CoV-2. Moreover the mycoplasma IgM result was also positive (1054.4 U/mL) with an equivocal level of IgG (242.5 U/mL) and the mycoplasma PCR result was negative.
Fig. 1.
Chest radiographs on (A) day 2, (B) day 7, and (C) day 14 after the onset of symptoms.
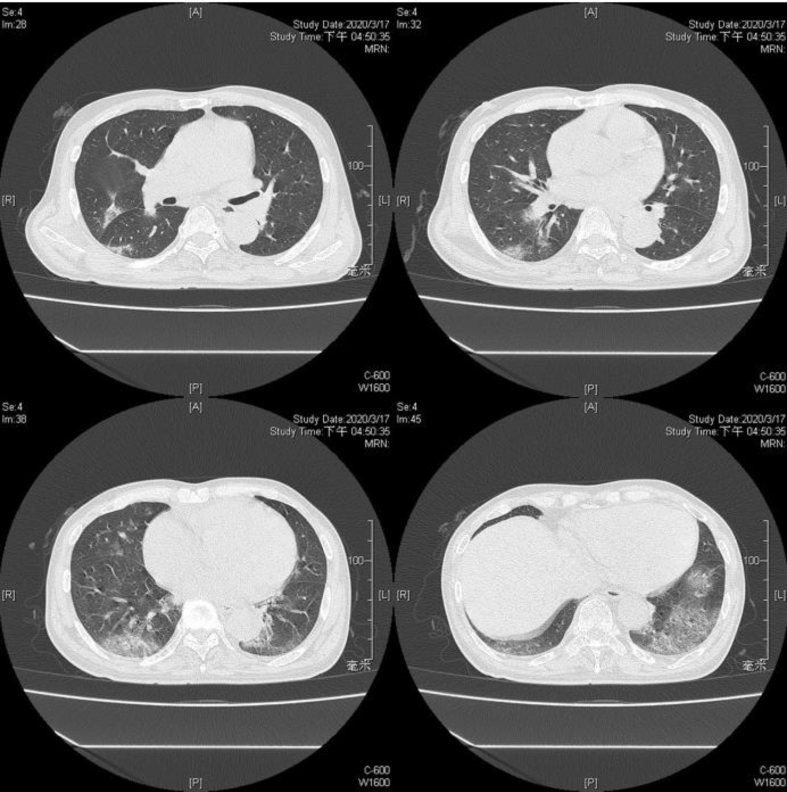
During hospitalization, the patient received standard therapy. A fever of up to 38.2 °C developed on day 3 after the onset of symptoms and subsided one day later. At the same time, the patient also experienced diarrhea and respiratory distress, which required the use of an oxygen cannula. Chest radiography showed the progression of bilateral ground-glass patches [Fig. 1B]. High-resolution computed tomography (HRCT) was ordered on day 5, which revealed multiple patches of ground-glass opacity, crazy-paving pattern, and peribronchial consolidation on the right upper lobe, middle lobe, and bilateral lower lobes [Fig. 2].
Fig. 2.
HRCT on day 5 after the onset of symptoms.
Azithromycin at 500 mg QD was prescribed for three days along with hydroxychloroquine at 200 mg Q8H for a total of eight days. No adverse event was observed after the therapy. The patient's clinical condition and chest plain film both improved [Fig. 1C]. In follow-up examinations, mycoplasma IgM and IgG levels returned to the normal range (471.3 and 154.1 U/mL, respectively) on March 30th, and the RT-PCR result of a nasopharyngeal swab was negative for SARS-CoV-2 on April 8th.
Discussion
COVID-19 has become a global pandemic in 2020, with confirmed cases and mortalities increasing each day around the world [1,7]. Mysycoplasma pneumoniae accounts for 10–40% of CAP, which predominantly affects children more than 4 years old and adolescents. However, the prevalence may be underestimated in adults and the elderly [8]. The exact number of cases of concomitant infection of COVID-19 and M. pneumoniae is not yet known. The positive RT-PCR results confirmed the diagnosis of COVID-19, and the rise and fall of mycoplasma IgM titers in our patient suggested an acute phase with M. pnumoniae infection. Patients with COVID-19 can present a wide variety of non-specific symptoms that are common for viral infections. Life-threatening complications may develop, including septic shock and ARDS, especially in individuals with comorbidities and the elderly [3]. Because of the ongoing nature of the COVID-19 outbreak, the number of mortalities varies from country to country. Although mycoplasma pneumonia is presumably benign in nature, its presentation may also range from mild viral-infection-like symptoms to life-threatening conditions, including ARDS and multiple organ failure. A study on patients with mycoplasma infections identified 416 patients, of which 68 (16.3%) required admission to the intensive care unit (ICU), and the ICU mortality rate was 29.4% [8].
In terms of image findings, the most common features in chest radiographs of COVID-19 pneumonia include ground-glass opacities, bilateral or local patchy shadowing, and interstitial abnormalities [3,9]. In chest radiographs of mycoplasma pneumonia, the most common patterns are peribronchial and perivascular interstitial infiltrates, airspace consolidation, and nodular opacification [10,11]. In HRCT, the most common features reported for COVID-19 pneumonia are bilateral and subpleural areas of ground-glass opacification, consolidation affecting the lower lobes, or both [4,[12], [13], [14]].
One study analyzed the HRCT patterns in 28 patients with mycoplasma pneumonia, and the most common patterns were ground glass attenuation (86%) and airspace consolidation (79%) [10].Thus, based on the current findings and previous reports, it may be difficult to distinguish between the two diseases using chest radiographs and HRCT. Indeed, the HRCT of our patient exhibited features resembling both COVID-19 and mycoplasma pneumonia.
Currently, there is no standard therapy for COVID-19 infected patients and supportive care remains the mainstay of treatment. Meanwhile, macrolides such as azithromycin are considered the drugs of choice for non-macrolide-resistant M. pneumoniae due to their efficacy, and they are generally well tolerated [15]. The importance of early administration of effective antibiotics for patients with mycoplasma pneumonia has been demonstrated in a study which reported that patients required admission to ICUs for acute respiratory failure did not receive appropriate antibiotics until approximately 10 days after diagnosis [16]. Our patient received Azithromycin therapy when mycoplasma pneumonia was diagnosed with good response.
Conclusion
Patients with mycoplasma pneumonia and COVID-19 pneumonia may have similar presentations in clinical and radiographic features. With the continuing increase in the number of COVID cases, the presence of mycoplasma coinfection could be easily overlooked. We have reported a patient who presented with non-specific symptoms, including general malaise and dry cough, and there was no lymphopenia. Further testing confirmed the co-infection with SARS-CoV-2 and M. pneumoniae, and there was good recovery after combination therapy. Therefore, every COVID-19 patient should undergo a meticulous screening routine to ensure that adequate treatment is provided.
Ethics approval and consent to participate
The Institutional Review Board of Chang Gung Medical Foundation approved this study (202000631B0).
Conflicts of interest
The authors declare that they have no competing interests.
Footnotes
Peer review under responsibility of Chang Gung University.
Contributor Information
Cheng-Ta Yang, Email: yang1946@cgmh.org.tw.
Han-Chung Hu, Email: h3226@cgmh.org.tw.
References
- 1.World Health Organization Coronavirus disease 2019 (COVID-19): situation report, 51. https://apps.who.int/iris/handle/10665/331475
- 2.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guan W.J., Ni Z.Y., Hu Y., Liang W.H., Ou C.Q., He J.X. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;82:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ai T., Yang Z., Hou H., Zhan C., Chen C., Lv W. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 2020;296:E32–E40. doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Khaddour K., Sikora A., Tahir N., Nepomuceno D., Huang T. Case report: the importance of novel coronavirus disease (COVID-19) and coinfection with other respiratory pathogens in the current pandemic. Am J Trop Med Hyg. 2020;102:1208–1209. doi: 10.4269/ajtmh.20-0266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fan B.E., Lim K.G.E., Chong V.C.L., Chan S.S.W., Ong K.H., Kuperan P. COVID-19 and mycoplasma pneumoniae coinfection. Am J Hematol. 2020;95:723–724. doi: 10.1002/ajh.25785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sohrabi C., Alsafi Z., O'Neill N., Khan M., Kerwan A., Al-Jabir A. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19) Int J Surg. 2020;76:71–76. doi: 10.1016/j.ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Khoury T., Sviri S., Rmeileh A.A., Nubani A., Abutbul A., Hoss S. Increased rates of intensive care unit admission in patients with Mycoplasma pneumoniae: a retrospective study. Clin Microbiol Infect. 2016;22:711–714. doi: 10.1016/j.cmi.2016.05.028. [DOI] [PubMed] [Google Scholar]
- 9.Wong H.Y.F., Lam H.Y.S., Fong A.H., Leung S.T., Chin T.W., Lo C.S.Y. Frequency and distribution of chest radiographic findings in COVID-19 positive patients. Radiology. 2020;296:E72–E78. doi: 10.1148/radiol.2020201160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Reittner P., Muller N.L., Heyneman L., Johkoh T., Park J.S., Lee K.S. Mycoplasma pneumoniae pneumonia: radiographic and high-resolution CT features in 28 patients. Am J Roentgenol. 2000;174:37–41. doi: 10.2214/ajr.174.1.1740037. [DOI] [PubMed] [Google Scholar]
- 11.Miyashita N., Sugiu T., Kawai Y., Oda K., Yamaguchi T., Ouchi K. Radiographic features of Mycoplasma pneumoniae pneumonia: differential diagnosis and performance timing. BMC Med Imag. 2009;9:7. doi: 10.1186/1471-2342-9-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Xie X., Zhong Z., Zhao W., Zheng C., Wang F., Liu J. Chest CT for typical 2019-nCoV pneumonia: relationship to negative RT-PCR testing. Radiology. 2020;296:E41–E45. doi: 10.1148/radiol.2020200343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shi H., Han X., Jiang N., Cao Y., Alwalid O., Gu J. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20:425–434. doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fang Y., Zhang H., Xie J., Lin M., Ying L., Pang P. Sensitivity of chest CT for COVID-19: comparison to RT-PCR. Radiology. 2020;296:E115–E117. doi: 10.1148/radiol.2020200432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ishiguro N., Koseki N., Kaiho M., Ariga T., Kikuta H., Togashi T. Therapeutic efficacy of azithromycin, clarithromycin, minocycline and tosufloxacin against macrolide-resistant and macrolide-sensitive Mycoplasma pneumoniae pneumonia in pediatric patients. PLoS One. 2017;12 doi: 10.1371/journal.pone.0173635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Miyashita N., Obase Y., Ouchi K., Kawasaki K., Kawai Y., Kobashi Y. Clinical features of severe Mycoplasma pneumoniae pneumonia in adults admitted to an intensive care unit. J Med Microbiol. 2007;56:1625–1629. doi: 10.1099/jmm.0.47119-0. [DOI] [PubMed] [Google Scholar]