N-terminal pro brain natriuretic peptide elevation is an independent risk factor for in-hospital death in severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and its disease, coronavirus disease 2019 (COVID-19).1 Pulmonary arterial hypertension (PAH) with right ventricular dysfunction may be at risk from COVID-19. Angiotensin-converting enzyme 2 (ACE2) is the known cellular receptor and a necessary entry point for SARS-CoV and SARS-CoV-2 infection.2 Priming of the S glycoprotein present in the SARS-CoV-2 spikes by the host protease transmembrane protease serine 2, and possibly furin and cathepsin L, is essential for the interaction of the virus with ACE2.
The Gene Expression Omnibus (GEODataset, https://www.ncbi.nlm.nih.gov/gds/) was searched for transcriptomic datasets with key words “pulmonary,” “hypertension,” “homo,” and “lung” and containing lung mRNA expression data from patients with PAH. Four datasets—GSE113439, GSE48149, GSE15197, and GSE53408—met the criteria and were selected for analysis. Details of the study cohorts, analytic procedures, and ethical approval are given in the original reports. Briefly, the datasets contained the gene expression profile of samples from explanted lungs of patients with PAH. Controls were lung samples without associated cardiovascular disease obtained from organ donors whose lungs were not used for lung transplantation or from healthy tissue flanking lung cancer resections. Only samples identified as PAH (class I pulmonary hypertension) were included for the analysis. Datasets contained samples from patients with idiopathic PAH, connective tissue disease–associated PAH, or congenital heart disease–associated PAH. The sample preparation, RNA extraction, cDNA synthesis, microarray analysis, gene annotation, preprocessing, and data curation and normalization followed standard procedures. Microarrays were processed with either Affymetrix or Illumina platforms as described in the original reports. Random effects meta-analysis was performed using the Cochrane software RevMan version 5.4. The effect size as standardized mean difference was calculated and p < 0.05 was considered statistically significant.
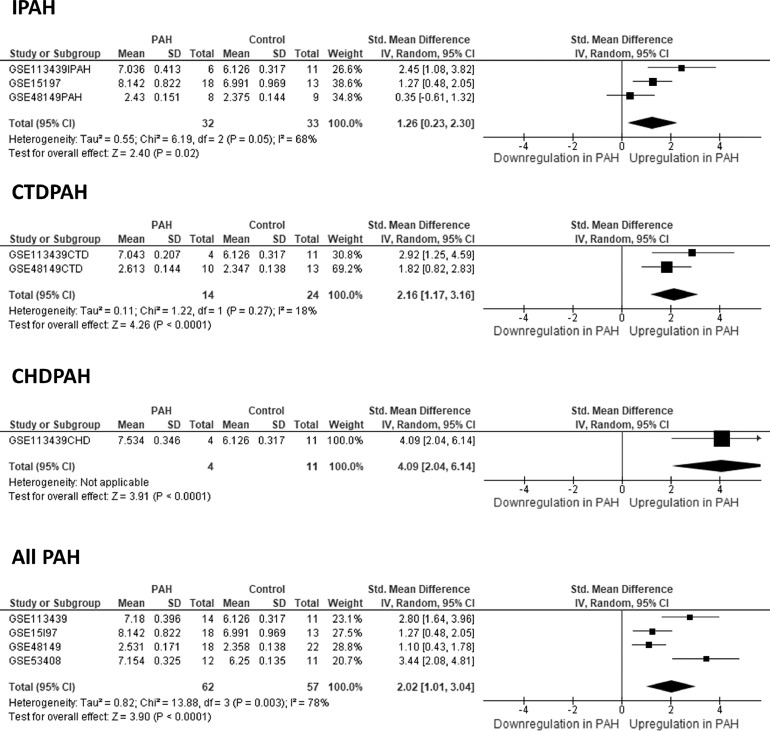
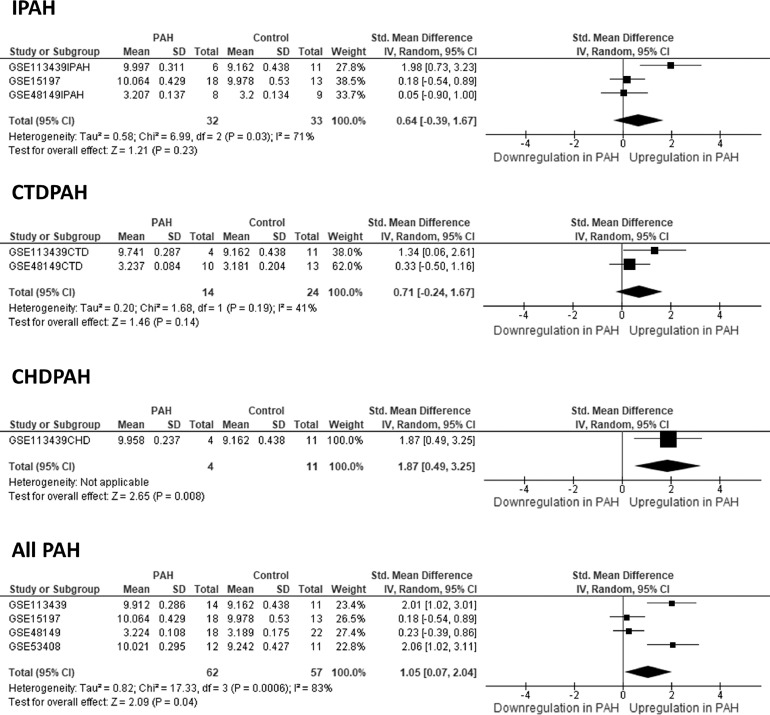
ACE2 gene expression in explanted lungs from patients with PAH was strongly and consistently upregulated compared with controls in all datasets analyzed and in the meta-analysis (∼6-fold, p < 0.0001, Figure 1 ). This was independent of the PAH subtype. Likewise, upregulated mRNA ACE2 (4-fold) has been reported in rat lungs with PAH induced by monocrotaline.3 ACE2 exists in 2 forms, the most abundant membrane-bound ACE2 (mACE2) and the relatively scarce circulating soluble ACE2 (sACE2). sACE2 may serve as a competitive interceptor of the virus, decreasing the binding of the viral particles to mACE2 and, hence, preventing viral infection.4 sACE2 results from proteolytic cleavage of mACE2 by the tumor necrosis factor α converting enzyme ADAM17 in a process known as shedding, which governs the mACE2/sACE2 ratio. Thus, the lung expression of ADAM17 was meta-analyzed and resulted to be also significantly upregulated (Figure 2 ), which favors a decreased mACE2/sACE2 ratio and presumably a reduced infectivity. Likewise, a recent report has also found an increase in circulating plasma protein ACE2 concentration in patients with PAH.5
Figure 1.
Forest plot of the meta-analysis of ACE2 lung gene expression. Data are Hedges’ g effect size (standardized mean difference in log10 scale) and the lines represent the 95% CI. Square sizes are proportional to weight. CHDPAH samples were from GSE113439; CTDPAH samples were from GSE113439 and GSE53408; and IPAH samples were from GSE113439, GSE15197, and GSE53408. The GSE53408 dataset did not identify the PAH subtypes. n indicates patients vs controls. Only samples with PAH (class I pulmonary hypertension) were included. CHDPAH, congenital heart disease–associated pulmonary arterial hypertension; CTDPAH, connective tissue disease–associated pulmonary arterial hypertension; IPAH, idiopathic pulmonary arterial hypertension; PAH, pulmonary arterial hypertension.
Figure 2.
Forest plot of the meta-analysis of ADAM17 lung gene expression. See Figure 1 legend for details. CHDPAH, congenital heart disease–associated pulmonary arterial hypertension; CTDPAH, connective tissue disease–associated pulmonary arterial hypertension; IPAH, idiopathic pulmonary arterial hypertension; PAH, pulmonary arterial hypertension.
Besides the receptor function of ACE2 for SARS-CoV-2, its catalytic activity has important pathophysiological consequences for both PAH5 and COVID-19.4 First, ACE2 converts angiotensin I into Ang1–9 and angiotensin II into Ang1–7 and thereby negatively regulates the renin angiotensin system, promoting vasodilation and anti-inflammatory effects. Second, ACE2 degrades des-Arg9-bradykinin and prevents the subsequent release of proinflammatory chemokines and exaggerated lung injury. Therefore, ACE2 activity is protective in acute lung injury induced by bacterial endotoxin or SARS-CoV-24. During SARS-CoV infection, ACE2 is downregulated, resulting in a loss of its protective anti-inflammatory effects, enhanced lung vascular permeability, and exacerbated pneumonia progression.4 Altogether, upregulated ACE2 activity should be interpreted as a beneficial effect for PAH5 and in part for COVID-19.4 However, despite the increased ACE2 protein in plasma of patients with PAH, its activity was reported to be diminished, possibly because of the increased presence of autoantibodies against ACE2.5 This reduced ACE2 activity together with increased angiotensin-converting enzyme activity is detrimental for both PAH5 and COVID-19.4 In addition, increased ADAM17 has negative effects on inflammation by promoting shedding of several membrane-bound proteins, including tumor necrosis factor α, releasing the active form of this proinflammatory cytokine.
In conclusion, ACE2 and ADAM17 are upregulated in patients with PAH undergoing lung transplantation in a meta-analysis performed on lung transcriptomes. The changes are similar in idiopathic PAH, connective tissue disease–associated PAH, and congenital heart disease–associated PAH. These 2 proteases seem to be double-edged swords in the context of SARS-CoV-2 infection. By itself, increased ACE2 may increase viral entry but together, ACE2 and ADAM17 upregulation accounts for increased sACE2 protein, potentially intercepting the coronavirus. These hypotheses require validation and further study.
References
- 1.Gao L, Jiang D, Wen XS. Prognostic value of NT-proBNP in patients with severe COVID-19. Respir Res. 2020;21:83. doi: 10.1186/s12931-020-01352-w. 2020/04/16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Letko M, Marzi A, Munster V. Functional assessment of cell entry and receptor usage for SARS-CoV-2 and other lineage B betacoronaviruses. Nat Microbiol. 2020;5:562–569. doi: 10.1038/s41564-020-0688-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ferreira AJ, Shenoy V, Yamazato Y. Evidence for angiotensin-converting enzyme 2 as a therapeutic target for the prevention of pulmonary hypertension. Am J Respir Crit Care Med. 2009;179:1048–1054. doi: 10.1164/rccm.200811-1678OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Imai Y, Kuba K, Rao S. Angiotensin-converting enzyme 2 protects from severe acute lung failure. Nature. 2005;436:112–116. doi: 10.1038/nature03712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sandoval J, Del Valle-Mondragón L, Masso F, et al. Angiotensin converting enzyme 2 and angiotensin (1-7) axis in pulmonary arterial hypertension [e-pub ahead of print]. Eur Respir J. 2020;56:1902416. Accessed July 23, 2020. [DOI] [PubMed]