Abstract
Objectives
The 2019 novel coronavirus (COVID-19) pandemic is a severe global crisis which has resulted in many public health problems. This study aimed to investigate the prevalence of poor sleep quality and its related factors among employees who returned to work during the COVID-19 pandemic.
Methods
Our online cross-sectional study included 2,410 participants aged ≥17 years in Deqing and Taizhou, Zhejiang Province, China from 5th to 14th March 2020. The questionnaire covered information on demographic characteristics, health status, workplace, lifestyle, attitude towards COVID-19, assessment of anxiety, depression and sleep quality. The Chinese version of the Pittsburgh Sleep Quality Index (CPSQI) was administered to measure the poor sleep quality. Poor sleep quality was defined as a global PSQI score>5. Factors associated with sleep quality were analyzed by logistic regression models.
Results
In sum near half (49.2%) of 2,410 returning workers were females and the average year of subjects was 36.3 ± 9.1 years. The overall prevalence of poor sleep quality was 14.9% (95%CI: 13.5%–16.3%). The average score of PSQI was 3.0 ± 2.5 and average sleep duration was 7.6 ± 1.2 h. Independent related factors of poor sleep quality included age older than 24 years, higher education level, negative attitude towards COVID-19 control measures, anxiety and depression.
Conclusions
Poor sleep quality was common and there was a shorter sleep duration among returning workers during the COVID-19 pandemic. Possible risk factors identified from this study may be of great importance in developing proper intervention for the targeted population to improve the sleep health during the COVID-19 public health emergency.
Keywords: Poor sleep quality, Pittsburgh sleep quality index, COVID-19, Occupational population, China
Highlights
-
•
Poor sleep quality was common among Chinese returning workers during the COVID-19 pandemic.
-
•
Poor sleep duration was shortened among Chinese among returning workers.
-
•
Possible risk factors identified in this study may be beneficial in developing psychological intervention and health education for the targeted population during this public health emergency.
1. Introduction
The 2019 novel coronavirus (COVID-19) pandemic is a global health crisis which can damage both physical health and mental health. Previous studies have shown that infectious disease epidemics like severe acute respiratory syndrome (SARS) and Ebola virus disease (EVD) could cause sleep-related problems in relevant individuals [[1], [2], [3]]. Good sleep quality is very important to health [4]. Several recent studies focused on sleep quality of medical workers and individuals who self-isolated for 14 days during the COVID-19 pandemic. Frontline medical workers (fMW) had worse sleep compared to non-fMW [5,6]. Anxiety was associated with stress and sleep quality in individuals who self-isolated at home for 14 day [7].
Since mid-February, due to the fact that the COVID-19 pandemic has largely been under control in China, employees have been returning to work in many areas. The returning workers experienced lifestyle changes from prolonged state of not working to working again. As of March 5, it was reported that more than 100 people in 26 companies were infected with COVID-19, and more than 10,000 people were quarantined after returning to work in China, which suggested that returning to work may increase the risk of infecting COVID-19 [8]. On one hand, the fear of infection risk or losing job due to economic downturn may worse the sleep quality among the returning worker. On the other hand, the benefit of improving the financial status after returning to work may help reduce the stress and lead to better sleep quality. So far, no studies of sleep quality and their related factors for returning workers. Therefore, we aimed to investigate the prevalence and associated factors of poor sleep quality among Chinese who returned to work during the COVID-19 pandemic.
2. Methods
2.1. Study population
A cross-sectional study was conducted among individuals after the first two-week of returning to work in Deqing and Taizhou, Zhejiang Province, China from 5th to 14th March 2020. Returning workers were the employees who were approved to back to work and returned to work at those enterprises or home during 15th Feb. to 5th March 2020. Deqing was a low-risk epidemic area with less than 10 confirmed cases of COVID-19 and Taizhou was a high-risk epidemic area with more than 100 confirmed cases of COVID-19 [9]. Inclusion criteria of the enterprises was that the annual business turnover of 20 million RMB or above and reopened since mid-February. Exclusion criteria was that the general manager or director refused to participate into this study. In each area, the eligible enterprises were engaged to support this survey until recruited subjects more than 900. The different kinds of enterprises were covered as many as possible. Finally, 43 of 996 enterprises in Taizhou and 120 of 738 enterprises in Deqing were included in this study. Inclusion criteria of returning workers were as follows: (a) older than 17 years old; (b) full-time employees; and (c) who had returned to work since mid-February. The returning workers whose completion time on survey was more than 30 min or less than 2 min or those who were diagnosed with COVID-19, had family members being diagnosed, or had close contact with confirmed cases of COVID-19 were deleted. Totally, 2,410 of 2,461 of returning workers were eligible and included in this study.
2.2. Data collection
All subjects completed an online questionnaire. Data collected included demographic characteristics, health status, workplace, lifestyle, attitude towards COVID-19 control, and assessments of anxiety, depression and sleep quality.
Legislators, senior officials, managers, (associate) professionals, technicians, and clerks were defined as white-collar workers according to the International standard classification of occupations (ISCO) [10]. Annual household income was classified into three groups: low income (0–50,000RMB), middle income (50,001–200,000RMB) and high income (>200,000RMB) in 2019. Smoking was defined as consuming at least one cigarette per day for at least six months [11]. Alcohol drinking was defined as drinking any alcohol at least three times per week for at least six months [12]. Tea consumption was defined as drinking any tea at least three times per week for at least six months [13]. Regular physical exercise was defined as having physical exercise at least three times a week for at least 30 min each time [14]. The nine-item Patient Health Questionnaire (PHQ-9) was used to measure the depressive symptom with a summed score ranging from 0 to 27 for the nine items, and mild depression was defined as a PHQ-9 score≥5 in this study [15]. Cronbach's alpha for the internal consistency reliability and two-week test-retest reliability of the Chinese version of the PHQ-9 were 0.86 [16]. The seven-item Generalized Anxiety Disorder (GAD-7) was used to measure anxiety symptom with a summed score ranging from 0 to 21, and mild anxiety was defined as a GAD-7 score ≥5 in this study [17]. Cronbach's alpha for the internal consistency reliability of the Chinese version of the GAD-7 was 0.90 and the test-retest reliability was 0.86 [18].
2.3. Measurement of sleep quality
The Pittsburgh Sleep Quality Index (PSQI) questionnaire was used to measure the sleep quality of study subjects, and included 19 items that assess seven domains of sleep quality: subjective sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbance, use of sleeping medication and daytime dysfunction. Every domain weighed equally on a 0–3 scale. Scores for all seven domains are summed up to yield a global PSQI score, ranging from 0 to 21. Poor sleep quality was defined as a global PSQI score>5 in this study [19]. The Chinese version of the Pittsburgh Sleep Quality Index (CPSQI) had good overall reliability (r = 0.82–0.83) and test–retest reliability (r = 0.77–0.85) [20].
2.4. Ethical approval
The study was approved by the Institutional Review Board of the Fudan University School of Public Health (IRB#2020040817). All the participants gave an online informed consent.
2.5. Statistical analysis
Data were analyzed using SPSS version 24.0 (IBM Corp, Armonk, New York, USA). Continuous variables were described as means ± standard deviations (SD) and categorical variables as frequencies and percentages. Chi-square was occupied to compare the distributions of categorical variables between good sleep quality group and poor sleep quality group, or sex groups, or age groups. Mean differences of continuous variables between different sex groups was tested by t-test or Mann–Whitney U test, and those between different age groups were tested by one way analysis of variance (ANOVA) or Kruskal–Wallis test. Univariate and multivariate logistic regression models were used to identify factors associated with poor sleep quality. The univariate OR, multivariate OR and their corresponding 95% confidence intervals (CI) were estimated. Two-sided P value < 0.05 was considered to be statistically significant.
3. Results
3.1. General characteristics of study population
The social-demographic and other characteristics of 2,410 subjects according to sleep quality were shown in Table 1 . The average age was 36.3 ± 9.1 years, and sex ratio was about 1:1. Near 60% of subjects were from Deqing. Most of them worked only at enterprise (90.4%). 40% of subjects had the quarantine experience during the COVID-19 pandemic. There were significant differences in age, education level, alcohol drinking, regular physical exercise, being negative for the COVID-19 control, anxiety and depression between subjects with and without poor sleep (P < 0.05).
Table 1.
Characteristics of participants by sleep quality.
| Characteristics | Good sleep quality (n = 2,051) | Poor sleep quality (n = 359) | Total (n = 2,410) | P value |
|---|---|---|---|---|
| Age (years), n (%) | 0.047 | |||
| 17-24 | 211 (90.6) | 22 (9.4) | 233 (100.0) | |
| 25-34 | 848 (86.5) | 143 (14.4) | 991 (100.0) | |
| 35-44 | 583 (83.2) | 118 (16.8) | 701 (100.0) | |
| ≥45 | 409 (84.3) | 76 (15.7) | 485 (100.0) | |
| Sex, n (%) | 0.076 | |||
| Male | 1027 (83.8) | 198 (16.2) | 1225 (100.0) | |
| Female | 1024 (86.4) | 161 (13.6) | 1185 (100.0) | |
| Married (yes), n (%) | 1575 (85.4) | 270 (14.6) | 1845 (100.0) | 0.514 |
| Education year, n (%) | <0.001 | |||
| <9 education years | 718 (88.6) | 92 (11.4) | 810 (100.0) | |
| ≥9 education years | 1333 (83.3) | 267 (16.7) | 1600 (100.0) | |
| Annual household incomea | 0.300 | |||
| Low | 335 (84.8) | 60 (15.2) | 395 (100.0) | |
| Middle | 1069 (85.2) | 185 (14.8) | 1254 (100.0) | |
| High | 240 (81.6) | 54 (18.4) | 294 (100.0) | |
| Enterprise location | 0.187 | |||
| Deqing | 1230 (85.9) | 202 (14.1) | 1432 (100.0) | |
| Taizhou | 821 (83.9) | 157 (16.1) | 978 (100.0) | |
| Workplace | 0.106 | |||
| Enterprise | 1860 (85.4) | 318 (14.6) | 2178 (100.0) | |
| Home | 160 (84.2) | 30 (15.8) | 190 (100.0) | |
| Both | 31 (73.8) | 11 (26.2) | 42 (100.0) | |
| White-collar worker (yes), n (%) | 1450 (84.4) | 269 (15.6) | 1719 (100.0) | 0.102 |
| Smoking (yes), n (%) | 491 (82.7) | 103 (17.3) | 594 (100.0) | 0.054 |
| Alcohol drinking (yes), n (%) | 151 (77.8) | 43 (22.2) | 194 (100.0) | 0.003 |
| Tea consumption (yes), n (%) | 595 (86.1) | 96 (13.9) | 691 (100.0) | 0.380 |
| Regular physical exercise (yes), n (%) | 1739 (86.0) | 282 (14.0) | 2021 (100.0) | 0.003 |
| Quarantine experience (yes), n (%) | 820 (85.1) | 144 (14.9) | 964 (100.0) | 0.963 |
| Negative for the COVID-19 control (yes), n (%) | 582 (82.2) | 126 (17.8) | 708 (100.0) | 0.010 |
| Anxiety (yes), n (%) | 165 (55.4) | 133 (44.6) | 298 (100.0) | <0.001 |
| Depression (yes), n (%) | 284 (60.2) | 188 (39.8) | 472 (100.0) | <0.001 |
Note: P value < 0.05 means that the difference was significant.
Annual household income had 467 missing value.
3.2. Comparison of domain scores and prevalence in different sex and age groups
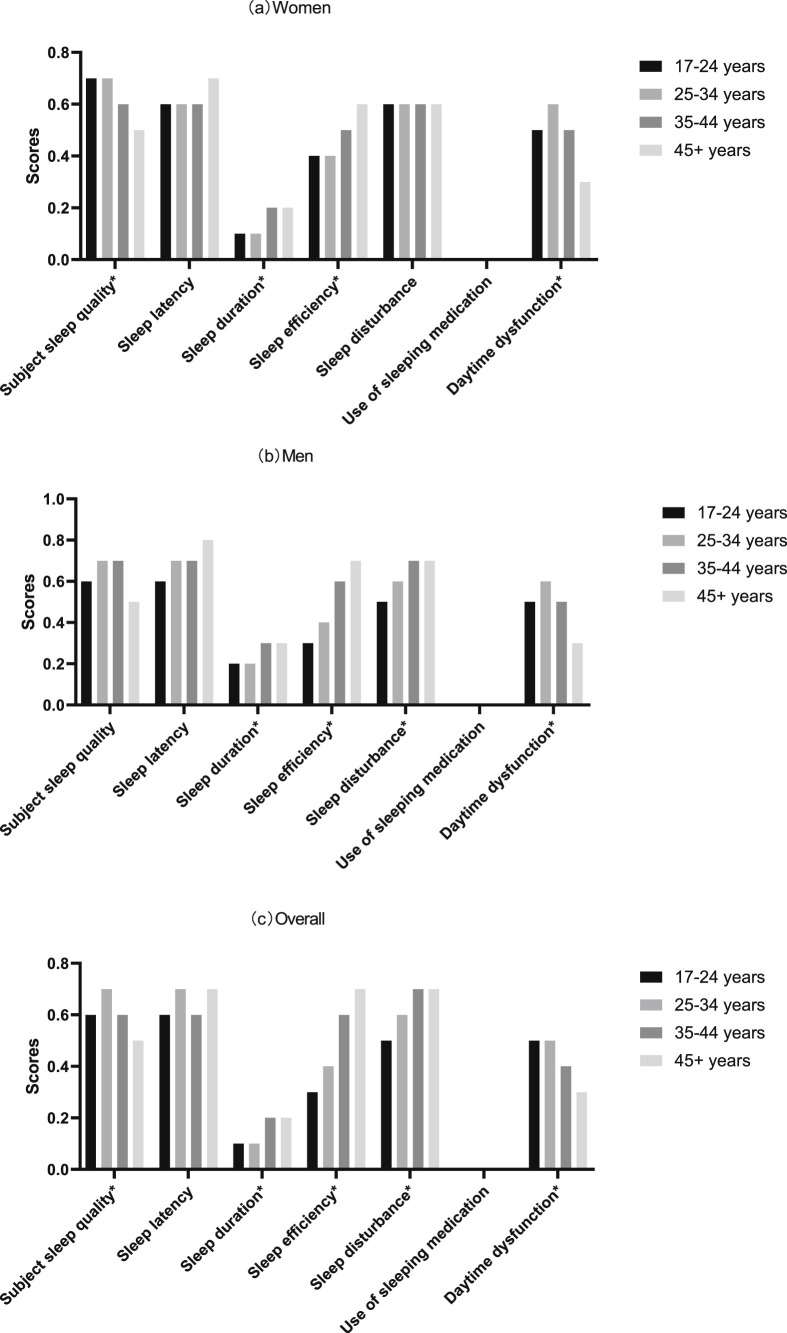
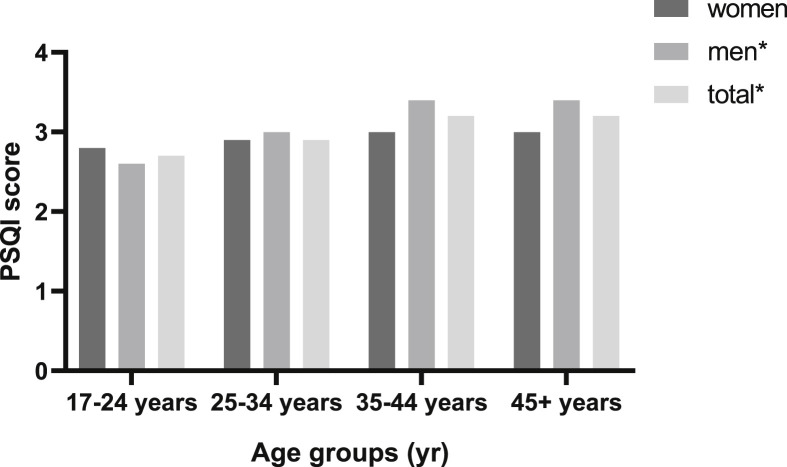
The subjects had an average sleep duration of 7.6 ± 1.2 h. The overall mean score (±SD) was 0.6 (±0.7) for subjective sleep quality, 0.7 (±0.7) for sleep latency, 0.2 (±0.5) for sleep duration, 0.5 (±0.8) for sleep efficiency, 0.6 (±0.5) for sleep disturbance, 0.0 (±0.1) use of sleeping medication and 0.5 (±0.7) for daytime dysfunction. For these PSQI domain scores, sleep latency was the highest, and the use of sleeping medication was the lowest. The average score of PSQI was 3.0 ± 2.4 and was higher in males than females (3.2 ± 2.5 vs 2.9 ± 2.4, P < 0.001). The detailed sex- and age-specific domain scores of sleep quality and PSQI score were presented in Fig. 1 and Fig. 2 . Older subjects were more likely to have sleep disturbance and poor sleep efficiency while younger subjects were more likely to have frequent day dysfunctions (Fig. 1c).
Fig. 1.
Sex- and age-specific domain scores of sleep quality during the COVID-19 pandemic. Note: ∗ Significant difference over different age groups (P value < 0.05).
Fig. 2.
Sex- and age-specific PSQI score during the COVID-19 pandemic. Note: ∗ Significant difference over different age groups (P value < 0.05).
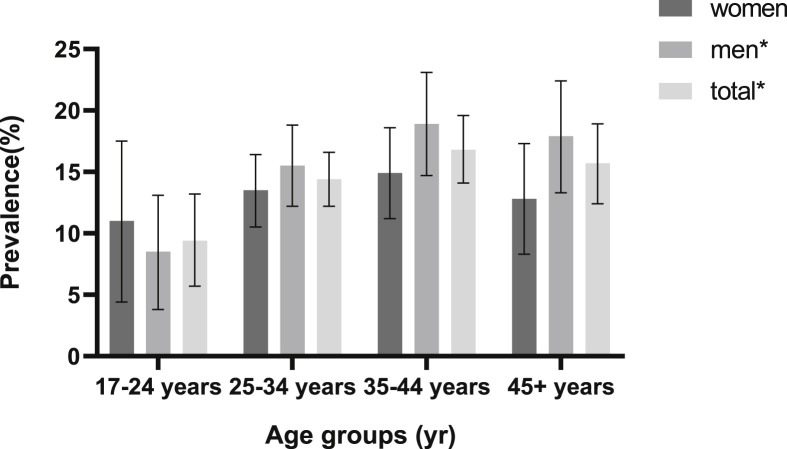
The prevalence of poor sleep quality was 14.9% (95% CI: 13.5%–16.3%) overall, and was higher in males than females (16.2% vs 13.6%, P = 0.071). Subjects who aged 35–44 years had the highest prevalence of poor sleep quality (16.8%, 95% CI: 14.1%–19.6%). The sex- and age-specific prevalence of poor sleep quality was shown in Fig. 3 .
Fig. 3.
Sex- and age-specific prevalence of poor sleep quality during the COVID-19 pandemic. Note: ∗ Significant difference over different age groups (P value < 0.05). The error bars mean 95% confidence intervals.
3.3. Related factors of poor sleep quality
As presented in Table 2 , after the adjustment of covariates, the independent factors of poor sleep quality were age, education levels, being negative for the COVID-19 control, anxiety and depression. The risk of poor sleep quality increased with age. Higher education level was associated with a higher risk of poor sleep quality (aOR: 1.39; 95% CI: 1.02–1.89). Subjects with negative attitude towards the COVID-19 control measures (aOR: 1.36; 95% CI: 1.05–1.76) were more likely to have poor sleep quality. In addition, anxiety (aOR: 2.75; 95% CI: 1.96–3.84) and depression (aOR: 4.60; 95% CI: 3.37–6.28) were significantly associated with poor sleep quality.
Table 2.
Univariate and multivariate logistic regression analysis of factors associated with poor sleep quality.
| Variables | Univariate OR (95% CI) | P value | Multivariate OR (95% CI) | P value | |
|---|---|---|---|---|---|
| Sex | |||||
| Female | 1.00 | 1.00 | |||
| Male | 1.23 (0.98–1.54) | 0.076 | 1.29 (0.96–1.74) | 0.097 | |
| Age (years) | |||||
| 17-24 | 1.00 | 1.00 | |||
| 25-34 | 1.62 (1.01–2.60) | 0.047 | 2.12 (1.27–3.56) | 0.004 | |
| 35-44 | 1.94 (1.20–3.14) | 0.007 | 3.49 (2.03–5.98) | <0.001 | |
| ≥45 | 1.78 (1.08–2.95) | 0.024 | 4.27 (2.39–7.62) | <0.001 | |
| Education | |||||
| <9 education years | 1.00 | 1.00 | |||
| ≥9 education years | 1.56 (1.21–2.02) | <0.001 | 1.39 (1.02–1.89) | 0.038 | |
| Enterprise location | |||||
| Deqing | 1.00 | 1.00 | |||
| Taizhou | 1.16 (0.93–1.46) | 0.188 | 1.06 (0.81–1.40) | 0.652 | |
| Workplace | |||||
| Enterprise | 1.00 | 1.00 | |||
| Home | 1.10 (0.73–1.65) | 0.657 | 1.20 (0.74–1.96) | 0.458 | |
| Both | 2.08 (1.03–4.17) | 0.040 | 1.73 (0.78–3.81) | 0.174 | |
| White-collar worker | |||||
| No | 1.00 | 1.00 | |||
| Yes | 1.24 (0.96–1.60) | 0.102 | 1.01 (0.75–1.37) | 0.925 | |
| Smoking | |||||
| No | 1.00 | 1.00 | |||
| Yes | 1.28 (1.00–1.64) | 0.054 | 1.03 (0.73–1.44) | 0.882 | |
| Drinking alcohol | |||||
| No | 1.00 | 1.00 | |||
| Yes | 1.71 (1.20–2.45) | 0.003 | 1.51 (0.98–2.34) | 0.064 | |
| Tea consumption | |||||
| No | 1.00 | 1.00 | |||
| Yes | 0.89 (0.69–1.15) | 0.381 | 0.80 (0.59–1.09) | 0.155 | |
| Regular physical exercise | |||||
| No | 1.00 | 1.00 | |||
| Yes | 0.66 (0.50–0.87) | 0.003 | 0.80 (0.58–1.10) | 0.174 | |
| Quarantine experience | |||||
| Yes | 1.00 | 1.00 | |||
| No | 0.99 (0.79–1.25) | 0.963 | 1.02 (0.79–1.32) | 0.897 | |
| Negative for the COVID-19 control | |||||
| No | 1.00 | 1.00 | |||
| Yes | 1.37 (1.08–1.73) | 0.010 | 1.36 (1.05–1.76) | 0.022 | |
| Anxiety | |||||
| No | 1.00 | 1.00 | |||
| Yes | 6.73 (5.15–8.78) | <0.001 | 2.75 (1.96–3.84) | <0.001 | |
| Depression | |||||
| No | 1.00 | 1.00 | |||
| Yes | 6.84 (5.37–8.71) | <0.001 | 4.60 (3.37–6.28) | <0.001 | |
Note: P value < 0.05 means the difference was significant.
4. Discussion
The overall prevalence of poor sleep quality among returning workers during COVID-19 pandemic was 14.9% (95%CI: 13.5%–16.3%) with the average sleep duration of 7.6 ± 1.2 h. Our multivariate analysis found that poor sleep quality was significantly associated with advanced age, higher education level, negative attitude towards the COVID-19 control measures, anxiety, and depression.
Compared with previous study, we found that employees who returned to work had poor sleep quality and a shorter sleep duration. Before the COVID-19 pandemic, a China National Study among different occupational populations found that the overall prevalence of poor sleep quality was 26.98% varied from 14.47% in Jiangsu Province to 31.83% in Hubei Province. In addition, white-collar workers had better sleep quality. Farmers had the longest sleep duration (8.22 h) while civil servants had the shortest sleep duration (7.85 h) [21]. A recent cross-sectional survey conducted from 3rd to 17th February 2020 showed that the prevalence of poor sleep quality among enterprise or institution workers during COVID-19 outbreak in China was 12.7%, which was similar to our findings [22]. It should be noted that PSQI asked about the sleep habits during the past month so that our results covered the sleep quality during the outbreak for those recruited in earlier March. Our findings suggested that the sleep quality of the study population during such pandemic was similar to the findings form Jiangsu Province before such pandemic and one recent study during COVID-19 outbreak in China [21,22]. One of possible reasons was that Zhejiang Province as the study area is most similar to Jiangsu Province in socioeconomic status and they are located at East China, the most developed areas of China. Another of possible reasons was that the quick and effective control of COVID-19 might have improved the quality of sleep of subjects in China. In addition, most of the participants in this study were white-collar workers, and white-collar workers generally have better sleep quality blue collar worker [21]. Long sleep latency was found to be the most serious problem among seven PSQI domains of sleep quality, which was consistent with some previous Chinese studies [13,23,24]. A recent study found that participants with Wuhan COVID-19 exposure history or traumatic experience showed more latency of sleep than those without [25]. Long sleep latency can be caused by reactions of fear and increased presleep cognitions [26,27].
Previous studies found that women were more likely to suffer from poor sleep quality [24,28]. Sleep quality decreases with age, because older people tend to have more chronic diseases [13], different circadian rhythms and poor psychiatric conditions [29]. Therefore, attitude and practice (KAP) model, public health emergencies can impact individual health status through knowledge, attitude, practice and their interaction effects. In this study, subjects with lower education level had better sleep quality, which is consistent with the results from some recent surveys [30,31]. Higher education can increase negative emotion and sleep problems when there are public health emergencies, probably because of high self-awareness of health [32]. Psychological problems such as anxiety and depression were significantly associated with poor sleep quality in this study. Longitudinal studies showed that sleep quality was bidirectionally related to anxiety and depression [33,34]. The psychological intervention should be taken to improve anxiety and depression symptoms, which may improve the sleep quality of returning workers during the COVID-19 pandemic. In addition subjects with negative attitude towards the COVID-19 control measures were more likely to have poor sleep quality in this study. Moreover, this remained significant after the control for possible confounders (including the anxiety and depression symptoms). Previous studies suggested that females had lower education level, lower individual income, and were more susceptible to fear, anxiety and depression than males [24,35,36]. In the current study, however, we found no sex difference in sleep quality.
This study was the first cross-sectional survey concerning sleep quality among Chinese employees who returned to work during the COVID-19 pandemic, and covered approximately 10% of enterprises in two sites with different severity of the COVID-19 pandemic. There were several limitations for the study. First, this study did not include small enterprises. As a consequence, the sleep quality could be underestimated because workers in small or private enterprises tended to have higher risk jobs, which was a risk factor of insomnia [37]. Second, the cross-sectional design cannot infer a causal relationship between associated factors and poor sleep quality. In addition, the assessment of sleep quality with PSQI questionnaire was more subjective compared with polysomnography.
5. Conclusions
The cross-sectional survey showed poor sleep quality and a shorter sleep duration among employees who just returned to work. Employees who were older than 24 years old, had higher education level or negative attitude towards the COVID-19 control, or had anxiety and depressive symptoms tended to have a higher risk of poor sleep quality. These findings suggested that the proper measures should be taken to reduce the negative attitude and to care psychological symptoms of anxiety and depression for the targeted population to improve the sleep health during the COVID-19 pandemic.
Footnotes
The authors declare no potential conflicts of interest.
The ICMJE Uniform Disclosure Form for Potential Conflicts of Interest associated with this article can be viewed by clicking on the following link: https://doi.org/10.1016/j.sleep.2020.06.034.
Conflict of interest
The following are the supplementary data related to this article:
References
- 1.Moldofsky H., Patcai J. Chronic widespread musculoskeletal pain, fatigue, depression and disordered sleep in chronic post-SARS syndrome; a case-controlled study. BMC Neurol. 2011;11:37. doi: 10.1186/1471-2377-11-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wilson H.W., Amo-Addae M., Kenu E. Post-Ebola syndrome among Ebola virus disease survivors in Montserrado County. Liberia. 2018;2016:2018. doi: 10.1155/2018/1909410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Luyt C.E., Combes A., Becquemin M.H. Long-term outcomes of pandemic 2009 influenza A(H1N1)-associated severe ARDS. Chest. 2012;142(3):583–592. doi: 10.1378/chest.11-2196. [DOI] [PubMed] [Google Scholar]
- 4.Huang T., Mariani S., Redline S. Sleep irregularity and risk of cardiovascular events: the multi-ethnic study of atherosclerosis. J Am Coll Cardiol. 2020;75(9):991–999. doi: 10.1016/j.jacc.2019.12.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lai J., Ma S., Wang Y. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3(3) doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Qi J., Xu J., Li B. The evaluation of sleep disturbances for Chinese frontline medical workers under the outbreak of COVID-19. medRxiv. 2020 doi: 10.1016/j.sleep.2020.05.023. 2020.03.06.20031278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xiao H., Zhang Y., Kong D. Social capital and sleep quality in individuals who self-isolated for 14 Days during the coronavirus disease 2019 (COVID-19) outbreak in January 2020 in China. Med Sci Mon. 2020;26 doi: 10.12659/MSM.923921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.N News Forced to stop work! More than 100 people infected in 26 companies! More than 10,000 people were quarantined! 2020. https://dy.163.com/v2/article/detail/F73ICACD05459WW8.html
- 9.ChinaCDC Distribution of the COVID-19 epidemic. 2020. http://2019ncov.chinacdc.cn/2019-nCoV/
- 10.ILO, International Standard classification of occupations (ISCO) 2020. https://ilostat.ilo.org/resources/methods/classification-occupation/
- 11.Lasser K., Boyd J.W., Woolhandler S. Smoking and mental illness: a population-based prevalence study. J Am Med Assoc. 2000;284(20):2606–2610. doi: 10.1001/jama.284.20.2606. [DOI] [PubMed] [Google Scholar]
- 12.Bellos S., Skapinakis P., Rai D. Longitudinal association between different levels of alcohol consumption and a new onset of depression and generalized anxiety disorder: results from an international study in primary care. Psychiatr Res. 2016;243:30–34. doi: 10.1016/j.psychres.2016.05.049. [DOI] [PubMed] [Google Scholar]
- 13.Dong X., Wang Y., Chen Y. Poor sleep quality and influencing factors among rural adults in Deqing, China. Sleep Breath = Schlaf Atmung. 2018;22(4):1213–1220. doi: 10.1007/s11325-018-1685-8. [DOI] [PubMed] [Google Scholar]
- 14.Nelson M.E., Rejeski W.J., Blair S.N. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39(8):1435–1445. doi: 10.1249/mss.0b013e3180616aa2. [DOI] [PubMed] [Google Scholar]
- 15.Kroenke K., Spitzer R.L., Williams J.B. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang W., Bian Q., Zhao Y. Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatr. 2014;36(5):539–544. doi: 10.1016/j.genhosppsych.2014.05.021. [DOI] [PubMed] [Google Scholar]
- 17.Spitzer R.L., Kroenke K., Williams J.B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 18.He X.Y., Li C., Qian J. Reliability and validity of a generalized anxiety scale in general hospital outpatients. Shanghai Archiv Psychiat. 2010;22:200–203. [Google Scholar]
- 19.Buysse D.J., Reynolds C.F., 3rd, Monk T.H. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatr Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 20.Tsai P.S., Wang S.Y., Wang M.Y. Psychometric evaluation of the Chinese version of the Pittsburgh Sleep Quality Index (CPSQI) in primary insomnia and control subjects. Qual Life Res. 2005;14(8):1943–1952. doi: 10.1007/s11136-005-4346-x. [DOI] [PubMed] [Google Scholar]
- 21.Sun W., Yu Y., Yuan J. Sleep duration and quality among different occupations-China national study. PloS One. 2015;10(3) doi: 10.1371/journal.pone.0117700. e0117700-e0117700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Huang Y., Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatr Res. 2020;288:112954. doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li J., Yao Y.S., Dong Q. Characterization and factors associated with sleep quality among rural elderly in China. Arch Gerontol Geriatr. 2013;56(1):237–243. doi: 10.1016/j.archger.2012.08.002. [DOI] [PubMed] [Google Scholar]
- 24.Wang P., Song L., Wang K. Prevalence and associated factors of poor sleep quality among Chinese older adults living in a rural area: a population-based study. Aging Clin Exp Res. 2020;32(1):125–131. doi: 10.1007/s40520-019-01171-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang F., Shang Z., Ma H. High risk of infection caused posttraumatic stress symptoms in individuals with poor sleep quality: a study on influence of coronavirus disease (COVID-19) in China. medRxiv. 2020 2020.03.22.20034504. [Google Scholar]
- 26.Fast K. University of Hawaii at Manoa; 2003. The relationship between presleep cognitions and delayed sleep-onset in a sample of women seeking treatment for sexual assault. [Google Scholar]
- 27.Van Egeren L., Haynes S.N., Franzen M. Presleep cognitions and attributions in sleep-onset insomnia. J Behav Med. 1983;6(2):217–232. doi: 10.1007/BF00845382. [DOI] [PubMed] [Google Scholar]
- 28.Madrid-Valero J.J., Martinez-Selva J.M., Ribeiro do Couto B. Age and gender effects on the prevalence of poor sleep quality in the adult population. Gac Sanit. 2017;31(1):18–22. doi: 10.1016/j.gaceta.2016.05.013. [DOI] [PubMed] [Google Scholar]
- 29.Miner B., Kryger M.H. Sleep in the aging population. Sleep Med Clin. 2017;12(1):31–38. doi: 10.1016/j.jsmc.2016.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li J.-B., Yang A., Dou K. Chinese public's knowledge, perceived severity, and perceived controllability of the COVID-19 and their associations with emotional and behavioural reactions, social participation, and precautionary behaviour: a national survey. PsyArXiv. 2020 doi: 10.1186/s12889-020-09695-1. 2020.02.28.1031234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhong B.L., Luo W., Li H.M. Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: a quick online cross-sectional survey. Int J Biol Sci. 2020;16(10):1745–1752. doi: 10.7150/ijbs.45221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Qiu J., Shen B., Zhao M. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiat. 2020;33(2) doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Alvaro P.K., Roberts R.M., Harris J.K. A systematic Review assessing bidirectionality between sleep disturbances, anxiety, and depression. Sleep. 2013;36(7):1059–1068. doi: 10.5665/sleep.2810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Altena E., Baglioni C., Espie C.A. Dealing with sleep problems during home confinement due to the COVID-19 outbreak: practical recommendations from a task force of the European CBT-I Academy. J Sleep Res. 2020 doi: 10.1111/jsr.13052. [DOI] [PubMed] [Google Scholar]
- 35.Felmingham K., Williams L.M., Kemp A.H. Neural responses to masked fear faces: sex differences and trauma exposure in posttraumatic stress disorder. J Abnorm Psychol. 2010;119(1):241–247. doi: 10.1037/a0017551. [DOI] [PubMed] [Google Scholar]
- 36.Wang Y.M., Chen H.G., Song M. Prevalence of insomnia and its risk factors in older individuals: a community-based study in four cities of Hebei Province, China. Sleep Med. 2016;19:116–122. doi: 10.1016/j.sleep.2015.10.018. [DOI] [PubMed] [Google Scholar]
- 37.Ota A., Masue T., Yasuda N. Psychosocial job characteristics and insomnia: a prospective cohort study using the Demand-Control-Support (DCS) and Effort-Reward Imbalance (ERI) job stress models. Sleep Med. 2009;10(10):1112–1117. doi: 10.1016/j.sleep.2009.03.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.