Abstract
Background:
The purpose of this study was to identify the effects of eight weeks of conventional and suspension core stability exercises by use of the designed device on characteristic of intervertebral discs in low back pain.
Methods:
A total of 27 men with chronic low back (CLB) pain due to lumbar disc herniation in L4-L5 and L5-S1 regions were enrolled in this quasi-experimental study. After assessing the pain intensity using a visual analog scale (VAS) and determining the disc herniation index using MRI, each group of patients were asked to perform either conventional or suspension exercises for eight weeks, each week consisting of three training sessions. The pain intensity was assessed at the end of the first, second, third, fourth and eighth weeks and the disc hernia index was determined again at the end of the eight weeks of exercises.
Results:
The results indicated significant changes in the intensity of pain in both groups through the period of eight weeks of exercise with a remarkable pain relief. In relation to the structural characteristics of the intervertebral disc, data analysis did not reveal any significant change between the pre- and post-test.
Conclusion:
Considering the beneficial effects of the stability exercises and specially suspension stability exercises with respect to pain alleviation and reduced use of sedatives and anti-inflammatory drugs, this method can be helpful at early stages of treatment for chronic pains.
Key Words: ore stability exercises, Disc herniation, ain, uspension core stability exercises
Introduction
Work is an inseparable aspect of human life. A review of literature indicate that three-fourths of the world’s jobs will be sedentary in the future (1). As a result, occupational diseases have also been on the rise due to the musculoskeletal disorders. These disorders constitute the most prevalent occupation-related disabilities (2, 3). Musculoskeletal disorders are usually due to prolonged or repeated pressures imposed on soft tissues such as nerves, muscles, tendons, and joints. Among these disorders, low back pain is extremely prevalent (3). It is especially common (about 41.7%) among office staffs who work several hours (about 7 to 8 hours) in a seated and steady position per day (4, 5). The herniation or bulging of the intervertebral discs, besides the deterioration of the core stability muscle is one of the main causes of these pains. Although the exact causes of these disorders have not been fully understood to date; factors such as poor posture, inappropriate chair, and prolonged seating accelerate the degeneration of discs and deterioration of core stability muscles (6).
With the increased pressure on the intervertebral discs, their structure and functions may be metabolically disturbed. As a result, the fluid discharge from the herniated discs diminishes and height loss is caused (7). At the same time, as joint surfaces are drawn together and joint movement or mobility’s restrained, the core stability muscles, rectus abdominis, transverses abdominis, internal and external oblique, diaphragm, and pelvic floor deteriorate (8). About one to four millimeter height loss was observed in lumbar discs after 30 minutes of steady sitting (9). In the same vein, Corlett and Eklund reported 5-5.5 mm height loosen the vertebral column in three different types of chairs after half an hour, with the greatest loss being observed in the lumbar vertebrae, especially l4-l5 and l5-s1 (10). As a consequence, the intervertebral disc herniation, particularly, in L4-L5 and L5-S1, lead to height loss and muscle atrophy. These alterations due to prolonged sitting can be considered as the main causes of low back pain, stenosis of intervertebral foramen, and symptoms of legs diffusion pains (11, 12).
Therefore, it is reasonable to seek a solution for the treatment and prevention of intervertebral discs erosion and the weakness of core stability muscles in individuals working in sedentary jobs (13-15). In previous studies, a number of coping strategies such as manipulative therapy, physiotherapy, electrotherapy, water therapy, traction therapy, and therapeutic exercises have been proposed to deal with the loss of fluid in discs and prevent or treat damaged discs in individuals with sedentary jobs (16, 17). For instance, Billy et al. (2014) studied tensile movements during the daily work revealing that leaving chair and stretching every 15 min would preclude the loss of intervertebral disc height and consequently the possibility of intervertebral disc bulging (18). Kashi (2012), in his study on stretching exercises or walking and running while staying in the same place, indicated significant improvement in low back pain and disability of individuals in the experimental group (19).
We have to keep in mind that, under some circumstances, it might be not possible to perform such exercises, and employees may refuse to do so, whether due to the pressure on the vertebral column or exacerbation of the symptoms of low back pain by these exercises (20). Thereby, the main question and goal of this study are to design and construct a safe and practical device for proper suspension of the seat to soften the pressure on the intervertebral discs and allow core muscle stability exercises. Thus, we can examine the effect of this type of core stability exercises on the severity of pain, height variation, and herniation index in the L4-L5 and L5-S1 regions.
Materials and Methods
The present quasi-experimental study was performed with a pre- and post-test design on two groups of individuals. The participants consisted of 30 men with unilateral or bilateral lumbar and radicular leg pains due to lumbar disc herniation. The participants were randomly divided into two experimental groups (n=15 in each): conventional group (age: 43.4±8.6, height: 176.5±2.3 and weight: 87.7±6.5) and the suspension group (age: 37.2±5.3, height: 179.5±5.6 and weight: 87.0±7.4). During the eight weeks of training, three participants of the suspension group and two participants of the conventional group were dropped from the present study due to pain deterioration and personal reasons.
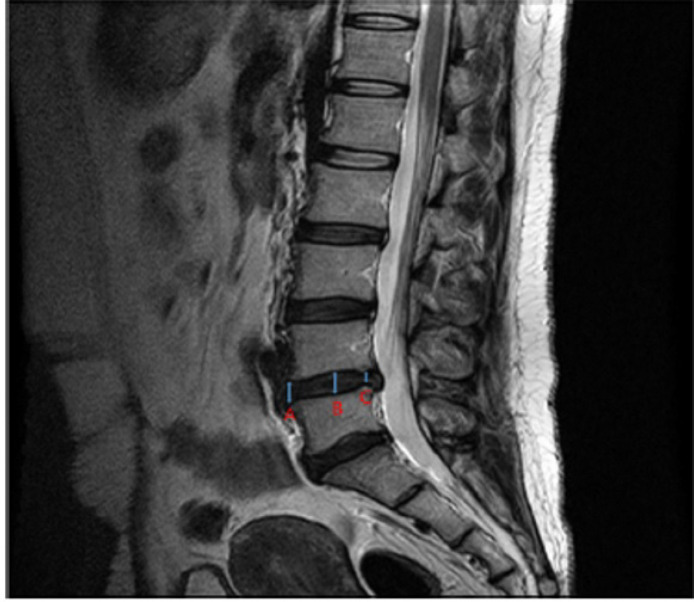
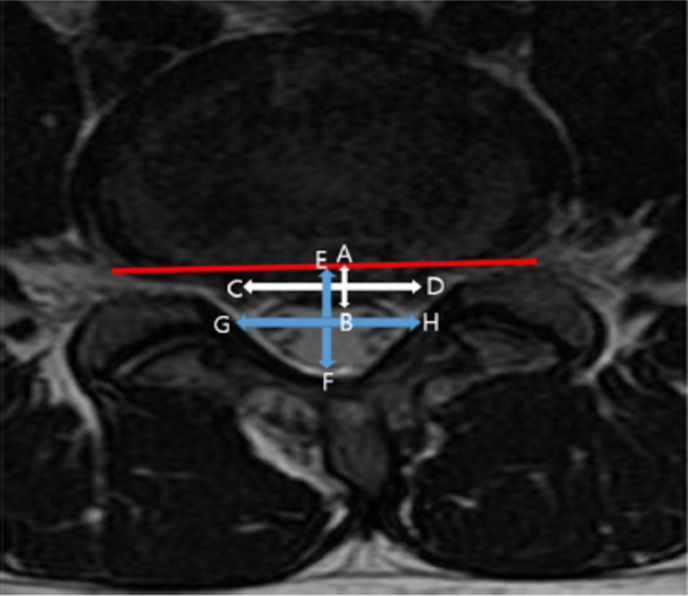
The participants were selected using convenient and target sampling. The sample population were recruited from a local-state hospital during a one-month period. Two orthopedic specialists at the hospital made the initial diagnosis based on Straight Leg Raising (SLR) and Gait Monitoring (GM) tests. After recording the demographic characteristics, their pain was also measured by a Visual Analog Scale (VAS). MRI was also performed to assess the structural characteristics (height and disc herniation index) of lumbar intervertebral disc (21). The vertebral height and disc herniation index were determined by using MRI (Magnetom Prisma Tim+Dot System 3 Tesla); the disc height was analyzed by using T2-weighted axial-section MRI; and the images were analyzed by using the PACS (picture archiving and communication system). The subject was laid supine with a cushion under their bent knees at a 25° angle. In this position, the lumbar vertebral L4 and L5 segments were photographed. The disc height was analyzed by using the image obtained [Figure 1]. The disc and intervertebral foramen were measured at the intercept of the axial direction. The sagittal distance of the herniated disc was recorded as the maximum anteroposterior disk height (AB), and that of the vertebral foramen was recorded as the maximum anteroposterior canal length (EF). The width of the herniated material was measured by drawing a line at the mid-level of the maximum anteroposterior disk length (CD). The width of the spinal canal was calculated at the same level (GH). The formula used for calculating the disc herniation index was ([AB ×CD]/ [EF ×GH]) ×1,000 [Figure 2] (21, 22).
Figure 1.
Suspension device
Figure 2.
measurement of disc height
Further, an orthopedic specialist approved their admission. The inclusion criteria were: (a) male office staff with chronic low back (CLB) and radicular leg pain due to lumbar disc herniation with a history of at least three months suffering, (b) age 30-50 years, and a posterolateral disc herniation in L4-L5 or L5-S1, (c) elicited pain in the leg, buttock, or back at 60 degrees of leg elevation as the diagnostic inclusion criterion for SLR. Sensitivity of this test is relatively 91% and its specificity is a typical of 26% (23). The heel strikes were ascertained in terms of vertical heel marker, stride time, and stride frequency; (d) all participants have to be normal from the perspective of these gate parameters (24). The exclusion criteria were: (a) Using pain-related medications three consecutive days before taking VAS (from no pain to maximal pain) both in pretest and posttest, (b) Smoking, (c) Previous back surgery, (d) Severe modification or fracture of the spine on X-ray, presence of an unstable medical condition or a known uncontrolled systemic disease, (e) “red flags sign” (i.e., serious spinal pathology or nerve root pain signs), (f) Any conditions or situations that might place the patient at significant risk during the study and individuals with less than three-month pain, (g) Pain of the other related areas including dorsiflexion, or neck flexion that might indicate other sources such as a lesion in the sacroiliac, lumbosacral, or hamstring area was a matter of exclusion in the present study, (h) female gender (23). Based on our protocol of intervention, we could not include female because every first four week over the present study the rate of pain was assessed by VAS. Therefore, having a group of female individual with different menstrual cycle were not possible to arrange for this weekly assessment. Participation in the present study was voluntarily. An informed consent letter was taken from participants and their participation was approved by the Ethics Committee of the University of Isfahan (IRCT20190115042365N1).
In the first stage of the present study, attempts were made to design and manufacture a prototype device for suspension exercises [Figure 3]. Then, in a pilot study, the effectiveness of the device in preventing injury or any complication in participants was investigated. Thus, under the observation of an orthopedic surgeon, five healthy volunteers (three males and two females) without any motor restrictions were asked to seat on the device. The individuals sat with their back facing the device and knees in a perpendicular position. The protective arms covered the upper body in the abdomen-chest region. the protective belt embraced their back and they placed their forearms on the specified area on the device. In this mode, they were able to lean and apply full weight on the device without trepidation. Afterwards, by pressing the control button of the actuator jack, the device was slowly and passively put in the suspended mode by either the subject or the therapist (when the device jack is operated, its seat is shifted downwards and the patient remains in suspension). When the patient seat was in complete suspension, the subject was able to carry out stability exercises or at least perform self-control traction to alleviate lumbar discs’ pressure and continue the designed exercises. Simultaneously, changes in blood pressure, heart rate, respiratory rate, and pressure of the device belt on the chest were recorded and studied.
Figure 3.
measurement of disc herniation index
In the second stage of present study after validation of the device by medical experts, the participants in both groups performed the designed protocols for eight weeks, three sessions per week. The participants in the conventional group preformed conventional core stability exercises for 30 minutes in each training session [Table 1] (21). The suspension group also preformed suspension core stability exercises while their buttock was suspended with the help of the device for 30 minutes in each training session [Table 2]. The ratios of exercise and resting times in suspended group were 2:1 and 60:30 sec, respectively. The change of training phases was determined according to the individuals’ conditions and over time. After eight weeks of training, all the related tests were performed again. Furthermore, the pain intensity was assessed in first, second, third, fourth, and eighth week.
Table 1.
Exercises protocol in conventional group
| Exercise schedule | exercises | time | stage | |
|---|---|---|---|---|
| General stretching exercises | Whole body General stretching exercises | 5 minutes | Warm up | |
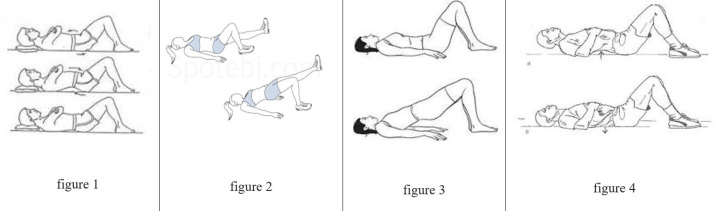
| Posterior tilt of the pelvis with bent knees (90 °) (Figure 1) hollow in maneuver with bent knees (90 °) (Figure 4) Anterior pelvic tilt with bent knee (90 °) (Figure 1) |
phase 1 | Core stability exercises | 20 minutes | Main exercises |
| lifting the hips on two legs with curved knees (90 °) (Figure 3) | phase 2 | |||
| lifting the hips on one leg with bent knees (90 °) (Figure 2) | phase 3 | |||
| Walking in and doing simple exercises | Aerobic and breathing exercises | 5 minutes | Cool down | |
Table 2.
Exercises protocol in suspension group
| Exercise schedule | Exercises | time | stage | |
|---|---|---|---|---|
| General stretching exercises | Whole body General stretching exercises | 5 minutes | Warm up | |
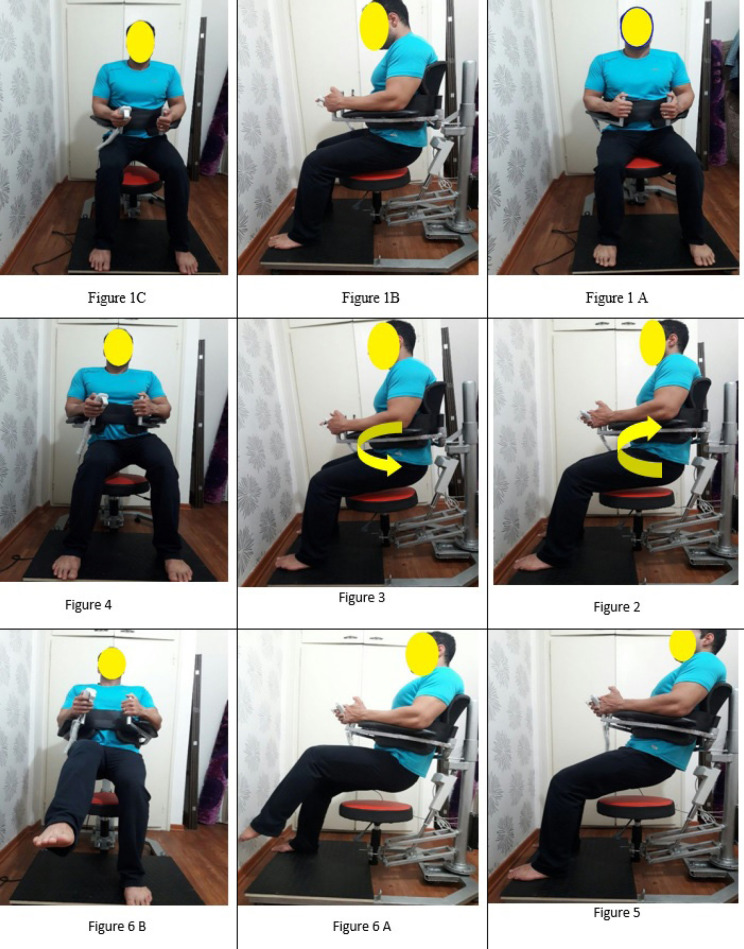
| Suspended hip ( figure 1) | stretching exercises | 20 minutes | Main exercises | |
| Posterior tilt of the pelvis with bent knees (90 °) (Figure 2) hollow in maneuver with bent knees (90 °) (Figure 2) Anterior pelvic tilt with bent knees (90 °) (Figure 3) lateral Pelvic tilt with bent knees (90 °) (Figure 4) |
phase 1 | Core stability exercises | ||
| Perform the previous stage exercises in addition for lifting the hips on two legs with curved knees (90 °) (Figure 5) |
phase 2 | |||
| Perform the previous stage exercises in addition lifting the buttocks on one leg with curved knees (90 °) (Figure 6) |
phase 3 | |||
| Walking in and doing simple exercises | Aerobic and breathing exercises | 5 minutes | Cool down | |
Results
Changes in all indexes including the L4-L5 and L5-S1 intervertebral disc height, herniation index in L4-L5 and L5-S1, and VAS were analyzed via paired-samples t-test to compare the pre- and post-test. Repeated measures analysis was used to compare the conventional and suspension groups.
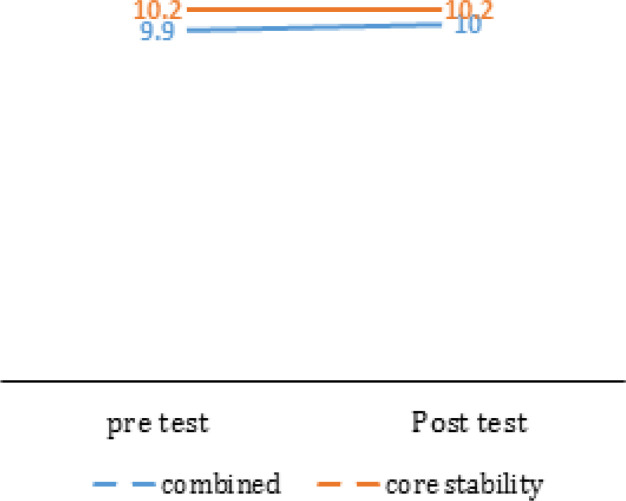
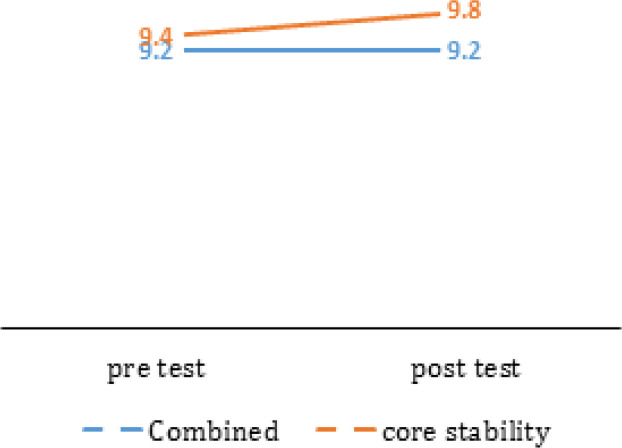
No significant change was seen in the height of the intervertebral discs in L4-L5 and L5-S1 (P<0.05) neither in the conventional nor the suspension group after 8 weeks of training. Besides, training, in both groups, did not make any significant change in herniation index in the L4-L5 and the L5-S1 (P<0.05). In other words, eight weeks of conventional and suspension training exercises did not have a significant effect on the characteristics of intervertebral disc in office staff with chronic pain due to lumbar disc herniation [Table 3].
Table 3.
characteristics of intervertebral discs
| index | Variable | area | Group |
stage
|
Intragroup changes
|
Intergroup changes
|
|||
|---|---|---|---|---|---|---|---|---|---|
|
Pre- test
M±SD |
Post -test
M±SD |
t | P | F | P | ||||
| Structural characteristic of intervertebral disc | Height | l4-l5 | Combined | 9.9±0.7 | 10±0.8 | -0.55 | 0.593 | 1.00 | 0.327 |
| core stability | 10.2±0.6 | 10.2±0.5 | -0.56 | 0.583 | |||||
| l5-s1 | Combined | 9.2±1.3 | 9±1.3 | -0.48 | 0.640 | 0.63 | 0.434 | ||
| core stability | 9.4±1.3 | 9.8±1.1 | -1.95 | 0.074 | |||||
| herniation index | l4-l5 | combined | 322.5±276.3 | 320.7±273.4 | 0.61 | 0.556 | 0.04 | 0.835 | |
| core stability | 351.9±224.0 | 332.9±219.7 | 0.83 | 0.425 | |||||
| l5-s1 | combined | 301.7±212.1 | 293.5±205.1 | 1.57 | 0.144 | 0.58 | 0.456 | ||
| core stability | 377.1±220.6 | 345.6±211.0 | 1.29 | 0.220 | |||||
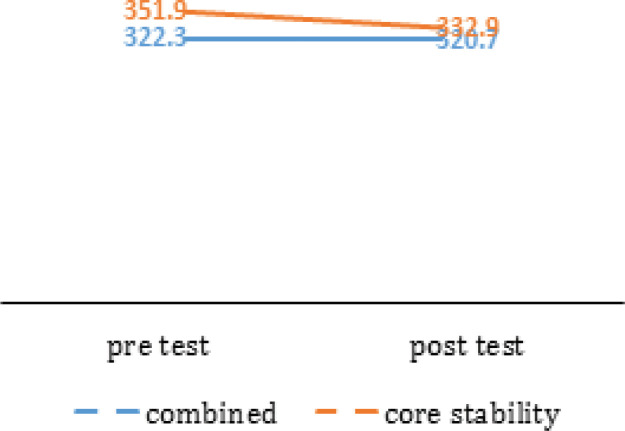
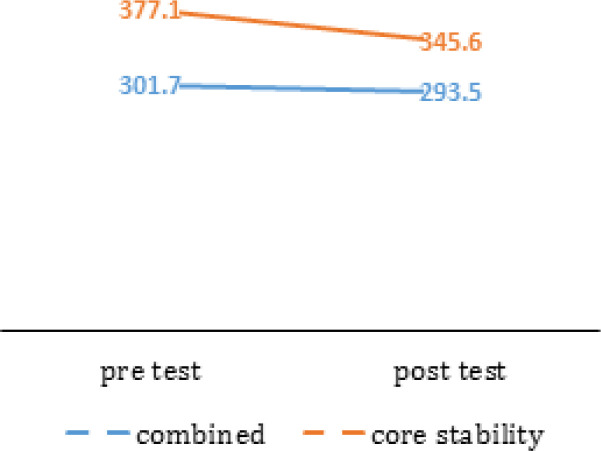
Charts 1 and 2 show a slight increase in the height of the intervertebral discs in L4-L5 and L5-S1 and Charts 3 and 4 show a slight decrease in herniation index in L4-L5 and L5-S1.
Chart 1.
Height of intervertebral discs l4-l5
Chart 2.
Height of intervertebral discs l5-s1
Chart 3.
Herniation index of intervertebral discs l4-l5
Chart 4.
Herniation index of intervertebral discs l5-s1
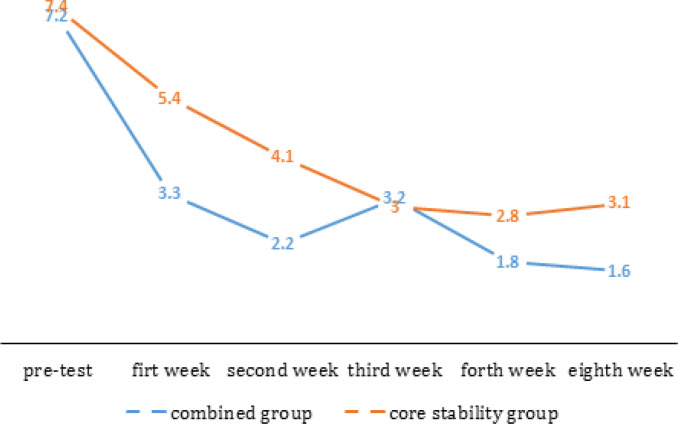
The results of the paired t-test indicated a significant decrease in pain intensity in both conventional and suspension groups after the first, second, third, and forth weeks (P<0.05) [Table 4]. However, only the individuals in suspension group experienced a significant decrease in pain in the second week compared to the first week (P<0.05). In the fourth week, the decrease in pain was only significant in the suspension group in comparison to the third week (P<0.05). Finally, in the eighth week (post-test), pain was not significantly improved in neither of the groups compared to the fourth week (P<0.05).
Table 4.
description pf pain during the 8 weeks
| Variable | stage | group | Mean ± standard deviation |
Intragroup changes
|
Intergroup changes
|
||
|---|---|---|---|---|---|---|---|
| t | P | F | P | ||||
| pain | Pre test (W0*) | combined | 7.2±1.6 | 12.85 (W0 and W8) | 0.001 | 3.06(W0 and W8) | 0.094 |
| Core stability | 7.4±0.9 | 9.2 (W0 and W8) | 0.001 | ||||
| First week (W1*) | combined | 3.3±2.3 | 6.82 (W0 and W1) | 0.001 | 3.31 (W0 and W1) | 0.082 | |
| Core stability | 5.3±2.1 | 3.95 (W0 and W1) | 0.002 | ||||
| second week (W2*) | combined | 5.2±2.3 | 1.68 (W1 and W2) | 0.121 | 11.93 (W1 and W2) | 0.002 | |
| Core stability | 4.1±2.1 | 2.42 (W1 and W2) | 0.032 | ||||
| third week (W3*) | combined | 3.2±1.4 | -2.34 (W2 and W3) | 0.039 | 3.61 (W2 and W3) | 0.07 | |
| Core stability | 3.0±1.6 | 2.74 (W2 and W3) | 0.018 | ||||
| forth week (W4*) | combined | 1.8±1.1 | 2.93(W3 and W4) | 0.014 | 0.71 (W3 and W4) | 0.408 | |
| Core stability | 2.8±1.2 | 0.47(W3 and W4) | 0.650 | ||||
| Eighth week (W8*) | combined | 1.6±1.5 | 1.39 (W4 and W8) | 0.191 | 5.02(W4 and W8) | 0.035 | |
| Core stability | 3.1±1.7 | -1.48 (W4 and W8) | 0.165 | ||||
* Abbreviation for each step or week.
In addition, the results of repeated measures analysis showed a significant difference in pain intensity between the conventional and suspension groups just in the first, second, fourth, and eighth weeks (P<0.05), but, no significant difference was seen between the two groups in rest of the weeks (P>0.05) [Table 4]. Therefore, it can be concluded that the effect of 8 weeks of conventional and suspension trainings on pain in office staff with chronic pain due to lumbar disc herniation has been quite significant (P<0.05).
The descending pain rate in conventional and suspension trainings group is presented in Chart (5).
Chart 5.
Changes in the degree of pain through weeks and stages by research groups
Figures of Table 1.
Figures of Table 2.
Discussion
Based on the results, eight weeks of conventional core stabilizing exercises and their combination with suspended exercises had a positive effect on pain alleviation and insignificant structural characteristics of the intervertebral discs L4-L5 and L5-S1. The insignificant changes in the structural characteristics of the discs were due to the limited exercise time of training (8 weeks) and uncontrolled sitting time of individuals at work (although they should have been sitting at least 6 to 8 hours a day). These findings undermined the effect of both suspended and conventional stabilizer exercises. Besides, the impossibility of accurate measurement by specialists due to blurring around MRI images, considering the millimeters scale of these changes, complicated the measurement and judgment.
A review of previous studies suggested that judgments were concerned with the total length of the spine. Simmerman and Boocock reported a general length of vertebrae in their study, but few studies have examined the thickness of one or two discs (1). Since the focus was on two discs in the present study, the lack of significant changes is completely normal. Moreover, since the device and exercises were specifically designed for lumbar area, evaluation of the entire spine length was not possible. With regard to the nutrition of the discs, it has been shown that remaining in a sedentary position for a long time diminishes the disc height and consequently decreases the disc fluid, which makes up almost 70% of disc herniations (7, 25). As a result of continuous pressure, it is not possible for the fluid to flow back in the discs through the distal plates of the vertebral body. It motivated the researchers like Deursen et al. (2000), to design a chair with a mobile seat that can automatically swivel at specific intervals. The results of their study revealed that using this movable chair precluded the negative effect of seating on the spine length (26). This is a reasonable way to protect against height loss in discs and improper disc nourishment. However, another important point to note is the kind of exercises that support the spine muscles during the process of degeneration and erosion of discs and long-term sitting in offices along with loss of disc height, suffering from weakness, shortage, and protective spasms (27). This is not possible by performing passive movements alone. In addition, using this movable chair on extending the spinal cord length is less effective than the effect of spinal traction tools which are either mechanical or self-controlled. For example, the results of studies on mechanical traction have revealed a 3.2-mm increase in lumbar intervertebral disc height in supine position and a 5-mm increase in vertical traction in the water (28). Traction in the reverse supine positional exhibited a 2.5-mm increase in lumbar intervertebral discs height after successive jumps (29). A gravity traction device installed in the water also presented up to 31 mm increase in the total height of the vertebral column (30). This height escalation, and consequently the unloading of pressure from the nerve roots as well as proper feeding of the intervertebral discs is highly important, but not everyone can afford to use pool due to its exorbitant costs or personal conditions.
In the case of inversion traction devices, there was a problem with increased intraocular pressure so that ophthalmologists advised not to use in many circumstances. Therefore, Podeinet al. designed a device that allowed gravity traction for the lumbar spine and individuals were able to perform core stability exercises in the suspension mode with hip and knee at an 90° angle as in most of mechanical and automatic traction controls, the patient is not able to control the intensity of the traction and the patient’s fear of pain leads to severe involuntary muscular contraction (30). This condition complicates the full recovery of the intervertebral discs and strengthening of the core stability muscles (31). The subject seats constantly on these devices and is strapped to the device. Using a Podein device, the subject is enabled to strengthen the stabilizing muscles and pelvic floor while the seat is suspended and lumbar traction is applied.
An important point during this exercise is to maintain a 90° hip angle and disengage the psoas muscle since Iliacus is the only muscle group that is attached directly to the spine, hip, and thigh. Therefore, it can indirectly transfer the mutual forces between the spine, pelvis, and thighs. The Iliacus is a postural muscle and, according to Janda, it is susceptible to shortness (32, 33). It has been suggested that 20 to 35 percent of normal people experience limited extension of hip joint due to shortened Iliacus muscles with a gradient of about 5° or more (34). In many studies, suspension exercises are executed in the case of hip joint extension, with this extension generating shear forces on the intervertebral discs and reducing disc space in the posterior region (33, 35). This important point was taken into consideration in the device designed by Podein et al., but their study did not discuss how exercises were performed and how effective they were (30).
Further, the literature on intervertebral discs has shown that the pressure and traction processes should be applied in parallel (36). In addition, the discs can exchange nutrients through this diffusion phenomenon (1, 37). Therefore, conditions must be provided so that pressure forces equal to the upper body weight of the individuals can be sought in traction intervals (38). For this to happen, the person should be able to bear his weight in the seated position for a short period that was included in our protocol. However, the problem is related to the patient’s control over sitting and standing in the face of pain and discomfort because the patient has trouble sitting and standing due to the pain and even fear of pain. The execution of these actions provokes protective spasms that hamper the treatment procedure and exacerbate the patient’s pain and distress (39).
In the present study, we decided to design and construct a device that is more complex and advanced than the one proposed by Podein for the prevention and treatment of intervertebral lumbar disc; especially intervertebral disc bulging and strengthening of stability muscles [Figure 3] (30). This device provided the patient with self-controlled traction so that they could perform conventional core stability exercises in the absence of compressive forces on the intervertebral discs and nerve roots while the body was in the suspended state. These exercises, which included pelvic tilts (anterior-posterior-lateral) and abdominal pull-in, mitigated the patient’s pain by relieving pressure from the nerve roots (40), and enabled the person to perform stability exercises. Moreover, during the training periods, the participants were able to sit on the device momentarily in a relatively passive and weight bearing state disregarding any fear of protective spasms with the aim of generating compressive force on the intervertebral discs, so that the pumping operation was expedited and the proper nutrition of the discs was achieved (35). However, another important point to note is that these kinds of exercises support the spine muscles, which in the process of degeneration and erosion of discs and long-term sitting in offices along with loss of disc height, suffer from weakness, shortage, and protective spasms (27). This is not possible by performing passive movements alone.
The present study suffers from two limitations including the lack of a control group and exclusion of female gender. Since it was morally inappropriate to maintain the control group without any treatment for eight weeks, we could not have a control group without any exercise or other methods of treatments in this study. To avoid the effects of women’s menstruation period and their different physical conditions, this study focused on the effect of suspension stability exercises on men solely. Being a female usually has the consequence of undergoing monthly menstruation; during which, she cannot participate in a procedure such as our physical intervention. Therefore, the researchers could not include female gender in the present study. Future studies are encouraged to conduct similar procedure considering this issue. Another reservation that might enhance the results of the present study was the use of Oswestry questionnaire. However, so as to the time limitation and the main focus which was pain measurement by VAS and the disc alteration measurements by MRI, the use of Oswestry questionnaire was overlooked.
Considering the beneficial effects of the designed device in relation to the pain relief and empowerment of participants, increased thickness of intervertebral discs and pressure reduction in nerve roots, it can be proposed as a useful therapeutic modality. Therefore, the individuals who suffer from disc-related pain can benefit from suspension and traction exercises. The use of this device relieves pain, reduces the use of sedatives and anti-inflammatory drugs, and can improve the quality of life from the perspective of pain reduction.
Patient consent: All participants have studied the conditions of the research and have completed the consent form.
Acknowledgements
We appreciate the respected personnel of Reza Imaging and Oncology Center-Mashhad, and all the dear participants who helped us with great patience in this research under the title of a doctoral thesis. It is worth mentioning that the financing of this research is the responsibility of the researcher.
This Manuscript has been read and approved by all the authors and each author believes that the manuscript represents honest work.
References
- 1.Chan SC, Ferguson SJ, Gantenbein-Ritter B. The effects of dynamic loading on the intervertebral disc. European Spine Journal. 2011;20(11):1796. doi: 10.1007/s00586-011-1827-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Choobineh A, Rajaeefard AR, Neghab M. Perceived demands and musculoskeletal disorders among hospital nurses. Hakim research journal. 2007;10(2):70–5. doi: 10.1080/10803548.2006.11076699. [DOI] [PubMed] [Google Scholar]
- 3.Sokas RK, Levy BS, Wegman DH, Baron SL. Recognizing and preventing occupational and environmental disease and injury. New York: Oxford University Press; 2011. [Google Scholar]
- 4.Aghilinejad M, Choobineh AR, Sadeghi Z, Nouri MK, Ahmadi AB. Prevalence of musculoskeletal disorders among Iranian steel workers. Iranian Red Crescent Medical Journal. 2012;14(4):198. [PMC free article] [PubMed] [Google Scholar]
- 5.Oha K, Viljasoo V, Merisalu E. Prevalence of musculoskeletal disorders, assessment of parameters of muscle tone and health status among office workers. Agron Res. 2010;8(1):192–200. [Google Scholar]
- 6.Das SM, Dowle P, Iyengar R. Effect of spinal mobilization with leg movement as an adjunct to neural mobilization and conventional therapy in patients with lumbar radiculopathy: Randomized controlled trial. J Med Sci Res. 2018;6(1):11–9. [Google Scholar]
- 7.Embleton J, Lines L. Spinal decompression therapy: Vibroseis of the body. InSEG Technical Program Expanded Abstracts. 2018:4787–4791. [Google Scholar]
- 8.Koçak FA, Tunç H, Sütbeyaz ST, Akkuş S, Köseoğlu BF, Yılmaz E. Comparison of the short-term effects of the conventional motorized traction with non-surgical spinal decompression performed with a DRX9000 device on pain, functionality, depression, and quality of life in patients with low back pain associated with lumbar disc herniation: A single-blind randomized-controlled trial. Turkish Journal of Physical Medicine and Rehabilitation. 2018;64(1):17. doi: 10.5606/tftrd.2017.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wegner I, Widyahening IS, van Tulder MW, Blomberg SE, de Vet HC, Brønfort G, et al. Traction for low-back pain with or without sciatica. Cochrane Database of Systematic Reviews. 2013:8. doi: 10.1002/14651858.CD003010.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eklund JA, Corlett EN. Shrinkage as a measure of the effect of load on the spine. Spine. 1984;9(2):189–94. doi: 10.1097/00007632-198403000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Sorkin JD, Muller DC, Andres R. Longitudinal change in the heights of men and women: consequential effects on body mass index. Epidemiologic reviews. 1999;21(2):247–60. doi: 10.1093/oxfordjournals.epirev.a018000. [DOI] [PubMed] [Google Scholar]
- 12.Weiner DK, Kim YS, Bonino P, Wang T. Low back pain in older adults: are we utilizing healthcare resources wisely? Pain Medicine. 2006;7(2):143–50. doi: 10.1111/j.1526-4637.2006.00112.x. [DOI] [PubMed] [Google Scholar]
- 13.van Tulder MW, Malmivaara A, Esmail R, Koes BW. Exercise therapy for low-back pain. Cochrane Database of Systematic Reviews. 2000(2) doi: 10.1002/14651858.CD000335. [DOI] [PubMed] [Google Scholar]
- 14.Cleland J, Schulte C, Durall C. The role of therapeutic exercise in treating instability-related lumbar spine pain: a systematic review. Journal of back and musculoskeletal rehabilitation. 2002;16(2-3):105–15. doi: 10.3233/bmr-2002-162-309. [DOI] [PubMed] [Google Scholar]
- 15.Kolar K. Lumbar-Disk Herniations: Conservative Clinical Applications. Athletic Therapy Today. 2005;10(5) [Google Scholar]
- 16.Gibbs BB, Hergenroeder AL, Perdomo SJ, Kowalsky RJ, Delitto A, Jakicic JM. Reducing sedentary behaviour to decrease chronic low back pain: the stand back randomised trial. Occupational and environmental medicine. 2018;75(5):321–7. doi: 10.1136/oemed-2017-104732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Benoist M. The natural history of lumbar disc herniation and radiculopathy. Joint Bone Spine. 2002;69(2):155–60. doi: 10.1016/s1297-319x(02)00385-8. [DOI] [PubMed] [Google Scholar]
- 18.Billy GG, Lemieux SK, Chow MX. Changes in lumbar disk morphology associated with prolonged sitting assessed by magnetic resonance imaging. PM&R. 2014;6(9):790–5. doi: 10.1016/j.pmrj.2014.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.GHAEINI S, KASHI A. THE EFFECT OF TRAINING MICROPAUSES ON FUNCTIONAL DISABILITY OF CHRONIC LOW BACK PAIN AFFECTED EMPLOYEES. 2012. [Google Scholar]
- 20.Mens JM, Snijders CJ, Stam HJ. Diagonal trunk muscle exercises in peripartum pelvic pain: a randomized clinical trial. Physical Therapy. 2000;80(12):1164–73. [PubMed] [Google Scholar]
- 21.Kang JI, Jeong DK, Choi H. Effect of spinal decompression on the lumbar muscle activity and disk height in patients with herniated intervertebral disk. Journal of physical therapy science. 2016;28(11):3125–30. doi: 10.1589/jpts.28.3125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fagerlund MK, Thelander U, Friberg S. Size of lumbar disc hernias measured using computed tomography and related to sciatic symptoms. Acta radiologica. 1990;31(6):555–8. [PubMed] [Google Scholar]
- 23.Ham P, Leiber JD. Chapter 11 - Physical Examination of the Lumbar Spine. In: Seidenberg PH, Beutler AI, editors. The Sports Medicine Resource Manual. Philadelphia: W.B. Saunders; 2008. pp. 100–9. [Google Scholar]
- 24.Huang YP, Bruijn SM, Lin JH, Meijer OG, Wu WH, Abbasi-Bafghi H, et al. Gait adaptations in low back pain patients with lumbar disc herniation: trunk coordination and arm swing. Eur Spine J. 2011;20(3):491–9. doi: 10.1007/s00586-010-1639-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jeong DK, Choi HH, Kang JI, Choi H. Effect of lumbar stabilization exercise on disc herniation index, sacral angle, and functional improvement in patients with lumbar disc herniation. Journal of physical therapy science. 2017;29(12):2121–5. doi: 10.1589/jpts.29.2121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Van Deursen DL, Goossens RH, Evers JJ, Van der Helm FC, Van Deursen LL. Length of the spine while sitting on a new concept for an office chair. Applied Ergonomics. 2000;31(1):95–8. doi: 10.1016/s0003-6870(99)00030-7. [DOI] [PubMed] [Google Scholar]
- 27.Lis AM, Black KM, Korn H, Nordin M. Association between sitting and occupational LBP. European Spine Journal. 2007;16(2):283–98. doi: 10.1007/s00586-006-0143-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Simmerman SM, Sizer PS, Dedrick GS, Apte GG, Brismée JM. Immediate changes in spinal height and pain after aquatic vertical traction in patients with persistent low back symptoms: a crossover clinical trial. PM&R. 2011;3(5):447–57. doi: 10.1016/j.pmrj.2011.01.010. [DOI] [PubMed] [Google Scholar]
- 29.Boocock MG, Garbutt G, Linge K, Reilly T, Troup JD. Changes in stature following drop jumping and post-exercise gravity inversion. Medicine and science in sports and exercise. 1990;22(3):385–90. [PubMed] [Google Scholar]
- 30.Podein RJ, Iaizzo PA. Applied forces and associated physiologic responses induced by axial spinal unloading with the LTX 3000™ lumbar rehabilitation system. Archives of physical medicine and rehabilitation. 1998;79(5):505–13. doi: 10.1016/s0003-9993(98)90063-6. [DOI] [PubMed] [Google Scholar]
- 31.Krause M, Refshauge KM, Dessen M, Boland R. Lumbar spine traction: evaluation of effects and recommended application for treatment. Manual therapy. 2000;5(2):72–81. doi: 10.1054/math.2000.0235. [DOI] [PubMed] [Google Scholar]
- 32.Janda V. The neurobiologic mechanisms in manipulative therapy. Springer; 1978. Muscles, central nervous motor regulation and back problems; pp. 27–41. [Google Scholar]
- 33.Jorgensson A. The iliopsoas muscle and the lumbar spine. Australian Journal of Physiotherapy. 1993;39:125. doi: 10.1016/S0004-9514(14)60477-3. [DOI] [PubMed] [Google Scholar]
- 34.Hellsing A, Nordgren B, Schele R, Ahlborg B, editors. Predictability of back pain around the age of 20. Reproducibility of examination variables: Proceedings of the Tenth International Conference of the World Confederation for Physical Therapy. Sydney; 1987. [Google Scholar]
- 35.Abbott EE, Lobo B, Benzel EC. Biomechanics of the Lumbar Degenerative Intervertebral Disk. Advanced Concepts in Lumbar Degenerative Disk Disease. Springer; 2016. pp. 305–10. [Google Scholar]
- 36.Gringmuth RH, Jackson C. Therapeutic exercise for spinal segmental stabilization in low back pain: scientific basis and clinical approach. The Journal of the Canadian Chiropractic Association. 2000;44(2):125. [Google Scholar]
- 37.Oh HJ, Jeon CB, Jeong MG, Choi SJ. The Effects of Spinal Decompression Therapy on Pain and Disability in Patients with Chronic Low Back Pain. The Journal of Korean Physical Therapy. 2017;29(6):299–302. [Google Scholar]
- 38.Steele J, Bruce-Low S, Smith D, Osborne N, Thorkeldsen A. Can specific loading through exercise impart healing or regeneration of the intervertebral disc? The Spine Journal. 2015;15(10):2117–21. doi: 10.1016/j.spinee.2014.08.446. [DOI] [PubMed] [Google Scholar]
- 39.Marshall PW, Murphy BA. Core stability exercises on and off a Swiss ball. Archives of physical medicine and rehabilitation. 2005;86(2):242–9. doi: 10.1016/j.apmr.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 40.Karimi N, Akbarov P, Rahnama L. Effects of segmental traction therapy on lumbar disc herniation in patients with acute low back pain measured by magnetic resonance imaging: A single arm clinical trial. Journal of back and musculoskeletal rehabilitation. 2017;30(2):247–53. doi: 10.3233/BMR-160741. [DOI] [PubMed] [Google Scholar]