Abstract
Background:
Angioleiomyomas are rare tumors arising from vascular tissue that can occasionally present in the hand. Reports of angioleiomyomas in this location are highly limited. Here, we describe the presentation and outcomes of a series of cases of angioleiomyomas.
Methods:
A retrospective case review of five patients with angioleiomyomas arising in the hand was performed. Patients were identified via International Classification of Diseases, Ninth and Tenth Revision (ICD-9 and ICD-10) diagnosis codes and were reviewed through the electronic medical record for demographic information, tumor characteristics, management, and outcomes. A literature review was also conducted of angioleiomyomas.
Results:
Five patients were diagnosed with angioleiomyoma at our institution between 1992 and 2015. Patients presented with a painful, slow-growing hand mass in all cases. The majority of patients were male and of middle-age. All of the patients were successfully treated with marginal excision and had full return to functional status without recurrence.
Conclusion:
Angioleiomyomas are rare tumors that can arise in the hand and should be included in the differential diagnosis of a patient presenting with a painful hand mass. They can be successfully treated with marginal excision.
Key Words: Angioleiomyoma, and tumors, ascular tumor
Introduction
Benign and malignant vascular tumors make up only a small proportion of tumors occurring in the hand and upper extremity and have an estimated incidence of approximately 8% in this location (1). Within this group, angioleiomyomas comprise a benign subgroup of vascular tumors that arise from the tunica media of subcutaneous vessels, themselves accounting for less than 1% of all soft tissue tumors in the upper extremity (2–6). These tumors are frequently painful and are often successfully treated with marginal excision (4).
In general, angioleiomyomas tend to occur in middle-aged adults, present more commonly in the lower extremity, and, when presenting in the lower extremity, have a predominance in females (7,8). Genetic inheritance has been suggested as a possible contributor to developing angioleiomyomas, with a proposed autosomal dominant inheritance pattern noted in familial cases, similar to lipomas (9).
Given their rarity, the diagnosis of angioleiomyoma in the hand is often initially overlooked, and they may be confused for giant cell tumors of the tendon sheath or ganglion cysts (4,10). These tumors may also be difficult to distinguish from giant cell tumors or ganglion cysts even on advanced imaging modalities such as magnetic resonance imaging (MRI), which may demonstrate non-specific findings of heterogeneity on T2-weighted imaging and appear isointense to muscle on T1-weighted imaging (11, 12). Nonetheless, it is important to consider angioleiomyoma as a potential diagnosis particularly when patients present with a painful mass in the hand or upper extremity, and biopsy should be considered in patients in whom the diagnosis is at all ambiguous.
Current literature on angioleiomyomas of the upper extremity and, specifically of the hand, is very limited (4, 13). In this case series, we report our experience with patients treated for angioleiomyomas of the hand and describe their demographics and clinical courses. Additionally, we present a review of the published literature about these tumors.
Materials and Methods
This was an Institutional Review Board (IRB)-approved, by the Partners IRB in Boston, Massachusetts, retrospective review of all patients treated at our institution, Massachusetts General Hospital in Boston, Massachusetts, for angioleiomyoma of the hand between the years of 1992 to 2015. A waiver for consent was obtained in all cases. Given the small sample size available, no inferential statistics and no a priori power analysis was able to be performed. Statistical analyses were carried out in the Statistical Package for the Social Sciences (SPSS) 25.0 (IBM). Patient demographic and surgical data was collected from the electronic medical record.
Results
Five patients presented with and were treated for angioleiomyoma of the hand between the years of 1992 and 2015. All patients were male. Four patients were Caucasian and one was Hispanic. The median age at presentation was 48.6 years of age (interquartile range [IQR] 38.8-57.3 years). One angioleiomyoma occurred in the dominant hand and three in the non-dominant hand; one patient did not have a recorded hand dominance. These patients had a median follow up of 75.8 months (IQR 30.3-160.7 months).
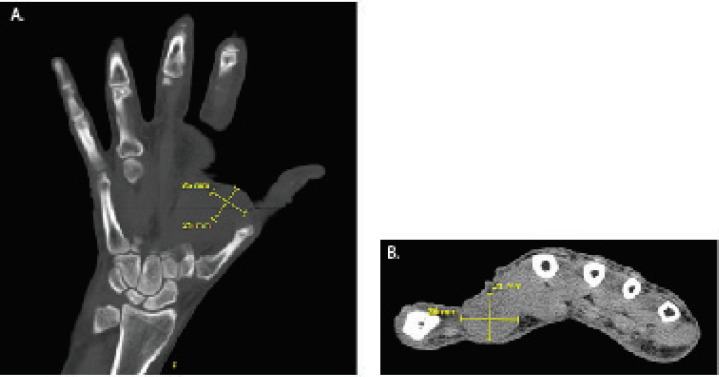
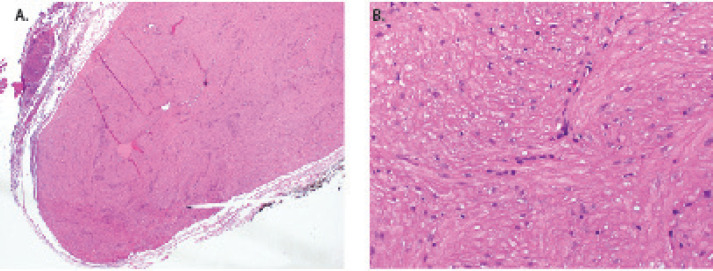
Tumors were located in the long finger, ring finger, fourth webspace, first webspace, and index finger. All patients presented with a painful, slow-growing mass. Two of the five patients reported fluctuating size of the mass and a periodically firm consistency. In three patients, a prior contusion at the eventual site of the angioleiomyoma was reported in the setting of a sports injury or hyperextension injury. A physical exam along with evaluation of medical history determined whether a CT or MRI of the affected region was necessary. All patients underwent routine radiographs of the hand [Figure 1]. Only one patient underwent a CT scan for preoperative evaluation, while the other four patients underwent excision without other advanced imaging studies; no patients underwent frozen section due to low concern for a malignancy given the superficial location of the masses, the history of indolent growth, as well as the small and well-circumscribed nature of the lesions [Figure 2]. The median volume of the tumor was 0.336 cm3 (IQR 0.28-3.18 cm3). Gross pathology showed a tan-yellow angioleiomyoma in case 1; lobulated tan-pink tissue with focal areas of hemorrhage in case 2; and masses with a bluish hue in cases 3, 4 and 5. Histology of the tumors in our series demonstrated a relatively minimal component of cavernous/dilated tissue and a large smooth muscle component [Figure 3]. In this series, no recurrences were observed [Table 1]. All patients had return to full functional status without any post-operative complications.
Figure 1.
Conventional radiograph of angioleiomyoma of the first webspace. There is a non-specific radiodensity noted in the first webspace representative of a soft tissue mass
Figure 2.
Angioleiomyoma of the first webspace. A. Coronal view B. Axial view. Largest dimensions are 25 x 25 mm on coronal imaging and 21 x 26 mm on axial imaging
Figure 3.
Hematoxylin and eosin staining of a representative angioleiomyoma from our patient series. A. 4X magnification and B. 40X magnification. Histology demonstrates a large smooth muscle component with a relatively rare cavernous tissue component
Table 1.
Demographic Patient Data and Angioleiomyoma Descriptive Data
| Case | Age (years) [Gender] | Follow-up (months) | Race | Location [Side] | Dominance | History | Diagnostics | Intraoperative Finding | Size (cm) | Volume (cm 3 ) |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 41.0 [M] | 3.5 | Caucasian | Long finger [L] | Right | Painful swelling, fluctuating size | None | Blueish mass with stalk | 1.2 x 0.7 x 0.4 | 0.336 |
| 2 | 50.1 [M] | 159.6 | Caucasian | Ring finger [L] | Right | Swelling, fluctuating size | None | Small mass from vein | 0.8 x 0.8 x 0.5 | 0.32 |
| 3 | 48.6 [M] | 161.8 | Caucasian | 4th webspace [R] | Not recorded | Swelling with blueish hue | None | Tumor with dilated peri-tumorous veins | 0.8 x 0.6 x 0.5 | 0.24 |
| 4 | 64.5 [M] | 57.1 | Caucasian | 1st webspace [R] | Right | Slow growing swelling | CT scan | Encapsulated glistening rubbery nodule | 2.5 x 2.0 x 1.2 | 6 |
| 5 | 36.5 [M] | 75.8 | Hispanic | Index finger [L] | Right | Swelling with blueish hue | None | Discrete firm mass | 1.0 x 0.9 x 0.4 | 0.36 |
M = Male, L = Left, R = Right
Discussion
Our cohort of five patients, though modest in sample size, recapitulated several known findings from prior series reported in the literature [Table 2]. Specifically, all of our patients presented with pain and complaints of a slow-growing mass. Additionally, surgical excision led to successful resolution in all cases in our series. Dimensions of the angioleiomyomas and the median age at presentation were also consistent with findings reported in the literature [Table 2]. Subjectively noted fluctuations in size were also reported by many in our cohort, and this has been previously noted in prior literature as well, though not specifically in the hand (14).
Table 2.
Angioleiomyoma Case Series in the Literature
| Author | N | Mean Age (years) | Most Common Location | Most Common Presenting Symptom | Mean or Range of Tumor Size (mm) | Most Common Histology | Most Common Treatment | Follow-up Time (years) | Recurrence Rate (%) | |
|---|---|---|---|---|---|---|---|---|---|---|
| Houdek et al. | 26 | 55 | Hand | Painful mass | 10 ± 7 | NR | Marginal excision | 1-21 | 0 | |
| Lawson et al. | 14 | 50 | Volar hand | Increasing size | 15 | Venous | Excision | NR | 0 | |
| Uchida et al. | 11 | 39 | Flexor surface | Increasing size | 12 | Solid | Simple excision | 11 | 0 | |
| Hachisuga et al. | 562 | 47 | Extremities | Pain | 2-43 | Solid | Excision | NR | 0.3 | |
| Kulkarni et al. | 1 | 49 | Dorsum | Painless swelling | 30 | Venous | Excision | 2 | 0 | |
mm = millimeters, NR=not reported
We note as a potential limitation in our study that there were (with the exception of one patient) no ultrasonography, advanced imaging studies undertaken, nor frozen section done at the time of excision. However, the rationale for this treatment strategy was due to the superficial and well-circumscribed nature of the masses, the small size of the lesions, and the history of indolent growth, making the diagnosis of a malignancy highly unlikely. This decision-making is in keeping with other prior published literature with regard to angioleiomyomas of the hand (4). Nonetheless, in all cases, patients were counseled that should the final pathology return as concerning for a malignancy, additional resections or adjunctive treatment might be required. In addition, if there is heightened concern for malignancy in the setting of features such as a deep location of the mass, larger size, or poorly defined borders, one should consider having frozen pathology available at the time of resection and include a pre-operative plan for a longitudinal incision that would accommodate a more extensile resection if needed based on frozen pathology results. In addition, these patients might also benefit from additional pre-operative advanced imaging or a pre-operative core needle biopsy rather than excisional biopsy as was the case in our series (4).
The histological findings in our series differed from those of angioleiomyomas reported in the literature. Specifically, while prior case series reporting on angioleiomyomas of the hand noted a large cavernous tissue component with vascular dilation and a small smooth muscle component, our histological findings noted minimal cavernous or dilated tissue and demonstrated a larger smooth muscle component (9).
With regard to this finding, prior classification systems proposed have divided angioleiomyomas into three subgroups: solid, venous, and cavernous. Solid angioleiomyomas have a primarily smooth muscle component with abundant, slit-like vasculature and are typically painful; venous tumors have little smooth muscle but thick muscular vessel walls; cavernous tumors have multiple dilated vascular channels difficult to distinguish from the muscle of the vessel channels (15). Based on this classification, the angioleiomyomas noted in our study appear to be most consistent with the solid subgroup. Immunohistochemical analysis was not performed in these specimens as the diagnosis was consistent with angioleiomyoma based on characteristic histological features alone, though prior immunohistochemical analyses of angioleiomyoma are frequently positive for alpha-smooth muscle actin, myosin, and h-caldesmon (2, 9, 15, 16).
Differential diagnosis of angioleiomyoma commonly include giant cell tumor, benign nerve sheath tumor, or ganglion cyst, but may also include lipoma or neuroma. Indeed, these conditions also present as subcutaneous, generally small masses that may be painful, particularly in the case of neuromas (16). Glomus tumors should also be considered, though these typically occur in the very distal extremity such as in the fingertip and are often found under the nail (17). Pain in angioleiomyomas has previously been postulated to result from local ischemia due to tumor vascularity or mass effect (2).
Angioleiomyomas have an unclear pathogenesis. Some studies have suggested a link to smooth muscle proliferation or a hamartomatous nature, while other studies point to a link to hormonal changes or trauma (2, 3, 18). Indeed, trauma was cited by a majority of patients in our study prior to the development of an angioleiomyoma, though there is a paucity of current literature to definitively support this.
Marginal excision appears to be sufficient to achieve complete resolution of the tumor, and prior studies have noted that patients are recommended for surveillance for one year after excision, followed by additional follow-up only if the patient develops new symptoms (4, 9).
In conclusion, angioleiomyoma are vascular tumors rarely found in the hand. We found in our case series that patients are often male and of middle age. In keeping with existing studies, angioleiomyomas of the hand can be successfully treated with marginal excision alone, and typically without need for preoperative advanced imaging studies given the usual benign features of a superficial location, indolent growth, and well-circumscribed nature and small size. Definitive diagnosis is often then made with histological analysis alone. Though rare, this diagnosis should be considered in patients who present with a painful mass in the hand with insidious onset and slow growth.
Disclosures: The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Acknowledgements
There are no acknowledgements.
References
- 1.Vandevender DK, Daley RA. Benign and malignant vascular tumors of the upper extremity. Hand Clin. 1995;11(2):161–81. [PubMed] [Google Scholar]
- 2.Hachisuga T, Hashimoto H, Enjoji M. Angioleiomyoma A clinicopathologic reappraisal of 562 cases. Cancer. 1984;54(1):126–30. doi: 10.1002/1097-0142(19840701)54:1<126::aid-cncr2820540125>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 3.Lawson GM, Salter DM, Hooper G. Angioleiomyomas of the hand A report of 14 cases. J Hand Surg Am. 1995;20(4):479–83. doi: 10.1016/s0266-7681(05)80157-3. [DOI] [PubMed] [Google Scholar]
- 4.Houdek MT, Rose PS, Shon W, Kakar S. Angioleiomyoma of the upper extremity. J Hand Surg Am. 2013;38(8):1579–83. doi: 10.1016/j.jhsa.2013.04.022. [DOI] [PubMed] [Google Scholar]
- 5.Kulkarni MS, Vijayan S, Naik M, Rao SK. A rare tumour of hand: angioleiomyoma. BMJ Case Rep. 2017;2017:bcr-2017-220005. doi: 10.1136/bcr-2017-220005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Freedman AM, Meland NB. Angioleiomyomas of the extremities: report of a case and review of the Mayo Clinic experience. Plast Reconstr Surg. 1989;83(2):328–31. [PubMed] [Google Scholar]
- 7.Park HJ, Kim SS, Lee SY, Choi YJ, Chung EC, Rho MH. Sonographic appearances of soft tissue angioleiomyomas: differences from other circumscribed soft tissue hypervascular tumors. J Ultrasound Med. 2012;31(10):1589–95. doi: 10.7863/jum.2012.31.10.1589. [DOI] [PubMed] [Google Scholar]
- 8.Smith J, Wisniewski SJ, Lee RA. Sonographic and clinical features of angioleiomyoma presenting as a painful Achilles tendon mass. J Ultrasound Med. 2006;25(10):1365–8. doi: 10.7863/jum.2006.25.10.1365. [DOI] [PubMed] [Google Scholar]
- 9.Woo KS, Kim SH, Kim HS, Cho PD. Clinical Experience with treatment of angioleiomyoma. Arch Plast Surg. 2014;41(4):374–8. doi: 10.5999/aps.2014.41.4.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Callé SC, Eaton RG, Littler JW. Vascular leiomyomas in the hand. J Hand Surg Am. 1994;19(2):281–6. doi: 10.1016/0363-5023(94)90020-5. [DOI] [PubMed] [Google Scholar]
- 11.Yoo HJ, Choi JA, Chung JH, Oh JH, Lee GK, Choi JY, et al. Angioleiomyoma in soft tissue of extremities: MRI findings. Am J Roentgenol. 2009;192(6):W291–4. doi: 10.2214/AJR.07.3952. [DOI] [PubMed] [Google Scholar]
- 12.Hwang JW, Ahn JM, Kang HS, Suh JS, Kim SM, Seo JW. Vascular leiomyoma of an extremity: MR imaging-pathology correlation. Am J Roentgenol. 1998;171(4):981–5. doi: 10.2214/ajr.171.4.9762979. [DOI] [PubMed] [Google Scholar]
- 13.Uchida M, Kojima T, Hirase Y, Lizuka T. Clinical characteristics of vascular leiomyoma of the upper extremity: report of 11 cases. Br J Plast Surg. 1992;45(7):547–9. doi: 10.1016/0007-1226(92)90153-o. [DOI] [PubMed] [Google Scholar]
- 14.Kanitakis J. Angioleiomyoma of the auricle: an unusual tumor on a rare location. Case Rep Otolaryngol. 2017;2017:8289710. doi: 10.1155/2017/8289710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Morimoto N. Angioleiomyoma [vascular leiomyoma]-a clinicopathologic study. Med J Kagoshima Univ. 1974;24(1):663–6. [Google Scholar]
- 16.Matsuyama A, Hisaoka M, Hashimoto H. Angioleio-myoma: a clinicopathologic and immunohistochemical reappraisal with special reference to the correlation with myopericytoma. Hum Pathol. 2007;38(4):645–51. doi: 10.1016/j.humpath.2006.10.012. [DOI] [PubMed] [Google Scholar]
- 17.Shafi M, Hattori Y, Doi K. Angioleiomyoma of distal ulnar artery of the hand. Hand (N Y) 2010;5(1):82–5. doi: 10.1007/s11552-009-9200-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gombos Z, Zhang PJ. Glomus tumor. Arch Pathol Lab Med. 2008;132(9):1448–52. doi: 10.5858/2008-132-1448-GT. [DOI] [PubMed] [Google Scholar]