Abstract
Background:
Surgery in the time of COVID-19 pandemic is a challenging issue while treatment of affected fracture patients is inevitable. The present study summarizes the challenges that an orthopedic surgeon is confronting during the surgical treatment of fracture patients with concomitant COVID-19 infection.
Methods:
Demographic and fracture related data of 13 fracture patients with concomitant COVID-19 infection who were treated with surgery was collected from three trauma centers in Tehran and Kermanshah cities from 21, February 2020 to April 3, 2020.
Results:
All patients were male with mean age of 38.6±19.5 years. Eight patients had high energy fracture and seven patients had multiple fractures and trauma. Wrist and hand were the common sites of fracture following hip and pelvis. The mean interval time period between the diagnosis of COVID-19 infection and surgery was 2.3±1.5 days. Before surgery, all patients except one had been admitted to the corona dedicated wards, while two patients were admitted to the intensive care unit (ICU). One of the ICU admitted patients died. All the 12 alive patients remained in home isolation after discharge.
Conclusion:
Fracture surgery in COVID-19 patients has many challenges such as lack of medical resources, delay of surgery, medial staff fear, and patient isolation. However, a multidisciplinary approach using all potential hospital resources would lead to successful operation and acceptable outcome.
Key Words: oronavirus, COVID-19, racture, Orthopedic, rauma
Introduction
In the last month of 2019, before celebrating the new year, reports of a new life-threatening pneumonia outbreak in Wuhan shocked China. Early investigations showed coronavirus as the cause of this new type of pneumonia. On January 7, 2020, Chinese researchers succeeded in isolating the novel coronavirus named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (1). WHO was named coronavirus disease 2019 as COVID-19 on 11, February 2020. Considering the highly contagious nature and rapid spread of COVID-19 worldwide, it became a global health emergency as the director-general of WHO on March 11, 2020, announced the situation as a pandemic (2). Iran was one of the first countries to report COVID-19 on February 19. The known cases of the disease increased up to 70029 until April 23, 2020, according to WHO (3, 4).
Iran has a high rate of road traffic accidents, where 226,514 people died from 2006 to 2016 (5). A high number of orthopedic surgeries are done for the treatment of traumatic injuries in Iran. Despite social quarantine from the beginning of COVID-19 pandemic, orthopedic surgeons in Iran are still dealing with noticeable numbers of trauma patients; some of whom have been infected with COVID-19. Surgery in COVID-19 patients is a challenging issue, so is the treatment of fracture patients with COVID-19 (6,7). We conceive this study to investigate the challenges that an orthopedic surgeon is confronting during the surgical treatment of fracture patients with known COVID-19 infection.
Materials and Methods
In this case series study, the data of 17 consecutive patient admitted to three trauma centers (Shohada Tajrish and Imam Hossein Hospitals, Shahid Beheshti University of Medical Science, Tehran, Iran and Taleghani Hospital, Kermanshah University of Medical science, Kermanshah, Iran) with orthopedic trauma and concomitant COVID-19 infection were studied between 21, February 2020 and April 3, 2020.
Low dose high resolution computed tomography (HRCT) was used to diagnose COVID-19 infection in all patients as a routine protocol (8). Four cases who were treated with non-operative methods excluded from the study .Two patients with Lisfranc injury and lumbar spine fracture had no indications for surgery and were treated by casting and brace. One patient with pathological humerus fracture died before surgery and one patient with intertrochanteric fracture and concomitant acute deep vein thrombosis was treated non-operatively. Finally, 13 cases with confirmed diagnoses before surgical treatment were enrolled in the study.
Demographic data including age, gender, body mass index (BMI), and educational level were collected from patients’ records. The data pertaining to the time interval between COVID 19 diagnosis to surgery, hospitalization duration after surgery, isolation protocols, mortality, and finally patient residence situation after discharge from hospital were documented. The data related to orthopedic injury included fractures or injury sites, mechanism of fracture, associated injuries, and duration of surgery time were also documented. All data were analyzed with SPSS software (version 23.0; IBM).
Results
All 13 patients (100 %) were males with age ranging from 17 to 81 years (38.6±19.5). BMI ranged from 19.1 to 30.7 (24.5±2.76). Three patients had academic degrees (23.0 %), four had high school diplomas (30.7 %), and six patients had not completed high school (46.1 %).
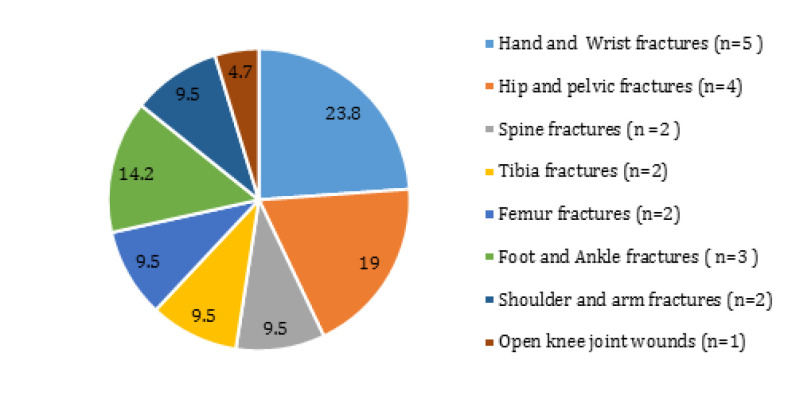
Eight patients (61.5 %) had high energy fractures following road traffic accidents while five patients (38.4 %) had low energy traumas including slipping or direct trauma. Seven out of 13 patients (53.8 %) had multiple traumas and fractures [Table 1]. Common associated injuries were head injury in five patients and chest trauma in three cases following one case of abdominal injury and one patient with cord injury. Chest tube was inserted for two patients and other associated injuries were treated conservatively. Two patients had more than one associated injuries. Figure 1 shows the location distribution of fractures in all patients. Wrist and hand were the common sites of fractures followed by hip and pelvis. Nine patients had at least one fracture in the lower extremity, whereas four patients had only upper limb fractures alone [Table 1]. All patients underwent 17 orthopedic surgeries with a mean surgery time duration of 2.7±1.4 hours.
Table 1.
Orthopedic trauma and COVID-19 patient’s data (BMI: Body Mass Index, RTA: Road Traffic Accident, h: hours)
| Age | Gender | Education | BMI | Trauma mechanism | Fracture site | Associated injuries | Surgery time duration | Days between COVID-19 diagnosis and surgery | Days of hospitalization after surgery | Mortality | Residence situation after discharge | Ward | CRP level before surgery | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 24 | M | Bachelor | 25.9 | RTA | Open knee joint | - | 0.5h | 5 | 3 | No | Home | Corona ICU | 55 | |
| 2 | 25 | M | Unfinished education | 26.2 | RTA | Femoral shaft fracture, scaphoid fracture ,bimaleolar fracture | Head | 4h | 1 | 4 | No | Home | Corona | 59 | |
| 3 | 23 | M | Unfinished education | 19.1 | RTA | Distal femur fracture | Head | 6h | 1 | 5 | No | Home | Clean | 44 | |
| 4 | 28 | M | High school diploma | 22 | RTA | Subtrochanteric fracture ,lisfranc injury | Head | 4h | 2 | 2 | No | Home | Corona | 97 | |
| 5 | 61 | M | PHD in History | 24.4 | Slipping | Distal radius fracture | - | 1h | 1 | 3 | No | Home | Corona | 35 | |
| 6 | 27 | M | High school diploma | 23.3 | RTA | Tibia and fibula fracture , proximal humerus fracture, cervical spine fracture | Head , Chest ,Cord injury | 4 h | 6 | 7 | Yes | Home | Corona ICU | 30 | |
| 7 | 29 | M | Unfinished education | 24.1 | RTA | Intertrochanteric fracture, shoulder fracture-dislocation ,cervical spine fracture | Head , Chest ,Abdomen | 3h | 5 | 5 | No | Home | Corona | 102 | |
| 8 | 81 | M | High school diploma | 24.1 | Slipping | Intertrochanteric fracture | - | 3h | 1 | 2 | No | Home | Corona | 65 | |
| 9 | 61 | M | Associate degree | 23.6 | Slipping | Distal radius fracture | - | 1.5 h | 1 | 1 | No | Home | Corona | 71 | |
| 10 | 17 | M | Unfinished education | 23.6 | RTA | Tibia and fibula fracture | - | 2h | 3 | 2 | No | Home | Corona | 55 | |
| 11 | 54 | M | Unfinished education | 27.6 | Slipping | Distal radius fracture | Chest | 1.5h | 3 | 3 | No | Home | Corona | 34 | |
| 12 | 44 | M | Unfinished education | 24.4 | Direct trauma |
Metacarpus 1 fracture with tendon injury | - | 2h | 1 | 5 | No | Home | Corona | 28 | |
| 13 | 29 | M | High school diploma | 30.7 | RTA | Pelvic fracture , Bimalleolar fracture | Chest | 3h | 1 | 5 | No | Home | Corona | 60 |
Figure 1.
Distribution of fracture sites.
The mean time period between diagnosis of COVID-19 infection and surgery was 2.3±1.5 days in all 13 patients, 2.7±1.9 in multiple trauma group, and 1.7±1.5 in a single trauma group. The surgery to discharge meantime was 3.6±2.8 days in all groups, 4.4±1.5 in multiple trauma group, and 2.2±1.2 in a single trauma group [Table 2].
Table 2.
Surgery time duration, Days between COVID-19 diagnosis and surgery, Days of hospitalization after surgery in multiple trauma group and single trauma group
| Multiple trauma (n=7) | Single trauma (n=6) | P – value | |
|---|---|---|---|
| Surgery time duration (hours) | 3.6 ±1.2 | 1.4 ±0.8 | p> o.05 |
| Days between COVID-19 diagnosis and surgery (days) | 2.7 ±1.9 | 1.7 ± 1.5 | p> o.05 |
| Days of hospitalization after surgery (days) | 4.4 ± 1.5 | 2.2 ± 1.2 | p > o.05 |
Before surgery, all patients had been admitted to the corona dedicated wards except one patient who was hospitalized in the non-corona ward and two patients who were admitted to the corona intensive care unit (ICU). The reasons for admission to ICU were loss of consciousness in one multiple trauma patient with head trauma with Glasgow Coma Score of 9 and oxygen saturation drop in one patient with knee wound. Postoperatively, two patients were transferred to the corona ICU and the rest were sent to the corona wards.
One of the ICU admitted cases died after cervical spine fixation surgery due to COVID-19 pneumonia and severity of the injury including head and chest trauma. All 12 alive patients remained in home isolation after discharge.
Discussion
The treatment of fractures that require surgical intervention is usually urgent. During the COVID-19 pandemic in countries like Iran with a high rate of road traffic accidents, it is not uncommon to see patients with fracture and concomitant COVID-19 infection. There is little information in the literature regarding the surgical management of fracture in COVID-19 patients (9, 10). We developed this study to clarify the issues orthopedic surgeons have confronted in these circumstances.
Our study showed that eight out of 13 patients were younger than 30 years and most of them suffered from high energy trauma. The milder symptoms of COVID-19 infection in younger patients and the multi-trauma nature of the cases made the diagnosis of COVID-19 infection more difficult and the first challenge for the surgeons. Also, the management of multiply injured patients needs a multidisciplinary approach as well as a well-equipped ICU (11). Shortage of medical resources is a concern in pandemic and management of trauma patients in crisis needs careful triage for optimal use of hospital facilities (12, 13). However, unavailability of ICU beds is another challenge at the time of epidemics and therefore some patients may be admitted to floors rather than ICU. The situation is more complicated if the multiple trauma patients have concomitant COVID-19 infection. For this reason, we could admit only two of the seven multiple injured patients in ICU.
The other challenge for the surgeon is the delay in the surgery in COVID-19 patients. The main reason for this lag is the fact that infectious disease specialists and pulmonologists should clear the patient for the operation (14). This delay in surgical fixation of fracture patients can increase the mortality and morbidity rates of inadequately resuscitated and stable patients (15). The delay in surgery was more in multiple trauma patients in our study which could be related to non-orthopedic traumatic injuries that needed further intervention.
Isolation of patients with COVID-19 is another challenge for an orthopedic surgeon. All patients should be transferred to a special corona ward, and it is essential to reduce disease transmission. Separate floors were dedicated for COVID patients but sometimes the shortage of corona dedicated beds might have obliged the treating physicians to transfer patients to the clean ward as it happened in one of the patients in this study. In this case, it is necessary to alarm all physicians and healthcare workers of this mismatch to follow the standard personal protective measures.
In our experience, the fear of operating room staff is another problem. It may affect the quality of service patients receive. To solve this problem, we started with education about the COVID-19 characteristics, personal protection guidelines, and necessity of surgery in these complex patients. Then we equipped them with standard personal protection equipment. Using these strategies, most physicians, nurses, and medical staffs found their way from fear zone to the growth zone through learning. The mean time of hospitalization after surgery was 3.6±2, and there was no significant difference between the multiple and single trauma groups. It seems that COVID-19 infection elongated hospitalization period because of the delay before surgery and long hospital stay after it. As the patient is still a COVID-19 carrier, another issue is where to discharge the patient. If patient goes home, other households might get infected. If the patient stays at the hospital, the risk of nosocomial infection will increase. Therefore, we decided to send patients home with all instructions regarding isolation and household protection.
The last but not least challenge was the postoperative patient rehabilitation. Nine of 13 patients in this study suffered from lower extremity fractures and all of them were transferred to home isolation after discharge. Inability to walk without help and home isolation make the postoperative care and rehabilitation of these patients very complicated. We believe that family education about the ways of transmission and personal protection as well as providing them with the necessary equipment might be a solution to this problem (16). Patient follow ups were done through phone calls.
The mortality rate in our study was low at 7.6% comparing to 40% reported by Bobin et al. (9). This difference could be due to several reasons. First, their patients were older than ours. Second, they treated their patients non-operatively, and only three patients in their cohort underwent surgery. Third, the younger age of our patients was associated with milder forms of COVID-19 infection. Despite this, the surgical intervention and mobilizing patients as soon as possible might have played a role in better survival of our patients.
Our study had several significant limitations. It was a retrospective study of cases that forms multiple centers with all potential weaknesses of a retrospective study. Furthermore, the follow up duration was short. The diagnosis of COVID-19 was based on HRCT, so we included patients in a different stage of the disease. Fourth, we did not take into account the duration of COVID-19 infection before the patient’s appearance in the hospital.
We believe that the above shortcomings do not undermine the main findings of this study. Fracture surgery in COVID-19 infected patient is a challenging procedure from preoperative period up to the rehabilitation. However, a multidisciplinary approach using all potential hospital resources would lead to successful operation and acceptable outcomes.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Funding:
There is no funding source.
Conflict of Interests:
The authors declare that they have no conflict of interest.
References
- 1.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. The Lancet. 2020 Mar 11; doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bedford J, Enria D, Giesecke J, Heymann DL, Ihekweazu C, Kobinger G, Lane HC, Memish Z, Oh MD, Schuchat A, Ungchusak K. COVID-19: towards controlling of a pandemic. The Lancet. Mar ;:17. doi: 10.1016/S0140-6736(20)30673-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO official site. https://who.sprinklr.com.
- 4.Shariyate MJ, Kachooei AR. Association of New Coronavirus Disease with Fragility Hip and Lower Limb Fractures in Elderly Patients. Arch Bone Jt Surg. 2020;8(Supplement 1):297–301. doi: 10.22038/abjs.2020.47626.2333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shahbazi F, Soori H, Khodakarim S, Ghadirzadeh MR, Nazari SS. Analysis of mortality rate of road traffic accidents and its trend in 11 years in Iran. Archives of Trauma Research¦ Volume. 2019 ;8(1) [Google Scholar]
- 6.Ashford RU, Nichols JS, Mangwani J. Annotation: The COVID-19 pandemic and clinical orthopaedic and trauma surgery. Journal of Clinical Orthopaedics & Trauma. 2020 Apr ; doi: 10.1016/j.jcot.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abolghasemian M, Ebrahimzadeh MH, Enayatollahi M, et al. Iranian Orthopedic Association (IOA) Response Guidance to COVID-19 Pandemic April 2020. Arch Bone Jt Surg. 2020;8(Supplement 1):209–217. doi: 10.22038/ABJS.2020.47678.2370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mahdavi A, Khalili N, Davarpanah AH, Faghihi T, Mahdavi A, Haseli S, Sabri A, Kahkouee S, Kazemi MA, Mehrian P, Falahati F. Radiologic management of COVID-19: preliminary experience of the Iranian Society of Radiology COVID-19 Consultant Group (ISRCC) Iranian Journal of Radiology. 2020 In Press) [Google Scholar]
- 9.Mi B, Chen L, Xiong Y, Xue H, Zhou W, Liu G. Characteristics and Early Prognosis of COVID-19 Infection in Fracture Patients. JBJS. 2020 Apr; doi: 10.2106/JBJS.20.00390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Abdi R, Shojaeian R, Hajian S, Sheikh S. Surgical practice in the shadow of COVID-19 outbreak. The Archives of Bone and Joint Surgery. 2020 ;8(Covid-19 Special Issue):0–9. doi: 10.22038/abjs.2020.47757.2348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chua C, Wisniewski T, Ramos A, Schlepp M, Fildes JJ, Kuhls DA. Multidisciplinary trauma intensive care unit checklist: impact on infection rates. Journal of Trauma Nursing. 2010 ;17(3):163–6. doi: 10.1097/JTN.0b013e3181fb38a6. [DOI] [PubMed] [Google Scholar]
- 12.Xie J, Tong Z, Guan X, Du B, Qiu H, Slutsky AS. Critical care crisis and some recommendations during the COVID-19 epidemic in China. Intensive care medicine. 2020 Mar ; doi: 10.1007/s00134-020-05979-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Khak M, Manafi-Rasi A, Oryadi Zanjani L, et al. Orthopedic Trauma Surgeries in COVID-19 Pandemic; A Trauma Management Algorithm. Arch Bone Jt Surg. 2020;8(Supplement 1):286–290. doi: 10.22038/abjs.2020.47741.2344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kalantar SH, Farhoud AR, Mortazavi SMJ. Lockdown of an Orthopedic Department During COVID-19 Epidemics, Our Experience in a General Hospital. Arch Bone Jt Surg. 2020;8(Supplement 1):235–241. doi: 10.22038/abjs.2020.47834.2362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vallier HA, Wang X, Moore TA, Wilber JH, Como JJ. Timing of orthopaedic surgery in multiple trauma patients: development of a protocol for early appropriate care. Journal of orthopaedic trauma. 2013 ;27(10):543–51. doi: 10.1097/BOT.0b013e31829efda1. [DOI] [PubMed] [Google Scholar]
- 16.Chehrassan M, Ebrahimpour A, Ghandhari H, et al. Management of Spine Trauma in COVID-19 Pandemic: A Preliminary Report. Arch Bone Jt Surg. 2020;8(Supplement 1):270–276. doi: 10.22038/abjs.2020.47882.2368. [DOI] [PMC free article] [PubMed] [Google Scholar]