Abstract
Patellofemoral (PF) osteoarthritis (OA) is a somewhat predominant illness, affecting up to 24% of women and 11% of men over the age of 55 years who suffer from symptomatic knee OA. The purposes of this narrative overview are to summarize the present situation of patellofemoral arthroplasty (PFA) in the treatment of solitary PF-OA, and to give an account of the clinical results of PFA for the management of solitary PF degenerative OA of the knee. A Cochrane Library and PubMed (MEDLINE) examination related to the position of PFA in PF-OA was carried out. A number of publications have encountered that PFA is an efficacious treatment for solitary PF-OA. Additionally, a systematic review described fairly good results of PFA survivorship and functional outcomes at short- and mid-run follow-up in the setting of solitary PF-OA. Success of PFA depends on accurate patient selection rather than prosthetic failure or wear. In many reports, the main cause of PFA failure is advancement of tibiofemoral OA. In contemporary times, encouraging results have been accomplished by the association of PFA and unicompartmental knee arthroplasty (UKA). In conclusion, patients with solitary PF-OA with severe anterior knee pain may be candidates for PFA. The success of the surgical procedure and the long-run survivorship of PFA are related to a good surgical technique and observation to meticulous indications and contraindications in patient selection. Newer prostheses have also played a part to ameliorated outcomes. PFA is an alternative for younger patients with solitary PF-OA.
Key Words: Isolated patellofemoral osteoarthritis, Management, patellofemoral arthroplasty, Results
Introduction
Patellofemoral (PF) osteoarthritis (OA) is a somewhat predominant illness affecting up to 24% of women and 11% of men over the age of 55 years who have symptomatic knee OA (1). Isolated symptomatic PF-OA has been reported in 2% of men and 8% of women older than the age of 55 years whereas it is reported in 9% of radiographs of symptomatic knees in people over the age of 40 years (2). Approximately 75% of all PF arthroplasties (PFAs) are performed in women, and the augmented incidence of PF disease may be related to the incidence of knee malalignment and dysplasia in women, although some reports have observed no sex-specific differences in knee kinematics (3).
PFA is one of the existing options designed to confront with pain elicited by severe, isolated PF-OA (4). PFA abides debatable, principally due to the high failure rates published with early designs. Many case series have been reported over the years (5).
Isolated PF-OA has received minimal attention in the past. It is now acknowledged to be relatively prevalent, especially in women. Treatment options such as patellectomy, unloading osteotomies, debridement, and cartilage transplant have not yielded long-term endurable benefits. Therefore, there is a necessity for a dependable PFA (6, 7).
The objectives of this narrative overview are to establish the present situation of PFA in the management of solitary PF-OA, and to give a description of the clinical outcomes of PFA for the treatment of solitary PF degenerative OA.
Materials and Methods
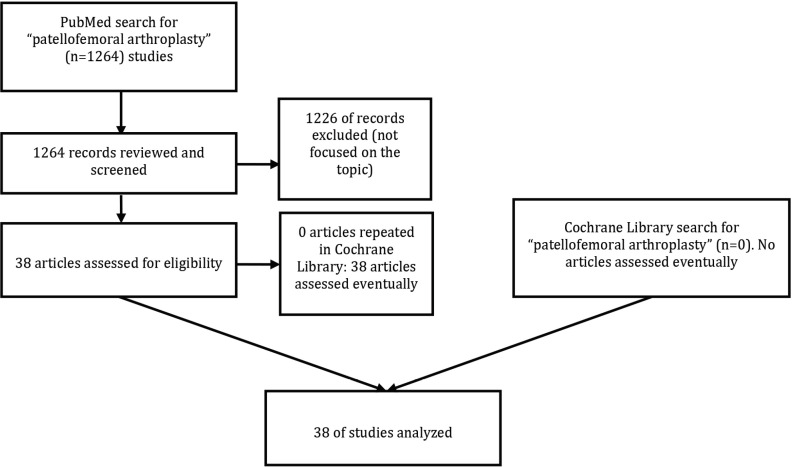
A Cochrane Library and PubMed (MEDLINE) search related to the role of PFA in PF-OA was carried out. The main criteria for selection were that the articles were focused in the role of PFA in PF-OA. Figure 1 shows our search strategies (PubMed /Medline and Cochrane Library). The searches were made since the existence of the search engines (PubMed and Cochrane Library) until 7 December 2018.
Figure 1.
Flow chart of our search strategy regarding the role of patellofemoral arthroplasty (PFA) in patellofemoral (PF) osteoarthritis (OA)
Results
Table 1 shows the results of the main reported studies on the role of PFA in PF-OA (3, 8-29).
Table 1.
Main papers on the role of patellofemoral arthroplasty (PFA) in isolated patellofemoral (PF) osteoarthritis (OA).
| AUTHOR [REFERENCE] | YEAR | COMMENTS |
|---|---|---|
| Sreekumar et al (8) | 2009 | Midterm results showed a success rate of around 80% to 90% with modern PFAs. The reported failure causes associated with PFA include progressive tibiofemoral OA, patellar pain, catching or subluxation caused by soft-tissue imbalance, component malposition, and problematic designs. |
| Gupta et al (9) | 2010 | Historically, the outcomes with PFA have been inconsistent; recent developments in prosthesis design and surgical indications have ameliorated the results of PFA. |
| Lonner (3) | 2010 | PFA is an effective treatment for isolated OA of the anterior compartment of the knee. The best results were obtained when there is no patellar malalignment, the prosthesis is appropriately aligned, the soft tissues are balanced, and the implant has sound design features. The prevalence of PF dysfunction and failure caused by patellar maltracking and catching has been considerably reduced by the use of contemporary implant designs rather than earlier implant designs. |
| Lonner (10) | 2010 | PFA has a legitimate role in the treatment of isolated anterior compartment OA. With onlay trochlear designs, early patella instability problems have been reduced, leaving late tibiofemoral degeneration as the primary cause of failure of PFAs. Several long-term studies have shown a rate of tibiofemoral degeneration of approximately 20% at 15 years. |
| Courtney et al (11) | 2012 | PFA is a viable treatment option of the patient with isolated PF-OA. Some of the purported advantages of PFA compared with TKA include less invasive approach, less bone resection and tissue destruction, decreased operative time, shorter rehabilitation, better knee kinematics, and decreased blood loss. |
| Akhbari et al (12) | 2015 | PFA has a number of advantages over TKA, including being less invasive, preserving the unaffected parts of the knee, allowing faster recovery and better range of motion and function. |
| Goh et al (13) | 2015 | PFA is an option for younger patients with isolated PF-OA. Older PFAs had high failure rates due to poor design |
| van der List et al (14) | 2017 | A systematic review showed that fairly good results of PFA survivorship and functional outcomes were reported at short- and midterm follow-up in the setting of isolated PF-OA. Heterogeneity existed mainly in prosthesis design and year the cohort started |
| Christ et al (15) | 2017 | Success of PFA depends upon correct patient selection rather than implant failure or wear. Conversion of PFA to TKA is technically similar to primary TKA, with similar post-operative pain relief and range of motion. However, infection rates and complications requiring further surgery are more consistent with results seen in revision TKA |
| Pisanu et al (16) | 2017 | The outcomes for PFA are quite variable with a trend toward good to excellent results, mainly owing to the improvement in surgical techniques, patient selection, and implant design. The development of the second generation of PFA improved the outcomes, which is attributed to the different trochlear designs. |
| Saffarini et al (17) | 2018 | This study evaluated the accuracy of preoperative planning for patellofemoral arthroplasty (PFA) by comparing: (1) virtual implant positioning simulated on pre-operative images versus (2) real implant positioning from post-operative images. Pre-operative planning was insufficiently accurate to follow intra-operatively, the greatest errors being angular alignment (varus-valgus and flexum-recurvatum). The clinical relevance of these findings is that PFA is difficult to plan pre/operatively due to non-visibility of cartilage on CT scans and to trochlear dysplasia in most cases. |
| Reihs et al [18] | 2018 | This meta-analysis did not reveal significant differences in the comparison between developer over independent publications and between ‘first-generation-resurfacing’ over ‘trochlear-cutting’ implants. ‘Trochlear-cutting’ devices of PFA had slightly superior outcomes, but that benefit was not statistically significant. Nevertheless, these authors recommended ‘trochlear-cutting’ devices for further use in PFA. |
| Middleton et al [19] | These authors performed 103 PFA in 85 patients, mean age 64, mean follow up time 5.6 years, with 93 implants still in situ. The Avon PFA delivered reproducible and effective pain relief and function to patients with isolated PF OA. These authors believed that PFA had an important role to play, and they will continue to perform this procedure for a carefully selected group of patients. Conversion to TKA does not and should not be regarded as failure of the index operation. | |
| Odgaard et al (20) | 2018 | Patients undergoing PFA obtained a better overall knee-specific quality of life than patients undergoing TKA throughout the first 2 years after operation for isolated PF OA. At 2 years, only KOOS function differs between patients undergoing PFA and those undergoing TKA, whereas other PRO dimensions do not show a difference between groups. The observations can be explained by patients undergoing PFA recovering faster than patients undergoing TKA and the functional outcome being better for patients undergoing PFA up to 9 months. Patients undergoing PFA regain their preoperative ROM, whereas patients undergoing TKA at 2 years have lost 10° of ROM. These authors found no differences in complications. |
| Van Joubergen et al (21) | 2018 | The findings of this study showed that when using the medial malleolus as a landmark to guide rotation, the femoral component of the PFA was oriented in external rotation relative to the anatomical transepicondylar axis in 80% of knees. This study did not show a relation between the amount of external rotation and clinical outcomes. |
| Perrone et al (22) | 2018 | The aim of this study was to compare Oxford Knee Score (OKS), KOOS-PS and Kujala Score results in patients who received either PFA or TKA with and without patella resurfacing in the treatment of knee OA. No statistical significance was found for OKS, KOOS-PS and Kujala scores between the three groups. However, patients with PFA experienced higher levels of pain. |
| Cuthbert et al (23) | 2018 | This comprehensive review of PFA in the literature to date concluded that, in carefully selected patients, PFA is worthy of consideration as a functionally superior and economically beneficial joint-preserving procedure - delaying TKA until implant failure or tibiofemoral OA progression. |
| Strickland et al (24) | 2018 | These authors reported that advances in patient selection, implant design, and surgical technique have resulted in improved performance and longevity of these implants. Although short- and mid-term data for modern PFA appear promising, further long-term clinical studies are needed to evaluate how new designs and technologies will affect patient outcomes and long-term implant performance. |
| Metcalfe et al (25) | 2018 | A total of 558 Avon PFA in 431 patients, with minimum two-year follow-up, were identified from a prospective database. Patient-reported outcomes and implant survivorship were analyzed, with follow-up of up to 18 years. Satisfactory long-term results were obtained with the Avon PFA, with maintenance of patient-reported outcome measures (PROMs), satisfactory survival, and low rates of loosening and wear. |
| Ajnin et al (26) | 2018 | A total of 43 FPV (Femoro Patella Vialli) PFA were implanted in 32 patients. Mean follow-up was 65 months. Midterm results with FPV prosthesis demonstrated that moderate outcomes can be achieved. PFA may be used to delay TKA but judicious patient selection to identify truly isolated PF OA is necessary. Chondral lesion in weight bearing area can lead to early implant failure. The main cause of failure was progressive tibiofemoral OA. |
| Bunyoz et al (27) | 2018 | A systematic search showed excellent postoperative weighted mean AKSS knee scores in both the second-generation PFA group and in the TKA group, suggesting that both surgical options can result in a satisfying patient-reported outcome. Higher revision rates in the second-generation PFA studies may in part be due to challenges related to patient selection. Based on evaluation of PROMs, the use of second-generation PFA seemed to be an equal option to TKA for treatment of isolated PF OA in appropriately selected patients. Hopefully, this can be considered by physicians in their daily clinical work. |
| Godshaw et al (28) | 2018 | A 37-year-old female with a contralateral right below-knee amputation and progressive left PF OA had failed multiple conservative treatment modalities. She underwent isolated PFA using an inlay-designed implant. Inlay PFA was a valid treatment option for isolated PF OA. Successful results can be achieved with this procedure after failure of conservative measures in patients with limited or no evidence of tibiofemoral OA. |
| Imhoff et al (29) | 2018 | These authors evaluated the clinical and radiographic outcomes and survivorship at 2 and 5 years after isolated contemporary inlay PFA. Thirty-four patients were prospectively enrolled in the study and were evaluated preoperatively and at 2 and 5 years postoperatively. Five of the 34 patients were lost to follow-up resulting in a final follow-up rate of 86%. A total of six patients (17.1%) failed leaving a survival rate of 91% after 2 years and 83% after 5 years. The main cause for postoperative failure was persistent knee pain; however, no significant preoperative risk factor in patient characteristics could be identified. |
TKA = Total knee arthroplasty; ; KOOS = Knee Injury and Osteoarthritis Outcome Score; KOSS-PS = KOOS Physical Function Short Form; AKSS = American Knee Society Score
Discussion
Cataloging and treatment of patients with isolated PF-OA are difficult. Many of these patients are seen at a young age and it is paramount to differentiate degenerative change in the PF joint from the other diverse causes of anterior knee pain. When the diagnosis of isolated PF-OA has been made, nonoperative and conservative surgical procedures should be advised prior to prosthetic arthroplasty (30).
Severe OA of the knee is an incapacitating disease, with over 50,000 knee replacements carried out each year in the UK. Isolated PF-OA happens in over 10% of these patients with the management alternatives being PFA or total knee arthroplasty (TKA). While many surgeons opine that TKA is the ‘gold standard’ management for severe knee OA, PFA has unquestionable inherent advantages. Fundamentally, because this surgical procedure permits the patient to retain the majority of their own knee articulation; conserving bone-stock and the patients’ own ligaments. PFA has also been acknowledged as a less ‘invasive’ surgical procedure than primary TKA, expediting a more fast recuperation. With the development of ameliorated designs and surgical procedures, interest in the use of PFA has augmented. The primary goal of the newer generation of PFA designs has been to more precisely replicate normal knee kinematics (31).
PFA has been an alternative for patients with painful PF-OA since the 1950’s. Many of the initial failures were due to a combination of implant design and surgeon’s technique (32). PFA can be an efficacious intermediary management for patients with isolated PF-OA. In the absence of patellar malalignment, outcomes are improved when a design with sound geometric features is utilized, the prosthesis is adequately aligned, and the soft tissues are balanced. Although preceding prosthesis designs resulted in a relatively high percentage of failure due to PF maltracking, PF catching, and anterior knee pain, newer prosthesis designs exhibit promise in decreasing the rate of PF dysfunction. Advancing tibiofemoral cartilage degradation is another so-called failure mechanism; such advancing degeneration emphasizes the significance of limiting the surgical technique to patients who do not have tibiofemoral chondromalacia. Considering that long-run failure as a result of tibiofemoral degradation may happen in around 25% of patients, PFA may be considered an intermediary procedure for selected patients with PF-OA (33).
The outcomes of PFA have been improved over the past three decades along with improvement in the surgical techniques. Moreover, patellofemoral-related problems have been decreased such as patellar maltracking, and catching following PFA. While these problems were attributed to mistakes in surgical techniques or component malposition, the design of the trochlear component might have been another reason.. Contemporary PFAs have a decreased rate of such problems related to patellar maltracking that typically plagued earlier generation designs (34).
Successful PFA depends on proper patient selection, accurate prosthesis design, and precise surgical procedure (35). The trochlear components have changed from inlay-style to onlay-style designs, which have decreased the rate of patellar instability [Figures 2; 3 Table 2]. Reducing the risk of patellar instability with onlay-design PFAs has improved mid-term and long-term outcomes and leaves progressive tibiofemoral osteoarthritis as the principal failure mechanism beyond 10 to 15 years (36, 37).
Figure 2.

Inlay design patellofemoral arthroplasty (PFA).
Figure 3.
Onlay design patellofemoral arthroplasty (PFA).
Table 2.
Generalized design characteristics of inlay and onlay designed patellofemoral arthroplasties (AP=Anteroposterior)
| CHARACTERISTICS | ONLAY | INLAY |
|---|---|---|
| Positioning | Inset flush with native throchlea | Replaces entire throchlea, perpendicular to AP axis |
| Rotation | Determined by native trochlea | Set by surgeon, perpendicular to AP axis |
| Width | Narrower | Wider |
| Proximal extension | No further than native trochlear surface | Extends further proximal than native trochlea |
PFA keeps on controversial, mainly due to the high failure percentages published with early implants. A number of case series have been reported over the years, which depict the outcomes with various first- and second-generation prostheses. First-generation resurfacing designs had relatively elevated failure percentages in the medium run. Second-generation prostheses, with femoral cuts based on TKA designs, have yielded more encouraging medium-term outcomes.
The earliest PFA design was a solitary resurfacing of the patella with a screw-on Vitallium patellar shell. Despite initial promising results, it was speedily left behind due to extreme wear in the trochlear groove. The first generation of comprehensive PFA (both sides) solely replaced the trochlear cartilage maintaining the subchondral bone untouched (inlay design); consequently, the location of the PFA was connected to the anatomy of the natural trochlea. Additionaly, the trochlear component was placed flush with the encircling cartilage, the rotational lining up was parallel to the trochlear tilt, the mediolateral coverage was restricted, and the surgical technique was principally free hand. The results of first-generation PFA were favorable in the short-run, yielding early pain mitigation, but the results were not sustained over time and more than 50% of the prostheses failed in the mid- to long-run follow-up with an elevated reoperation rate (16).
The second-generation PFA was arranged to yield better clinical results and solve the problems of the previous design, principally related to maltracking and instability. These prostheses utilized identical anterior femoral cuts as in TKA and entirely replaced the anterior part of the knee (onlay design). Moreover, these were defined by a wide trochlear flange that became narrower in its distal part, a valgus tracking angle and a good coincidence all over the whole range of motion, eluding catching, snapping, or popping (16).
Nowadays, inlay implants have been mostly abandoned and onlay implants are mainly used worldwide (16).
Short-run adverse events are commonly related to patellar maltracking, while long-run adverse events are habitually related to advancement of OA in the tibiofemoral articulation. Implant loosening and polyethylene wear are rare. In general,innovative betterments in prosthesis design and surgical techniques have produced better short- and medium-run results. Despite this, more research is compulsory to determine the long-run outcomes ofcontemporary implant designs (38).
In conclusion, solitary PF-OA is an uncommon illness, whose treatment is defiant and debatable. PFA can be an efficacious management for this illness. The basic concepts of a PFA have changed through the years, resulting in more anatomic prostheses and reproducible surgical procedures. The results of PFA are rigidly related to surgical indications, implant model and adequate surgical procedure.
Acknowledgements
There are no acknowledgements.
References
- 1.Walker T, Perkinson B, Mihalko WM. Patellofemoral arthroplasty: the other unicompartmental knee replacement. J Bone Joint Surg Am. 2012;94(18):1712–20. doi: 10.2106/JBJS.L.00539. [DOI] [PubMed] [Google Scholar]
- 2.Monk AP, van Duren BH, Pandit H, Shakespeare D, Murray DW, Gill HS. In vivo sagittal plane kinematics of the FPV patellofemoral replacement. Knee Surg Sports Traumatol Arthrosc. 2012;20(6):1104–9. doi: 10.1007/s00167-011-1717-4. [DOI] [PubMed] [Google Scholar]
- 3.Lonner JH. Patellofemoral arthroplasty. Orthopedics. 2010;33(9) doi: 10.3928/01477447-20100722-39. [DOI] [PubMed] [Google Scholar]
- 4.Cannon A, Stolley M, Wolf B, Amendola A. Patellofemoral resurfacing arthroplasty: literature review and description of a novel technique. Iowa Orthop J. 2008;28(1):42–8. [PMC free article] [PubMed] [Google Scholar]
- 5.Lustig S, Magnussen RA, Dahm DL, Parker D. Patellofemoral arthroplasty, where are we today? Knee Surg Sports Traumatol Arthrosc. 2012;20(7):1216–26. doi: 10.1007/s00167-012-1948-z. [DOI] [PubMed] [Google Scholar]
- 6.Lonner JH. Patellofemoral arthroplasty: pros, cons, and design considerations. Clin Orthop Relat Res. 2004;428(1):158–65. [PubMed] [Google Scholar]
- 7.Lotke PA, Lonner JH, Nelson CL. Patellofemoral arthroplasty: the third compartment. J Arthroplasty. 2005;20(4 Suppl 2):4–6. doi: 10.1016/j.arth.2005.03.011. [DOI] [PubMed] [Google Scholar]
- 8.Sreekumar R, Subramanian S, Mohammed A. Patellar button dissociation in a mobile-bearing LCS patellofemoral joint arthroplasty. J Knee Surg. 2009;22(3):275–8. doi: 10.1055/s-0030-1247763. [DOI] [PubMed] [Google Scholar]
- 9.Gupta RR, Zywiel MG, Leadbetter WB, Bonutti P, Mont MA. Scientific evidence for the use of modern patellofemoral arthroplasty. Expert Rev Med Devices. 2010;7(1):51–66. doi: 10.1586/erd.09.53. [DOI] [PubMed] [Google Scholar]
- 10.Lonner JH. Patellofemoral arthroplasty. Instr Course Lect. 2010;59(1):67–84. [PubMed] [Google Scholar]
- 11.Courtney J, Liebelt D, Nett MP, Cushner FD. Blood loss and transfusion rates following patellofemoral arthroplasty. Orthop Clin North Am. 2012;43(5):e44–7. doi: 10.1016/j.ocl.2012.07.007. [DOI] [PubMed] [Google Scholar]
- 12.Akhbari P, Malak T, Dawson-Bowling S, East D, Miles K, Butler-Manuel PA. The Avon patellofemoral joint replacement: mid-term prospective results from an independent centre. Clin Orthop Surg. 2015;7(2):171–6. doi: 10.4055/cios.2015.7.2.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goh GS, Liow MH, Tay DK, Lo NN, Yeo SJ. Four-year follow up outcome study of patellofemoral arthroplasty at a single institution. J Arthroplasty. 2015;30(6):959–63. doi: 10.1016/j.arth.2015.01.020. [DOI] [PubMed] [Google Scholar]
- 14.van der List JP, Chawla H, Villa JC, Pearle AD. Why do patellofemoral arthroplasties fail today? A systematic review. Knee. 2017;24(1):2–8. doi: 10.1016/j.knee.2015.11.002. [DOI] [PubMed] [Google Scholar]
- 15.Christ AB, Baral E, Koch C, Shubin Stein BE, Gonzalez Della Valle A, et al. Patellofemoral arthroplasty conversion to total knee arthroplasty: retrieval analysis and clinical correlation. Knee. 2017;24(5):1233–9. doi: 10.1016/j.knee.2017.06.015. [DOI] [PubMed] [Google Scholar]
- 16.Pisanu G, Rosso F, Bertolo C, Dettoni F, Blonna D, Bonasia DE, et al. Patellofemoral arthroplasty: current concepts and review of the literature. Joints. 2017;5(4):237–45. doi: 10.1055/s-0037-1606618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Saffarini M, Müller JH, La Barbera G, Hannink G, Cho KJ, Toanen C, et al. Inadequacy of computed tomography for pre-operative planning of patellofemoral arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2018;26(5):1485–92. doi: 10.1007/s00167-017-4474-1. [DOI] [PubMed] [Google Scholar]
- 18.Reihs B, Reihs F, Labek G, Hochegger M, Leithner A, Böhler N, et al. No bias for developer publications and no difference between first-generation trochlear-resurfacing versus trochlear-cutting implants in 15,306 cases of patellofemoral joint arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2018;26(9):2809–16. doi: 10.1007/s00167-017-4692-6. [DOI] [PubMed] [Google Scholar]
- 19.Middleton SW, Toms AD, Schranz PJ, Mandalia VI. Mid-term survivorship and clinical outcomes of the Avon patellofemoral joint replacement. Knee. 2018;25(2):323–8. doi: 10.1016/j.knee.2018.01.007. [DOI] [PubMed] [Google Scholar]
- 20.Odgaard A, Madsen F, Kristensen PW, Kappel A, Fabrin J. The mark Coventry award: patellofemoral arthroplasty results in better range of movement and early patient-reported outcomes than TKA. Clin Orthop Relat Res. 2018;476(1):87–100. doi: 10.1007/s11999.0000000000000017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.van Jonbergen HW, Westerbeek RE. Femoral component rotation in patellofemoral joint replacement. Knee. 2018;25(3):485–90. doi: 10.1016/j.knee.2018.02.007. [DOI] [PubMed] [Google Scholar]
- 22.Perrone FL, Baron S, Suero EM, Lausmann C, Kendoff D, Zahar A, et al. Patient-reported outcome measures (PROMs) in patients undergoing patellofemoral arthroplasty and total knee replacement: a comparative study. Technol Health Care. 2018;26(3):507–14. doi: 10.3233/THC-181185. [DOI] [PubMed] [Google Scholar]
- 23.Cuthbert R, Tibrewal S, Tibrewal SB. Patellofemoral arthroplasty: current concepts. J Clin Orthop Trauma. 2018;9(1):24–8. doi: 10.1016/j.jcot.2017.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Strickland SM, Bird ML, Christ AB. Advances in patellofemoral arthroplasty. Curr Rev Musculoskelet Med. 2018;11(2):221–30. doi: 10.1007/s12178-018-9477-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Metcalfe AJ, Ahearn N, Hassaballa MA, Parsons N, Ackroyd CE, Murray JR, et al. The Avon patellofemoral joint arthroplasty. Bone Joint J. 2018;100-B(9):1162–7. doi: 10.1302/0301-620X.100B9.BJJ-2018-0174.R1. [DOI] [PubMed] [Google Scholar]
- 26.Ajnin S, Buchanan D, Arbuthnot J, Fernandes R. Patellofemoral joint replacement - Mean five year follow-up. Knee. 2018;25(6):1272–7. doi: 10.1016/j.knee.2018.08.014. [DOI] [PubMed] [Google Scholar]
- 27.Bunyoz KI, Lustig S, Troelsen A. Similar postoperative patient-reported outcome in both second generation patellofemoral arthroplasty and total knee arthroplasty for treatment of isolated patellofemoral osteoarthritis: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2018;27(7):2226–37. doi: 10.1007/s00167-018-5151-8. [DOI] [PubMed] [Google Scholar]
- 28.Godshaw B, Kolodychuk N, Williams GK Jr, Browning B, Jones D. Patellofemoral arthroplasty. Ochsner J. 2018;18(3):280–7. doi: 10.31486/toj.18.0009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Imhoff AB, Feucht MJ, Bartsch E, Cotic M, Pogorzelski J. High patient satisfaction with significant improvement in knee function and pain relief after mid-term follow-up in patients with isolated patellofemoral inlay arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2018;27(7):2251–8. doi: 10.1007/s00167-018-5173-2. [DOI] [PubMed] [Google Scholar]
- 30.Tarassoli P, Punwar S, Khan W, Johnstone D. Patellofemoral arthroplasty: a systematic review of the literature. Open Orthop J. 2012;6(1):340–7. doi: 10.2174/1874325001206010340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Odumenya M, McGuinness K, Achten J, Parsons N, Spalding T, Costa M. The Warwick patellofemoral arthroplasty trial: a randomised clinical trial of total knee arthroplasty versus patellofemoral arthroplasty in patients with severe arthritis of the patellofemoral joint. BMC Musculoskelet Disord. 2011;12(1):265. doi: 10.1186/1471-2474-12-265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Farr J 2nd, Barrett D. Optimizing patellofemoral arthroplasty. Knee. 2008;15(5):339–47. doi: 10.1016/j.knee.2008.05.008. [DOI] [PubMed] [Google Scholar]
- 33.Lonner JH. Patellofemoral arthroplasty. J Am Acad Orthop Surg. 2007;15(8):495–506. doi: 10.5435/00124635-200708000-00006. [DOI] [PubMed] [Google Scholar]
- 34.Lonner JH. Patellofemoral arthroplasty: the impact of design on outcomes. Orthop Clin North Am. 2008;39(3):347–54. doi: 10.1016/j.ocl.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 35.Sisto DJ, Sarin VK. Patellofemoral arthroplasty with a customized trochlear prosthesis. Orthop Clin North Am. 2008;39(3):355–62. doi: 10.1016/j.ocl.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 36.Walker T, Perkinson B, Mihalko WM. Patellofemoral arthroplasty: the other unicompartmental knee replacement. Instr Course Lect. 2013;62(1):363–71. [PubMed] [Google Scholar]
- 37.Lonner JH, Bloomfield MR. The clinical outcome of patellofemoral arthroplasty. Orthop Clin North Am. 2013;44(3):271–80. doi: 10.1016/j.ocl.2013.03.002. [DOI] [PubMed] [Google Scholar]
- 38.Lustig S. Patellofemoral arthroplasty. Orthop Traumatol Surg Res. 2014;100(1 Suppl):S35–43. doi: 10.1016/j.otsr.2013.06.013. [DOI] [PubMed] [Google Scholar]