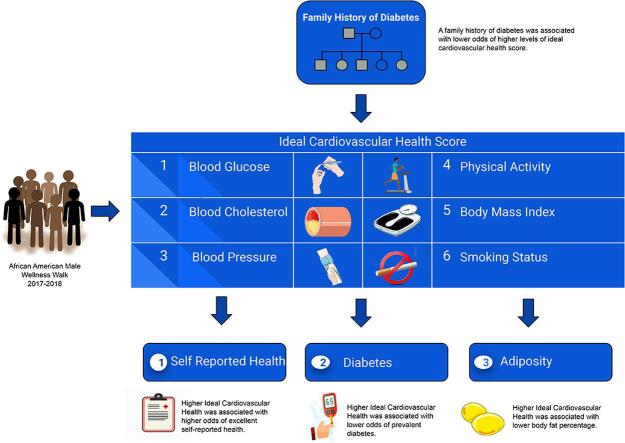
Graphical abstract
Abbreviations: AA, African American; AAMWI, African American Male Wellness Initiative; AAMWW, African American Male Wellness Walk; AHA, American Heart Association; BF%, Body Fat Percentage; BMI, Body Mass Index; CVD, Cardiovascular Disease; ICH, Ideal Cardiovascular Health; US, United States of America
Keywords: African Americans, Self-Reported Health, Cardiovascular Health, Diabetes, Body Fat Percentage, Health Disparities
Abstract
African American (AA) men have the highest age-adjusted all-cause mortality rate in the United States of America (US) and a high burden of cardiovascular risk factors. The African American Male Wellness Walk (AAMWW) seeks to reduce such health disparities among AA males. The association of a combination of ideal cardiovascular health (ICH) metrics (blood pressure, glucose, cholesterol, body mass index (BMI), physical activity, and smoking) with self-reported health, diabetes, and body fat percentage was examined among 729 AA male participants from the 2017 and 2018 AAMWWs. Six metrics of ICH were categorized into a three-tiered ICH score 0–2, 3–4, 5–6. Linear and logistic regression modeling was performed with adjustment for age and insurance. Seven percent of men attained 5–6 ICH metrics at baseline. Participants with 5–6 ICH metrics versus 0–2 had 256% higher odds of excellent self-reported health compared to good, fair or poor (p < 0.0001). After exclusion of glucose from the ideal cardiovascular health score, participants with 3–4 versus 0–2 ICH metrics had a 48% lower odds of diabetes (p < 0.0031). After exclusion of BMI from the ICH score, participants with 5 ICH metrics had a 14.1% lower body fat percentage versus participants with 0–2 ICH metrics (p = 0.0057). Attainment of higher ideal cardiovascular health scores is associated with higher odds of self-reported health, lower odds of diabetes and lower body fat percentage among AA men. Future strategies leading to greater attainment of cardiovascular health in AA males will be important to advance health equity.
1. Introduction
As the United States of America (US) population expands, it is projected that more than half of all Americans will belong to a minority group by 2044 (Colby and Ortman, 2015). Thus, to improve the overall health status of the US, it is critical to improve health in minority groups and advance health equity. African American (AA) men had the lowest life-expectancy among any sex or racial/ethnic group in 2017, with a disparity of 4.6 and 7.6 years compared to non-Hispanic white and Hispanic men and an astounding 9.5 and 12.8 years compared to non-Hispanic white and Hispanic women (Kochanek et al., 2019). AA men are disproportionately burdened by hypertension, diabetes, cancer and other chronic diseases (Carnethon et al., 2017, Cronin et al., 2018). AA men have the highest age-adjusted all-cause mortality and the lowest health status of any race-gender category in the US (Kochanek et al., 2019, Shikany et al., 2018). AA men share a disproportionate burden of modifiable risk factors that contribute to chronic diseases including physical inactivity, poor dietary intake, and obesity (Shikany et al., 2018). Therefore, health promotion strategies and healthy behavior change are critical to preventing chronic disease and premature mortality among AA men.
In 2010, the American Heart Association (AHA) defined metrics for cardiovascular health promotion and disease reduction including 7 metrics of cardiovascular health (blood pressure, cholesterol, glucose, body mass index (BMI), smoking, healthy diet and physical activity) (Lloyd-Jones et al., 2010). Attaining higher levels of cardiovascular health is associated with lower risk of diabetes, cancer, cardiovascular disease (CVD), and mortality (Dong et al., 2012, Joseph et al., 2016, Rasmussen-Torvik et al., 2013). There is a lack of evidence in community settings on: 1) the prevalence of ideal cardiovascular health among AA men; 2) the role of ideal cardiovascular health with self-reported health, diabetes and adiposity among AA men; and 3) the role of a family history of diabetes in attainment of ideal cardiovascular health. Thus, we examined the prevalence of six of the ideal cardiovascular health metrics (blood pressure, cholesterol, glucose, BMI, smoking, and physical activity) and the association of ideal cardiovascular health score with self-reported health, body fat percentage (BF%), and diabetes in AA men participating in health screenings at the AA Male Wellness Walks (AAMWW). Second, we examined the association of family history of diabetes with attainment of ideal cardiovascular health among AA men. We hypothesized that: 1) higher attainment of ideal cardiovascular health would be associated with higher odds of self-reported health, lower odds of diabetes and lower BF%; and 2) family history of diabetes would be associated with lower attainment of ideal cardiovascular health.
2. Methods
2.1. Study design and study population
The National African American Male Wellness Initiative (AAMWI) established in Columbus, Ohio in 2004 aims to reduce disparities in premature death and chronic diseases among AA males through AAMWWs and annual health events. Since 2004, the AAMWI has expanded to other cities in Ohio and across the nation (e.g., New Orleans, LA; Washington D.C.; Atlanta, GA; Silver Spring, MD; Renton, WA; and Niagara Falls, NY). The AAMWWs (5k walks) host free health screenings for AA men, along with community partners. The events are promoted in the community through various methods (i.e. mass and social media). Since its inception, the AAMWW mantra has been: “Know Your Numbers.” The AAMWI encouraged AA men to be more active in self-management of their health through evaluations of blood pressure, glucose, cholesterol, BMI, smoking and physical activity. It has grown to average over 50,000 participants annually. In 2016, the AAMWI and researchers at The Ohio State University formed a collaborative academic, healthcare and community partnership, aiming to transform the AAMWWs from health promotion awareness to evaluating and reducing disease among AA men.
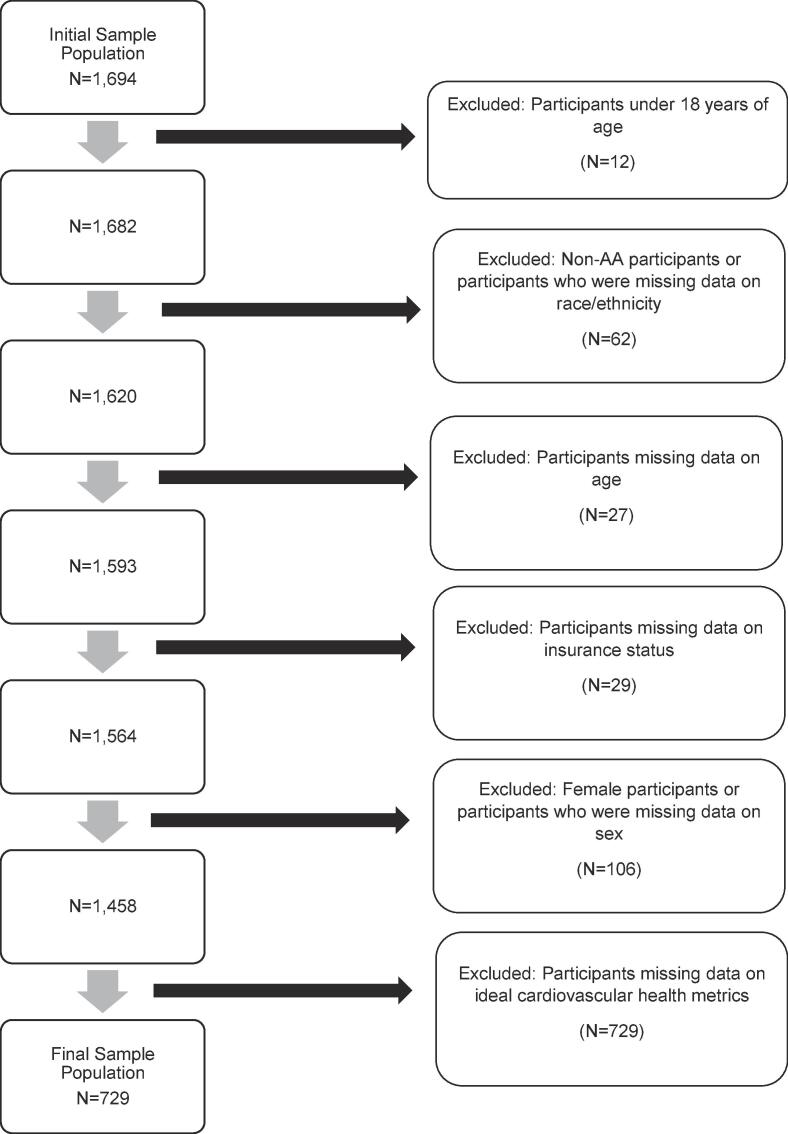
In the 2017 and 2018 AAMWWs, 1,694 individuals participated in the screenings. The participants were from six communities in Ohio: Akron, Cincinnati, Cleveland, Columbus, Toledo, and Youngstown and three cities nationally including New Orleans, LA; Washington, DC; and Niagara Falls, NY. Participants excluded were under 18 years of age (n = 12), female or did not answer the question related to sex (n = 106), non-AA or missing data on race/ethnicity (n = 62), missing data on age (n = 27), insurance status (n = 29) or any ideal cardiovascular health metric (n = 729), as shown in Fig. 1. After exclusions, 729 participants were included in the analytic cohort. The excluded participants had similar age, smoking status, physical activity, body fat percentage, family history of diabetes, self-reported health and hypercholesteremia status. The excluded group had higher percentages of Medicaid/Medicare insurance, with better levels of blood pressure, BMI, and hypertension, but worse levels of glucose, diabetes and cholesterol (Supplemental Table 1). This project used existing data collected for non-research purposes from participants in the AAMWW, with no identifiers linking human participants to the data. The project was approved by The Ohio State University Biomedical Sciences Institutional Review Board.
Fig. 1.
2017 and 2018 African American Male Wellness Walks Sample Exclusion Flowchart 2017 and 2018 Study Population. Data included 1,694 individuals who participated in African American Male Wellness Walks. Exclusions: Following data collection, we excluded: Participants who were under 18 years of age (n = 12) participants who were women or missing data on sex (n = 106), participants of other racial/ethnic groups (n = 62), participants with missing data on age (n = 27), participants with missing data on insurance (n = 29), and participants with missing data on ideal metrics (n = 729). After exclusions, we included 729 participants in the final analysis.
During the AAMWWs, standardized questionnaires were used to collect information on demographics (age, sex [male/female], race/ethnicity [Black/AA, Asian, Caucasian/White, Native American, Hispanic, Other]), smoking status (Do you smoke? Yes/No), self-reported health (Rate your health: Poor, Fair, Good, Excellent), insurance status (Private Insurance, Medicaid, Medicare, No Insurance), chronic diseases (high blood pressure/hypertension, high cholesterol/hypercholesterolemia and diabetes, medications use for the chronic diseases (Yes/No), family history of diabetes (Yes/No), and level of physical activity (I exercise 3 or more times per week, Yes/No). Blood glucose and cholesterol were measured using the Cardio Check Silver® (Polymer Technology, Inc., Heath, OH, US). Blood pressure was measured using Lifesource Automatic Blood Pressure Monitors (Lifesource Medical, Inc., Greensboro, NC, US). Weight was measured using various zeroed scales and height was self-reported. BMI was calculated by multiplying weight (lbs) by 703, and then dividing by height squared (inch2). During the health screenings, cardiovascular health was measured using six of the AHA’s ideal cardiovascular health metrics, which includes targets for blood pressure, cholesterol, glucose, BMI, smoking, and physical activity.
2.2. Main exposures
2.2.1. Blood pressure
Ideal blood pressure was classified as <120/80 mmHg. Intermediate blood pressure was defined as systolic blood pressure of 120–139 mmHg or a diastolic level of 80–89 mmHg or being treated to ideal blood pressure goal. Poor blood pressure was classified as ≥140/90 mmHg (Lloyd-Jones et al., 2010).
2.2.2. Total cholesterol
Ideal cholesterol was classified as total cholesterol < 200 mg/dL. Intermediate cholesterol was defined as total cholesterol between 200 and 239 mg/dL or being treated to ideal cholesterol goal. Poor cholesterol was ≥ 240 mg/dL (Lloyd-Jones et al., 2010).
2.2.3. Blood glucose
A modified ideal blood glucose was created due to some participants in the non-fasting state. Ideal blood glucose was defined as a fasting glucose < 100 mg/dL or a non-fasting glucose (<140 mg/dL). Intermediate blood glucose was defined as having a fasting glucose of 100–125 mg/dL or non-fasting glucose (140–199 mg/dL) or being treated to goal. Poor blood glucose was defined as having a fasting glucose ≥ 126 mg/dL or non-fasting glucose (≥ 200 mg/dL) (Lloyd-Jones et al., 2010).
2.2.4. Body mass index
Ideal, intermediate, and poor BMI were defined as BMI < 25, 25–29.9, and ≥ 30 kg/m2, respectively (Lloyd-Jones et al., 2010).
2.2.5. Smoking
Ideal smoking was defined as not currently smoking. Poor smoking was defined as current smoking (Lloyd-Jones et al., 2010).
2.2.6. Physical activity
A modified ideal physical activity classification with ideal physical activity defined as exercising 3 times a week. Poor physical activity was defined as exercising <3 times a week.
2.2.7. Ideal cardiovascular health score
A composite ideal cardiovascular health score was defined by the presence of ideal levels of the 6 metrics: untreated blood pressure < 120/80 mmHg, untreated cholesterol < 200 mg/dL, fasting glucose < 100 mg/dL or a random glucose < 140 mg/dL, BMI < 25 kg/m2, non-smoking status, and/or physical activity of 3 times or more per week. The score was categorized as 0–2, 3–4, and 5–6, as has been performed previously (Joseph et al., 2019, Joseph et al., 2016, Spahillari et al., 2017, Veromaa et al., 2017).
2.3. Secondary exposure
2.3.1. Family history of diabetes
Family history of diabetes was the participant's self-report of whether or not there was a history of diabetes in the family through first-degree relatives.
2.4. Outcomes
2.4.1. Self-reported health
Self-reported health was the participant’s characterization of their health in the following categories: poor, fair, good, or excellent.
2.4.2. Diabetes
Diabetes status was ascertained based on self-report, antihyperglycemic medication use, and/or fasting blood glucose ≥ 126 mg/dL or random blood glucose ≥ 200 mg/dL (American Diabetes Association, 2017).
2.4.3. Body fat percentage (adiposity)
Body Fat percentage was measured using bioelectrical impedance on the scales.
2.5. Covariates
The covariates were age and insurance status (Uninsured, Medicaid, Medicare, Other, Private Insurance, and Combination of Insurances).
2.6. Statistical analysis
Descriptive statistics were used to compare the baseline characteristics of included participants and included vs. excluded participants using appropriate parametric tests for continuous variables (ANOVA, t-tests) and the chi-square tests for categorical variables. Hypertension was defined as systolic blood pressure ≥ 140 mmHg, diastolic blood pressure ≥ 90 mmHg, self-report or use of antihypertensive therapy (Lloyd-Jones et al., 2010). Hypercholesterolemia was defined as total cholesterol ≥ 240 mg/dL, self-report or use of lipid lowering therapy (Lloyd-Jones et al., 2010). The participants that did not report a history of diabetes, hypertension and/or hypercholesterolemia, but had screening consistent with one of these conditions were considered to have the disease. Ordinal logistic regression and logistic regression models were used to examine: 1) the cross-sectional associations of the ideal cardiovascular health score (exposure) with self-reported health and diabetes (outcomes); and 2) the cross-sectional association of family history of diabetes (exposure) with ideal cardiovascular health score (outcome). Each of these analyses were performed separately. The ideal cardiovascular health metric glucose was excluded from the diabetes analysis, due to glucose being in the definition for diabetes, thus, the score ranged from 0 to 5. Odds ratios were estimated for exposures and the associated outcomes: 1) per 1-unit increase in ideal cardiovascular health score; and 2) comparing 3–4 and 5–6 (5 when score ranged from 0 to 5) ideal cardiovascular health metrics to the 0–2 referent group. Linear regression models were used to examine the linear relationship between ideal cardiovascular health score (BMI excluded) and BF%. BMI was excluded due to the high correlation with BF%. Models were adjusted for age and insurance status. All analyses were performed using SAS version 9.4 software. Statistical significance was defined as a two-sided p-value < 0.05.
3. Results
3.1. Characteristics of the analytic cohort
The characteristics of the cohort overall and stratified by ideal cardiovascular heath score in categories 0–2, 3–4 and 5–6 are presented in Table 1. The mean age of the cohort was 48.0 years, 67% of participants had private insurance, and mean systolic and diastolic blood pressure were 140 and 87 mmHg, respectively. The mean BMI was 30.6 kg/m2 and mean total cholesterol was 158 mg/dl. Mean fasting and random glucose were 102 and 107 mg/dl, respectively. Eighty-four percent of individuals were non-smokers, 65% of participants had ideal physical activity, 7.3% of participants had ideal blood pressure, 71% of participants had ideal glucose, 15% of participants had ideal BMI, and 74% of participants had ideal cholesterol. Forty-seven percent of participants had a family history of diabetes. The prevalence of diabetes, hypertension and hypercholesterolemia was 15.6%, 61.2% and 8.6%, respectively. Self-reported health was 0.6%, 19%, 58% and 22% for the poor, fair, good and excellent categories, respectively. For those with higher levels of ideal cardiovascular health metrics, there was lower age, BMI, blood pressure, glucose, cholesterol, family history of diabetes and higher self-reported health. The characteristics of participants by city are presented in Supplemental Table 2. Most variables were similar across cities with notable variance in age, ideal physical activity and ideal blood glucose.
Table 1.
Characteristics of Participants in the African American Male Wellness Walk by Ideal Cardiovascular Health Score 2017–2018.
| All | 0–2 Ideal CV Health Score | 3–4 Ideal CV Health Score | 5–6 Ideal CV Health Score | ||
|---|---|---|---|---|---|
| Baseline Characteristicsa | n = 729 | n = 187 | n = 488 | n = 54 | p-valuea |
| Age (years) | 48.0 (13.6) | 51.0 (12.7) | 47.3 (13.4) | 43.7 (16.3) | p = 0.0005 |
| Insurance Status (%) | p = 0.0088 | ||||
| Uninsured | 10.7 | 13.9 | 9.0 | 14.8 | |
| Combination | 2.9 | 5.4 | 2.3 | 0.0 | |
| Medicaid | 7.1 | 7.0 | 6.6 | 13.0 | |
| Medicare | 12.2 | 16.6 | 10.3 | 14.8 | |
| Other | 0.3 | 0.0 | 0.4 | 0.0 | |
| Private Insurance | 66.8 | 57.2 | 71.5 | 57.4 | |
| Ideal AHA Smokingb (%) | 84.0 | 66.3 | 89.8 | 92.6 | p < 0.0001 |
| Ideal AHA Physical Activityb (%) | 64.6 | 34.8 | 72.5 | 96.3 | p < 0.0001 |
| Ideal AHA Blood Pressureb (%) | 7.3 | 1.1 | 5.1 | 48.2 | p < 0.0001 |
| Ideal AHA Glucoseb (%) | 70.6 | 30.0 | 83.4 | 96.3 | p < 0.0001 |
| Ideal AHA Body mass indexb (%) | 15.0 | 3.2 | 12.1 | 81.5 | p < 0.0001 |
| Ideal AHA Cholesterolb (%) | 74.2 | 42.8 | 83.6 | 98.2 | p < 0.0001 |
| Body-mass Index (kilograms/meter2) | 30.6 (6.3) | 32.7 (6.8) | 30.6 (5.8) | 23.4 (2.9) | p < 0.0001 |
| Systolic blood pressure (mmHg) | 139.8 (19.3) | 146.3 (19.1) | 139.2 (17.6) | 122.2 (22.0) | p < 0.0001 |
| Diastolic blood pressure (mmHg) | 87.1 (12.4) | 91.9 (12.2) | 86.3 (11.8) | 77.6 (11.5) | p < 0.0001 |
| Cholesterol | 157.6 (38.7) | 162.1 (44.0) | 157.2 (36.7) | 146.2 (33.7) | p = 0.0265 |
| Fasting glucose (mg/dL)c | 101.5 (35.7) | 124.0 (43.2) | 92.3 (26.9) | 81.4 (16.2) | p < 0.0001 |
| Random glucose (mg/dL)d | 107.2 (41.9) | 136.9 (63.6) | 100.9 (29.5) | 84.2 (19.1) | p < 0.0001 |
| Body fat percentagee | 25.4 (6.8) | 28.9 (4.7) | 25.6 (6.6) | 17.4 (5.8) | p = 0.0057 |
| Family History of Diabetes (%)f | p = 0.0002 | ||||
| Yes | 47.2 | 59.0 | 44.5 | 31.5 | |
| Prevalence of Diabetes (%) | 15.6 | 40.6 | 7.8 | 0.0 | p < 0.0001 |
| Self-Reported Health (%)g | p < 0.0001 | ||||
| Poor | 0.6 | 1.1 | 0.4 | 0.0 | |
| Fair | 19.0 | 24.2 | 18.5 | 5.6 | |
| Good | 58.2 | 60.4 | 59.3 | 40.7 | |
| Excellent | 22.3 | 14.3 | 21.8 | 53.7 | |
| Prevalence of hypertension (%) | 61.0 | 73.3 | 60.3 | 25.9 | p < 0.0001 |
| Prevalence of hypercholesterolemia (%) | 8.6 | 18.2 | 5.7 | 1.9 | p < 0.0001 |
Mean (SD) or percentages are listed, p-values calculated using chi-square (categorical variables), and ANOVA (parametric continuous variables).
AHA = American Heart Association, Ideal Cardiovascular (CV) Health recommendations were defined by AHA “2020” guidelines with the following modifications. Physical activity was considered ideal if participant exercised ≥ 3 times per week. Glucose was defined using standard fasting glucose guidelines and random glucose guidelines < 140 ideal, 140–180 intermediate and ≥ 180 “poor”.
Fasting glucose, n = 336, (0–2 Ideal Cardiovascular Health Score, n = 103), (3–4 Ideal Cardiovascular Health Score, n = 212), (5–6 Ideal Cardiovascular Health Score, n = 21);
Random glucose, n = 393, (0–2 Ideal Cardiovascular Health Score, n = 84), (3–4 Ideal Cardiovascular Health Score, n = 276),(5–6 Ideal Cardiovascular Health Score, n = 33);
Body fat percentage, n = 42, (0–2 Ideal Cardiovascular Health Score, n = 10), (3–4 Ideal Cardiovascular Health Score, n = 27), (5–6 Ideal Cardiovascular Health Score, n = 5);
Family History of Diabetes, n = 720 (0–2 Ideal Cardiovascular Health Score, n = 183), (3–4 Ideal Cardiovascular Healt.h Score, n = 483), (5–6 Ideal Cardiovascular Health Score, n = 54);
Self-Reported Health, n = 722 total, (0–2 Ideal Cardiovascular Health Score, n = 182), (3–4 Ideal Cardiovascular Health Score, n = 486),(5–6 Ideal Cardiovascular Health Score, n = 54).
3.2. The association of ideal cardiovascular health score with self-reported health
The association of ideal cardiovascular health score with self-reported health is presented in Table 2. In continuous analyses, a 1-unit increase in ideal cardiovascular health score was associated with a 33% higher odds of excellent compared to good, fair or poor self-reported health in fully adjusted models (p = 0.0008). In categorical analyses, the odds of self-reporting excellent compared to good, fair or poor health was 256% higher for those with an ideal cardiovascular health score of 5–6 compared to 0–2 in fully adjusted analyses (p < 0.0001). The odds of self-reporting excellent or good health versus fair or poor health was 619% higher for those with an ideal cardiovascular health score of 5–6 compared to 0–2 in fully adjusted analyses (p = 0.0017). There were positive associations in all cities except for Toledo, Ohio with limited power to detect significant associations due to sample size in some cities (Supplemental Table 3).
Table 2.
The Association of Ideal Cardiovascular Health Score with Self-Reported Health.
| Self-Reported Health - Ordinal Logistic Regression – Odds Ratio (95%CI), p-valuea | |||
|---|---|---|---|
| Model 0 (n = 722) | Model 1 (n = 722) | Model 2 (n = 722) | |
| Continuous Ideal CV Health Score | 1.36 (1.18, 1.57), p < 0.0001 | 1.32 (1.14, 1.53), p < 0.0001 | 1.33 (1.15, 1.54), p = 0.0008 |
| Categorical Ideal CV Health Score | |||
| 0–2 Ideal CV Health Score | Referent | Referent | Referent |
| 3–4 Ideal CV Health Score | 1.20 (0.86, 1.69), p = 0.2863 | 1.14 (0.81, 1.61), p = 0.4474 | 1.14 (0.81, 1.62), p = 0.4488 |
| 5–6 Ideal CV Health Score | 3.84 (2.15, 6.86), p < 0.0001 | 3.49 (1.94, 6.27), p < 0.0001 | 3.56 (1.98, 6.42), p < 0.0001 |
| Good or Excellent vs. Fair or Poor Self-Reported Health - Logistic Regression – Odds Ratio - (95%CI), p-valuea | |||
| Continuous Ideal CV Health Score | 1.28 (1.07, 1.54), p = 0.0065 | 1.36 (1.13, 1.64), p = 0.0010 | 1.33 (1.11, 1.60), p = 0.0025 |
| Categorical Ideal CV Health Score | |||
| 0–2 Ideal CV Health Score | Referent | Referent | Referent |
| 3–4 Ideal CV Health Score | 1.45 (0.97, 2.17), p = 0.0723 | 1.60 (1.06, 2.41), p = 0.0262 | 1.48 (0.97, 2.24), p = 0.0690 |
| 5–6 Ideal CV Health Score | 5.75 (1.71, 19.31), p = 0.0047 | 7.16 (2.10, 24.39), p = 0.0017 | 7.19 (2.09, 24.69), p = 0.0017 |
Models:
Model 0: unadjusted
Model 1: age
Model 2: age and insurance status
Interpretation: In continuous analyses, a 1-unit increase in Ideal CV Health Score was associated with a 33% higher odds of excellent compared to good, fair or poor self-reported health (Model 2). A 1-unit increase in Ideal CV Health Score was associated with a 33% higher odds of excellent or good compared to fair or poor self-reported health (Model 2).
In the categorical analyses, the odds of self-reporting excellent compared to good, fair or poor health was 256% higher for those with an ideal cardiovascular health score of 5–6 compared to 0–2 (Model 2). The odds of self-reporting excellent or good health versus fair or poor health was 619% higher for those with an ideal cardiovascular health score of 5–6 compared to 0–2 (Model 2).
Analyses completed among 722 participants, as there were 7 participants missing self-reported health status. CV = cardiovascular.
3.3. The association of ideal cardiovascular health score with diabetes and body fat percentage
In continuous and categorical fully adjusted analyses excluding glucose from the ideal cardiovascular health score, a 1-unit increase in ideal cardiovascular health score was associated with a 34% lower odds of diabetes (p = 0.0010) and an ideal cardiovascular health score of 3–4 compared to 0–2 was associated with a 48% lower odds of diabetes (p = 0.0031) [Table 3]. In continuous and categorical fully adjusted analyses excluding BMI from the ideal cardiovascular health score, a 1-unit increase in ideal cardiovascular health score was associated with a 2.95% lower BF% (p = 0.0033) and an ideal cardiovascular health score of 5 compared to 0–2 was associated with a 14.11% lower BF% (p = 0.0057) [Table 4].
Table 3.
The Association of Ideal Cardiovascular Health with Diabetesa.
| Diabetes vs. None - Logistic Regression – Odds Ratio (95% CI), p-value | |||
|---|---|---|---|
| Model 0 | Model 1 | Model 2 | |
| Continuous Ideal CV Health Score (0–5) | 0.63 (0.50, 0.80), p = 0.0001 | 0.65 (0.51, 0.83), p = 0.0005 | 0.66 (0.52, 0.85), p = 0.0010 |
| Diabetes vs. None - Logistic Regression – Odds Ratio (95% CI), p-value | |||
| Model 0 | Model 1 | Model 2 | |
| 0–2 Ideal CV Health Score | Referent | Referent | Referent |
| 3–4 Ideal CV Health Score | 0.50 (0.33, 0.76), p = 0.0011 | 0.51 (0.33, 0.79), p = 0.0024 | 0.52 (0.34, 0.80), p = 0.0031 |
| 5 Ideal CV Health Score | n/a | n/a | n/a |
Models:
Model 0: unadjusted
Model 1: age
Model 2: age and insurance status
Interpretation: In continuous analyses, a 1-unit increase in ideal CV health score was associated with a 34% lower odds of diabetes in Model 2. In categorical analyses, an ideal cardiovascular health score of 3–4 compared to 0–2 was associated with a 48% lower odds of diabetes in Model 2. There were not enough cases of prevalent diabetes in the 5 ideal cardiovascular health score group to calculate an estimate for odds compared to 0–2, thus n/a is placed in the table.
CV = cardiovascular
The exposure (ideal cardiovascular health score) included blood pressure, cholesterol, body mass index, smoking, physical activity and excluded glucose due to glucose being a component of the diagnostic criteria for diabetes.
Table 4.
The Association of Ideal Cardiovascular Health Score with Body Fat Percentage among 42 participants in the AAMWW.
| Body Fat % - Linear Regression – Beta Coef. (95% CI), p-valuea | |||
|---|---|---|---|
| Model 0 | Model 1 | Model 2 | |
| Continuous Ideal CV Health Score (0–5) | −2.85 (−4.89, −0.81), p = 0.0073 | −2.69 (−4.52, −0.87), p = 0.0049 | −2.95 (−4.85, −1.05), p = 0.0033 |
| Body Fat % - Linear Regression – Beta Coef. (95% CI), p-valuea | |||
| 0–2 Ideal CV Health Score | Referent | Referent | Referent |
| 3–4 Ideal CV Health Score | −4.23 (−9.07, 0.60), p = 0.0844 | −2.95 (−7.33, 1.44), p = 0.1813 | −3.80 (−8.30, 0.71), p = 0.0963 |
| 5 Ideal CV Health Score | −10.40 (−20.66, −0.14), p = 0.0471 | −11.54 (−20.72, −2.37), p = 0.0151 | −14.11 (−23.84, −4.37), p = 0.0057 |
Models:
Model 0: unadjusted
Model 1: age
Model 2: age and insurance status
Interpretation: In the continuous analysis, a 1-unit increase in ideal cardiovascular health score was associated with a 2.95% lower body fat percentage in Model 2. In the categorical analysis, an ideal cardiovascular health score of 5 compared to 0–2 was associated with a 14.11% lower body percentage in Model 2.
CV = cardiovascular
The exposure (ideal cardiovascular health score) included blood pressure, glucose, cholesterol, smoking, and physical activity. Body mass index was excluded due to the high correlation between body mass index and body fat percentage.
3.4. The association of family history of diabetes with ideal cardiovascular health score
In Table 5, A family history of diabetes was associated with 49% lower odds of an ideal cardiovascular health score of 5–6 compared to 0–2, or 3–4 in fully adjusted analyses.
Table 5.
The Association of Family History of Diabetes with Ideal Cardiovascular Health Score.
| Ideal Cardiovascular Health Score Categories (0–2, 3–4, 5–6) – Ordinal Logistic Regression – Odds Ratio (95% CI), p-valuea | |||
|---|---|---|---|
| Model 0 (n = 720) | Model 1 (n = 720) | Model 2 (n = 720) | |
| - Family History of Diabetes | Referent | Referent | Referent |
| + Family History of Diabetes | 0.52 (0.38, 0.71), p < 0.0001 | 0.51 (0.37, 0.70), p < 0.0001 | 0.51 (0.37, 0.70), p < 0.0001 |
Models:
Model 0: unadjusted
Model 1: age
Model 2: age and insurance status
Interpretation: A family history of diabetes was associated with 49% lower odds of an ideal cardiovascular health score of 5–6 compared to 0–2, or 3–4 in Model 2.
The analyses were conducted in 720 participants, as 9 participants were missing data on family history of diabetes.
4. Discussion
In this study, we report the association of ideal cardiovascular health score with self-reported health, prevalent diabetes, and BF% in over 700 AA community-dwelling males from 2017 and 2018 AAMWWs. We demonstrated the novel positive association of ideal cardiovascular health score with self-reported health, suggesting that individuals with better underlying cardiovascular health perceive better health. Furthermore, we found negative associations of an ideal cardiovascular health score with diabetes and BF% among AA men with cardiovascular health metrics performed at community health screening events. Family history of diabetes was associated with attainment of lower cardiovascular health. All of these findings were independent of age and insurance status, a measure of socioeconomic status. Although, there is a known association of higher attainment of cardiovascular health with lower risk of incident diabetes (Effoe et al., 2017, Joseph et al., 2019, Joseph et al., 2016), cancer (Rasmussen-Torvik et al., 2013), CVD (Dong et al., 2012), and cardiovascular-related and all-cause mortality (Ford et al., 2012a, Ford et al., 2012b), there have been persistent racial/ethnic disparities in attainment of cardiovascular health. Previous studies demonstrated that AAs have low attainment of ideal cardiovascular health (Joseph et al., 2016, Shay et al., 2012). In our study, only 7% of the AA men had ideal blood pressure, 15% of participants had ideal BMI, and 65% of participants had ideal physical activity. Thus, strategies to promote greater attainment of ideal cardiovascular health components in AA men is warranted, given the potential to decrease the burden of CVD, diabetes, cancer, and premature mortality in this population.
Our study is the first to examine the association of ideal cardiovascular health score with self-reported health among community-dwelling AA men. The group of men with attainment of higher ideal cardiovascular health scores had higher odds of rating their self-reported health in a higher category. Thus, objectively better health was concordant with self-reported health. This finding is important in community-based and community-engaged health interventions because if individuals recognize when they are in poor or good health, they may be better able to manage and engage in their health care. Finding a positive association of measured cardiovascular health with self-reported health is consistent with limited studies in other racial/ethnic groups. Self-reported health was associated with ideal cardiovascular health among working-aged Finnish women and among participants in the Multi-Ethnic Study of Atherosclerosis (Osibogun et al., 2018, Veromaa et al., 2017). Self-reported health was considered a predictor of cardiovascular health and therefore, self-reported health was useful to assess cardiovascular health (Osibogun et al., 2018, Veromaa et al., 2017). In conjunction, other studies showed that poor self-reported health is associated with higher risk of incident diabetes and diabetes complications (Hayes et al., 2008, Noh et al., 2019, Wennberg et al., 2013), cancer (Flensborg-Madsen et al., 2011), CVD (Mavaddat et al., 2014), and cardiovascular and non-cardiovascular mortality (Barger et al., 2016, Benjamins et al., 2004, DeSalvo et al., 2006, Mavaddat et al., 2014). Importantly, these findings are independent of established risk factors for chronic diseases and mortality, which suggests that self-reported health may be an important intervention target to reduce disparities in premature mortality. Thus, our finding that higher levels of ideal cardiovascular health were associated with better self-reported health indicates that AA men understand their cardiovascular health. This knowledge can be utilized to select individuals who would benefit from targeted interventions.
Higher levels of ideal cardiovascular health were associated with lower odds of diabetes, independent of the glucose metric. Additionally, the prevalence of diabetes was 41% in those with 0–2 ideal cardiovascular health metrics compared to 0% in those with 5–6 ideal cardiovascular health metrics. While few studies have evaluated the association of ideal cardiovascular health with prevalent diabetes, this finding is consistent with incident diabetes studies in American Indians, AAs, Bi-Racial and Multi-Ethnic Cohorts (Effoe et al., 2017, Fretts et al., 2014, Joseph et al., 2019, Joseph et al., 2016).
In this analysis, higher ideal cardiovascular health scores excluding BMI were associated with lower body fat percentage. In a study that analyzed adiposity with ideal cardiovascular health in children and adolescents, individuals with lower levels of adiposity had better cardiovascular health metrics (Fyfe-Johnson et al., 2018). To our knowledge, this is the first study to assess cardiovascular health scores with adiposity in AA community-dwelling men. Further, lower BF% is associated with lower all-cause mortality (Padwal et al., 2016). Therefore, the association of higher ideal cardiovascular health score with lower body fat percentage provides another potential target to improve premature mortality in AA men.
Interestingly, we report the novel association of family history of diabetes with lower ideal cardiovascular health score. Family history of diabetes may indicate hereditable genetic and environmental influences related to attainment of cardiovascular health metrics (Joseph and Golden, 2017). Thus, early intervention among those with a family history of diabetes may be necessary to promote attainment of ideal cardiovascular health.
4.1. Strengths and limitations
A strength of our study is the inclusion of a large, socioeconomically diverse cohort of AA men that attended AAMWWs in US cities. Second, the questionnaires were structured and consistent over the two-year time period. Third, trained medical staff performed the clinical assessments. In spite of these strengths, there are several potential limitations. First, commonly available blood pressure cuffs and scales were used to measure blood pressure and weight, which may have been non-calibrated in some instances. However, this limitation may have been a potential strength due to the real-world applicability of the measurements. Second, we did not assess dietary intake as a cardiovascular health metric due to the lack of a brief validated measure to assess all the components of AHA ideal diet. Based on previous studies, only 0–1.8% of AA individuals attain ideal dietary intake (Effoe et al., 2017, Joseph et al., 2016, Shay et al., 2012); thus, the ideal cardiovascular health score may be minimally impacted. Third, our study assessed the frequency of physical activity, but not the duration or intensity via self-report or objective measurement; thus, our measure may over or underestimate the actual adherence to the original definition of the AHA physical activity goal that is based on minutes of physical activity per week. Fourth, BF% was measured through bioelectrical impedance, as a rapid and non-invasive measurement tool. Bioelectrical impedance measurements are impacted by hydration, exercise, race/ethnicity, and medical conditions that impact blood flow (Dehghan and Merchant, 2008). The majority of the men were fasting for the bioelectrical impedance measurements, the test was performed prior to exercise and the men were all of a single race/ethnicity, but we cannot exclude differences due to underlying medical conditions. Additionally, we did not transform the bioelectrical impedance analysis using predictive equations due to our study sample being of one race and sex and the interest in continuous associations versus absolute percentages (Courville et al., 2020). Fifth, the original intent of the AAMWW was programmatic rather than research focused. Therefore, we used a structured questionnaire that was not assessed for its psychometric properties. Nonetheless, our study provides novel knowledge underscoring the utility of ideal cardiovascular health in AA men.
5. Conclusion
Higher attainment of ideal cardiovascular health is significantly associated with greater self-reported health and inversely associated with BF% and prevalent diabetes among AA men participating in the AAMWWs. Family history of diabetes is associated with lower attainment of ideal cardiovascular health in AA men. Successful strategies to attain ideal cardiovascular health may be one conduit to improve the overall health, reduce premature mortality and advance health equity in AA men.
CRediT authorship contribution statement
Emmanuela B. Aboagye-Mensah: Conceptualization, Investigation, Writing - original draft, Writing - review & editing, Visualization. Rosevine A. Azap: Conceptualization, Investigation, Writing - original draft, Writing - review & editing, Visualization. James B. Odei: Conceptualization, Methodology, Software, Validation, Formal analysis, Investigation, Writing - review & editing. Darrell M. Gray: Conceptualization, Investigation, Writing - review & editing. Timiya S. Nolan: Conceptualization, Investigation, Writing - review & editing. Rana Elgazzar: Investigation, Writing - review & editing. DeVeonne White: Conceptualization, Resources, Data curation, Writing - review & editing. John Gregory: Conceptualization, Resources, Data curation, Writing - review & editing. Joshua J. Joseph: Conceptualization, Methodology, Software, Formal analysis, Investigation, Resources, Writing - original draft, Writing - review & editing, Visualization, Supervision, Project administration, Funding acquisition.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors wish to thank the staff and participants of the AAMWW. Preparation of this manuscript was supported by The Robert Wood Johnson Foundation (Harold Amos Medical Faculty Development Program ID# 76236, JJJ) and the NIH National Institute of Diabetes and Digestive and Kidney Diseases (K23DK117041, JJJ).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2020.101151.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- American Diabetes Association Standards of Medical Care in Diabetes-2017: Summary of Revisions. Diabetes Care. 2017;40:S1–S142. doi: 10.2337/dc17-S003. [DOI] [PubMed] [Google Scholar]
- Barger S.D., Cribbet M.R., Muldoon M.F. Participant-reported health status predicts cardiovascular and all-cause mortality independent of established and nontraditional biomarkers: evidence from a representative US sample. J. Am. Heart Assoc. 2016;5 doi: 10.1161/JAHA.116.003741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benjamins M.R., Hummer R.A., Eberstein I.W., Nam C.B. Self-reported health and adult mortality risk: an analysis of cause-specific mortality. Soc. Sci. Med. 2004;59:1297–1306. doi: 10.1016/j.socscimed.2003.01.001. [DOI] [PubMed] [Google Scholar]
- Carnethon, M.R., Pu, J., Howard, G., Albert, M.A., Anderson, C.A.M., Bertoni, A.G., Mujahid, M.S., Palaniappan, L., Taylor, H.A., Willis, M., Yancy, C.W., American Heart Association Council on Epidemiology and Prevention; Council on Cardiovascular Disease in the Young; Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology; Council on Functional Genomics and Translational Biology; and Stroke Council, 2017. Cardiovascular Health in African Americans: A Scientific Statement From the American Heart Association. Circulation 136, e393–e423. doi:10.1161/CIR.0000000000000534. [DOI] [PubMed]
- Colby, S.L., Ortman, J.M., 2015. Projections of the Size and Composition of the U.S. Population: 2014 to 2060. Population Estimates and Projections. Current Population Reports. P25-1143. US Census Bureau.
- Courville A.B., Yang S.B., Andrus S., Hayat N., Kuemmerle A., Leahy E., Briker S., Zambell K., Chung S., Sumner A.E. Body adiposity measured by bioelectrical impedance is an alternative to dual-energy x-ray absorptiometry in black Africans: the Africans in America Study. Nutrition. 2020;74 doi: 10.1016/j.nut.2020.110733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cronin K.A., Lake A.J., Scott S., Sherman R.L., Noone A.-M., Howlader N., Henley S.J., Anderson R.N., Firth A.U., Ma J., Kohler B.A., Jemal A. Annual Report to the Nation on the Status of Cancer, part I: national cancer statistics. Cancer. 2018;124:2785–2800. doi: 10.1002/cncr.31551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dehghan M., Merchant A.T. Is bioelectrical impedance accurate for use in large epidemiological studies? Nutr. J. 2008;7:26. doi: 10.1186/1475-2891-7-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeSalvo K.B., Bloser N., Reynolds K., He J., Muntner P. Mortality prediction with a single general self-rated health question. J. Gen. Intern. Med. 2006;21:267. doi: 10.1111/j.1525-1497.2005.00291.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong C., Rundek T., Wright C.B., Anwar Z., Elkind M.S.V., Sacco R.L. Ideal cardiovascular health predicts lower risks of myocardial infarction, stroke, and vascular death across whites, blacks, and hispanics: the northern Manhattan study. Circulation. 2012;125:2975–2984. doi: 10.1161/CIRCULATIONAHA.111.081083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Effoe V.S., Carnethon M.R., Echouffo-Tcheugui J.B., Chen H., Joseph J.J., Norwood A.F., Bertoni A.G. The American Heart Association ideal cardiovascular health and incident type 2 diabetes mellitus among blacks: the Jackson heart study. J. Am. Heart Assoc. 2017;6 doi: 10.1161/JAHA.116.005008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flensborg-Madsen T., Johansen C., Grønbæk M., Mortensen E.L. A prospective association between quality of life and risk for cancer. Eur. J. Cancer. 2011;47:2446–2452. doi: 10.1016/j.ejca.2011.06.005. [DOI] [PubMed] [Google Scholar]
- Ford Earl S., Greenlund Kurt J., Yuling Hong. Ideal cardiovascular health and mortality from all causes and diseases of the circulatory system among adults in the United States. Circulation. 2012;125:987–995. doi: 10.1161/CIRCULATIONAHA.111.049122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford E.S., Greenlund K.J., Hong Y. Ideal cardiovascular health and mortality from all causes and diseases of the circulatory system among adults in the United States. Circulation. 2012;125:987–995. doi: 10.1161/CIRCULATIONAHA.111.049122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fretts A.M., Howard B.V., McKnight B., Duncan G.E., Beresford S.A.A., Mete M., Zhang Y., Siscovick D.S. Life’s simple 7 and incidence of diabetes among American Indians: The strong heart family study. Diabetes Care. 2014;37:2240–2245. doi: 10.2337/dc13-2267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fyfe-Johnson A.L., Ryder J.R., Alonso A., MacLehose R.F., Rudser K.D., Fox C.K., Gross A.C., Kelly A.S. Ideal cardiovascular health and adiposity: implications in youth. J. Am. Heart Assoc. Cardiovasc. Cerebrovasc. Dis. 2018;7 doi: 10.1161/JAHA.117.007467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes A.J., Clarke P.M., Glasziou P.G., Simes R.J., Drury P.L., Keech A.C. Can self-rated health scores be used for risk prediction in patients with type 2 diabetes? Diabetes Care. 2008;31:795–797. doi: 10.2337/dc07-1391. [DOI] [PubMed] [Google Scholar]
- Joseph, J.J., Golden, S.H., 2017. Diabetes in Native Populations and Underserved Communities in the USA, in: Dagogo-Jack, S. (Ed.), Diabetes Mellitus in Developing Countries and Underserved Communities. Springer International Publishing, Cham, pp. 251–284.
- Joseph J.J., Echouffo-Tcheugui J.B., Carnethon M.R., Bertoni A.G., Shay C.M., Ahmed H.M., Blumenthal R.S., Cushman M., Golden S.H. The association of ideal cardiovascular health with incident type 2 diabetes mellitus: the Multi-Ethnic Study of Atherosclerosis. Diabetologia. 2016;59:1893–1903. doi: 10.1007/s00125-016-4003-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joseph J.J., Bennett A., Echouffo Tcheugui J.B., Effoe V.S., Odei J.B., Hidalgo B., Dulin A., Safford M.M., Cummings D.M., Cushman M., Carson A.P. Ideal cardiovascular health, glycaemic status and incident type 2 diabetes mellitus: the REasons for Geographic and Racial Differences in Stroke (REGARDS) study. Diabetologia. 2019;62:426–437. doi: 10.1007/s00125-018-4792-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kochanek K., Murphy S., Xu J., Arias E. Deaths: Final data for 2017. Natl. Vital Stat. Rep. 2019;68:77. [PubMed] [Google Scholar]
- Lloyd-Jones, D.M., Hong, Y., Labarthe, D., Mozaffarian, D., Appel, L.J., Van Horn, L., Greenlund, K., Daniels, S., Nichol, G., Tomaselli, G.F., Arnett, D.K., Fonarow, G.C., Ho, P.M., Lauer, M.S., Masoudi, F.A., Robertson, R.M., Roger, V., Schwamm, L.H., Sorlie, P., Yancy, C.W., Rosamond, W.D., American Heart Association Strategic Planning Task Force and Statistics Committee, 2010. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation 121, 586–613. doi:10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed]
- Mavaddat N., Parker R.A., Sanderson S., Mant J., Kinmonth A.L. Relationship of self-rated health with fatal and non-fatal outcomes in cardiovascular disease: a systematic review and meta-analysis. PLoS ONE. 2014;9 doi: 10.1371/journal.pone.0103509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noh J.-W., Chang Y., Park M., Kwon Y.D., Ryu S. Self-rated health and the risk of incident type 2 diabetes mellitus: a cohort study. Sci. Rep. 2019;9:1–8. doi: 10.1038/s41598-019-40090-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osibogun O., Ogunmoroti O., Spatz E.S., Burke G.L., Michos E.D. Is self-rated health associated with ideal cardiovascular health? The Multi-Ethnic Study of Atherosclerosis. Clin. Cardiol. 2018;41:1154–1163. doi: 10.1002/clc.22995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Padwal R., Leslie W.D., Lix L.M., Majumdar S.R. Relationship among body fat percentage, body mass index, and all-cause mortality: a cohort study. Ann. Intern. Med. 2016;164:532. doi: 10.7326/M15-1181. [DOI] [PubMed] [Google Scholar]
- Rasmussen-Torvik L.J., Shay C.M., Abramson J.G., Friedrich C.A., Nettleton J.A., Prizment A.E., Folsom A.R. Ideal cardiovascular health is inversely associated with incident cancer: the Atherosclerosis Risk In Communities study. Circulation. 2013;127:1270–1275. doi: 10.1161/CIRCULATIONAHA.112.001183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shay C.M., Ning H., Allen N.B., Carnethon M.R., Chiuve S.E., Greenlund K.J., Daviglus M.L., Lloyd-Jones D.M. Status of cardiovascular health in US adults: prevalence estimates from the National Health and Nutrition Examination Surveys (NHANES) 2003–2008. Circulation. 2012;125:45–56. doi: 10.1161/CIRCULATIONAHA.111.035733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shikany J.M., Schoenberger Y.-M.M., Konety B.R., Vickers S.M. African American Men’s Health: research, practice, and policy. Am. J. Prev. Med. 2018;55:S1–S4. doi: 10.1016/j.amepre.2018.07.011. [DOI] [PubMed] [Google Scholar]
- Spahillari A., Talegawkar S., Correa A., Carr J.J., Terry J.G., Lima J., Freedman J.E., Das S., Kociol R., de Ferranti S., Mohebali D., Mwasongwe S., Tucker K.L., Murthy V.L., Shah R.V. Ideal cardiovascular health, cardiovascular remodeling, and heart failure in blacks: the Jackson heart study. Circ. Heart Fail. 2017;10 doi: 10.1161/CIRCHEARTFAILURE.116.003682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veromaa V., Kautiainen H., Juonala M., Rantanen A., Korhonen P.E. Self-rated health as an indicator of ideal cardiovascular health among working-aged women. Scand. J. Prim. Health Care. 2017;35:322–328. doi: 10.1080/02813432.2017.1397299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wennberg, P., Rolandsson, O., A, D.L. van der, Spijkerman, A.M.W., Kaaks, R., Boeing, H., Feller, S., Bergmann, M.M., Langenberg, C., Sharp, S.J., Forouhi, N., Riboli, E., Wareham, N., 2013. Self-rated health and type 2 diabetes risk in the European Prospective Investigation into Cancer and Nutrition-InterAct study: a case-cohort study. BMJ Open 3, e002436. doi:10.1136/bmjopen-2012-002436. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.