Abstract
Purpose of Review
This review discusses the role of the patient-centered medical home (PCMH) in treating depression, focusing on findings from primary care-based studies and their implications for the PCMH.
Recent Findings
Pharmacotherapy, psychotherapy, and collaborative care are evidence-based treatments for depression that can be delivered in primary care and extended to diverse populations. Recent research aligns with the core components of the PCMH model.
Summary
The core components of the PCMH are critical elements of depression treatment. Comprehensive care within the PCMH addresses medical and behavioral health concerns, including depression. Psychiatric and psychological care must be flexibly delivered so services remain accessible yet patient-centered. To ensure the quality and safety of treatment, depression symptoms must be consistently monitored. Coordination within and occasionally outside of the PCMH is needed to ensure patients receive the appropriate level of care. More research is needed to empirically evaluate depression treatment within the PCMH.
Keywords: Depression, Primary care, Integrated behavioral health, Mental health integration, Evidence-based care, Implementation and dissemination
Introduction
The patient-centered medical home (PCMH) model was first proposed by the American Academy of Pediatrics (AAP) in 1967 and expanded by the American Academy of Family Physicians, AAP, American College of Physicians, and American Osteopathic Association in 2007. The original joint principles of the PCMH [1] have been further distilled into five core components (Table 1) [2]. In short, the PCMH serves as the cornerstone of healthcare for patients and their families; a multidisciplinary team works together to meet most patient needs through the provision of evidence-based, patient-centered, easily accessible comprehensive care and coordinates with other specialties as necessary.
Table 1.
Core components of the patient-centered medical home (PCMH) model adapted from the Agency for Healthcare Research and Quality [2]
| Core component | Description |
|---|---|
| Comprehensive care | Multidisciplinary team meets most of patients’ medical and behavioral health needs through prevention, acute care, and chronic care |
| Patient-centered | Adopt a whole-person perspective, which respects patients’ needs, culture, values, and preferences and includes patients and their families in the decision-making process |
| Coordinated care | Increase coordination with emergency, specialty, home health, and community services in the healthcare system and improve communication between care teams |
| Accessible services | Expand patients’ access through urgent availability, extended in-person hours, and multimodal communication with the care team |
| Quality and safety | Apply evidence-based practices in a population health perspective, use a data-driven approach to assess and improve practice performance, and regularly evaluate outcomes, adverse events, and patients’ perspectives to advance services |
In 2014, the Working Party Group on Integrated Behavioral Healthcare called for behavioral healthcare to be included in the PCMH model. Behavioral health is a more holistic approach that addresses the emotional, behavioral, and physical aspects of well-being. More than half of primary care patients experience emotional or behavioral problems, which can negatively impact their physical health and impair their ability to fully engage in treatment [3]. Consequently, the PCMH model must include behavioral health for care to be considered comprehensive [4]. Different strategies for delivering behavioral health services within primary care have been proposed. The World Federation of Societies of Biological Psychiatry’s Collaborative Mental Health Care Task Force advocated for incorporating primary care providers in the delivery of mental health services, increasing communication and collaboration with behavioral health providers, and implementing systems-level approaches to improve existing services, develop novel programs, and reduce barriers [5••].
Within the PCMH, depression is the most commonly occurring mental health condition. Prevalence rates in primary care range from 8 to 14% [6], though this is likely an underestimate given the low rate of depression screening conducted in this setting [7]. Depression is considered to be a chronic condition, with recurrence rates of 40% observed over time [8]. Depression has a significant impact on health and functioning as evidenced by increased rates of disability and risk for morbidity and mortality among depressed individuals [9]. Together, this highlights the need for screening, prevention, intervention, and relapse prevention.
Primary care is well positioned to undertake such efforts as the majority of patients already obtain depression treatment from their general medical provider [10]. The structure of the PCMH model is well suited to deliver the majority of depression treatment [3], with specialty care available for more critical cases. First, the population-based model of care used in the PCMH allows for more timely access to treatment than specialty care. Second, the PCMH can offer more comprehensive services when psychiatric and psychological treatments are provided in the same setting, resulting in a wider range of treatment options for patients to choose from. Third, the PCMH consists of a multidisciplinary team, which can enhance coordination between behavioral health and primary care providers compared to specialty care. Finally, the PCMH can consistently monitor depressive symptoms over time due to more frequent contact than specialty care, which enables treatment to be adjusted or re-initiated.
The purpose of this review is to contextualize the role of the PCMH in treating depression. We will review the most recent research on depression treatment in primary care. The vast majority of the literature has been conducted in this setting rather than specifically within a PCMH. While primary care practices that demonstrate fidelity to the PCMH model can obtain recognition through different organizations [11], few articles note if certification has been obtained. This makes it challenging to accurately discern if the setting in which studies have taken place adheres to the PCMH model. Therefore, we will review the research more generally and discuss the applicability of these findings in the PCMH based on their alignment with the model’s five core components [2].
Components of Depression Treatment in the PCMH
Pharmacotherapy
Antidepressant medications can be an important component of depression treatment in the PCMH. Research has supported the use of antidepressant medications within the primary care setting. Meta-analyses of randomized controlled trials (RCTs) conducted in primary care suggest that antidepressant medications are superior to placebo, though this research-base is smaller and less robust than trials conducted in research or specialty settings [12, 13]. The Sequenced Treatment Alternative to Relieve Depression (STAR*D) study, the largest depression-focused RCT to date, showed similar outcomes when antidepressant medications were prescribed in either the primary or specialty setting [14]. There are challenges in translating these findings to clinical practice. STAR*D involved close follow-up and multiple stepped-care options, which included switching or augmenting antidepressant medications or initiating cognitive behavioral therapy. In both specialty and primary care settings, there are challenges in arranging multiple points of contact to ensure that depressed patients who are not improving are offered other treatment options. In addition, multiple barriers make it difficult for patients to receive an adequate medication trial [15]. Consequently, there are concerns about nonadherence and discontinuation in real-world settings.
Studies have assessed if interventions addressing such barriers can be used to improve antidepressant medication adherence in primary care in an effort to increase the likelihood of response and remission. LeBlanc and colleagues [16] reported that patients who used a shared decision making aid reported more comfort, knowledge, and satisfaction with their choice of antidepressant medication and were more involved in the decision-making process than those receiving usual care. However, depression response and remission and medication use and adherence did not differ by group. Sirey and colleagues [17] showed that patients who engaged in a psychosocial intervention targeting antidepressant medication adherence were more likely to be adherent at 6 and 12 weeks than those receiving usual care. Although the intervention group exhibited a larger initial reduction in depressive symptom severity, symptom improvement was similar across groups at 24 weeks.
One major difference between usual practice and research studies conducted in this setting, such as STAR*D, is the consistent use of measures to track patient recovery and adjust treatment accordingly. Measurement-based care for depression has been associated with increased treatment adjustments, resulting in improved remission rates [18•, 19]. This research highlights the importance of regularly providing prescribers and patients with feedback on treatment progress. However, this can be challenging to translate into clinical practice. A recent quality improvement study by Jha and colleagues [20•] showed low engagement in a measurement-based care depression program delivered by primary care providers, highlighting the need for further efforts to help bridge the gap between science and practice.
Shared decision-making interventions and the use of feedback on improvement, or lack thereof, are all examples of patient-centered care. Patient-centered care encourages patients and their families to be involved in their treatment, which can be facilitated through individualized treatment plans and data-driven medication adjustments. Interventions such as actively engaging patients in the decision-making process [16], addressing barriers to adherence [17], and consistently evaluating symptomatology, safety, and tolerability [18•] are practical ways that prescribers can enhance patient-centered care within the PCMH. Implementing these interventions will likely involve coordination with other behavioral health providers working within the PCMH to leverage the time and skill set of the multidisciplinary team.
Psychotherapy
Psychological interventions are another important component of depression treatment in the PCMH. Research has suggested that brief psychotherapy for depression (e.g., cognitive behavioral therapy, problem solving therapy, interpersonal therapy) can be effectively delivered within the primary care setting [21••]. Meta-analyses indicate that psychological interventions for depression outperform waitlist, sham, or usual care control comparisons in primary care, with effect sizes ranging from small to medium [22–28]. There is some evidence that psychotherapy provided in research studies or specialty clinics is associated with larger effect sizes, which could be due to enhanced personalization, longer treatment length, patient characteristics, or provider availability and experience [26, 27]. Barriers to psychotherapy are similar to pharmacotherapy and include poor treatment attendance and adherence, limited access to psychotherapy in primary care, and inconsistent use of measurement-based care across practices. In addition, psychotherapy trials include measures of adherence to the therapy delivered, while in practice as usual, there may be differences in the quality of therapy that is offered [29].
An important next step is evaluating how psychological interventions for depression perform in real-world settings. Large-scale implementation efforts, such as the Improving Access to Psychological Therapies (IAPT) program in the UK, have reported promising results among depressed patients [30, 31]. While these results are encouraging, there are significant differences in practices, populations, and resources across healthcare systems. Therefore, psychological interventions for depression must be evaluated in a wide variety of primary care settings.
Primary care practices that adhere to the PCMH model have begun to conduct naturalistic studies of their outcomes. Sawchuk and colleagues [32•] sampled five PCMH clinics at Mayo Clinic delivering short-term evidence-based psychotherapy. This approach includes a registry to track clinical outcomes with self-report measures, consultation for challenging cases, and concerted efforts to maintain fidelity to a given therapeutic approach [33]. While anxiety was the most common presenting problem, 28% of patients met criteria for a depressive disorder. Among depressed patients, the psychological principles most frequently used during treatment included cognitive strategies and behavioral activation. Compared to baseline, depressed patients reported a significant decrease in self-reported depressive symptoms on the Patient Health Questionniare-9 (PHQ-9) at the last recorded session (d = 0.51). Among patients reporting moderate to severe depressive symptoms at the time of initial consultation, 39% responded to treatment and 23% achieved remission. While these findings support the use of short-term psychotherapy for depression in the PCMH, the conclusions that can be drawn are limited as this survey lacked a comparison condition and did not control for potential confounding variables. This study adds value in showing the feasibility of including measurement-based care and a formalized process for addressing fidelity to therapeutic skills in general practice. A combination of pragmatic trials and observational studies across diverse settings are needed to further this research.
When undertaking such efforts in the PCMH, psychotherapy must be evidence-based yet accessible. There is a growing body of evidence that psychological interventions can be effectively delivered using diverse methods [22–27]. Consequently, there is some flexibility with how such services can be provided within the PCMH. One option is to employ a stepped-care approach. For example, therapist-guided technology- and group-based psychotherapy can serve as lower-intensity, resource-conservative approaches with in-person individual psychotherapy available as a step-up option for patients with more severe symptoms or who have not responded to lower levels of care [34]. While this approach can increase the accessibility of evidence-based treatment for a larger portion of the population, it must be flexibly applied. Patients should be included in the decision-making process to ensure care remains patient-centered.
Collaborative Care
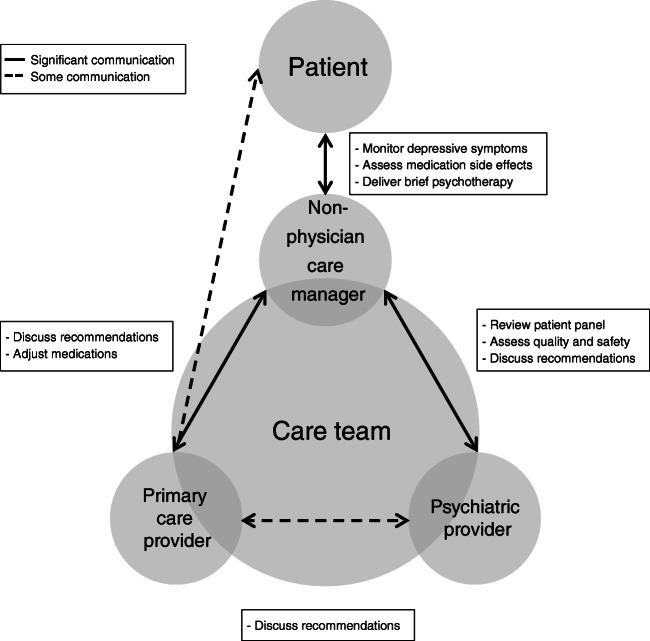
Collaborative care is a key approach to depression treatment in the PCMH. Collaborative care conceptualizes depression as a chronic condition that must be managed over time. The chronic care model [35] originally developed for managing chronic physical conditions was used as the conceptual framework for collaborative care for depression. Across collaborative care programs, the core components include team-driven, population-focused, measurement-guided, and evidence-based care [36]. The model addresses some of the previously mentioned challenges in primary care by increasing self-report measures and establishing feedback loops to ensure patients who are not improving are identified so treatment can be modified. Services are delivered by a multidisciplinary team with non-physician care managers providing direct patient care (Fig. 1).
Figure 1.
Roles of the multidisciplinary care team and patterns of communication within the collaborative care model
Collaborative care leverages the multidisciplinary team to provide services to a larger swath of the population than could be managed by face-to-face evaluations. Communication between the multidisciplinary team is formally facilitated through a systematic case review (SCR) during which care managers review their patient panels with a psychiatric provider who provides individualized treatment recommendations for each patient that are reviewed with the primary care provider. Best practices for SCR include regularly scheduled meetings, maintaining a focus on collaborative care rather than other topics, ensuring adequate time is spent on all patients, discussing patient responders and non-responders, and guiding care managers in establishing appropriate boundaries with challenging patients [37•]. A regular SCR has been shown to be associated with increased likelihood of medication adjustments [38] and improvement in depressive symptoms [39] among primary care patients who do not report a decrease in self-reported depressive symptoms within the first 8 weeks of treatment. The Centers for Medicare and Medicaid Services (CMS) released billing codes to support collaborative care for behavioral health problems, which were designed to reinforce the key components of care coordination including the SCR [40].
The empirical evidence supports collaborative care for depression. A Cochrane review [41] found that collaborative care was associated with improved depression outcomes, increased antidepressant medication use, and enhanced mental health quality of life compared to care as usual at 0–6, 7–12, and 13–24 months. More recent studies have replicated this finding, with primary care patients enrolled in collaborative care programs reporting greater reductions in depressive symptoms and improvements in quality of life at 3 to 12 months follow-up compared to treatment as usual and co-location of behavioral health [42–44]. There has been an effort to disseminate collaborative care programs to more diverse populations, with encouraging results among racial/ethnic minorities [45, 46] and patients with limited English language proficiency [47]. Observational studies from our certified PCMH at Mayo Clinic have indicated that patients participating in collaborative care remitted sooner and experienced residual depressive symptoms for a shorter length of time than patients receiving usual care [48]. Among Mayo Clinic employees enrolled in collaborative care, depression response and remission were greater at 12 months compared to usual care [49•].
Collaborative care programs have also expanded to include depressed patients diagnosed with chronic medical conditions given their high comorbidity among this population [50]. A recent meta-analysis found that collaborative care programs for depression and comorbid chronic medical conditions result in greater reductions in illness burden (d = 0.27) and depressive symptoms (d = 0.35) than treatment as usual, with improvements in physical outcomes observed for some, but not all, chronic health conditions (OR = 1.31–4.19) [51]. One of the largest primary care-based initiatives was the Care of Mental, Physical and Substance-use Syndromes (COMPASS) trial, a collaborative care program for patients with depression and comorbid diabetes and/or cardiovascular disease delivered in primary care clinics across eight states [52]. Results from the COMPASS trial were promising, with improvements in depressive symptoms (24% response, 16% remission) and control of blood sugar (23%) and blood pressure (58%) observed around 11 months [53]. This project generated important insights on how to effectively implement large-scale multi-site programs to address population health [54].
Qualitative research surveying healthcare providers, institutional administrators, and insurance companies experienced with collaborative care found a surprising degree of consensus that collaborative care was worthwhile and should be a part of primary care [55, 56]. Despite the available evidence, collaborative care has not been widely implemented across primary care practices. A national survey indicated that collaborative care programs for depression were less common than those for diabetes, asthma, and congestive heart failure [57]. Several groups, such as the American Psychiatric Association, have advocated for the expansion of collaborative care for depression as CMS has established new billing opportunities [40]. While recent studies have explored ways to improve implementation efforts [58], there are challenges associated with successfully implementing and sustaining collaborative care [59–61]. A major challenge is the tension between fidelity to an evidence-based model and the need for local adaptations. To this point, a study examining the implementation of collaborative care in primary care practices across Minnesota failed to find differences in depression remission rates among patients enrolled in collaborative or usual care, which was probably related to challenges in ensuring fidelity in real-world implementation efforts as compared to research trials [62].
While the literature clearly supports the efficacy and effectiveness of collaborative care programs for depression, there is still work to be done to enhance and expand implementation. Such efforts are especially important in the PCMH. Coordination of care through formal (i.e., SCR) and informal mechanisms uses the time and expertise of the multidisciplinary team more efficiently, enabling a larger number of patients to access care. Collaborative care programs often provide care through multiple modalities (e.g., in-person, telephone), allowing patients to easily access both psychiatric and psychological services. Patients are able to discuss questions and concerns with their non-physician care manager who communicates with the multidisciplinary team so care remains patient-centered. Consistent symptom monitoring allows the multidisciplinary team to evaluate the quality and safety of care, adjust treatment, and identify if a higher-level of care is necessary.
Special Considerations for Treating Depression in the PCMH: Specific Populations
A diverse range of patients commonly present in primary care clinics, which may be an optimal location to serve their behavioral health needs. Recent research has focused on special considerations for treating depression in pediatric, geriatric, and rural populations.
Pediatrics
Depression begins to present early in life, with prevalence rates sharply increasing from childhood to adolescence [63]. However, depression diagnosis and treatment are inadequate among pediatric populations as the limited numbers of specialists makes it challenging to access care [64, 65]. Primary care is an ideal setting to manage pediatric depression as this population is cared for by a family medicine or pediatric team, allowing for routine assessments and greater opportunity for intervention [66].
Multiple models of care have been proposed for treating depression in youth including co-location, coordinated care, and integrated care. While these models can increase access to and engagement with behavioral health services for pediatric populations, collaboration between providers is necessary to positively impact depression outcomes [66, 67]. Improving collaboration with the limited specialty mental health providers results in improved depression care despite personnel shortages. A meta-analysis on depression treatment in pediatric populations found small yet significant effects for primary care-based integrated care, with the strongest evidence found for collaborative care [68]. Adolescents enrolled in collaborative care programs have shown increased engagement in active treatment despite initial hesitation compared to those receiving treatment as usual [69]. Observational studies from our PCMH at the Mayo Clinic found that pediatric patients enrolled in collaborative care reported higher depression response and remission rates than patients receiving usual care [70•]. Over a quarter (27%) of pediatric patients participating in collaborative care exhibited sustained remission, or minimal depressive symptoms for 3 months [71].
Evidence also supports the efficacy of more intensive interventions for emotional and behavioral problems among pediatric patients in primary care [68•], suggesting that high-quality behavioral health services can be provided in this setting. Weersing and colleagues [72] found support for a brief behavior therapy intervention for youth anxiety and depressive disorders. Children and adolescents who participated in treatment exhibited greater and faster depression and anxiety symptom reduction and functional improvements than those referred for outpatient care. The authors noted that the magnitude of these results was comparable to large-scale RCTs, suggesting that such interventions can be delivered in primary care.
The PCMH is well positioned to serve as the behavioral healthcare hub for children and adolescents. While collaborative care programs have the strongest evidence among pediatric populations, psychological interventions have also been supported should children, adolescents, and their caregivers desire a non-pharmacological option. Providing comprehensive depression treatment for pediatric populations in the PCMH can increase accessibility of services that align with patient and family preferences and improve the continuity of behavioral health care as adolescents transition into young adulthood [65]. Recent publications have supported such efforts with the Guidelines for Adolescent Depression in Primary Care advocating for the advancement of integrated care models such as the PCMH [73].
Geriatrics
There are differences in the presentation, course, and treatment of depression as individuals age. As reviewed by Haigh and colleagues [74], there is a lower prevalence and incidence of major depressive disorder in older versus younger cohorts. However, older adults experience elevated depressive symptoms, subsyndromal depression, and depressive disorders; experience a more chronic course; and may be less responsive to antidepressant medications. Primary care is the ideal setting to manage late-life depression due to the high rate of depression in and service utilization of primary care by geriatric populations [75].
Multiple treatment approaches have been proposed for depression treatment among older adults including co-location, collaborative care, and integrated care. Similar to pediatric populations, these models can increase access to behavioral health services but collaboration between providers is necessary to improve depression outcomes [75]. Collaborative care programs have been adapted to meet the needs of geriatric populations. For example, programs have assessed if depression treatment could be delivered in patients’ homes. A RCT and naturalistic study have shown promising results with reductions in depressive symptoms observed among older adults with moderate to severe depressive symptoms at 3–12 months follow-up [76, 77]. Collaborative care programs have also been adapted for subclinical depression given its higher prevalence among older adults. One RCT showed that collaborative care was associated with greater reductions in depressive symptoms at 4 and 12 months and lower rates of moderate to severe depressive symptoms at 12 months compared to usual care, though there was significant attrition at follow-up [78]. These studies provide preliminary evidence that adapted collaborative care programs may help to manage depressive symptoms and mitigate the onset of a major depressive episode in geriatric populations.
Worldwide, older adults are the fastest growing segment of the population [79]. The PCMH model is well suited to manage their behavioral healthcare needs. Collaborative care programs are a promising method for providing coordinated and comprehensive care to geriatric populations. Adapted collaborative care programs [76–78] may help to make services more accessible and enable older adults experiencing subclinical symptoms to still access evidence-based care. Further evaluation is necessary to ensure there is a sufficient evidence-base before adapted collaborative care programs are implemented on a large-scale.
Cultural Considerations
The primary care population includes patients from diverse backgrounds. There is a budding literature on the cultural considerations for behavioral healthcare providers practicing in such settings, which includes cultural case formulations, culturally informed interventions, and effective use of interpreters [80]. While all aspects of diversity are important, there has been a recent focus on expanding primary care services to rural populations.
Rural populations have limited access to behavioral health services. Telehealth has been explored as a potential way to improve access to care without increasing the burden of travel. Telehealth services have been shown to be as effective as in-person services [81]. This has led to a rapid expansion of such services, with annual growth rates averaging 45% among Medicare patients residing in a rural community with a mental health diagnosis [82]. There has been a concerted effort to disseminate telehealth-based collaborative care for depression in primary care settings that serve rural populations. RCTs recruiting rural populations have found that telehealth-based collaborative care results in higher depression response and remission rates than practice-based collaborative care or care as usual [83•, 84•]. Recent research has suggested that outcomes among rural populations may differ based on patient-level factors. For example, a comparison of civilian and veteran populations engaged in collaborative care found lower depression response rates among male veterans [85•]. Among patients enrolled in our collaborative care program at the Mayo Clinic, we observed increased depression remission among rural versus urban populations, though this association diminished with increased distance from the PCMH [86•]. Together, these studies suggest that more work is needed to tailor telehealth services for rural populations.
More broadly, telehealth is one way to increase the access of behavioral health services within the PCMH. A pressing question for the PCMH is how to provide population-based depression treatment. The use of technology can help the multidisciplinary team leverage resources more efficiently, enabling a larger proportion of the primary care population to easily access evidence-based treatment [87, 88•]. The importance of such services has become evident in the context of COVID-19 with the continued need for services despite restricted in-person contact. While the expansion of telehealth is necessary to meet patients’ needs, it should be one of many options available as certain populations have limited internet access and online literacy, or are concerned about privacy and security [89]. Therefore, it is important that the PCMH adopts a patient-centered response to ensure that telehealth services reduce, rather than exaggerate, health disparities.
Challenges of Treating Depression in the PCMH
While the PCMH is well positioned to provide a large proportion of depression treatment, the care of some patients can be challenging. One example is patients with treatment-resistant depression, which has been operationalized as a lack of response or remission following two or more adequate courses of treatment [90]. The literature on treatment-resistant depression is limited, with some support for antidepressant augmentation and adjunctive psychotherapy [91, 92]. Even fewer studies have been conducted in the primary care setting [93–95], resulting in uncertainty over what may be the most effective practices. Providing care for patients with treatment-resistant depression will require the PCMH to determine how to balance the needs of the patient with the needs of the population. While the multidisciplinary team can provide comprehensive care and monitor depressive symptoms [94–96], it may be necessary to coordinate with specialty clinics that can offer a wider variety of treatment options. Additional examples include patients with subclinical depression as this will encompass a large proportion of the PCMH population and patients with suicidal ideation or behavior who require consistent monitoring and coordination with emergency services if hospitalization is necessary.
Conclusions
In this review, we presented the recent advances in primary care-based depression treatment. Pharmacotherapy and psychotherapy can be used to treat depression in primary care, though there is some evidence that treatment effect sizes are smaller in this setting. While antidepressant medications are an evidence-based treatment option, nonadherence and discontinuation continue to be a challenge. Shared decision-making interventions targeting adherence have not been shown to significantly impact clinical outcomes, but do appear to influence patient perception of or engagement with treatment. When treatment is combined with feedback in measurement-based care, outcomes improve. Psychological interventions are typically provided in-person to individual patients. There do not appear to be significant differences based on how treatment is formatted and delivered, indicating that psychotherapy can be flexibly provided in primary care. The potential of psychotherapy in primary care may not yet be fully realized as there remain barriers of access, fidelity, and adherence. Further research with comparison populations is needed. Collaborative care has also demonstrated improved outcomes for depression in primary care. Studies disseminating collaborative care programs to diverse populations and patients with comorbid medical concerns have found promising results. Despite this, implementation of collaborative care programs for depression has lagged compared to those for chronic medical conditions.
We then discussed how these findings are applicable to and align with the PCMH model. The core components of the PCMH model can help to guide depression treatment (Table 2), striking the delicate balance between individual patient care and overall population needs to ensure the best possible care is provided. The routine use of outcome measures helps to ensure that individual patients are monitored effectively during early stages of recovery for changes in treatment and/or referral to appropriate services, and that those most needing attention in a population are contacted and invited into care. At the provider-level, the core components should guide treatment recommendations, clinical practice, and patient interactions. This extends to all providers employed in primary care, including primary care providers, as interdisciplinary coordination is essential to depression treatment in the PCMH. At the practice-level, the core components should inform program development and quality improvement projects. Such efforts are needed to ensure that depression treatment aligns with the PCMH model. Ideally, behavioral health services would be integrated into primary care and depression care within the primary care setting would include measurement of outcomes, shared decision-making, on-site psychotherapy, collaborative care, and appropriate adaptations for special populations. Of note, many of the treatment strategies, methods, and modalities discussed are not widely available across primary care practices but are necessary for care to be patient-centered and accessible to the entire population. A thoughtful approach to implementation based on the lessons learned from previous endeavors may be helpful for ensuring initial success and sustainability of these programs. At the systems-level, these findings point to the need to advocate for the continuation of telehealth benefits after COVID-19 has resolved and further expansion of billing codes for primary care-based depression care. While more research is needed to fully characterize the costs and benefits of the PCMH model as it applies to mental health issues [97, 98], its conceptual framework has been shown to improve the quality, safety, and accessibility of depression treatment in the primary care setting.
Table 2.
Depression treatment within the patient-centered medical home (PCMH) model [2]
| Core component | Description | Depression treatment in the PCMH |
|---|---|---|
| Comprehensive care | Multidisciplinary team meets most of patients’ medical and behavioral health needs through prevention, acute care, and chronic care | Comprehensive care is rarely provided in the traditional healthcare system. Including behavioral health in the PCMH enables all aspects of health to be addressed in a single setting, which is especially important for depression as medical comorbidity is common. Psychiatric and psychological services can meet acute and chronic needs. |
| Patient-centered | Adopt a whole-person perspective, which respects patients’ needs, culture, values, and preferences and includes patients and their families in the decision-making process | Depression is difficult to treat with a single approach, which is the typical model of care in specialty settings. The PCMH offers psychiatric and psychological treatments delivered in diverse ways to meet the needs of the population. Patients, rather than providers, decide which treatment they want to pursue and obtain assistance from providers in achieving their treatment goals. |
| Coordinated care | Increase coordination with emergency, specialty, home health, and community services in the healthcare system and improve communication between care teams | Communication between providers is uncommon in the fragmented healthcare system. To adequately treat depression, a multidisciplinary team must address the medical, behavioral health, and social needs of the patient in a coordinated fashion. When indicated, the PCMH coordinates with other specialties to ensure patients receive the appropriate level of care. |
| Accessible services | Expand patients’ access through urgent availability, extended in-person hours, and multimodal communication with the care team | Access to behavioral health care is limited in the traditional healthcare system. The PCMH population-based model of care can increase access to depression treatment, especially for underserved populations who typically obtain care in this setting. A stepped-care approach leverages the team’s time and expertise to increase access to psychiatric and psychological services. |
| Quality and safety | Apply evidence-based practices in a population health perspective, use a data-driven approach to assess and improve practice performance, and regularly evaluate outcomes, adverse events, and patients’ perspectives to advance services | While measurement-based care is less common in psychiatric and psychological practices, it is expected within the PCMH. Consistent depression symptom monitoring can identify patients within the population who require treatment and assess progress among patients receiving evidence-based treatment. This information can be used to guide treatment on a patient-level and monitor performance at the practice-level. |
Importantly, further empirical evaluation of depression treatment in the PCMH is needed. Studies should assess treatment outcomes, patient experience, and service utilization in PCMHs and if these findings differ from non-PCMH practices. While PCMH practices have started to report treatment outcomes, the literature base is limited. Additional studies across diverse practices are needed to understand the effectiveness of depression treatment in the PCMH and inform program development and implementation efforts. Patient perception of care appears to be an important factor, with higher rates of treatment initiation and continuation observed among depressed patients who reported positive PCMH experiences [99]. Additional investigations are needed to increase our understanding of the aspects of care associated with improved patient experience and how these factors impact treatment engagement and outcomes within the PCMH. Another important factor is service utilization. Some studies have shown that the greater adherence to the PCMH model is associated with reduced specialty mental health [100] and emergency department visits [101] among patients with a depressive disorder. Further research is warranted to determine if providing depression treatment in the PCMH impacts the larger healthcare system, including reductions in healthcare costs, which can strengthen the argument for further expansion of the PCMH model. Ultimately, empirical evidence will determine the role of the PCMH in treating depression.
Acknowledgments
Olivia E. Bogucki, Mark D. Williams, and Craig N. Sawchuk were supported by the Division of Integrated Behavioral Health, Mayo Clinic. Leif I. Solberg and Rebecca C. Rossom were supported by HealthPartners Institute.
Compliance with Ethical Standards
Conflict of Interest
Olivia E. Bogucki, Mark D. Williams, Leif I. Solberg, Rebecca C. Rossom, and Craig N. Sawchuk declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Psychiatry in Primary Care
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.American Academy of Family Physicians, American Academy of Pediatrics, American College of Physicians, American Osteopathic Association. Joint Principles of the Patient-Centered Medical Home. http://www.aafp.org/dam/AAFP/documents/practice_management/pcmh/initiatives/PCMHJoint.pdf. 2007. Accessed February 1, 2020.
- 2.U.S. Department of Health and Human Services Agency for Healthcare Research and Quality. Defining the PCMH. http://pcmh.ahrq.gov/page/defining-pcmh. Accessed February 1, 2020.
- 3.Baird M, Blount A, Brungardt S, Dickinson P, Dietrich A, Epperly T, et al. Joint principles: integrating behavioral health care into the patient-centered medical home. Ann Fam Med. 2014;12(2):183–5. 10.1370/afm.1633. [DOI] [PMC free article] [PubMed]
- 4.Baird M, Blount A, Brungardt S, Dickinson P, Dietrich A, Epperly T, Green L, Henley D, Kessler R, Korsen N, McDaniel S, Miller B, Pugno P, Roberts R, Schirmer J, Seymour D, deGruy F. The development of joint principles: integrating behavioral health care into the patient-centered medical home. Ann Fam Med. 2014;12(2):183. doi: 10.1370/afm.1634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kates N, Arroll B, Currie E, Hanlon C, Gask L, Klasen H, et al. Improving collaboration between primary care and mental health services. World J Biol Psychiatry. 2019;20(10):748–765. doi: 10.1080/15622975.2018.1471218. [DOI] [PubMed] [Google Scholar]
- 6.Craven MA, Bland R. Depression in primary care: current and future challenges. Can J Psychiatr. 2013;58(8):442–448. doi: 10.1177/070674371305800802. [DOI] [PubMed] [Google Scholar]
- 7.Akincigil A, Matthews EB. National rates and patterns of depression screening in primary care: results from 2012 and 2013. Psychiatr Serv. 2017;68(7):660–666. doi: 10.1176/appi.ps.201600096. [DOI] [PubMed] [Google Scholar]
- 8.Mattisson C, Bogren M, Horstmann V, Munk-Jorgensen P, Nettelbladt P. The long-term course of depressive disorders in the Lundby Study. Psychol Med. 2007;37(6):883–891. doi: 10.1017/S0033291707000074. [DOI] [PubMed] [Google Scholar]
- 9.Kessler RC. The costs of depression. Psychiatr Clin N Am. 2012;35(1):1–14. doi: 10.1016/j.psc.2011.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Olfson M, Blanco C, Marcus SC. Treatment of adult depression in the United States. JAMA Intern Med. 2016;176(10):1482–1491. doi: 10.1001/jamainternmed.2016.5057. [DOI] [PubMed] [Google Scholar]
- 11.American Academy of Family Physicians. PCMH incentive, recognition, and accreditation programs. https://www.aafp.org/practice-management/transformation/pcmh/recognition.html. Accessed April 1, 2020.
- 12.Linde K, Kriston L, Rucker G, Jamil S, Schumann I, Meissner K, Sigterman K, Schneider A. Efficacy and acceptability of pharmacological treatments for depressive disorders in primary care: systematic review and network meta-analysis. Ann Fam Med. 2015;13(1):69–79. doi: 10.1370/afm.1687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arroll B, Chin WY, Martis W, Goodyear-Smith F, Mount V, Kingsford D, Humm S, Blashki G, MacGillivray S. Antidepressants for treatment of depression in primary care: a systematic review and meta-analysis. J Prim Health Care. 2016;8(4):325–334. doi: 10.1071/HC16008. [DOI] [PubMed] [Google Scholar]
- 14.Cain RA. Navigating the sequenced treatment alternatives to relieve depression (STAR*D) study: practical outcomes and implications for depression treatment in primary care. Prim Care. 2007;34(3):505–519. doi: 10.1016/j.pop.2007.05.006. [DOI] [PubMed] [Google Scholar]
- 15.Rush AJ, Thase ME. Improving depression outcome by patient-centered medical management. Am J Psychiatry. 2018;175(12):1187–1198. doi: 10.1176/appi.ajp.2018.18040398. [DOI] [PubMed] [Google Scholar]
- 16.LeBlanc A, Herrin J, Williams MD, Inselman JW, Branda ME, Shah ND, Heim EM, Dick SR, Linzer M, Boehm DH, Dall-Winther KM, Matthews MR, Yost KJ, Shepel KK, Montori VM. Shared decision making for antidepressants in primary care: a cluster randomized trial. JAMA Intern Med. 2015;175(11):1761–1770. doi: 10.1001/jamainternmed.2015.5214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sirey JA, Banerjee S, Marino P, Bruce ML, Halkett A, Turnwald M, et al. Adherence to depression treatment in primary care: a randomized clinical trial. JAMA Psychiat. 2017;74(11):1129–35. 10.1001/jamapsychiatry.2017.3047. [DOI] [PMC free article] [PubMed]
- 18.• Fortney JC, Unutzer J, Wrenn G, Pyne JM, Smith GR, Schoenbaum M, et al. A tipping point for measurement-based care. Psychiatr Serv. 2017;68(2):179–88. 10.1176/appi.ps.201500439 This review paper overviews the rationale and evidence for measurement-based care. [DOI] [PubMed]
- 19.Gondek D, Edbrooke-Childs J, Fink E, Deighton J, Wolpert M. Feedback from outcome measures and treatment effectiveness, treatment efficiency, and collaborative practice: a systematic review. Admin Policy Ment Health. 2016;43(3):325–43. 10.1007/s10488-015-0710-5. [DOI] [PMC free article] [PubMed]
- 20.• Jha MK, Grannemann BD, Trombello JM, Clark EW, Eidelman SL, Lawson T, et al. A structured approach to detecting and treating depression in primary care: VitalSign6 project. Ann Fam Med. 2019;17(4):326–35. 10.1370/afm.2418 This observational study of measurement-based care for depression highlights the challenges associated with implementation, an important next step for improving clinical practice. [DOI] [PMC free article] [PubMed]
- 21.•• Cuijpers P, Quero S, Dowrick C, Arroll B. Psychological treatment of depression in primary care: recent developments. Curr Psychiatry Rep. 2019;21(12):129–39. 10.1007/s11920-019-1117-xThis review paper provides thorough discussion of psychological treatments for depression in primary care. [DOI] [PMC free article] [PubMed]
- 22.Linde K, Rucker G, Sigterman K, Jamil S, Meissner K, Schneider A, et al. Comparative effectiveness of psychological treatments for depressive disorders in primary care: network meta-analysis. BMC Fam Pract. 2015;16:103–17. 10.1186/s12875-015-0314-x. [DOI] [PMC free article] [PubMed]
- 23.Linde K, Sigterman K, Kriston L, Rucker G, Jamil S, Meissner K, Schneider A. Effectiveness of psychological treatments for depressive disorders in primary care: systematic review and meta-analysis. Ann Fam Med. 2015;13(1):56–68. doi: 10.1370/afm.1719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Twomey C, O’Reilly G, Byrne M. Effectiveness of cognitive behavioural therapy for anxiety and depression in primary care: a meta-analysis. Fam Pract. 2015;32(1):3–15. doi: 10.1093/fampra/cmu060. [DOI] [PubMed] [Google Scholar]
- 25.Wells MJ, Owen JJ, McCray LW, Bishop LB, Eells TD, Brown GK, et al. Computer-assisted cognitive-behavior therapy for depression in primary care: systematic review and meta-analysis. Prim Care Companion CNS Disord. 2018;20(2). 10.4088/PCC.17r02196. [DOI] [PubMed]
- 26.Santoft F, Axelsson E, Ost LG, Hedman-Lagerlof M, Fust J, Hedman-Lagerlof E. Cognitive behaviour therapy for depression in primary care: systematic review and meta-analysis. Psychol Med. 2019;49(8):1266–1274. doi: 10.1017/S0033291718004208. [DOI] [PubMed] [Google Scholar]
- 27.Zhang A, Borhneimer LA, Weaver A, Franklin C, Hai AH, Guz S, Shen L. Cognitive behavioral therapy for primary care depression and anxiety: a secondary meta-analytic review using robust variance estimation in meta-regression. J Behav Med. 2019;42:1117–1141. doi: 10.1007/s10865-019-00046-z. [DOI] [PubMed] [Google Scholar]
- 28.Zhang A, Park S, Sullivan JE, Jing S. The effectiveness of problem-solving therapy for primary care patients' depressive and/or anxiety disorders: a systematic review and meta-analysis. J Am Board Fam Med. 2018;31(1):139–150. doi: 10.3122/jabfm.2018.01.170270. [DOI] [PubMed] [Google Scholar]
- 29.Sawchuk CN, Craner JR. Evidence-based psychotherapy in primary care. Focus. 2017;15(3):264–270. doi: 10.1176/appi.focus.20170010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Clark DM, Layard R, Smithies R, Richards DA, Suckling R, Wright B. Improving access to psychological therapy: initial evaluation of two UK demonstration sites. Behav Res Ther. 2009;47(11):910–20. 10.1016/j.brat.2009.07.010. [DOI] [PMC free article] [PubMed]
- 31.Gyani A, Shafran R, Layard R, Clark DM. Enhancing recovery rates: lessons from year one of IAPT. Behav Res Ther. 2013;51(9):597–606. doi: 10.1016/j.brat.2013.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.• Sawchuk CN, Craner JR, Berg SL, Smyth K, Mack J, Glader M, et al. Initial outcomes of a real-world multi-site primary care psychotherapy program. Gen Hosp Psychiatry. 2018;54:5–11. 10.1016/j.genhosppsych.2018.06.005 This naturalistic study reports psychotherapy treatment outcomes in a primary care practice employing the PCMH model. [DOI] [PubMed]
- 33.Craner JR, Sawchuk CN, Mack JD, LeRoy MA. Development and implementation of a psychotherapy tracking database in primary care. Fam Syst Health. 2017;35(2):207–216. doi: 10.1037/fsh0000265. [DOI] [PubMed] [Google Scholar]
- 34.Andrews G, Williams AD. Up-scaling clinician assisted internet cognitive behavioural therapy (iCBT) for depression: a model for dissemination into primary care. Clin Psychol Rev. 2015;41:40–8. 10.1016/j.cpr.2014.05.006. [DOI] [PubMed]
- 35.Wagner EH. Chronic disease management: what will it take to improve care for chronic illness? Eff Clin Prac. 1998;1(1):2–4. [PubMed] [Google Scholar]
- 36.American Psychiatric Association, Academy of Psychosomatic Medicine. Dissemination of integrated care within adult primary care settings: The collaborative care model. http://www.psychiatry.org/File%20Library/Psychiatrists/Practice/Professional-Topics/Integrated-Care/APA-APM-Dissemination-Integrated-Care-Report.pdf2016. Accessed April 23, 2020.
- 37.• Bauer AM, Williams MD, Ratzliff A, Unutzer J. Best practices for systematic case review in collaborative care. Psychiatr Serv. 2019;70(11):1064–7. 10.1176/appi.ps.201900085 This paper provides practical information for conducting a collaborative care systematic case review. [DOI] [PubMed]
- 38.Sowa NA, Jeng P, Bauer AM, Cerimele JM, Unutzer J, Bao Y, et al. Psychiatric case review and treatment intensification in collaborative care management for depression in primary care. Psychiatr Serv. 2018;69(5):549–554. doi: 10.1176/appi.ps.201700243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bao Y, Druss BG, Jung HY, Chan YF, Unutzer J. Unpacking collaborative care for depression: examining two essential tasks for implementation. Psychiatr Serv. 2016;67(4):418–424. doi: 10.1176/appi.ps.201400577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.American Psychiatric Association. FAQs for billing the Psychiatric Collaborative Care Management (CoCM) codes (99492, 99493, 99494, and G0512 in FQHCs/RHCs) and General Behavioral Health Intervention (BHI) code (99484, and G0511 in FQHCs/RHCs). https://www.psychiatry.org/File%20Library/Psychiatrists/Practice/Professional-Topics/Integrated-Care/APA-CoCM-and-Gen-BHI-FAQs.pdf. 2019. Accessed April 23, 2020.
- 41.Archer J, Bower P, Gilbody S, Lovell K, Richards D, Gask L, et al. Collaborative care for depression and anxiety problems. Cochrane Database Syst Rev. 2012;10:1–277. 10.1002/14651858.CD006525.pub2. [DOI] [PMC free article] [PubMed]
- 42.Blackmore MA, Carleton KE, Ricketts SM, Patel UB, Stein D, Mallow A, Deluca JP, Chung H. Comparison of collaborative care and colocation treatment for patients with clinically significant depression symptoms in primary care. Psychiatr Serv. 2018;69(11):1184–1187. doi: 10.1176/appi.ps.201700569. [DOI] [PubMed] [Google Scholar]
- 43.Richards DA, Bower P, Chew-Graham C, Gask L, Lovell K, Cape J, Pilling S, Araya R, Kessler D, Barkham M, Bland JM, Gilbody S, Green C, Lewis G, Manning C, Kontopantelis E, Hill JJ, Hughes-Morley A, Russell A. Clinical effectiveness and cost-effectiveness of collaborative care for depression in UK primary care (CADET): a cluster randomised controlled trial. Health Technol Assess. 2016;20(14):1–192. doi: 10.3310/hta20140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Reed SJ, Shore KK, Tice JA. Effectiveness and value of integrating behavioral health into primary care. JAMA Intern Med. 2016;176(5):691–692. doi: 10.1001/jamainternmed.2016.0804. [DOI] [PubMed] [Google Scholar]
- 45.Lagomasino IT, Dwight-Johnson M, Green JM, Tang L, Zhang L, Duan N, Miranda J. Effectiveness of collaborative care for depression in public-sector primary care clinics serving Latinos. Psychiatr Serv. 2017;68(4):353–359. doi: 10.1176/appi.ps.201600187. [DOI] [PubMed] [Google Scholar]
- 46.Bowen DJ, Powers DM, Russo J, Arao R, LePoire E, Sutherland E, et al. Implementing collaborative care to reduce depression for rural native American/Alaska native people. BMC Health Serv Res. 2020;20(1):34–45. 10.1186/s12913-019-4875-6. [DOI] [PMC free article] [PubMed]
- 47.Garcia ME, Ochoa-Frongia L, Moise N, Aguilera A, Fernandez A. Collaborative care for depression among patients with limited english proficiency: a systematic review. J Gen Intern Med. 2018;33(3):347–357. doi: 10.1007/s11606-017-4242-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Garrison GM, Angstman KB, O'Connor SS, Williams MD, Lineberry TW. Time to remission for depression with collaborative care management (ccm) in primary care. J Am Board Fam Med. 2016;29(1):10–7. 10.3122/jabfm.2016.01.150128. [DOI] [PubMed]
- 49.• Adaji A, Newcomb RD, Wang Z, Williams M. Impact of collaborative care on absenteeism for depressed employees seen in primary care practices: a retrospective cohort study. J Occup Environ Med. 2018;60(1):83–9. 10.1097/JOM.0000000000001173 This observational study reports depression outcomes for a PCMH-based adult collaborative care program. [DOI] [PubMed]
- 50.Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet. 2007;370(9590):851–858. doi: 10.1016/s0140-6736(07)61415-9. [DOI] [PubMed] [Google Scholar]
- 51.van Eck van der Sluijs JF, Castelijns H, Eijsbroek V, Rijnders CAT, van Marwijk HWJ, van der Feltz-Cornelis CM. Illness burden and physical outcomes associated with collaborative care in patients with comorbid depressive disorder in chronic medical conditions: a systematic review and meta-analysis. Gen Hosp Psychiatry. 2018;50:1–14. doi: 10.1016/j.genhosppsych.2017.08.003. [DOI] [PubMed] [Google Scholar]
- 52.Coleman KJ, Magnan S, Neely C, Solberg L, Beck A, Trevis J, Heim C, Williams M, Katzelnick D, Unützer J, Pollock B, Hafer E, Ferguson R, Williams S. The COMPASS initiative: description of a nationwide collaborative approach to the care of patients with depression and diabetes and/or cardiovascular disease. Gen Hosp Psychiatry. 2017;44:69–76. doi: 10.1016/j.genhosppsych.2016.05.007. [DOI] [PubMed] [Google Scholar]
- 53.Rossom RC, Solberg LI, Magnan S, Crain AL, Beck A, Coleman KJ, Katzelnick D, Williams MD, Neely C, Ohnsorg K, Whitebird R, Brandenfels E, Pollock B, Ferguson R, Williams S, Unützer J. Impact of a national collaborative care initiative for patients with depression and diabetes or cardiovascular disease. Gen Hosp Psychiatry. 2017;44:77–85. doi: 10.1016/j.genhosppsych.2016.05.006. [DOI] [PubMed] [Google Scholar]
- 54.Solberg LI, Ferguson R, Ohnsorg KA, Crain AL, Williams MD, Ziegenfuss JY, Boggs JM, Neely C, Brooks L, Molitor BA, Monkman J, Coughlin M. The challenges of collecting and using patient care data from diverse care systems: lessons from COMPASS. Am J Med Qual. 2017;32(5):494–499. doi: 10.1177/1062860616674272. [DOI] [PubMed] [Google Scholar]
- 55.Williams MD, Asiedu GB, Finnie D, Neely C, Egginton J, Finney Rutten LJ, et al. Sustainable care coordination: a qualitative study of primary care provider, administrator, and insurer perspectives. BMC Health Serv Res. 2019;19(1):92–102. 10.1186/s12913-019-3916-5. [DOI] [PMC free article] [PubMed]
- 56.Fontaine P, Whitebird R, Solberg LI, Tillema J, Smithson A, Crabtree BF. Minnesota’s early experience with medical home implementation: viewpoints from the front lines. J Gen Intern Med. 2015;30(7):899–906. doi: 10.1007/s11606-014-3136-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bishop TF, Ramsay PP, Casalino LP, Bao Y, Pincus HA, Shortell SM. Care management processes used less often for depression than for other chronic conditions in US primary care practices. Health Aff (Millwood). 2016;35(3):394–400. doi: 10.1377/hlthaff.2015.1068. [DOI] [PubMed] [Google Scholar]
- 58.Saldana L, Bennett I, Powers D, Vredevoogd M, Grover T, Schaper H, et al. Scaling implementation of collaborative care for depression: adaptation of the stages of implementation completion (SIC). Admin Pol Ment Health. 2017:1–9. 10.1007/s10488-019-00944-z. [DOI] [PMC free article] [PubMed]
- 59.Wood E, Ohlsen S, Ricketts T. What are the barriers and facilitators to implementing collaborative care for depression? A systematic review. J Affect Disord. 2017;214:26–43. doi: 10.1016/j.jad.2017.02.028. [DOI] [PubMed] [Google Scholar]
- 60.Overbeck G, Davidsen AS, Kousgaard MB. Enablers and barriers to implementing collaborative care for anxiety and depression: a systematic qualitative review. Implement Sci. 2016;11(1):165–81. 10.1186/s13012-016-0519-y. [DOI] [PMC free article] [PubMed]
- 61.Price-Haywood EG, Dunn-Lombard D, Harden-Barrios J, Lefante JJ. Collaborative depression care in a safety net medical home: facilitators and barriers to quality improvement. Popul Health Manag. 2016;19(1):46–55. doi: 10.1089/pop.2015.0016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Solberg LI, Crain AL, Maciosek MV, Unützer J, Ohnsorg KA, Beck A, et al. A stepped-wedge evaluation of an initiative to spread the collaborative care model for depression in primary care. Ann Fam Med. 2015;13(5):412–420. doi: 10.1370/afm.1842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ghandour RM, Sherman LJ, Vladutiu CJ, Ali MM, Lynch SE, Bitsko RH, Blumberg SJ. Prevalence and treatment of depression, anxiety, and conduct problems in US children. J Pediatr. 2019;206:256–267. doi: 10.1016/j.jpeds.2018.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zuckerbrot RA, Cheung A, Jensen PS, Stein RE, Laraque D, Group G-PS Guidelines for adolescent depression in primary care (GLAD-PC): part i. practice preparation, identification, assessment, and initial management. Pediatrics. 2018;141(3):e20174081. doi: 10.1542/peds.2017-4081. [DOI] [PubMed] [Google Scholar]
- 65.Babajide A, Ortin A, Wei C, Mufson L, Duarte CS. Transition cliffs for young adults with anxiety and depression: is integrated mental health care a solution? J Behav Health Serv Res. 2019;47:1–18. doi: 10.1007/s11414-019-09670-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kodish I, Richardson L, Schlesinger A. Collaborative and integrated care for adolescent depression. Child Adolesc Psychiatr Clin N Am. 2019;28(3):315–325. doi: 10.1016/j.chc.2019.02.003. [DOI] [PubMed] [Google Scholar]
- 67.Campo JV, Geist R, Kolko DJ. Integration of pediatric behavioral health services in primary care: improving access and outcomes with collaborative care. Can J Psychiatr. 2018;63(7):432–438. doi: 10.1177/0706743717751668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Asarnow JR, Rozenman M, Wiblin J, Zeltzer L. Integrated medical-behavioral care compared with usual primary care for child and adolescent behavioral health: a meta-analysis. JAMA Pediatr. 2015;169(10):929–37. 10.1001/jamapediatrics.2015.1141. [DOI] [PubMed]
- 69.Rapp AM, Chavira DA, Sugar CA, Asarnow JR. Integrated primary medical-behavioral health care for adolescent and young adult depression: predictors of service use in the youth partners in care trial. J Pediatr Psychol. 2017;42(9):1051–1064. doi: 10.1093/jpepsy/jsx057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.• Shippee ND, Mattson A, Brennan R, Huxsahl J, Billings ML, Williams MD. Effectiveness in regular practice of collaborative care for depression among adolescents: a retrospective cohort study. Psychiatr Serv. 2018;69(5):536–41. 10.1176/appi.ps.201700298 This observational study reports depression outcomes for a PCMH-based pediatric collaborative care program. [DOI] [PubMed]
- 71.Ginsburg AD, Stadem PS, Takala CR, Croarkin PE, Mattson AB, Billings ML, et al. An examination of screening tools for collaborative care of adolescent depression. J Clin Psychiatry. 2018;79(4):e1–e8. 10.4088/JCP.17m11543. [DOI] [PubMed]
- 72.Weersing VR, Brent DA, Rozenman MS, Gonzalez A, Jeffreys M, Dickerson JF, Lynch FL, Porta G, Iyengar S. Brief behavioral therapy for pediatric anxiety and depression in primary care: a randomized clinical trial. JAMA Psychiatry. 2017;74(6):571–578. doi: 10.1001/jamapsychiatry.2017.0429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Cheung AH, Zuckerbrot RA, Jensen PS, Laraque D, Stein RE, Group G-PS. Guidelines for adolescent depression in primary care (GLAD-PC): part ii. treatment and ongoing management. Pediatrics. 2018;141(3):e20174082. 10.1542/peds.2017-4082. [DOI] [PubMed]
- 74.Haigh EAP, Bogucki OE, Sigmon ST, Blazer DG. Depression among older adults: a 20-year update on five common myths and misconceptions. Am J Geriatr Psychiatry. 2018;26(1):107–122. doi: 10.1016/j.jagp.2017.06.011. [DOI] [PubMed] [Google Scholar]
- 75.Bruce ML, Sirey JA. Integrated care for depression in older primary care patients. Can J Psychiatr. 2018;63(7):439–446. doi: 10.1177/0706743718760292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Bruce ML, Raue PJ, Reilly CF, Greenberg RL, Meyers BS, Banerjee S, Pickett YR, Sheeran TF, Ghesquiere A, Zukowski DM, Rosas VH, McLaughlin J, Pledger L, Doyle J, Joachim P, Leon AC. Clinical effectiveness of integrating depression care management into medicare home health: the Depression CAREPATH Randomized trial. JAMA Intern Med. 2015;175(1):55–64. doi: 10.1001/jamainternmed.2014.5835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.LaMantia MA, Alder CA, Callahan CM, Gao S, French DD, Austrom MG, et al. The aging brain care medical home: preliminary data. J Am Geriatr Soc. 2015;63(6):1209–1213. doi: 10.1111/jgs.13447. [DOI] [PubMed] [Google Scholar]
- 78.Gilbody S, Lewis H, Adamson J, Atherton K, Bailey D, Birtwistle J, Bosanquet K, Clare E, Delgadillo J, Ekers D, Foster D, Gabe R, Gascoyne S, Haley L, Hamilton J, Hargate R, Hewitt C, Holmes J, Keding A, Lilley-Kelly A, Meer S, Mitchell N, Overend K, Pasterfield M, Pervin J, Richards DA, Spilsbury K, Traviss-Turner G, Trépel D, Woodhouse R, Ziegler F, McMillan D. Effect of collaborative care vs usual care on depressive symptoms in older adults with subthreshold depression: the CASPER randomized clinical trial. JAMA. 2017;317(7):728–737. doi: 10.1001/jama.2017.0130. [DOI] [PubMed] [Google Scholar]
- 79.United Nations Department of Economic and Social Affairs. World: population by broad age groups. https://population.un.org/wpp2019/Graphs/DemographicProfiles/Line/900. 2019. Accessed March 15, 2020.
- 80.Richmond A, Jackson J. Cultural considerations for psychologists in primary care. J Clin Psychol Med Settings. 2018;25(3):305–315. doi: 10.1007/s10880-018-9546-y. [DOI] [PubMed] [Google Scholar]
- 81.Fortney JC, Pyne JM, Turner EE, Farris KM, Normoyle TM, Avery MD, Hilty DM, Unützer J. Telepsychiatry integration of mental health services into rural primary care settings. Int Rev Psychiatry. 2015;27(6):525–539. doi: 10.3109/09540261.2015.1085838. [DOI] [PubMed] [Google Scholar]
- 82.Mehrotra A, Huskamp HA, Souza J, Uscher-Pines L, Rose S, Landon BE, Jena AB, Busch AB. Rapid growth in mental health telemedicine use among rural medicare beneficiaries, wide variation across states. Health Aff (Millwood) 2017;36(5):909–917. doi: 10.1377/hlthaff.2016.1461. [DOI] [PubMed] [Google Scholar]
- 83.Fortney JC, Pyne JM, Edlund MJ, Williams DK, Robinson DE, Mittal D, et al. A randomized trial of telemedicine-based collaborative care for depression. J Gen Intern Med. 2007;22(8):1086–93. 10.1007/s11606-007-0201-9. [DOI] [PMC free article] [PubMed]
- 84.Fortney JC, Pyne JM, Mouden SB, Mittal D, Hudson TJ, Schroeder GW, et al. Practice-based versus telemedicine-based collaborative care for depression in rural federally qualified health centers: a pragmatic randomized comparative effectiveness trial. Am J Psychiatry. 2013;170(4):414–25. 10.1176/appi.ajp.2012.12050696. [DOI] [PMC free article] [PubMed]
- 85.• Grubbs KM, Fortney JC, Pyne J, Mittal D, Ray J, Hudson TJ. A comparison of collaborative care outcomes in two health care systems: VA clinics and federally qualified health centers. Psychiatr Serv. 2018;69(4):431–7. 10.1176/appi.ps.201700067 This study reports differential depression outcomes among civilian and veteran populations following engagement in a PCMH-based collaborative care program. [DOI] [PMC free article] [PubMed]
- 86.• Wong H, Moore K, Angstman KB, Garrison GM. Impact of rural address and distance from clinic on depression outcomes within a primary care medical home practice. BMC Fam Pract. 2019;20(1):123–31. 10.1186/s12875-019-1015-7 This observational study reports differential depression outcomes among rural and urban populations enrolled in a PCMH-based collaborative care program. [DOI] [PMC free article] [PubMed]
- 87.Hilty DM, Rabinowitz T, McCarron RM, Katzelnick DJ, Chang T, Bauer AM, et al. An update on telepsychiatry and how it can leverage collaborative, stepped, and integrated services to primary care. Psychosomatics. 2018;59(3):227–250. doi: 10.1016/j.psym.2017.12.005. [DOI] [PubMed] [Google Scholar]
- 88.• Hilty DM, Sunderji N, Suo S, Chan S, McCarron RM. Telepsychiatry and other technologies for integrated care: evidence base, best practice models and competencies. Int Rev Psychiatry. 2018;30(6):292–309. 10.1080/09540261.2019.1571483 This review discusses the use of telepsychiatry within primary care, focusing how technology can be used at each level of services. [DOI] [PubMed]
- 89.Myers CR. Using telehealth to remediate rural mental health and healthcare disparities. Issues Ment Health Nurs. 2019;40(3):233–239. doi: 10.1080/01612840.2018.1499157. [DOI] [PubMed] [Google Scholar]
- 90.Gaynes BN, Lux L, Gartlehner G, Asher G, Forman-Hoffman V, Green J, Boland E, Weber RP, Randolph C, Bann C, Coker-Schwimmer E, Viswanathan M, Lohr KN. Defining treatment-resistant depression. Depress Anxiety. 2020;37(2):134–145. doi: 10.1002/da.22968. [DOI] [PubMed] [Google Scholar]
- 91.Davies P, Ijaz S, Williams CJ, Kessler D, Lewis G, Wiles N. Pharmacological interventions for treatment-resistant depression in adults. Cochrane Database Syst Rev. 2019;12:CD010557. doi: 10.1002/14651858.CD010557.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Ijaz S, Davies P, Williams CJ, Kessler D, Lewis G, Wiles N. Psychological therapies for treatment-resistant depression in adults. Cochrane Database Syst Rev. 2018;5:CD010558. doi: 10.1002/14651858.CD010558.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Kessler DS, MacNeill SJ, Tallon D, Lewis G, Peters TJ, Hollingworth W, et al. Mirtazapine added to SSRIs or SNRIs for treatment resistant depression in primary care: phase III randomised placebo controlled trial (MIR) BMJ. 2018;363:k4218. doi: 10.1136/bmj.k4218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Wiles N, Thomas L, Abel A, Barnes M, Carroll F, Ridgway N, Sherlock S, Turner N, Button K, Odondi L’, Metcalfe C, Owen-Smith A, Campbell J, Garland A, Hollinghurst S, Jerrom B, Kessler D, Kuyken W, Morrison J, Turner K, Williams C, Peters T, Lewis G. Clinical effectiveness and cost-effectiveness of cognitive behavioural therapy as an adjunct to pharmacotherapy for treatment-resistant depression in primary care: the CoBalT randomised controlled trial. Health Technol Assess. 2014;18(31):1–167. doi: 10.3310/hta18310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Wiles NJ, Thomas L, Turner N, Garfield K, Kounali D, Campbell J, et al. Long-term effectiveness and cost-effectiveness of cognitive behavioural therapy as an adjunct to pharmacotherapy for treatment-resistant depression in primary care: follow-up of the CoBalT randomised controlled trial. Lancet Psychiat. 2016;3(2):137–44. 10.1016/s2215-0366(15)00495-2. [DOI] [PubMed]
- 96.Preston TC, Shelton RC. Treatment resistant depression: strategies for primary care. Curr Psychiatry Rep. 2013;15(7):370–376. 10.1007/s11920-013-0370-7. [DOI] [PubMed]
- 97.Jackson GL, Williams JW. Does PCMH “work”?—the need to use implementation science to make sense of conflicting results. JAMA Intern Med. 2015;175(8):1369–1370. doi: 10.1001/jamainternmed.2015.2067. [DOI] [PubMed] [Google Scholar]
- 98.Sinaiko AD, Landrum MB, Meyers DJ, Alidina S, Maeng DD, Friedberg MW, Kern LM, Edwards AM, Flieger SP, Houck PR, Peele P, Reid RJ, McGraves-Lloyd K, Finison K, Rosenthal MB. Synthesis of research on patient-centered medical homes brings systematic differences into relief. Health Aff (Millwood). 2017;36(3):500–508. doi: 10.1377/hlthaff.2016.1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Jones AL, Mor MK, Haas GL, Gordon AJ, Cashy JP, Schaefer JH, Jr, et al. The role of primary care experiences in obtaining treatment for depression. J Gen Intern Med. 2018;33(8):1366–1373. doi: 10.1007/s11606-018-4522-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Leung LB, Yoon J, Escarce JJ, Post EP, Wells KB, Sugar CA, Yano EM, Rubenstein LV. Primary care-mental health integration in the VA: shifting mental health services for common mental illnesses to primary care. Psychiatr Serv. 2018;69(4):403–409. doi: 10.1176/appi.ps.201700190. [DOI] [PubMed] [Google Scholar]
- 101.Hearld KR, Hearld LR, Landry AY, Budhwani H. Evidence that patient-centered medical homes are effective in reducing emergency department admissions for patients with depression. Health Serv Manag Res. 2019;32(1):26–35. doi: 10.1177/0951484818794340. [DOI] [PubMed] [Google Scholar]