Abstract
Negative pressure pulmonary edema (NPPE) caused by airway obstruction was often life-threatening. Major cause of NPPE in adult patients was reported as post-operative laryngospasm. Therefore, NPPE was recognized widely among surgeons and anesthesiologist, but physicians also could face NPPE case in several clinical situation. NPPE in this case was caused by sleep apnea syndrome (SAS) as relatively rare cause. A 65-year-old female presented to emergency department due to disturbance of consciousness during sleep. This patient had desaturation requiring oxygen administration. Computed tomography showed pulmonary edema in bilateral lung fields. Comprehensive examination had no evident organic airway obstruction, and echocardiography showed normal cardiac function. This patient had been diagnosed with severe SAS with the apnea hypopnea index of 32 times/h. Therefore, we thought that the NPPE could be caused by severe SAS in this case. Continuous positive airway pressure therapy could improve this patient's symptoms promptly, and this patient could discharge without a complication. We should consider SAS as a cause of NPPE when examining NPPE patients especially with onset during sleep.
Keywords: Continuous positive airway pressure, Negative pressure pulmonary edema, Sleep apnea syndrome
1. Introduction
Negative pressure pulmonary edema (NPPE) was generally caused by upper airway problems. A mechanism of NPPE was explained by increased intrathoracic negative pressure following inspiration against obstructed upper airway. Previous literatures showed that causes of NPPE were mainly post-operative laryngospasm associated with airway obstruction in adult patients [1]. Meanwhile, the relation between sleep apnea syndrome (SAS) and NPPE was not widely known even in physician. Furthermore, NPPE was reported to be a fatal disease due to its severity with airway troubles and complications [2,3]. Although the treatment for NPPE might be supportive care mainly, we should understand which diseases could cause this clinical situation not to miss opportunity to treat NPPE patients. This case reported that a relatively rare case of NPPE was caused by severe SAS and adequate treatment improved the patient's prognosis.
2. Case report
A 65-year-old female without obesity presented to our emergency department due to clonic convulsion-like movement of bilateral upper extremities after growling during sleep and subsequent disturbance of consciousness. This patient had two previous episodes of disturbance of consciousness and desaturation without convulsion-like movement during sleep. This patient's husband noticed that she sometimes had snored strongly and stopped breathing for a while after snoring during sleep. This patient had been diagnosed as severe obstructive SAS after previous hospitalization. The severity of SAS was followings: The apnea hypopnea index (AHI) was 32 times/h, including obstructive apnea index 18 times/h and central apnea index 13 times/h. The minimum of saturation of percutaneous oxygen was 85% and the maximum duration of apnea/hypopnea was 79.5 seconds. Therefore, this patient had been recommended to use a nasal CPAP but had refused. This patient's blood pressure, heart rate and body temperature at admission were 179/87 mmHg, 77/min and 36.3 °C, respectively. This patient's saturation of percutaneous was 80% (room air) at first. Her consciousness level of Glasgow coma scale was E1V1M5. This patient's body mass index was 23.0 kg/m2. Laboratory analysis showed no evidence of abnormal results leading to disturbance of consciousness except for hypoxemia on arterial blood gas analysis with O2 2 L/min (partial pressure of O2 68.5 torr, partial pressure of CO2 45.9 torr). This patient's consciousness improved gradually with oxygen administration. However, desaturation (saturation of percutaneous oxygen 90–93% with O2 2 L/min) requiring oxygen administration continued after recovery of her consciousness. Computed tomography showed no evidence of intracranial abnormality and other cause leading to disturbance of consciousness. Electroencephalography showed no abnormal electroencephalogram at admission. Meanwhile, computed tomography showed a pattern of pulmonary edema indicating NPPE in bilateral whole lung fields (Fig. 1 and Fig. 2). Echocardiography showed normal cardiac function and no structural abnormality. Complete physical examination revealed no evident mechanical airway obstruction like tumor, laryngeal infection and foreign-body aspiration. As a result, this patient was diagnosed with NPPE related with severe obstructive SAS and started nasal CPAP therapy (positive end-expiratory pressure 4 cmH2O). This patient's symptoms were promptly improved with CPAP therapy by the next morning, and she did not recur with it after discharge for two months. Bilateral lung edema on chest X ray was improved with the treatment (Fig. 3). However, the similar episode occurred on the nasal CPAP therapy because of the device failure, especially dissonance of nasal mask. Although This patient was operated with an insertable cardiac monitor and further took electroencephalography and brain magnetic resonance imaging again to exclude the other cause, these examinations could not reveal the other cause of NPPE. Therefore, the CPAP with full mask was introduced, and the follow up of full polysomnography was performed on CPAP therapy. The AHI (6.7 times/h) was improved and the minimum of saturation of percutaneous oxygen level increased to 89%, and this patient's symptom could not recur over the half of year.
Fig. 1.
Axial image of bilateral lung field on computed tomography. Computed tomography showed that bilateral pulmonary edema in whole lung fields.
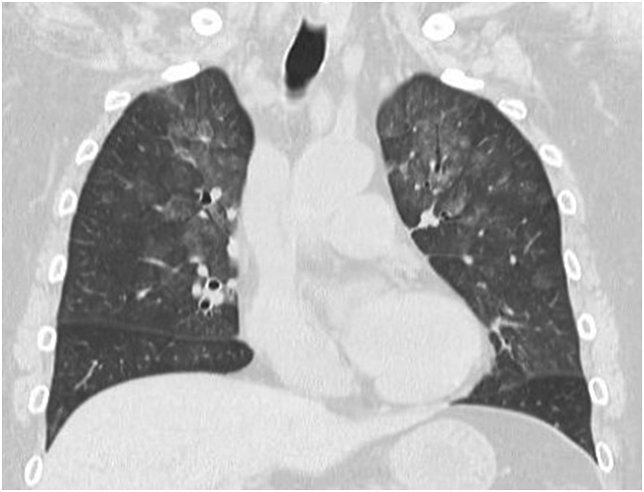
Fig. 2.
Coronal image of bilateral lung field on computed tomography. Computed tomography showed that bilateral pulmonary edema in whole lung fields.
Fig. 3.
Chest X ray image at admission and after discharge. Chest X ray on supine position image took oat admission was left side (A). Chest X ray on postero-anterior position image took after discharge was right side (B). Chest X ray image at admission showed the bilateral upper lobe edema, and the one showed its improvement after discharge.
3. Discussion
NPPE is one of notable diseases caused by serious airway problems. Generally, a mechanism of NPPE was explained that inspiration force against upper airway obstruction generates great negative intrathoracic pressure leading to pulmonary edema [1,4]. Previous literatures reported that laryngospasm associated with intubation and general anesthesia was the most common cause of upper airway obstruction leading to NPPE in adult patients [1]. NPPE caused by airway obstruction often could be life-threatening disease [2,5]. If physician do not recognize that SAS could cause NPPE during sleep, a patient with SAS might miss an opportunity to take an adequate treatment. This case was a relatively rare NPPE patient caused by severe obstructive SAS and showed that adequate CPAP therapy improved this patient's prognosis.
In adult patients with NPPE, onset of this disease under general anesthesia was considered as common situation [1,4]. Meanwhile, it was not well-known that the SAS could cause NPPE. The onset of NPPE after efforts at inspiration against an obstructed airway is very rapid, therefore, even temporary airway obstruction in patients with obstructive SAS could generate great intrathoracic negative pressure causing NPPE [6]. Although well-known symptoms of SAS are daytime sleepiness and decrease of cognitive performance associated with a serious accident [7], we should pay much attention to the fact that SAS could cause NPPE. Additionally, the previous study reported that SAS might make seizure occur more likely., and the seizure could be related with onset of NPPE [8,9]. Therefore, the presence of SAS itself could be related with onset of NPPE.
Treatment of NPPE was mainly supportive care including relieving the upper airway obstruction by endotracheal intubation, cricothyroidotomy, or introduction of lung-protective positive pressure ventilation like CPAP [4]. Among the treatment options, CPAP might resolute the pulmonary edema of NPPE caused by SAS rapidly because alveolar fluid clearance in patients with NPPE is maintained generally [4]. In contrast, patients with NPPE caused by infection like epiglottitis need to obtain endotracheal intubation, cricothyroidotomy or tracheotomy [4]. The mechanical obstruction which could not be released by positive pressure, such as foreign body and postoperative tracheal stenosis, also must be introduced with invasive airway protection including endotracheal intubation, because the secure airway opening was the first step of treatment [10]. Therefore, if airway obstruction causing NPPE is not recognized promptly, prognosis of patients might be miserable and fatal [11]. Fortunately, this patient treated with CPAP improved rapidly and did not recur after treatment and the device adjustment. Early recognition of existence of airway trouble might be a key to improve a condition of a patient with NPPE.
4. Conclusions
SAS was a rare cause of NPPE developing during sleep. Therefore, when we would examine a NPPE patient with onset during sleep, we should consider SAS as a cause of NPPE. Early recognition and prompt management might be a key to improve clinical outcomes of patients with NPPE.
Consent
Written informed consent was obtained from patient for the publication of this case report and any accompanying images.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Miller H.G. Negative pressure pulmonary edema. Can. Oper. Room Nurs. J. 1995;13(3):28–30. [PubMed] [Google Scholar]
- 2.Chen J., Wang S., Ma H., Wang W., Fu D., Huang W., Deng J., Tang H., He Y., Zheng Y. [Clinical analysis of 4 children with negative pressure pulmonary edema] Z. Chin. J. Pediatr. 2014;52(2):122–127. [PubMed] [Google Scholar]
- 3.Contou D., Voiriot G., Djibre M., Labbe V., Fartoukh M., Parrot A. Clinical features of patients with diffuse alveolar hemorrhage due to negative-pressure pulmonary edema. Lung. 2017;195(4):477–487. doi: 10.1007/s00408-017-0011-8. [DOI] [PubMed] [Google Scholar]
- 4.Bhattacharya M., Kallet R.H., Ware L.B., Matthay M.A. Negative-pressure pulmonary edema. Chest. 2016;150(4):927–933. doi: 10.1016/j.chest.2016.03.043. [DOI] [PubMed] [Google Scholar]
- 5.Venkatesh R., Gautam P., Dutta P., Bala P. Negative pressure pulmonary edema--a life-threatening condition in an eye care setting: a case report. J. Med. Case Rep. 2016;10:39. doi: 10.1186/s13256-016-0820-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chaudhary B.A., Nadimi M., Chaudhary T.K., Speir W.A. Pulmonary edema due to obstructive sleep apnea. South. Med. J. 1984;77(4):499–501. doi: 10.1097/00007611-198404000-00022. [DOI] [PubMed] [Google Scholar]
- 7.Maspero C., Giannini L., Galbiati G., Rosso G., Farronato G. Obstructive sleep apnea syndrome: a literature review. Minerva Stomatol. 2015;64(2):97–109. [PubMed] [Google Scholar]
- 8.Malow B.A., Levy K., Maturen K., Bowes R. Obstructive sleep apnea is common in medically refractory epilepsy patients. Neurology. 2000;55(7):1002–1007. doi: 10.1212/wnl.55.7.1002. [DOI] [PubMed] [Google Scholar]
- 9.Contou D., Voiriot G., Djibré M., Labbé V., Fartoukh M., Parrot A. Clinical features of patients with diffuse alveolar hemorrhage due to negative-pressure pulmonary edema. Lung. 2017;195(4):477–487. doi: 10.1007/s00408-017-0011-8. [DOI] [PubMed] [Google Scholar]
- 10.Liu R., Wang J., Zhao G., Su Z. Negative pressure pulmonary edema after general anesthesia: a case report and literature review. Medicine. 2019;98(17) doi: 10.1097/MD.0000000000015389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dempsey J.A., Veasey S.C., Morgan B.J., O'Donnell C.P. Pathophysiology of sleep apnea. Physiol. Rev. 2010;90(1):47–112. doi: 10.1152/physrev.00043.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]