Abstract
Shared decision making (SDM) is a management paradigm that empowers patients as partners in their own care in a bidirectional exchange of information and values, and optimize the decision-making process. During the current coronavirus disease 2019 pandemic, there is a greater need to encourage participation in the SDM process. The pandemic has created both challenges and opportunities for delivering care, as system adaptations influence the physician-patient relationship. Although social distancing and health service reallocation can interfere with preference for an in-person visit, these measures also provide an avenue to study and implement virtual SDM processes. Communicating risk at a time of heightened uncertainty may pose a barrier to SDM engagement but provides the opportunity to foster a patient-centered approach within a more personalized context. Social media influence during coronavirus disease 2019 has resulted in an “infodemic” but highlights the importance of patient engagement. The pandemic has changed how we deliver care but allows us to re-evaluate common practices and enhance effectiveness of our management strategies. Navigating the uncertainty of subsequent pandemic waves creates confusion about how to safely reinitiate clinical service. This will require ongoing SDM with our patients and among colleagues through current—and future—challenges. Coronavirus disease 2019 has created many difficulties but has forced us to reexamine how to provide more patient-centered and high-quality care.
Key words: COVID-19, SARS-CoV-2, Shared decision making, Decisional conflict, Decision aid
Abbreviations used: COVID-19, Coronavirus disease 2019; SDM, Shared decision making; VSDM, Virtual shared decision making
Introduction
Shared decision making (SDM) is an approach whereby physicians and patients share in the decision-making process in a 2-way (or sometimes 3- or 4-way) conversation incorporating best available evidence and patient preference.1 SDM integrates all available evidence-based screening, treatment, or management options and provides the opportunity to explore potential benefits, trade-offs, and risks of each approach before a decision is made, promoting patient engagement in decisions regarding their health care.1 SDM has been touted as a national priority for comparative effectiveness research by the Institute of Medicine due to the ability to emphasize “patient choice for preference-sensitive care”2 and has been adopted as a research priority by Patient-Centered Outcomes Research Institute.3 The Salzburg statement on SDM notes an ethical imperative on the part of clinicians to “stimulate a two-way flow of information” and to “tailor information to individual patient needs and allow them sufficient time to consider their options.”4 The use of SDM speaks to the larger context that evidence doesn't make decisions, people do.5
SDM has been incorporated into national policy in multiple countries.1 , 6, 7, 8 In the United States, 5 states have incorporated SDM laws, with some linking an SDM requirement to the formation of any Accountable Care Organizations. One such example is the Washington State law, which provides a higher level of protection in informed consent liability claims when SDM was used in keeping with state requirements.9 SDM has been shown to improve decision quality,10 decision-making processes,10 patient adherence,11 risk perception,1 , 11 and patient outcomes,12 while lowering health care costs12 and health care resource utilization12 and enhancing patient autonomy with respect to decision making.12 , 13 Within allergy and immunology, studies regarding the use of SDM have been predominantly within the field of asthma, which showed improved medication adherence,14 asthma clinical outcomes,14, 15, 16 quality of life,17 and engagement in health care decisions.18
Decision aids assist in the SDM process as “interventions that support patients by making their decisions explicit, providing information about options and associated benefits/harms, and helping clarify congruence between decisions and personal values.”19 A 2017 systematic review noted that the use of decision aids resulted in patients feeling more knowledgeable and better informed compared with usual care.19 Decision aids have been created for allergic rhinitis, asthma, venom allergy, and peanut allergy treatment (see Table E1 in this article's Online Repository at www.jaci-inpractice.org).13 , 20 , 21 The International Patient Decision-Aid Standards Collaboration has developed formalized guidance for standardized development and acceptability testing of decision aids, helping ensure SDM tools fully engage key stakeholders involved in the decision, though not all the aforementioned allergy decision-aids are compliant with International Patient Decision-Aid Standards.22 , 23 Table I addresses some common SDM myths.
Table I.
Common misperceptions regarding SDM
| Misperception | Comment |
|---|---|
| Face-to-face SDM is always the goal | Where SDM occurs is likely far less important than whether the process itself occurs. Although this has traditionally been achieved with in-office, in-person discussion, use of telehealth tools can extend the definition of the “office” and “in-person.” At home with the family may be superior for some, because it may allow for more individuals affected by the decision beyond the patient to participate |
| SDM takes too much time | Incorporating SDM should be viewed as an extension of the normal planning for any treatment decision, where patient input should be sought. Some discussions and decisions may be more involved and may require additional visits or conversations. Involving staff and validated SDM aids may be helpful to facilitate this process and can be distributed to the patient before or after a visit, which could save face-to-face time if this is a concern |
| Most patients prefer not to participate in medical decision making | There is no evidence that this is factual. The degree to which a patient wants to participate in this process is variable, and may depend on the issue at hand, the treatment decision, the patient, and the perception the clinician is receptive to patient input |
| Few health care decisions are appropriate for SDM | All decisions should have patient input. Where there is a very clear and strongly recommended treatment (eg, treating asthma vs leaving it untreated), there may be less efficacy of SDM tools vs situations in which there is less clarity in which option to choose (eg, which asthma treatment should be chosen) |
| SDM conflicts with guidelines and quality measures | SDM has been shown to only enhance not deter clinical outcomes, improve engagement, and would involve choices that are derived from guidelines and quality measures as part of the considerations in the treatment decision |
We face unprecedented times in health care with the novel coronavirus pandemic coronavirus disease 2019 (COVID-19), caused by the pathogen severe acute respiratory syndrome coronavirus 2, which has affected more than 11.5 million people internationally with more than 539,000 deaths as of July 6, 2020.24 The highest caseload is in the United States, with more than 2.9 million cases of COVID-19, which threatens to exceed health care capacity in certain areas over the next year.24 , 25 COVID-19 has forced a reconceptualization of how to provide quality health care while enforcing public health measures necessary for pandemic containment and optimal allocation of health care resources.26 With tough decisions, there is an even greater imperative to engage patients regarding care options, creating a unique role for SDM.
This unparalleled time presents some barriers to traditional SDM engagement given reduced face-to-face contact, but also an opportunity to evolve incorporation of SDM into our practices both during and in the postpandemic landscape. Herein, this article will discuss the challenges that COVID-19 poses for SDM, in terms of health service reallocation, communicating uncertainty, social media influence, re-evaluation of many of the current assumptions that guide the practice of allergy/immunology, and navigating the uncertainty of future pandemic waves.
Challenges and Opportunities for SDM During COVID-19
Physical distancing and health service reallocation
Challenges
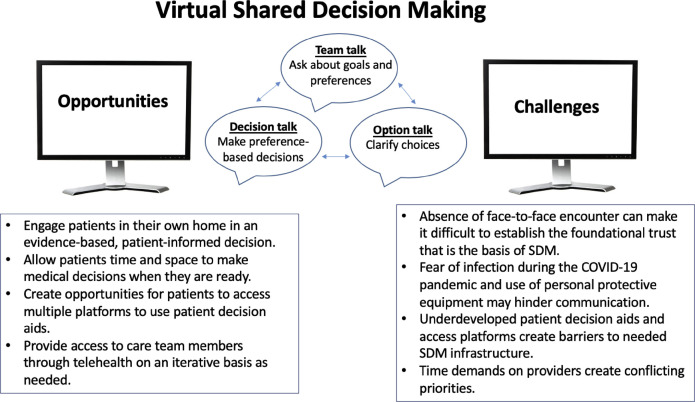
Public health requirements including physical distancing can interfere with patient preference among those valuing a face-to-face visit over a virtual visit (Figure 1 ).26 Although the encounter may be identical either in-person or virtually, many patients and clinicians are unfamiliar with the advantages of telehealth, or the risks of in-person care in a pandemic. This brings to light potential decisional conflict regarding what is appropriate to offer, and to whom, and introduces variation in what the patient and clinician may consider “essential care,” or how to define this. Health care reallocation and physical distancing measures can also interfere with SDM regarding certain choices of service that can be offered, such as recommendations to not initiate allergen immunotherapy in clinic during pandemic peaks.26 The recent North American contingency guidance for allergy care during COVID-19 notes that pandemic settings may limit ambulatory care provision and access to resources normally more available in nonemergent settings, which may impact some decisions.26
Figure 1.
VSDM. Images created by creative commons license. Three-talk model of shared decision adapted from Blaiss et al.13
Opportunities
The need for social distancing may lead to creative workarounds, such as “drive through immunotherapy” (Travis Miller, MD, email communication, 2020). Anecdotes have emerged of practices that, based on a mutually shared decision to continue immunotherapy if considered “essential” by both parties, patients remain in their car to receive immunotherapy, are observed in the parking lot for 30 minutes postinjection, and supervised by a staff member wearing personal protective equipment who minimizes patient interaction. Although this method is unpublished, it demonstrates how care can evolve in a pandemic in some practices, though data are needed to ensure safety is not sacrificed. Evidence also suggests that for highly health-literate patients, home allergen immunotherapy can be a cost-effective alternative to clinic immunotherapy during the pandemic in some circumstances.27
Enforced social distancing also provides a unique opportunity to study and implement “virtual” shared decision making (VSDM). It is unknown how significantly virtual visits impact the physician-patient relationship and the ability to engage in the SDM process, nor their utility in those with low health literacy or those who are less technologically adept. VSDM has not been studied in allergy/immunology, but other specialties have demonstrated improvement in clinical outcomes with a VSDM telemedicine approach.28 A subanalysis of a stratified randomized controlled trial (N = 60,185) showed that a telephonic SDM approach (incorporating telephonic coaching with decision aids that could be mailed, emailed, or delivered online) resulted in lower medical cost, hospital admission rate, and fewer preference-sensitive interventions compared with the usual care group in patients with various chronic health conditions such as diabetes, asthma, and chronic obstructive pulmonary disease.12 This suggested “a remote model, combining telephonic coaching with decision aids, should be considered as either an add-on to provider-based interventions or a stand-alone option.” Although SDM models often incorporate a team-based approach,29, 30, 31, 32 which is more difficult to implement and coordinate during a pandemic, telephonic SDM provides the potential to maintain a team-based SDM despite such circumstances. The pandemic may foster infrastructure changes that enhance care opportunities, care team collaboration, and tools to reach underserved populations.33 Potential benefits of VSDM may include increased number of services/specialist access, reduced access disparities, reduced travel, lower costs, and quality improvements from more efficient information transfer.34
Prepandemic Health Insurance Portability and Accountability Act constraints were lifted by the Centers for Medicare & Medicaid Services in March 2020, expanding clinician access to telehealth/VSDM, and creating an opportunity to advance care delivery. Such regulatory changes may enhance patient care and patient empowerment through more personalized, tailored, interactive encounters.35 , 36 The task is to understand how to leverage such opportunities and measure outcomes to maintain access to new patient-preference–centered care tools moving forward. Practical issues such as billing, time, and other infrastructure issues need to be addressed for the long-term success of VSDM, and patient acceptability of this distinct SDM method must be understood.
Communicating uncertainty
Challenges
The COVID-19 pandemic brings much uncertainty. Currently, no person—patient or clinician—has all the answers to how to navigate COVID-19, or the true impact of allergic comorbidity on risk/clinical course of disease. It is important to note that communicating uncertainty (such as discussing a medical decision where there is no “best” choice based on outcome evidence) may decrease patient satisfaction.37 As noted, “Implicitly or explicitly, application of evidence-based medicine to individual patients always requires a model”38 and currently no model exists. A systematic review on the barriers and facilitators of pediatric SDM noted that for adopters, in particular parents, lack of research for diagnostic and/or therapeutic options is a barrier to engaging in SDM, and that higher stake decisions reduced willingness to participate in SDM.39 Although SDM in the context of a pandemic has not been studied, higher degrees of uncertainty and perceived higher stakes with particular decisions may be a distinct barrier to the SDM process until more accurate data are available regarding the relative risks/benefits of options within the broader context of allergy/immunology services and COVID-19.
Opportunities
One patient-centered step that could be taken, which incorporates medical uncertainty, is to include goal setting and dispositional hope as a component of any physician-patient SDM approach, such as “what do you most hope to get out of treating your asthma?”40
Social media influence
Challenges
During public health crises, risk perception is elevated, resulting in the public relying even more heavily on the influence of social media to inform their understanding of health information and level of risk perception.41 , 42 More than 50% of all patients search online information sources before allergy appointments.43 However, if online information is incorrect, “this can not only damage the patient-provider relationship but also lead patients to seek non-evidence-based promises of miracle cures, costly treatments, or unnecessary testing.”41 This is even more likely to be the case during a pandemic, where “every new online platform is also a conduit for spreading criticism or misinformation.”44 , 45 The director general of the World Health Organization noted social media influence during COVID-19 to be a “coronavirus infodemic.”46 This “infodemic,” or mass amount of information, makes it even more difficult to address medical solutions and contributes to misinformation, which can “create confusion and distrust among people.”46 In allergy, the challenges of “de-educating” a flawed belief, and correctly “reeducating” an evidenced-based one has not been researched, nor has how to integrate social media influence into a broader SDM context.
Opportunities
This highlights an added importance of engaging patients in discussions. Studies into the implementation of SDM have noted positive patient-physician relationships and respectful communication to be facilitators of SDM and might mitigate previous social media impact on medical decision making.39 , 47 Incorporating advocacy groups and other key stakeholders in developing SDM can provide broad engagement and balance it with evidence-based discussion and framing.48 Although risks of social media cannot be underestimated, VSDM may be a means to provide ways for people to maintain their independence while also interacting with health care providers and rebuilding or preserving social networks.
Reevaluation of our current assumptions that guide the practice of allergy/immunology
Challenges
The pandemic has unequivocally forced change in how we deliver allergy/immunology care as a by-product of limited resources and heightened infection risk. However, there is a tendency for “paralysis by analysis,” in necessitating evidence from randomized controlled trials that are unlikely to be funded/performed. There are many decisions that are made—such as intradermal testing for delayed amoxicillin exanthems, preemptive screening before food introduction, and administering maintenance immunotherapy in the office in select circumstances—that have been shown to be largely unnecessary from a safety standpoint, not cost-effective, and even potentially harmful in some situations.49, 50, 51, 52, 53
Opportunities
This unprecedented time allows us to reopen the conversation that “evidence is derived from groups, whereas medicine is applied to individuals.”38 Every specialty has practices that require an evolutionary nudge to enhance effectiveness. Sometimes, there is room for the weight of experience and common sense to drive decisions on how to reevaluate the practice of allergy. During the pandemic, we have seen this relative to home omalizumab and rethinking default Emergency Medical Service activation postanaphylaxis. A greater appreciation for the role of contextual care has evolved within conditional recommendations presented in practice guidelines.54 However, to be effective SDM must be clear, and proactive when presenting relevant options.55
Some conventions that made sense before the pandemic have been revised in a pandemic setting. The larger question is which short-term changes will be adopted and continue to influence care after pandemic recovery. The pandemic leads to a much-needed discussion about essential care now, and in the future, which is precisely where SDM and incorporation of decision-support tools for preference-sensitive care options can play a tremendous role. This allows preservation of more established conventions, if the patient so chooses, but also for care options to evolve in those wishing something different. For decisions specifically within the context of providing care in the pandemic, decision aids could be created that incorporate the element of risk—such as the recently released COVID-19 palliative decision-making tool.56 Decision aids have validation steps, and there is little likelihood of studying and validating a decision aid during the first wave of this pandemic. However, the lessons learned could be applied toward future decision aids that incorporate the changes resulting from the pandemic moving forward, so that any future unforeseen issues, such as those of the pandemic, at least have a basic framework available for clarifying values to make a decision.
Navigating the uncertainty of subsequent pandemic waves
Challenges
Although the previous sections have dealt with longer-term issues of how to use the pandemic to engender more SDM in allergy practice, the short to intermediate decisional needs cannot be overlooked. In response to the initial wave of the pandemic in March/April 2020, most states issued stay at home orders and halted nonessential ambulatory care services. As regional first waves of the pandemic subside, many ambulatory care services deemed elective or less essential at the start of the pandemic may begin to resume.57 It is highly unlikely that treatment, vaccination, or cessation of severe acute respiratory syndrome coronavirus 2 transmission will occur in the coming months to allow normal medical practices to resume without needing personal protective equipment, and some measure of physical distancing. Adding to this uncertainty is whether second/third pandemic waves will cause resumption of strict physical distancing, stay at home orders, and repeated start/stop cycles of many aspects of society, including ambulatory care. Already, in response to a subjective determination of what constitutes “essential care,” some practices have forged ahead, whereas others have scaled back. Patient demand may be dependent on regional density of infection, and personal beliefs regarding the state of allergic/immunologic conditions versus their risk perception of acquiring COVID-19 through routine care.
Many of us will face a decision shortly (if not already) how to reinitiate service, and how to prioritize certain patients/diagnoses over others as capacity to provide more routine care emerges—a recently published document in this journal discusses a phased approach in doing so, which aims to help the clinician consider different choices and trade-offs, including the role of SDM.57 SDM needs to occur on 2 levels—within clinicians and then between the clinician and the patient. At the clinician level, decisions about the ability to protect staff/patients and sanitize rooms while maintaining effective spacing, as well decisions reflecting office/practice finance are crucial. Hard decisions will have to be made, on the basis of imperfect information, and some degree of trade-off that we may rather avoid in any other context. A parallel to this untenable decision-making situation can be drawn from the movie Star Trek 2: Wrath of Kahn, and the Kobyashi Maru training exercise, where cadets in leadership must choose between abandoning a disabled ship that has lost communication capacity in Klingon territory (where they will be destroyed) versus entering into the territory, sparking a war, and risking their own lives as well as the lives of the other ship in a rescue attempt.58 The point of the exercise is not to “win,” but to understand decisional trade-offs that may have to occur. Reflecting on the cultural reality of situations dominated by some degree of loss is informative and reminds us that we are neither alone nor at the end of this journey. Many may have faced, or will face, such untenable decisions to close their office, furlough/fire staff, curtail salary, or to remain open at a significant loss of revenue, and clinicians need to understand their own decisional needs in this context.
Opportunities
SDM with our patients in this context, where we contemplate starting to offer more services, has to be handled carefully but provides the opportunity to reexamine what is considered essential in-person care.57 Infection risk may be low enough to cross a threshold in favor of resumption of allergy/immunology care, though again this is a discussion to have with patients, possibly through telemedicine visits before an in-person appointment. For example, face-to-face visits for stable asthma, in someone due for a yearly evaluation, may have a different threshold than someone with asthma that has been less adequately controlled in the last few months. Making these decisions will require knowledge of community transmission risk and emergency services capacity. The opportunity to reexamine how to proceed with routine evaluation for allergic rhinitis and initiating immunotherapy exists, which may be viewed as less acute needs by some, but highly important to others. The clinician must be aware of the risks/benefits of the condition, deferment of traditional routes and time intervals of evaluations with respect to the condition, the risk of contracting COVID-19, and their own countertransference issues/financial conflicts as well.
Moving forward
Table II outlines a needs assessment for SDM in the current pandemic that includes defining an SDM process (either in-person or virtually), developing a certification process for decision aids and providing incentives for their evaluation and maintenance, promoting competency in SDM, developing pandemic-specific SDM measures, fostering a culture of SDM, and using SDM to help with documentation of quality improvement.
Table II.
Pandemic SDM needs assessment
| Clearly define the SDM process through either in-person or virtual encounters |
| Develop a certification process for decision aids and provide incentives for their evaluation and maintenance |
| Promote competency in SDM, and a skills assessment so that clinicians can understand their current competency level and needs assessment in SDM |
| Develop pandemic-specific SDM measures |
| Foster a culture of SDM |
| Use SDM to help with documentation of quality improvement |
It could be argued that SDM is more essential than ever to meet the individual needs of our patients during this era of change. In the day-to-day allergy practice, incorporating SDM when evaluating in-person versus virtual visits, and essential versus nonessential care, is of paramount importance. Decision aids are necessary for many aspects of ongoing allergy care. SDM should be incorporated into allergy policy and guidelines, and considered an inherent aspect of medical education.
In general, SDM has focused on short-term outcomes such as patient satisfaction, short-term clinical outcomes, or decisional conflict. However, there has been a call to conceptualized SDM within a broader interactional/adaptable and organizational framework.59 It has been suggested that SDM at an interactional level could lead to “the development of a culture where deliberation and collaboration are regarded as guiding principles, where patients are coached to assess the value of interventions, to trade-off benefits versus harms and assess their burdens–in short, to new social norms in the clinical workplace.”59 Within an organizational framework the incorporation of SDM principles has the potential to modify health care and service allocation and reduce costs.59
The lessons learned during COVID-19, and the increasing need for consideration of patient preference and values, may help to further the discussion about how to incorporate SDM more broadly on an organizational and interactional level. The Salzburg report has called on policymakers to adopt policies that encourage SDM and support the development of skills and tools for SDM.4 Careful and concerted efforts are needed to incorporate additional inputs and concerns that accompany virtual decisions, such as ethical issues expanded beyond the frequently considered constellation of privacy, security, confidentiality, and liability.
COVID-19 has forced us to tackle the larger issue of “the tension between needing to improve care and knowing how to do it.”60 During this time, it is even more important to remember that “to make decisions–with people–we must begin with the context and only after this go with the symptoms and signs.”5 Although broadly the context of a global pandemic can change this perspective, requiring specific guidance on our part, it provides a unique opportunity to reexamine how we provide care, how we counsel the benefits and risks of care, and how we engage patients as partners in their own medical decisions. Despite its many challenges, it is clear that this unprecedented period can provide opportunity to improve the care of our patients moving forward.
Footnotes
Conflicts of interest: E. M. Abrams is a collaborator with the Institute for Health Metrics and Evaluation, is on the National Advisory Board for Food Allergy Canada, and is on the National Food Allergy Action Plan Action Steering Team for Food Allergy Canada. M. Shaker is a member of the Joint Taskforce on Allergy Practice Parameters; has a family member who is CEO of Altrix Medical; serves on the Editorial Board of the Journal of Allergy and Clinical Immunology: In Practice, the Journal of Food Allergy, and the Annals of Allergy, Asthma, and Immunology. J. Oppenheimer has received financial support from DBV, Teva, GlaxoSmithKline adjudication/data safety monitoring board, AstraZeneca, Novartis, and Sanofi; and is associate editor of the Annals of Allergy, Asthma, and Immunology and AllergyWatch, an American Board of Internal Medicine (ABIM) Council Member and American Board of Allergy and Immunology Liaison to the ABIM, UpToDate Reviewer, ACCP Cough Guideline Committee Member, and WebMD Editor. R. S. Davis is a consultant for Shire, Baxalta, Circassia, Takeda, Genentech, Novartis, ALK, AAOA, Eastern Pulmonary Conference 2019, DBV Technologies, and Maculogix; is speaker for DBV Technologies, Novartis, and ALK; is the co-owner of The PBL Institute, LLC; and teaches problem-based learning techniques for many companies & Continuing Medical Education conferences. D. A. Bukstein is a consultant for the American Academy of Otolaryngic Allergy; has a CME grant; is a speaker for Odactra from ALK, AstraZeneca, Niox from Circassia, Teva Pharmaceutical Industries, Novartis, and Genentech; is a consultant for Cuvitru and HyQvia from Baxalta, and for Cuvitru, HyQvia, Xiidra, and Vyvanse from Shire; is the co-owner of The PBL Institute, LLC; and teaches problem-based learning techniques for many companies & CME conferences. M. Greenhawt is supported by the Agency for Healthcare Research and Quality (grant no. 5K08HS024599-02); is an expert panel and coordinating committee member of the National Institute of Allergy and Infectious Diseases–sponsored Guidelines for Peanut Allergy Prevention; has served as a consultant for the Canadian Transportation Agency, Thermo Fisher, Intrommune, and Aimmune Therapeutics; is a member of physician/medical advisory boards for Aimmune Therapeutics, DBV Technologies, Sanofi/Genzyme, Genentech, Nutricia, Kaleo Pharmaceutical, Nestle, Acquestive, Allergy Therapeutics, Allergenis, Aravax, and Monsanto; is a member of the Scientific Advisory Council for the National Peanut Board; has received honorarium for lectures from Thermo Fisher, Aimmune Therapeutics, DBV Technologies, Before Brands, multiple state allergy societies, the American College of Allergy, Asthma & Immunology, and the European Academy of Allergy and Clinical Immunology; is an associate editor for the Annals of Allergy, Asthma, and Immunology; and is a member of the Joint Taskforce on Allergy Practice Parameters.
Online Repository.
Table E1.
Decision aids for allergy/immunology
| Allergic condition | Decision aids |
|---|---|
| Asthma | 1. Inhaled corticostseroid treatment optionsE1 2. chestnet.orgE2 |
| Allergic rhinitis | Allergen immunotherapy∗E3, E4 |
| Food allergy | Peanut immunotherapyE5 |
| Stinging insect allergy | Venom immunotherapyE6 |
This decision aid is not compliant with International Patient Decision-Aid Standards.
References
- 1.Elwyn G., Laitner S., Coulter A., Walker E., Watson P., Thomson R. Implementing shared decision making in the NHS. BMJ. 2010;341:c5146. doi: 10.1136/bmj.c5146. [DOI] [PubMed] [Google Scholar]
- 2.National Academies of Sciences, Engineering, and Medicine Initial national priorities for comparative effectiveness research. https://www.nap.edu/read/12648/chapter/1 Available from:
- 3.Patient-Centered Outcomes Research Institute PCORI announces new initiative to support shared decision making. https://www.pcori.org/news-release/pcori-announces-new-initiative-support-shared-decision-making Available from:
- 4.Salzburg Global Seminar Salzburg statement on shared decision making. BMJ. 2011;342:d1745. doi: 10.1136/bmj.d1745. [DOI] [PubMed] [Google Scholar]
- 5.Haynes R.B., Devereaux P.J., Guyatt G.H. Physicians’ and patients’ choices in evidence based practice. BMJ. 2002;324:1350. doi: 10.1136/bmj.324.7350.1350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Washington State Legislature Shared decision making. https://depts.washington.edu/shareddm/waleg Available from:
- 7.Legare F., Stacey D., Forest P.-G. Shared decision-making in Canada: update, challenges and where next! Z Arztl Fortbild Qualitatssich. 2007;101:213–221. doi: 10.1016/j.zgesun.2007.02.024. [DOI] [PubMed] [Google Scholar]
- 8.Joseph-Williams N., Lloyd A., Edwards A., Stobbart L., Tomson D., Macphail S., et al. Implementing shared decision making in the NHS: lessons from the MAGIC programme. BMJ. 2017;357:j1744. doi: 10.1136/bmj.j1744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Washington State Law Shared decision making. https://app.leg.wa.gov/rcw/default.aspx?cite=7.70.060 Available from:
- 10.Stacey D., Legare F., Lewis K.B. Patient decision aids to engage adults in treatment or screening decisions. JAMA. 2017;318:657–658. doi: 10.1001/jama.2017.10289. [DOI] [PubMed] [Google Scholar]
- 11.Joosten E.A.G., DeFuentes-Merillas L., de Weert G.H., Sensky T., van der Staak C.P.F., de Jong C.A.J. Systematic review of the effects of shared decision-making on patient satisfaction, treatment adherence and health status. Psychother Psychosom. 2008;77:219–226. doi: 10.1159/000126073. [DOI] [PubMed] [Google Scholar]
- 12.Veroff D., Marr A., Wennberg D.E. Enhanced support for shared decision making reduced costs of care for patients with preference-sensitive conditions. Heal Aff. 2013;32:285–293. doi: 10.1377/hlthaff.2011.0941. [DOI] [PubMed] [Google Scholar]
- 13.Blaiss M.S., Steven G.C., Bender B., Bukstein D.A., Meltzer E.O., Winders T. Shared decision making for the allergist. Ann Allergy Asthma Immunol. 2019;122:463–470. doi: 10.1016/j.anai.2018.08.019. [DOI] [PubMed] [Google Scholar]
- 14.Wilson S.R., Strub P., Buist A.S., Knowles S.B., Lavori P.W., Lapidus J., et al. Shared treatment decision making improves adherence and outcomes in poorly controlled asthma. Am J Respir Crit Care Med. 2010;181:566–577. doi: 10.1164/rccm.200906-0907OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fiks A.G., Mayne S.L., Karavite D.J., Suh A., O’Hara R., Localio A.R., et al. Parent-reported outcomes of a shared decision-making portal in asthma: a practice-based RCT. Pediatrics. 2015;135:e965–e973. doi: 10.1542/peds.2014-3167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu T.-L., Taylor Y.J., Mahabaleshwarkar R., Blanchette C.M., Tapp H., Dulin M.F. Shared decision making and time to exacerbation in children with asthma. J Asthma. 2018;55:949–955. doi: 10.1080/02770903.2017.1378357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Taylor Y.J., Tapp H., Shade L.E., Liu T.-L., Mowrer J.L., Dulin M.F. Impact of shared decision making on asthma quality of life and asthma control among children. J Asthma. 2018;55:675–683. doi: 10.1080/02770903.2017.1362423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ludden T., Shade L., Reeves K., Welch M., Taylor Y.J., Mohanan S., et al. Asthma dissemination around patient-centered treatments in North Carolina (ADAPT-NC): a cluster randomized control trial evaluating dissemination of an evidence-based shared decision-making intervention for asthma management. J Asthma. 2019;56:1087–1098. doi: 10.1080/02770903.2018.1514630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stacey D., Legare F., Lewis K., Barry M.J., Bennett C.L., Eden K.B., et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2017;4:CD001431. doi: 10.1002/14651858.CD001431.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gagne M.E., Legare F., Moisan J., Boulet L.-P. Development of a patient decision aid on inhaled corticosteroids use for adults with asthma. J Asthma. 2016;53:964–974. doi: 10.3109/02770903.2016.1166384. [DOI] [PubMed] [Google Scholar]
- 21.Greenhawt M., Shaker M., Winders T., Bukstein D.A., Davis R.S., Oppenheimer J., et al. Development and acceptability of a shared decision-making tool for commercial peanut allergy therapies. Ann Allergy Asthma Immunol. 2020;125:90–96. doi: 10.1016/j.anai.2020.01.030. [DOI] [PubMed] [Google Scholar]
- 22.Sepucha K.R., Abhyankar P., Hoffman A.S., Bekker H.L., LeBlanc A., Levin C.A., et al. Standards for UNiversal reporting of patient Decision Aid Evaluation studies: the development of SUNDAE Checklist. BMJ Qual Saf. 2018;27:380–388. doi: 10.1136/bmjqs-2017-006986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Elwyn G., O’Connor A., Stacey D., Volk R., Edwards A., Coulter A., et al. Developing a quality criteria framework for patient decision aids: online international Delphi consensus process. BMJ. 2006;333:417. doi: 10.1136/bmj.38926.629329.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Johns Hopkins University & Medicine. Coronavirus Resource Center. https://coronavirus.jhu.edu/map.html Available from: Accessed July 6, 2020.
- 25.Institute for Health Metrics and Evaluation. Forecasting COVID-19 impact on hospital bed-days, ICU-days, ventilator days and deaths by US state in the next 4 months. http://www.healthdata.org/research-article/forecasting-covid-19-impact-hospital-bed-days-icu-days-ventilator-days-and-deaths Available from: Accessed July 6, 2020.
- 26.Shaker M.S., Oppenheimer J., Grayson M., Stukus D., Hartog N., Hsieh E., et al. COVID-19: pandemic contingency planning for the allergy and immunology clinic. J Allergy Clin Immunol Pract. 2020;8:1477–1488.e5. doi: 10.1016/j.jaip.2020.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shaker M.S., Mosnaim G., Oppenheimer J., Stukus D., Abrams E.M., Greenhawt M. Health and economic outcomes of home maintenance allergen immunotherapy in select patients with high health literacy during the COVID-19 pandemic: a cost-effectiveness analysis during exceptional times. J Allergy Clin Immunol Pract. 2020;8:2310–2321.e4. doi: 10.1016/j.jaip.2020.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Griffith M.L., Siminerio L., Payne T., Krall J. A shared decision-making approach to telemedicine: engaging rural patients in glycemic management. J Clin Med. 2016;5:103. doi: 10.3390/jcm5110103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yu C.H., Ivers N.M., Stacey D., Rezmovitz J., Telner D., Thorpe K., et al. Impact of an interprofessional shared decision-making and goal-setting decision aid for patients with diabetes on decisional conflict--study protocol for a randomized controlled trial. Trials. 2015;16:286. doi: 10.1186/s13063-015-0797-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stacey D., Briere N., Robitaille H., Fraser K., Desroches S., Legare F. A systematic process for creating and appraising clinical vignettes to illustrate interprofessional shared decision making. J Interprof Care. 2014;28:453–459. doi: 10.3109/13561820.2014.911157. [DOI] [PubMed] [Google Scholar]
- 31.Ottawa Hospital Research Institute Ottawa Hospital—interprofessional shared decision making models. https://decisionaid.ohri.ca/ip-sdm.html Available from:
- 32.Legare F., Stacey D., Gagnon S., Dunn S., Pluye P., Frosch D., et al. Validating a conceptual model for an inter-professional approach to shared decision making: a mixed methods study. J Eval Clin Pr. 2011;17:554–564. doi: 10.1111/j.1365-2753.2010.01515.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Layman E. Health informatics: ethical issues. Heal Care Manag. 2003;22:2–15. doi: 10.1097/00126450-200301000-00002. [DOI] [PubMed] [Google Scholar]
- 34.Bauer K.A. Home-based telemedicine: a survey of ethical issues. Camb Q Heal Ethics. 2001;10:137–146. doi: 10.1017/s0963180101002043. [DOI] [PubMed] [Google Scholar]
- 35.Kaplan B., Brennan P.F. Consumer informatics supporting patients as co-producers of quality. J Am Med Inf Assoc. 2001;8:309–316. doi: 10.1136/jamia.2001.0080309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bernhardt J.M. Health education and the digital divide: building bridges and filling chasms. Health Educ Res. 2000;15:527–531. doi: 10.1093/her/15.5.527. [DOI] [PubMed] [Google Scholar]
- 37.Politi M.C., Clark M.A., Ombao H., Dizon D., Elwyn G. Communicating uncertainty can lead to less decision satisfaction: a necessary cost of involving patients in shared decision making? Heal Expect. 2011;14:84–91. doi: 10.1111/j.1369-7625.2010.00626.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kent D.M., Shah N.D. Risk models and patient-centered evidence: should physicians expect one right answer? JAMA. 2012;307:1585–1586. doi: 10.1001/jama.2012.469. [DOI] [PubMed] [Google Scholar]
- 39.Boland L., Graham I.D., Legare F., Lewis K., Jull J., Shephard A., et al. Barriers and facilitators of pediatric shared decision-making: a systematic review. Implement Sci. 2019;14:7. doi: 10.1186/s13012-018-0851-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vermunt N., Elwyn G., Westert G., Harmsen M., Olde Rikkert M., Meinders M. Goal setting is insufficiently recognised as an essential part of shared decision-making in the complex care of older patients: a framework analysis. BMC Fam Pr. 2019;20:76. doi: 10.1186/s12875-019-0966-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Stukus D.R. How Dr Google is impacting parental medical decision making. Immunol Allergy Clin North Am. 2019;39:583–591. doi: 10.1016/j.iac.2019.07.011. [DOI] [PubMed] [Google Scholar]
- 42.Abrams E.M., Greenhawt M. Special article: risk communication during COVID-19. J Allergy Clin Immunol Pract. 2020;8:1791–1794. doi: 10.1016/j.jaip.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Carpio-Escalona L.V., Gonzalez-de-Olano D. Use of the Internet by patients attending allergy clinics and its potential as a tool that better meets patients’ needs. J Allergy Clin Immunol Pract. 2018;6:1064–1066. doi: 10.1016/j.jaip.2017.10.034. [DOI] [PubMed] [Google Scholar]
- 44.Ives M. When epidemics go viral. The Atlantic. October 18, 2016. https://www.theatlantic.com/health/archive/2016/10/when-epidemics-go-viral/504503/ Available from:
- 45.Fernandez-Luque L., Bau T. Health and social media: perfect storm of information. Heal Inf Res. 2015;21:67–73. doi: 10.4258/hir.2015.21.2.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Department of Global Communications UN tackles ‘infodemic’ of misinformation and cybercrime in COVID-19 crisis. https://www.un.org/en/un-coronavirus-communications-team/un-tackling-infodemic-misinformation-and-cybercrime-covid-19 Available from:
- 47.Boland L., McIsaac D.I., Lawson M.L. Barriers to and facilitators of implementing shared decision making and decision support in a paediatric hospital: a descriptive study. Paediatr Child Heal. 2016;21:e17–e21. doi: 10.1093/pch/21.3.e17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Schonberg M.A., Kistler C.E., Pinheiro A., Jacobson A.R., Aliberti G.M., Karamourtopoulos M., et al. Effect of a mammography screening decision aid for women 75 years and older: a cluster randomized clinical trial. JAMA Intern Med. 2020;180:831–842. doi: 10.1001/jamainternmed.2020.0440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shaker M., Kanaoka T., Feenan L., Greenhawt M. An economic evaluation of immediate vs non-immediate activation of emergency medical services after epinephrine use for peanut-induced anaphylaxis. Ann Allergy Asthma Immunol. 2019;122:79–85. doi: 10.1016/j.anai.2018.06.035. [DOI] [PubMed] [Google Scholar]
- 50.Abrams E.M., Singer A.G., Chan E.S. Pre-emptive screening for peanut allergy before peanut ingestion in infants is not standard of care. CMAJ. 2019;191:E1169–E1170. doi: 10.1503/cmaj.73447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Abrams E.M., Chan E.S. Potential pitfalls in applying screening criteria in infants at risk of peanut allergy. J Pediatr. 2018;195:269–274. doi: 10.1016/j.jpeds.2017.12.011. [DOI] [PubMed] [Google Scholar]
- 52.Abrams E.M., Ben-Shoshan M. Delabeling penicillin allergy: is skin testing required at all? J Allergy Clin Immunol Pract. 2019;7:1377. doi: 10.1016/j.jaip.2018.11.052. [DOI] [PubMed] [Google Scholar]
- 53.Greenhawt M., Shaker M. Determining levers of cost-effectiveness for screening infants at high risk for peanut sensitization before early peanut introduction. JAMA Netw Open. 2019;2:e1918041. doi: 10.1001/jamanetworkopen.2019.18041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Shaker M.S., Oppenheimer J., Wallace D.V., Golden D.B.K., Lang D.M., Lang E.S., et al. Making the GRADE in anaphylaxis management: toward recommendations integrating values, preferences, context, and shared decision making. Ann Allergy Asthma Immunol. 2020;124:526–535.e2. doi: 10.1016/j.anai.2020.03.009. [DOI] [PubMed] [Google Scholar]
- 55.Rabi D.M., Kunneman M., Montori V.M. When guidelines recommend shared decision-making. JAMA. 2020;323:1345–1346. doi: 10.1001/jama.2020.1525. [DOI] [PubMed] [Google Scholar]
- 56.National Hospice and Palliative Care Organization Coronavirus disease 2019 (COVID-19) shared decision making tool. https://www.nhpco.org/wp-content/uploads/COVID-19-Shared-Decision-Making-Tool.pdf Available from:
- 57.Searing D.A., Dutmer C.M., Fleischer D.M., Shaker M.S., Oppenheimer J., Grayson M.H., et al. A phased approach to resuming suspended allergy/immunology clinical services. J Allergy Clin Immunol Pract. 2020;8:2125–2134. doi: 10.1016/j.jaip.2020.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Meyer N., Shatner W., Nimoy L., Alley K. 1982. Star Trek II: The Wrath of Khan (DVD). Paramount. [Google Scholar]
- 59.Elwyn G., Frosch D.L., Kobrin S. Implementing shared decision-making: consider all the consequences. Implement Sci. 2016;11:114. doi: 10.1186/s13012-016-0480-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Auerbach A.D., Landefeld C.S., Shojania K.G. The tension between needing to improve care and knowing how to do it. N Engl J Med. 2007;357:608–613. doi: 10.1056/NEJMsb070738. [DOI] [PubMed] [Google Scholar]
References
- Gagne M.E., Legare F., Moisan J., Boulet L.-P. Development of a patient decision aid on inhaled corticosteroids use for adults with asthma. J Asthma. 2016;53:964–974. doi: 10.3109/02770903.2016.1166384. [DOI] [PubMed] [Google Scholar]
- Allergy & Asthma Network, CHEST Foundation. Severe asthma SDMK. http://severeasthmatreatments.chestnet.org/ Available from: Accessed April 24, 2020.
- https://www.nemours.org/content/dam/nemours/wwwv2/filebox/research/Environmental%20Allergies%20Decision%20Aid.pdf Available from: Accessed April 24, 2020.
- American College of Allergy, Asthma & Immunology. Allergen immunotherapy shared decision making. http://allergyrelief.acaai.org/ Available from: Accessed April 24, 2020.
- Greenhawt M., Shaker M., Winders T., Chan E.S., Stukus D.R., Matlock D., et al. Development and acceptability of a shared decision-making tool for commercial peanut allergy therapies. Ann Allergy Asthma Immunol. 2020;125:90–96. doi: 10.1016/j.anai.2020.01.030. [DOI] [PubMed] [Google Scholar]
- Ottawa Hospital Research Institute. Patient decision aids. https://www.healthwise.net/ohridecisionaid/Content/StdDocument.aspx?DOCHWID=rt1299 Available from: Accessed April 24, 2020.