Abstract
Wellens’ syndrome refers to electrocardiographic (ECG) abnormalities in the precordial T‐wave segment, which are associated with critical stenosis of the proximal left anterior descending (LAD) coronary artery. According to medical literature, this ECG abnormality is of paramount importance because this syndrome represents a preinfarction stage of coronary artery disease; however, same ECG pattern can also be seen in other conditions. Coronary fistula occurs due to anomalous communications between a coronary artery and a cardiac chamber or other vessel in the vicinity of the heart. We report a case of multiple coronary artery fistulae to the left ventricle in a 74‐year‐old woman who had a 2‐year history of intermittent atypical chest pain and exercise dyspnea with positive criteria mimicking Wellens’ syndrome without coronary atherosclerosis.
Keywords: cardiac anatomy, non‐invasive techniques‐electrocardiography
1. INTRODUCTION
The association of the positive criteria and ECG changes mimicking Wellens’ syndrome with the presence of multiple coronary artery fistulae (CF) is unusual. CF occur due to anomalous communications between a coronary artery and a cardiac chamber or other vessel in the vicinity of the heart. They are congenital coronary anomalies and are discovered in 0.15% of patients undergoing coronary angiography following chest pain or dyspnea. The positive criteria mimic Wellens’ syndrome, providing evidenced for the fact that this syndromeis not only associated with the presence of critical stenosis of the proximal LAD artery, but that many causes may mimic the syndrome. The term must be reviewed and discouraged to refer to its findings.
2. CASE REPORT
A 74‐year‐old woman presented with intermittent chest pain and dyspnea on exertion that worsened with exercise for the past 2 years (New York Heart Association class II/III). She had a medical history of hypercholesterolemia treatment with statins and smoking. The physical examination and arterial pressure measurement were normal. ECG performed without chest pain showed a mild depression of the ST segment and changes in T wave suggestive of Wellens’ syndrome type B (Figure 1). The echocardiography demonstrated a normal ejection fraction and hypokinetic apex. The value of the cardiac troponin was normal. A nuclear stress test was inconclusive and was followed by coronary angiography (CAG), without coronary obstructive disease, but a tortuous artery in the left anterior descending artery (LAD), left circumflex artery (LCx), and right coronary artery (RCA) was observed, and presence of multiple coronary artery fistulae in LAD, LCx, and RCA was detected (Figure 2, Videos 1 , 2 ). Medical treatment for ischemia was started without nitroglycerin.
Figure 1.

ECG. Wellens' Syndrome with pattern type B. Biphasic T‐wave inverted in leads V1 to V3 (arrows), and symmetrical and deep‐inverted T‐wave V4 to V6. ST segment with mild depression (V4‐V6) and normal precordial R‐wave progression, and absent Q waves
Figure 2.
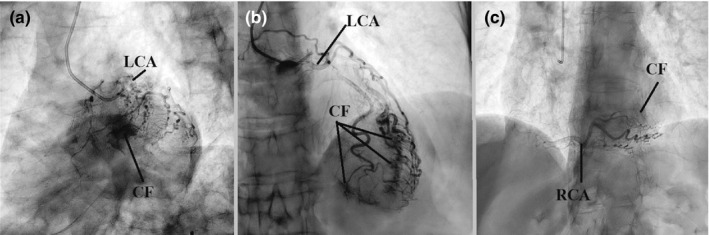
Coronary angiography: Panels a, b. LCA without atherosclerotic lesions. Tortuous artery in the LAD, LCX arteries. Presence of multiple coronary artery fistulae in territory of LAD and LCX arteries. Panel C. RCA dominant showed tortuous artery and coronary artery fistula. LCA, left coronary artery; LAD, left anterior descending artery; LCX, left circumflex artery. RCA, right coronary artery. CF: coronary fistula
3. DISCUSSION
Wellens’ syndrome refers to specific ECG abnormalities in the precordial T wave, which are associated with critical stenosis of the proximal LAD artery. The criteria include: (a) characteristic T‐wave changes, (b) history of anginal chest pain, (c) normal or minimally elevated cardiac enzyme levels, and (d) ECG without Q waves, without significant ST‐segment elevation, and with normal precordial R‐wave progression.
Recognition of this ECG abnormality is described to be paramount importance in the medical literature because this syndrome represents a preinfarction stage of coronary artery disease (CAD) that often progresses to an anterior wall myocardial infarction. (De Zwaan, Bär, & Wellens, 1982).
The ECG changes seen in Wellens’ syndrome are typically manifested when the patient is pain‐free but usually occur in the context of recent anginal chest pain. The ST segment will be straight or concave and will pass into a deep negative T wave at an angle of 60°–90°. In Wellens’ syndrome, these changes generally occur in leads V1–V4 but occasionally may also involve V5 and V6. In type B (25% of patients), biphasic T waves are typically observed in V2 and V3; However, similar ECG patterns have been described in other conditions.
Different causes are known to contribute toward the development of pseudo‐Wellens’ syndrome, and differential diagnosis is based on the following conditions: coronary artery vasospasm (cocaine), Takotsubo syndrome, increased cardiac demand, cerebral hemorrhage, myopericarditis, Wolf–Parkinson–White syndrome, digitalis effect, pulmonary embolic disease, and generalized hypoxia. (Krause, 1985).
Coronary arteriovenous fistulae (CAVF) are observed in 0.002% of the general population were first described by Krause in 1865. (Rhinehardt, Brady, Perron, & Mattu, 2002).
These coronary artery anomalies involve abnormal communication between one or more coronary arteries and one of the cardiac chambers (coronary cameral fistulae) or the great vessels adjacent to the heart (coronary artery or arteriovenous fistulae). (Ogden, 1970) This is anomalous communications between a coronary artery and a cardiac chamber or other vessel in the vicinity of the heart. They are the most frequently occurring congenital heart anomalies and are discovered in 0.15% of patients undergoing coronary angiography. Coronary artery fistulae are rare abnormalities of the coronary arteries that are usually discovered incidentally on coronary angiogram. The occurrence of multiple fistulae is an unusual condition. (Ata et al., 2009).
The feeding artery of the fistula may drain from a coronary artery or one of its branches and is usually dilated and tortuous. The more proximal the origin from the main coronary artery, the more dilated the feeding artery tends to be, and the more distal the origin, the more tortuous it appears to be. Fistulae originating from the left coronary artery and draining into the left ventricle tend to be particularly tortuous, presenting a challenge for transcatheter closure (TCC). Finally, there may be multiple feeding arteries to a single drainage point, and multiple drainage sites may exist. (Ata et al., 2009; Qureshi, 2006)
TCC of the coronary fistulae was advised for this patient and was discharged, and conservative approach with medical treatment was adopted.
4. CONCLUSION
The multiple coronary cameral fistulae are described, which cause myocardial ischemia or heart failure. Aggressive treatment with embolization with coils is recommended in coronary fistula, but this patient, with anomalous coronary anatomy without atherosclerotic lesions, showed poor prognosis with this treatment. In this case, the presentation of this referred patient and findings in ECG mimic Wellens’ syndrome. The so‐called “Wellens’ syndrome” is associated not only with the presence of critical stenosis of the proximal LAD artery, but many causes that can stimulate the onset of the syndrome. It is time to discard the term “Wellens’ syndrome” for obvious reasons. When referring to it, there are numerous causes that can mimic this condition. The use of the term Wellens’ syndrome should be discouraged. In this case, the conservative approach with medical treatment has been proven to be successful for the management of symptoms.
Supporting information
Ibarrola M. Wellens’ syndrome and finding of multiple coronary cameral fistulae: Is it time to discard this term? Ann Noninvasive Electrocardiol. 2020;25:e12693 10.1111/anec.12693
REFERENCES
- Ata, Y. , Turk, T. , Bicer, M. , Yalcin, M. , Ata, F. , & Yavuz, S. (2009). Coronary arteriovenous fistulas in the adults: Natural history and management strategies. Journal of Cardiothoracic Surgery, 4, 62 10.1186/1749-8090-4-62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Zwaan, C. , Bär, F. W. , & Wellens, H. J. (1982). Characteristic electrocardiographic pattern indicating a critical stenosis high in left anterior descending coronary artery in patients admitted because of impending myocardial infarction. American Heart Journal, 103(4), 730–736. 10.1016/0002-8703(82)90480-X [DOI] [PubMed] [Google Scholar]
- Krause, W. (1985). Über den Ursprung einer akzessorischen A. coronaria cordis aus der A. pulmonis . Z Rationelle Med, 24, 225–227. [Google Scholar]
- Ogden, J. A. (1970). Congenital anomalies of the coronary arteries. The American Journal of Cardiology, 25(4), 474–479. 10.1016/0002-9149(70)90016-0 [DOI] [PubMed] [Google Scholar]
- Qureshi, S. A. (2006). Coronary arterial fistulas. Orphanet Journal of Rare Diseases, 1(1), 10.1186/1750-1172-1-51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhinehardt, J. , Brady, W. J. , Perron, A. D. , & Mattu, A. (2002). Electrocardiographic manifestations of Wellens’ syndrome. The American Journal of Emergency Medicine, 20, 638–643. 10.1053/ajem.2002.34800 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


