Abstract
In developing countries, access to qualified medical personnel especially oral health care specialists by inhabitants of rural and remote areas remain a challenge due to the fact that these personnel are mostly located in urban communities. Teledentistry is an approach that will eliminate the problem of distance between qualified oral health care personnel and potential patients in rural and remote communities. The objective of this review is to investigate the history of teledentistry and its practical application in overcoming the rural-urban oral health care problems.
A scoping search of literature using keywords associated with telemedicine and teledentistry and its application was undertaken via PubMed and Scientific Electronic Library Online (SciELO). Literature published in English in the last 10 years (2008 - 2018) were selected. The review summarises the available literature related to origin and method of delivering teledentistry and its use in dental practice and education. It shows that teledentistry has the ability to improve access to and delivery of oral health care at a relatively lower cost as well as supplementing traditional teaching methods in dental education. However, despite the promising nature of teledentistry in improving oral health care provision, it is associated with some attending problems and challenges.
Keywords: Telemedicine, Teledentistry, Rural, Remote, Developing countries
INTRODUCTION
In both developed and developing countries, the importance of adequate and everyday routine and emergency medical and dental services for everyone cannot be overemphasized. However, over the years, the need has arisen for a wider reach of these services where medical experts may not be readily available. This is particularly so for developing countries where access to qualified medical personnel especially specialists by residents of rural and remote areas still remains a challenge. Several barriers to oral health care in rural area have been found, these barriers include lower health care provider to population ratio, cost of dental care, poor infrastructure and inadequate dental facilities. Other barriers include longer travel distances to dental facilities, lack of transportation to obtain dental care, lack of awareness about oral health, geographic barriers to care, poverty and cultural barriers. As a result of this discrepancy in oral health care delivery and availability between rural and urban areas, different modalities have been explored one of which is teledentistry.
The term "Teledentistry" was first used in 1997, when Cook defined it as "… the practice of using videoconferencing technologies to diagnose and provide advice about treatment over a distance"8. It uses electronic medical records, ICT and the internet to provide consultation at a distance8. Teledentistry can be applied in four ways namely teleconsultation, teleeducation, telemonitoring and telesurgery.
In teleconsultation, the local general dentist in a remote area can seek consultation from a specialist by transmitting data as the patients are being attended to or stored data of patients to the specialist. Practitioners in rural remote areas can receive continue medical education through interactive video-conferencing and web-based self-instruction which have been developed and stored.
Meanwhile in telemonitoring, patients’ condition can be monitored by the patient recording and transmitting data to physician by telephone, facsimile or the internet. Patients’ condition can also be monitored by continuous data collection and automatic transmission to another physician involved in the management of the patients. Using telesurgery, specialists in urban areas assist surgeons in rural remote areas via video and audio connections in the internet to provide adequate surgery to patients.
This technology allows collaborations between multiple dental practitioners with a view of reaching accurate diagnosis and adequate treatment plan of patients seen in areas where there is shortage or unavailability of dentists or dental specialists. Therefore, the purpose of this review is to investigate the history of teledentistry and its practical application in overcoming the rural-urban oral health care problems.
METHODOLOGY
This was a systematic review of literature on teledentistry and its possible application in rural and urban areas. Prior to this review, the following steps were taken; (i) identification of the reasons for the discrepancy oral health care between rural and urban areas, (ii) development of a question based on the history and possible role of teledentistry in providing solutions to these problems, (iii) definition of the inclusion and exclusion criteria of studies or search in literature (iv) critical analysis of the included studies (v) collation of results (vi) discussion of the practicability of our findings in solving the pending problems.
Only articles published in English in the last 10 years (2008 - 2018) were included in this review and the search for the articles that were reviewed was done on PubMed and Scientific Electronic Library Online (SciELO).
History of teledentistry
In 1989, a conference on dental informatics funded by the Westinghouse Electronics Systems Group in Baltimore, USA developed an initial idea about teledentistry. The idea was based on how to apply dental informatics in dental practice to directly affect the delivery of oral health care9. Subsequently, in 1994, a US Army's Total Dental Project aimed at improving patient care, dental education and effectuation of the communication between dentists and dental laboratories demonstrated the use of teledentistry in extending dental care to distant and rural areas and offering complete information required for deeper analyses6. As technology has advanced, new opportunities for teledentistry have been created thereby changing the dynamics of dental care delivery by offering improve patient care and reshaping current business models10.
Method of delivering teledentistry
Just like telemedicine, teledentistry can be delivered inform of teleconsultation, teleeducation, telemonitoring and telesurgery via the following 2 major ways:
-
Real-time teledentistry involves a videoconferencing in which dental professionals and their patients, at different locations, may see, hear and communicate with one another – Figure 111.
To enable live videoconferencing, a widely available standalone IP/ISDN videoconferencing solution or a PCI codec board that will accommodate audio and visual function should be installed into the system and a control unit that bridges three or more parties is also required12. A form of real time teledentistry is remote monitoring method which involves monitoring patients from a distance which could either be from a hospital or from home13.
-
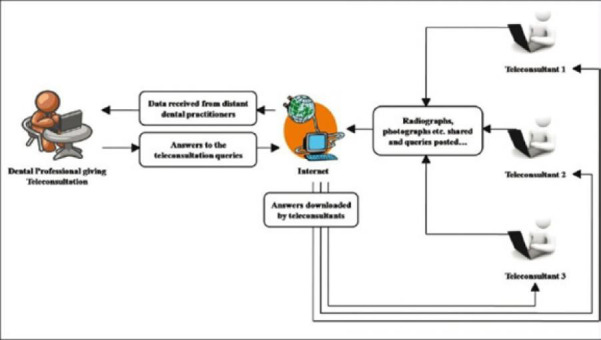
Store-and-Forward teledentistry involves the exchange of clinical information and static images collected and stored in a telecommunication equipment by a dental practitioner who later then forward them to another practitioner for consultation and treatment planning – Figure 214.
In this type of teledentistry, the patient is not present during the consultation15 and the dentist can share patient information, radiographs, graphical representations of oro-facial tissues, therapies applied, laboratory results, tests, remarks, photographs and other information transportable through multiple providers4. This allows collaboration between general practitioners and specialist regarding a patient and the necessary treatment for this patient. It involves the local dentist digitizing and electronically transmitting clinical photographs, and X-rays to the specialist and thus enables the specialist to make a diagnosis and recommend treatment options or referral15. A typical store and forward teledentistry system consists of a computer with substantial hard drive memory, adequate RAM, a speedy processor, an intraoral video camera and a digital camera, a modem for internet connection11, 14.
Figure 1:

Real time consultation Source: Jampani et al (4)
Figure 2:
Store and forward Source: Jampani et al4
Evidence of teledentistry use:
Oral medicine and diagnosis –
In oral medicine, adequate images of suspicious oral lesions can be taken and sent to a consultant who then makes adequate diagnosis and proffers a treatment plan for the on-site personnel to effect. Follow up of such patients after institution of treatment can then be done via telemonitoring where the specialist can appraise the patient and decide on the next course of management. For example, in Northern Ireland, patients referred by dentists and doctors to the Regional Oral Medicine Consultant were placed on a long waiting list based on urgency of the case but with the introduction of teledentistry in 2005, it was possible to triage oral medicine cases and to support locally based treatment16.
Similarly, in developing countries, oral lesions seen in rural remote areas can be adequately managed by the very few consultants located in urban communities. Images of these oral lesions can be taken with a camera and sent to these consultants via email and WhatsApp. The feasibility of adequately managing oral lesions via images sent through emails has been reported in a previous Brazilian study.17 Dental hygienists in Arizona, USA were able to provide oral health care to underserved populations by forwarding diagnostically efficacious digital data from remote settings to a distant oral health team18. This initiative if adopted in developing countries can help provide oral hygiene prophylaxis to inhabitants of rural and remote communities where dentists would not want to work. Use of teledentistry to diagnosis cases of traumatic dental injuries in person and remotely has been evaluated and the evaluation showed that the precision of the two diagnoses were comparable and the levels of inter-examiner agreement were higher when clinical data were included with the images19. In developing countries where the use of mobile smartphones has increased, their cameras can be used to take images of oral lesions in remote settings and diagnosis of the lesions made in distant locations. This was demonstrated in a previous study that showed intraoral camera to be a reliable tool in screening for oral diseases20. For example, Similarly, mobile teledentistry approach has shown the potential to detect occlusal caries from photographs taken by a smartphone camera with an acceptable diagnostic performance compared to traditional face-to-face screening21. Furthermore, teledentistry showed excellent accuracy for diagnosing dental pathology in older adults living in nursing homes and its use may allow more regular checkups to be carried out by dental professionals22. Cloud-based telemedicine application for screening for oral diseases was recently evaluated and provided evidence that a robust system for store-and-forward screening for dental problems can be developed, and leads to the need for further testing of its robustness to confirm the accuracy and reliability of the teledentistry system23.
Endodontology:
Endodontics is a specialised part of dental practice provided by endodontics who are rarely found in remote areas in developing countries. Teledentistry can be used to provide endodontic services in these underserved communities. For example, it can be used to recognise root canal orifices at a distance thereby suggesting that remote recognition of root canals by experienced dentists can help younger colleagues in the detection of root canal orifices24. Teledentistry based on the internet as a telecommunication medium can be successfully utilized in the diagnosis of periapical lesions of the anterior teeth, reducing the costs associated with distant visits and making urgent help available25. A study that compared conventional viewing versus a video conferencing system of artificial and in vivo periapical lesions showed no statistical significant difference between the ability of evaluators to identify periapical bone lesions using conventional radiographs on a view box and their ability to interpret the same images transmitted on a monitor screen by a video teleconferencing system.
Prosthodontology:
In prosthodontics, proper evaluation of edentulous ridges, supporting tissue structures and abutment teeth can be done via diagnostic casts, clinical photographs and radiographs obtained via teledentistry and the appropriate prosthesis can be fabricated by the on-site general dentist and dental technologist. In a study on the use of videoconferencing for diagnosis and treatment planning for patients requiring prosthetic or oral rehabilitative treatment, a diagnosis or treatment plan could be made in 24 out of 27 teleconsultations26. All participating dentists were satisfied with the consultation process and indicated that the technology used was of sufficient quality for clinical purposes.
Periodontology:
In periodontology, teleconsultation was used to diagnose and refer patients who required periodontology services from a remote location 150 miles way27. All patients who had periodontal surgery had their sutures removed at the remote location under the tele-supervision of the periodontologist.
Oral and Maxillofacial Surgery:
In oral surgery, adequate assessment of orofacial emergencies such as Ludwig’s angina and necrotising fasciitis can be done and appropriate medical and surgical intervention as it affects the maxillofacial region can be discussed with the general surgeon on-site via facilities provided by teledentistry. A study on efficiency of telemedicine consultation for preoperative assessment of patients for dentoalveolar surgery with general anaesthesia and nasotracheal intubation showed that telemedicine consultations were as reliable as those conducted by traditional methods28. Similarly, diagnostic assessment of the clinical diagnosis of impacted or semi-impacted third molars assisted by the telemedicine approach was equal to the real-time assessment of clinical diagnosis29. A store-and-forward telemedicine system was effective and accurate as a preoperative tool for impacted third molar pathology because it avoided unnecessary visits to the hospital and shortens waiting time30. Telecommunication is an efficient and cost-effective mechanism to provide pre-operative evaluation of conditions requiring dentoalveolar surgery in which patient transport is difficult or costly28. There is a need for change in the referral system of oral and maxillofacial surgery care, teledentistry could be one way to improve access to this care31. For example, smart phones could provide fast and clear access to electronically mailed images because the oral and maxillofacial surgeon can access them in places where there is no laptop or desktop computer32. This in turn will improve efficiency of the specialty consultation thereby ultimately improve care to the maxillofacial patient32.
Orthodontics:
The use of teledentistry in orthodontics has been reported in the literature. Its use in screening orthodontic referrals, consultations, and managing minor emergencies have been reported. Prior to comprehensive orthodontic treatment, initial assessment and pre-orthodontic treatment such as extractions and impression taking for study model can be done via teledentistry services. The sensitivity, positive predictive value, specificity and negative predictive value of teledentistry for screening new patient orthodontic referrals were 0.80, 0.92, 0.73 and 0.50 respectively indicating that it is a valid system for positively identifying new patient orthodontic referrals and it could be a significant factor in reducing inappropriate referral rate33. When referral to an orthodontist is not feasible, interceptive orthodontic treatments provided by general dentists and supervised remotely by orthodontists through teledentistry are a viable method to reducing the severity of malocclusion in disadvantaged children34. Teledentistry has been used to solve minor orthodontic emergencies arising from rubber ligature displacement, discomfort and irritations to cheek easily at home thereby limiting visits to the dental clinic35. Studies have reported that orthodontists support the use of teledentistry to provide advice to dentists and patients36. Similarly, general dental practitioners mentioned that teledentistry enabled them to offer better service to their patients and use specialist service more appropriately36. For example, it enabled them to have quick access to advice that enabled them to handle a wider range of cases themselves37.
Pediatric and Preventive Dentistry:
The use of teledentistry in paediatric and preventive dentistry was demonstrated by using it to screen preschool children for the presence of oral diseases. In one of such study, intraoral camera was a feasible and potentially cost-effective alternative to a visual oral examination for caries screening when 50 preschool children aged 4 to 6 years who were examined by a calibrated examiner38. In Rochester, New York, for the first time many children attending inner-city child-care centres have had their teeth examined at an early age and were given prompt feedback on the need for dental care via teledentistry39. Remote diagnosis of children dental problems based on non-invasive photographs constitute a valid resource40.
Dental Education:
Most dental practitioners and dental teachers do not know that teledentistry cannot only be used for increased access to dental care but also for dental education. In 2013, a systematic review of the literature on teledentistry showed that the most common type of teledentistry application was dental education41. Teledentistry in dental education can be divided into 2 main categories: self-instruction and interactive videoconferencing, the later has better results because of its ability to provide immediate feedback9. Teledentistry provides an opportunity to dental students and dental practitioners by supplementing traditional teaching methods in dental education. The effectiveness of video support in teaching of manual skills related to periodontal therapy42 and craniomaxillofacial surgery43suggest that computer based video support can be an effective aid in improving skills and treatment outcomes related to oral health. Video conferencing used as an instructional tool in a dental school course on health education44 and in examination of undergraduate dental students45 showed that it was feasible to use the tool and students were satisfied with its use. Furthermore, introduction of e-learning in dental radiology revealed significant improvement in the final year results of dental students.46 In postgraduate education, recorded interactive seminars and follow up discussions were effective method in orthodontic distance education because it allowed residents in orthodontics access to various materials and experts47, 48.
Short Coming of Teledentistry
Despite the promising nature of teledentistry in improving oral health care provision it is associated with some attending problems and challenges. One of these challenges is cost of the telemedicine equipment. Whitten et al.49 in a systematic review investigated the cost effectiveness of telemedicine interventions and found it not to be a cost-effective means of delivering healthcare. Similarly, Schuffman and Steed50 also found teledentistry to be cost ineffective but predicted that its cost effectivity would improve with its popularity and use. Another problem is the payment of the teledental oral healthcare professional. The question of "who pays the teledentistry service provider?" has been an unanswered one as majority of studies on teledentistry have been covered by grants and terminated on exhaustion of funds.
Globally, there is a significant variation with regards to confidentiality of dental information, privacy, consent, malpractice, liability, licensure and jurisdiction between countries. This difference has raised some medicolegal and copyright concerns. Presently, there is no measure to ensure safety and effectiveness of information and its transfer thus risk of compromise by unauthorized individuals is high. There is therefore a need to formulate well defined requirements protocols to prevent these foreseen issues.
Internet access may impose a major challenge. For example if there is loss of internet access during teledentistry service provision or data transmission, this may result in termination of consultation session or misdiagnosis. Another possibility is loss of data or interjection of data during the process of transmission by unauthorized individuals which may ultimately lead to the failure of the teledentistry program.
Teledentistry requires some computer knowledge both on the part of the service seeker and service provider. As a result, there is a need to train individuals in areas where teledentistry is to be utilized. This training will require financing and time. In addition, most of the teledentistry- based education programs are in English, therefore, for it is to be utilized globally, the programs need to be translated to different languages.
DISCUSSION
The use of teledentistry is expanding but there are still some barriers to its increased use. If the attending problems and challenges of using teledentistry is overcome, it will make oral health care services available to a wider group of the population in developing countries. If government can make internet technology available to oral health practitioners at low cost then teledentistry services will be easily adopted in patient care especially if the cost of care is affordable. Presently there is a dearth of studies on its use in developing countries. The potential of teledentistry in the delivery of oral health services to inhabitants of underserved areas in developing countries who have limited access to oral health care cannot be overemphasized. Teledentistry can be an alternative approach to deliver existing oral health services to these areas where there is shortage of oral health care providers. Application of teledentistry aim to bring about efficiency, provide access to underserved population, improve quality of care and reduce oral disease burden. Its application is especially of great value and importance to rural and remote areas of developing countries.
Images of dental conditions can be taken in a remote area and sent to a specialist in a distant location who will then make adequate diagnosis, proffer treatment and follow up management thereby improving or increasing access of inhabitants of remote areas to oral health care. This will also help to solve the problem of long waiting list of patients who want to access the services of specialists who are mainly located in urban communities. In developing countries where there are no specialists in remote communities, it can help to bring specialise care to these communities. If the projections on the shortages of dentists in some developing countries come to pass then teledentistry will not only be important for rural communities but also for urban and suburban communities. An added advantage of teledentistry is its utility as an excellent tool for triage23 as patients’ information sent to a specialist can be carefully prioritised in order of urgency with those needing prompt treatment at the top of the ladder while the other end features subtle cases which may not need referral thus aiding early detection and reducing waiting time for patients at risk.
Teledentistry as a tool has vast potential in improving health care delivery in developing countries because prompt treatment can be instituted with distance not being a constraint. In developing countries where transportation especially for patients is difficult or costly, teledentistry will help to minimise costs associated with distant travel. Telecommunication has been reported to be a cost-effective mechanism to provide preoperative evaluation, treatment and follow up.29 In developing countries where there is inequality in oral health care delivery between inhabitants of remote and urban communities, teledentistry can help bring equity. Teledentistry has the potential of bridging the gap in healthcare delivery between rural and urban regions and improve access of rural dwellers to oral health services at potentially reduced costs51. It may be more economical to move data from place to place than to move doctors or patients from place to place29. Also, health assistants, dental technologists, other health workers and even young dentists residing in rural areas can be brought up to speed on current advances in dental practice via tele-education which is a form of teledentistry52. In addition, teledentistry will allow interprofessional communications which will improve dentistry’s integration into the larger health care delivery system in developing countries11.
The advent of communication and information technologies has greatly affected the way in which health care is delivered and the relationship between doctors and patients53. The way it provided oral health care services to people in disadvantaged communities in some developed countries can be adopted in developing countries. Many people in rural communities in developing countries now use smart phones, the simplest device that can be used to undertake teledentistry. Mobile phones may be an effective tool for capturing images that assist in the remote diagnosis of traumatic dental injuries19. Estai et al. 23 reported its use for remote screening of dental caries by mid-level dental providers in Australia.
A previous study on knowledge and awareness of teledentistry among dental professionals in India showed that most of them lack adequate knowledge and awareness on teledentistry54. It is expected that this finding will most likely be the case in other developing countries. Therefore, there is a need to create awareness and instil positive attitudes on teledentistry among dental professionals in developing is countries. Dental practitioners in Australia generally reported optimism and support to the concept of teledentistry and its integration into current dental practices23. Addressing how teledentistry can benefit specific practice issues, would encourage more dentists to use telemedicine in routine practice23. For effective operation of teledentistry, adequate training of all participants including all oral health professionals at remote site and the distant specialist is crucial because it based on information technology. A potential challenge might be the initial cost involved in training personnel and acquiring the appropriate equipment and facilities to kick-start the programme and continuous costs for maintenance. However, the store and forward technology provides excellent results without excessive costs for equipment or connectivity4. A typical store and forward teledentistry system consists of a computer with substantial hard drive memory, adequate RAM, a speedy processor, an intraoral video camera, a digital camera, a modem and an internet connection11. Internet access necessary for the exchange of data in remote areas might also pose a challenge to the effective delivery of teledentistry in some developing countries. Efforts should be made to provide internet access because it remains the cornerstone of modern teledentistry. Concerns about the confidentiality of dental information arise from the transfer of medical histories and records as well as from general security issues of electronic information stored in computers55. If the practice of teledentistry is adopted in developing countries, practitioners should be aware of ethical and legal issues regarding its use. Utmost care to ensure that patient privacy is not compromised by unauthorised persons should put in place. Patients should be informed that their information is to be transmitted electronically and the possibility exists that the information will be intercepted despite maximum efforts to maintain security14. Informed consent that covers everything that exists in a standard consent form should obtained4.
Successful teledentistry programme would reduce the number of referrals to the specialists thus reducing the remuneration of participating consultants. Therefore, a balance must be found between the remuneration for teleconsultation and one on one consultation in their respective dental clinics. If government provide the required funding and enabling environment these challenges can be ameliorated. Empirical research is needed to establish the evidence base to support teledentistry practice in developing countries.
CONCLUSION
With its numerous benefits, incorporating teledentistry into the existing practice will go a long way in enhancing the standard of oral health care delivery to inhabitants of remote communities in developing countries if the attending problems and challenges of teledentistry are overcome. However, with the potential challenges discussed, there is the need to conduct pilot projects as these will provide better insight on the feasibility, acceptability and ultimately overall success of teledentistry in these communities.
REFERENCES
- 1.Norris C. Essentials of telemedicine and telecare. 2001;1:2–4. [Google Scholar]
- 2.Lehoux P, Sicotte C, Denis J, Berg M, Lacroix A. The theory of use behind telemedicine. SocSci Med. 2002;54:889–904. doi: 10.1016/s0277-9536(01)00063-6. [DOI] [PubMed] [Google Scholar]
- 3.Zundel M. Telemedicine: history, applications, andimpact on librarianship. Bull Med Libr Assoc. 1996;84(1):71–79. [PMC free article] [PubMed] [Google Scholar]
- 4.Jampani ND, Nutalapati BS, Dontula BSK, Boyapati R. Applications of teledentistry: A literature review and update. J IntSocPrev Community Dent . 2011;1(2):37–44. doi: 10.4103/2231-0762.97695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marescaux J, Leroy J, Rubino F, et al. Transcontinental Robot-Assisted Remote Telesurgery: Feasibility and potential applications. Annals of Surgery. 2002;235(4):487–492. doi: 10.1097/00000658-200204000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mihailovic B, Miladinovic M, Vujicic B. Telemedicine in Dentistry (Teledentistry) In: Graschew G, Roelofs TA, editors. Advances in Telemedicine: Applications in Various Medical Disciplines and Geographical Areas 2011. Rijeka (Croatia): InTech; 2011. pp. 215–230. [Google Scholar]
- 7.Sanchez E, et al. Teledentistry in the United States: a new horizon of dental care. International Journal of Dental Hygiene. 2004;2(4):161–164. doi: 10.1111/j.1601-5037.2004.00093.x. [DOI] [PubMed] [Google Scholar]
- 8.Fricton J, Chen H. Using teledentistry to improve access todental care for the underserved. Dental Clinics of North America . 2009;53(3):537–548. doi: 10.1016/j.cden.2009.03.005. [DOI] [PubMed] [Google Scholar]
- 9.Chen JW, Hobdell MH, Dunn K, et al. Teledentistry and its use in dental education. J Am Dent Assoc . 2003;134(3):342–346. doi: 10.14219/jada.archive.2003.0164. [DOI] [PubMed] [Google Scholar]
- 10.Birnbach JM. The Future of Teledentistry. J Calif Dent Assoc. 2000;28:141–143. [PubMed] [Google Scholar]
- 11.Bhambal A, Saxena S, Balsaraf SV. Teledentistry: Potentials Unexplored. J Int Oral Health. 2010;2:1–6. [Google Scholar]
- 12.Folke LE. Teledentistry: An Overview. Tex Dent J. 2001;118:10–18. [PubMed] [Google Scholar]
- 13.Weerasinghe JU. Clinical trials on computer based telemedicine – A systematic review. Sri Lankan J Bio-med Inform . 2010;1:12–20. [Google Scholar]
- 14.Chang SU, Plotkin DR, Mulligan R, et al. Teledentistry in Rural California-A USC Initiative. CDA J. 2003;31:601–608. [PubMed] [Google Scholar]
- 15.Golder D, Brennan K. Practicing dentistry in the age of telemedicine. J Am Dent Assoc. 2000;131(6):734–744. doi: 10.14219/jada.archive.2000.0272. [DOI] [PubMed] [Google Scholar]
- 16.Bradley M, Black P, Noble S, et al. Application of Teledentistry in Oral Medicine in a Community Dental Service, N. Ireland. Br Dent J. 2010;209:399–404. doi: 10.1038/sj.bdj.2010.928. [DOI] [PubMed] [Google Scholar]
- 17.Torres-Pereira C, Possebon RS, Simoes A, et al. Email for Distance Diagnosis of Oral Diseases- A Preliminary Study of Teledentistry. J Telemed Telecare. 2008;14:435–438. doi: 10.1258/jtt.2008.080510. [DOI] [PubMed] [Google Scholar]
- 18.Summerfelt FF. Teledentistry-assisted, affiliated practice for dental hygienists: An innovative workforce model. J Dent Educ. 2011;75:733–742. [PubMed] [Google Scholar]
- 19.de Almeida GR, de Lucas Rezende LVM, da-Silva CQ, Almeida JCF. Remote diagnosis of traumatic dental injuries using digital photographs captured via a mobile phone. Dent Traimatol . 2017;33(5):350–357. doi: 10.1111/edt.12347. [DOI] [PubMed] [Google Scholar]
- 20.Pentapati KC, Mishra P, Damania M, et al. Reliability of intra-oral camera using teledentistry in screening of oral diseases – Pilot study Saudi. Dent J . 2017;29(2):74–77. doi: 10.1016/j.sdentj.2017.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Estai M, Kanagasingam Y, Huang B, et al. 2017. Comparison of a smartphone - based photographic method with face-to-face caries assessment: A mobile teledentistry model. Telemed J E Health . 2017;23(5):435–440. doi: 10.1089/tmj.2016.0122. [DOI] [PubMed] [Google Scholar]
- 22.Queyroux A, Saricassapian B, Herzog D, et al. Accuracy of teledentistry for diagnosing dental pathology using direct examination as a Gold Standard; Results of the Tel-e-dent study of older adults living in nursing homes. J Am Med Dir Assoc. 2017;18(6):528–532. doi: 10.1016/j.jamda.2016.12.082. [DOI] [PubMed] [Google Scholar]
- 23.Estai M, Kanagasingam Y, Xiao D, et al. A proofof- concept evaluation of a cloud-based store-andforward telemedicine app for screening oral diseases. J Telemed Telecare. 2016;22(6):319–325. doi: 10.1177/1357633X15604554. [DOI] [PubMed] [Google Scholar]
- 24.Brullmann D, Schmidtmann I, Warzecha K, D'Hoedt B. Recognition of root canal orifices at a distance – a preliminary study of teledentistry. J Telemed Telecare . 2011;17(3):154–157. doi: 10.1258/jtt.2010.100507. [DOI] [PubMed] [Google Scholar]
- 25.Zivkovic D, Tosic G, Mihailovic B, et al. Diagnosis of periapical lesions of the front teeth using the internet. PONS Med J. 2010;7:138–143. [Google Scholar]
- 26.Ignatius E, Perala S, Makela K. Use of videoconferencing for consultation in Dental Prosthetics and oral rehabilitation. J Telemed Telecare . 2010;16:467–470. doi: 10.1258/jtt.2010.100303. [DOI] [PubMed] [Google Scholar]
- 27.Rocca MA, Kudryk VL, Pajak JC, Morris T. The evolution of a teledentistry system within the Department of Defense. Proc AMIA Symp . 1999. pp. 921–924. [PMC free article] [PubMed]
- 28.Rollet MK, Strauss RA, Abubakar AO, Hampton C. Telemedicine consultations in Oral and Maxillofacial Surgery. J Oral Maxillofac Surg. 1999;57:136–138. doi: 10.1016/s0278-2391(99)90226-4. [DOI] [PubMed] [Google Scholar]
- 29.Duka M, Mihailovic B, Miladinovic M, et al. Evaluation of Telemedicine systems for impacted third molars diagnosis. Vojnosanit Pregl . 2009;66:985–991. doi: 10.2298/vsp0912985d. [DOI] [PubMed] [Google Scholar]
- 30.Herce J, Lozano R, Salazar CI, et al. 2011. Management of impacted Molars based on telemedicine: A pilot study . Journal of Oral and Maxillofacial Surgery . 2011;69(2):471–475. doi: 10.1016/j.joms.2010.09.004. [DOI] [PubMed] [Google Scholar]
- 31.Brickley M. Oral Surgery: The Referral system and Telemedicine. Br Dent J . 2000;188:384. doi: 10.1038/sj.bdj.4800491. [DOI] [PubMed] [Google Scholar]
- 32.Aziz SR, Ziccardi VB. Telemedicine using smart phones for oral and maxillofacial surgery consultation, communication and treatment planning. J Oral Maxillofacial Surg . 2009;67:2505–2509. doi: 10.1016/j.joms.2009.03.015. [DOI] [PubMed] [Google Scholar]
- 33.Mandall NA, O'Brien KD, Brady J, et al. Teledentistry for screening new patient orthodontic referrals. Part 1 A randomised controlled trial. Br Dent J . 2005;199(10):659–662. doi: 10.1038/sj.bdj.4812930. [DOI] [PubMed] [Google Scholar]
- 34.Berndt J, Leone P, King G. Using Teledentistry to Provide Interceptive Orthodontic Services to Disadvantaged Children. Am J Orthod Dentofac Orthop. 2008;134:700–706. doi: 10.1016/j.ajodo.2007.12.023. [DOI] [PubMed] [Google Scholar]
- 35.Favero L, Pavan L, Arreghini A. Communication through telemedicine: Home telleassistance in orthodontics . Eur J Paediatric Dent . 2009;10:162–167. [PubMed] [Google Scholar]
- 36.Stephens CD, Cook J. Attitudes of UK consultants to teledentistry as a means of providing orthodontic advice to dental practitioners and their parents . J Orthod . 2002;29:137–142. doi: 10.1093/ortho/29.2.137. [DOI] [PubMed] [Google Scholar]
- 37.Cook J, Edwards J, Mullings C, Stephens C. Dentists' opinions of an online orthodontic advice service. J Telemed Telecare . 2001;7:334–337. doi: 10.1258/1357633011936967. [DOI] [PubMed] [Google Scholar]
- 38.Kopycka-Kedzierawski DT, Billings RJ, McConnochie KM. Dental screening of preschool children using teledentistry: a feasibility study. Peadiatr Dent . 2007;293:209–213. [PubMed] [Google Scholar]
- 39.Kopycka-Kedzierawski DT, Billings RJ. Teledentistry in inner-city child-care centres. J Telemed Telecare . 2006;12(4):176–181. doi: 10.1258/135763306777488744. [DOI] [PubMed] [Google Scholar]
- 40.Amavel R, Cruz-Correia R, Frias-Bulhosa J. Remote diagnosis of children dental problems based on non-invasive photographs: A valid proceeding . In: Adlassing KP, Blobel B, Mantas J, Masic I, editors. Medical Informatics in a United and healthy Europe 2009. Amsterdam (Netherlands): IOS Press; 2009. pp. 458–462. [PubMed] [Google Scholar]
- 41.Marino R, Ghanim A. Teledentistry: a systematic review of the literature. J Telemed Telecare . 2013;19(4):179–183. doi: 10.1177/1357633x13479704. [DOI] [PubMed] [Google Scholar]
- 42.Tani Botticelli A, Schittek JM, Botticelli D, et al. The effectiveness of video support in the teaching of manual skills related to initial periodontal therapy tested on phantoms. Int J Comput Dent. 2005;8(2): 117–127. [PubMed] [Google Scholar]
- 43.Ewers R, Schicho K, Wagner A, et al. Seven years of clinical experience with teleconsultation in craniomaxillo-facial Surgery. J Oral Max Surg. 2005;63(10): 1447–1454. doi: 10.1016/j.joms.2005.06.020. [DOI] [PubMed] [Google Scholar]
- 44.Lang WP. An application of computer conferencing in dental education . Int J Biomed Computb . 1992;31(3-4):221–231. doi: 10.1016/0020-7101(92)90006-e. [DOI] [PubMed] [Google Scholar]
- 45.Mattheos N, Nattestad A, Attstrom R. Feasibility of and satisfaction with the use of low-bandwidth videoconferencing for examination of undergraduate students. J Telemed Telecare. 2003;9(5):278–281. doi: 10.1258/135763303769211292. [DOI] [PubMed] [Google Scholar]
- 46.Meckfersel S, Stuhmer C, Bormann KH, et al. Introduction of e-learning in dental radiology reveals significantly improved results in final examination. J CraniomaxillofacSurg. 2011;39(1):40–48. doi: 10.1016/j.jcms.2010.03.008. [DOI] [PubMed] [Google Scholar]
- 47.Bednar ED, Hannum WM, Firestone A, et al. Application of distance learning to interactive seminar instruction in orthodontic residency programs. Am J Orthod Dentofacial Orthop. 2007;132(5):586–594. doi: 10.1016/j.ajodo.2007.06.008. [DOI] [PubMed] [Google Scholar]
- 48.Miller KT, Hannum WM, Proffit WR. Recorded interactive seminars and follow-up discussions as an effective method for distance learning. Am J Orthod Dentofacial Orthop . 2011;139930:412– 416. doi: 10.1016/j.ajodo.2010.12.013. [DOI] [PubMed] [Google Scholar]
- 49.Whitten Pamela, Mair FS, Hellmich S, et al. Systematic review of cost effectiveness studies of telemedicine inter ventions. BMJ. 2002;324(7351):1434–1437. doi: 10.1136/bmj.324.7351.1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Scuffham PA, Steed M. An economic evaluation of the highlands and islands teledentistry project. J Telemed Telecare . 2002;8(3):165–177. doi: 10.1177/1357633X0200800307. [DOI] [PubMed] [Google Scholar]
- 51.Reddy K. Using teledentistry for providing the specialist access to rural Indians. Indian J Dent Res. 2011;22:189. doi: 10.4103/0970-9290.84275. [DOI] [PubMed] [Google Scholar]
- 52.Elmokadem MSE. Applications of telemedicine in dentistry. Review of literature. 2013. Mater's Theses in Telemedicine and e-health. University of Tromso.
- 53.Kirshner M. The role of information technology and informatics research in the dentist-patient relationship . Adv Dent Res. 20003;17:77–81. doi: 10.1177/154407370301700118. [DOI] [PubMed] [Google Scholar]
- 54.Boringi M, Waghrav S, Lavanya R, et al. Knowledge and awareness of teledentistry among dental professional – A cross Sectional Study. J Clin Diagn Res . 2015;9(8): ZC41–44. doi: 10.7860/JCDR/2015/13303.6320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sfikas PM. Teledentistry – Legal and Regulatory issues explored. J Am Dent Assoc . 1997;128:1716–1718. doi: 10.14219/jada.archive.1997.0137. [DOI] [PubMed] [Google Scholar]


