Abstract
Diagnosing the affected side in Benign Paroxysmal Positional Vertigo (BPPV) involving the Lateral Semicircular Canal (LSC) is often challenging and uncomfortable in patients with recent onset of vertigo and intense autonomic symptoms. The Minimum Stimulus Strategy (MSS) aims to diagnose side and canal involved by BPPV causing as little discomfort as possible to the patient. The strategy applied for LSC-BPPV includes the evaluation of pseudo-spontaneous nystagmus and oculomotor responses to the Head Pitch Test (HPT) in upright position, to the seated-supine test and to the Head Yaw Test (HYT) while supine. Matching data obtained by these tests enables clinicians to diagnose the affected side in LSC-BPPV. The purpose of this preliminary study is to propose a new diagnostic test for LSC-BPPV complimentary to the HPT, the Upright Head Roll Test (UHRT), to easily determine the affected ear and the involved arm in the sitting position and to evaluate its efficiency. Our results suggest that the UHRT can increase the sensitivity of the MSS without resorting to the HYT, thus reducing patient’s discomfort.
Key words: benign paroxysmal positional vertigo, lateral semicircular canal, horizontal semicircular canal, minimum stimulus strategy, head roll test
Introduction
Benign paroxysmal positional vertigo (BPPV) involving the lateral semicircular canal (LSC) is characterized by positional vertigo and direction-changing horizontal nystagmus while turning the head to either side while supine.1,2 It represents the second most common type of BPPV, accounting for less than 15% of all BPPV cases.3
The pathophysiological mechanisms proposed to explain LSC-BPPV are canalolithiasis and cupulolithiasis. According to the first theory, free-floating otoliths inside the involved canal modify cupula sensitivity to accelerations, whereas in cupulolithiasis debris attached to the cupula overload the cupula itself altering its sensitivity to gravity.4-7 In both cases, the cupula becomes sensitive to linear accelerations such as gravity and any linear vectorial component induced by brisk head movements aligning with the plane of the involved canal.
Depending on the direction of nystagmus evoked by the Head Yaw Test (HYT) while supine (also known as supine head roll test or McClure-Pagnini maneuver), 2,4 two variants of LSC-BPPV are distinguished. In geotropic forms, paroxysmal nystagmus beats towards the undermost ear in both sides since otoliths lay within the non-ampullary arm of the LSC and move towards the ampulla, thus exciting the ampullary receptor.4,5 Conversely, in apogeotropic variants particles either settle in the ampullary arm of the canal or adhere to the cupola resulting in paroxysmal or persistent nystagmus, respectively, beating towards the uppermost ear as endolymphatic displacement is ampullifugal, inhibiting the afferent resting firing rate.4,5,8
The identification of the affected ear and the involved arm is pivotal for successful repositioning. The first clinical sign described to diagnose the affected side was nystagmus amplitude evoked by the HYT. The patient’s head is rotated about 90° on one side in supine position and then to the opposite side of 180°. Finally, the head is rotated again of 180° to the first side examined.1,2,9,10 According to Ewald’s second law, an excitatory stimulus results in a more intense response than an inhibitory input.11 Therefore, in geotropic variants the affected side is the one on which nystagmus is more intense, whereas in apogeotropic forms the nystagmus amplitude is greater with the healthy side down.1-8,12 Nevertheless, diagnosing the affected ear only relying on the comparison of nystagmus evoked by the HYT can be challenging, as it is sometimes difficult to visually discern differences in amplitude and intensity of eye movements.13,14 Moreover, repeating diagnostic maneuvers can frequently provoke discomfort in patients with recent onset BPPV and intense autonomic symptoms, especially in phobic and anxious subjects.12,13 Therefore, additional diagnostic tests exploiting minimal head movements would be of extreme help, especially in acute settings.
Other clinical signs to diagnose the affected side in LSC-BPPV have already been described and systematized into a decision-making algorithm known as Minimum Stimulus Strategy (MSS)15 that aims to study the behavior of nystagmus as a function of head position in space, sparing the patients troublesome symptoms. MSS test battery needs to be performed with the aid of Video-Frenzel goggles, monitoring plane and direction of eye movements, in order to figure out where otoliths are located following a nystagmus- guided approach.16 The first step includes the evaluation of Pseudo-Spontaneous Nystagmus (PSN) and nystagmic responses to the Head Pitch Test (HPT).15,17,18 Both tests are performed in the sitting position. Horizontal PSN is commonly detected in patients with LSC-BPPV as lateral canal acts as an inclined surface drawing a 30° front-open-angle with the horizontal plane allowing freefloating particles to gravitate along the canal in canalolithiasis or resulting in a persistent displacement of the overloaded cupula in case of cupulolithiasis. Therefore, PSN is generally directed to the healthy side in geotropic LSC-BPPV since debris floats away from the ampulla and beats to the affected side in apogeotropic forms where otoliths gravitate in the opposite direction.13,15,17 PSN is not a direction-fixed nystagmus as it may change according to the head-bending angle. The HPT, also known as bow-and-lean test or head-bending test, consists in changing the angle between LSC and the horizontal plane by tilting the patient’s head forward and backward. 17-19 Bending the head backward increases the abovementioned angle, thus enhancing PSN intensity, if present, or eliciting a nystagmus beating towards the healthy side in geotropic forms of LSC-BPPV or towards the affected side in the apogeotropic variants. Conversely, PSN decreases by bending the head forward, until reaching the so-called null-point, in which LSC aligns with the horizontal plane.12,17,19 At the null point, canaliths no longer move into the canal lumen or overloaded cupula cannot deflect and PSN ceases. Then, tilting the head further forward, beyond the null-point, PSN reverses. If PSN is not present, bending the patient’s head forward should elicit a nystagmus beating towards the affected side in geotropic forms or towards the heathy side in apogeotropic variants.
The second step of MSS is the Seated-Supine Test (SST), also known as lying-down test, which is performed by bringing the patient down from the sitting to the supine position7,20. In LSCBPPV, the SST evokes a nystagmus beating toward the unaffected ear in geotropic variants and toward the affected ear in apogeotropic forms.7,12,15,17,20,21 Finally, the third step of MSS consists in the HYT, as described above.1,2,4 The MSS algorithm is schematized in Figure 1. In the light of all the above, matching data acquired in the upright position with those obtained with the SST and the HYT while supine enables clinicians to properly diagnose the affected side in LSC-BPPV and treat the patient accordingly. The purpose of this preliminary study is to propose a new diagnostic test complimentary to the HPT, the Upright Head Roll Test (UHRT), to easily determine the affected ear and the involved arm in LSC-BPPV in the sitting position and evaluate its efficiency. Thanks to this minimum stimulus algorithm, the patient can immediately receive the proper physical treatment from the sitting position, avoiding disturbing symptoms related to the supine positioning.
Materials and Methods
Twelve consecutive patients (5 male, 7 females, mean age. 56.3 ± 11.2 years, range age: 35 – 83 years) diagnosed with LSCBPPV at different onset time at our institutions from May to July 2019 were enrolled in this preliminary study. All of them were evaluated with video-Frenzel goggles. All patients received a 5- steps diagnostic test battery according to the following order: i) PSN evaluation; ii) HPT; iii) UHRT; iv) SST; v) HYT. The aim of this report is to evaluate whether a proper diagnosis of LSC-BPPV could be achieved maintaining the patient in the sitting position with the sole PSN, HPT and UHRT, thus avoiding both SST and HYT and related patient’s discomfort.
Upright Head Roll Test (UHRT)
The three degrees of freedom of the human head can be described by rotation angles around the X (roll), Y (pitch) and Z (yaw) axes, perpendicular to the coronal, sagittal and transverse planes, respectively, with the origin located at the intersection of the mid-sagittal plane and the inter-ocular axis (the nasion) (Figure 2): i) Head movements in the yaw plane (i.e. around the vertical, rostral-caudal, yaw or z-axis) are horizontal; ii) Head movements in the pitch plane (i.e. around the horizontal, inter-aural, pitch or yaxis) are vertical; iii) Head movements in the roll plane (i.e. around the longitudinal, naso-occipital, roll or x-axis) are torsional.
We propose a new diagnostic maneuver for LSC-BPPV exploiting head rotations in the roll plane with the patient in the sitting position: the Upright Head Roll Test (UHRT) (Figure 3).
Figure 1.
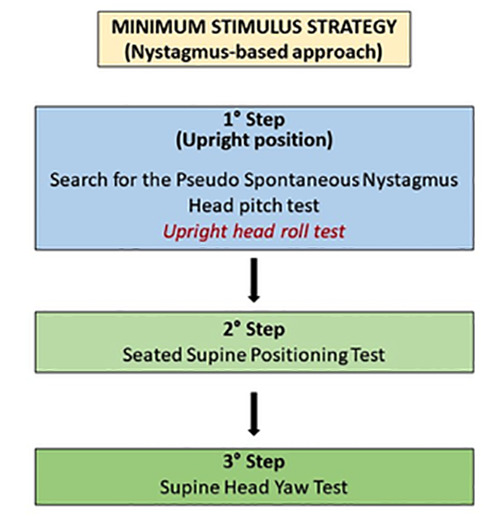
Minimum Stimulus Strategy to diagnose all type of benign paroxysmal positional vertigo.
Figure 2.
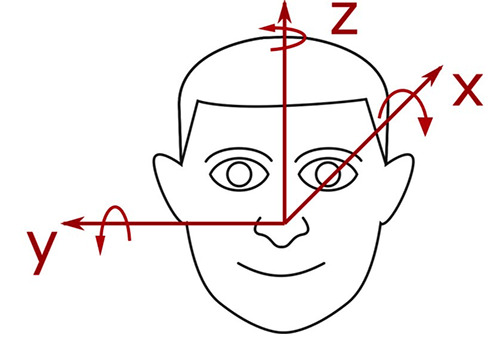
Orientation of the head in terms of pitch, roll, and yaw movements describing the three degrees of freedom of a human head.
The UHRT is performed with the patient in the sitting position, once both PSN and HPT have been evaluated. First, the head of the patient is slowly bent about 30° laterally toward one side, in the roll plane, bringing patient’s ear closer to his shoulder on the same side. The head is held still in this position for at least 30 seconds to allow the gravity vector to move debris within the membranous duct. Once horizontal nystagmus (either geotropic or apogeotropic) has been elicited, the head is slowly brought back in the center and held upright for additional 30 seconds to allow resulting endolymphatic flows to restore. Then, the same maneuver is performed toward the contralateral side to check if resulting nystagmus beats in the opposite direction to that previously assessed (i.e. if right-sided UHRT elicits a right-beating geotropic nystagmus, a geotropic nystagmus toward the left side should be observed at the UHRT on the left and vice versa for apogeotropic nystagmus). Examiner should not pay attention to compare the intensity of nystagmus between the two sides, but its direction should be uniquely evaluated. Normally, no head accelerations need to be imparted since this test exploits mainly gravitational vector and inertial forces are not needed to induce endolymphatic flows.
LSC-BPPV treatment
All patients were treated with specific Canalith Repositioning Maneuvers (CRM) for LSC-BPPV. Patients with geotropic variants directly received CRM towards the healthy side as proposed by Gufoni22,23 and were instructed to lay on the healthy side according to the forced prolonged position24 for the following 48-72 hours. Subjects presenting with apogeotropic nystagmus were first treated either with the maneuver proposed by Ciniglio-Appiani towards the impaired side25 or with the prolonged position on the affected side until the following evaluation, 26 in order to convert nystagmus in geotropic type (consistently with otoconial progression toward the non-ampullary arm of LSC). Once ensured nystagmus conversion with the HYT, patients received Gufoni CRM towards the unaffected side and were suggested to lay on the same side for the following 3 days. Therefore, at the end of each specific physical treatment, all patients were checked after 72 hours with the HYT to ensure resolution of BPPV symptoms and signs.
Results
In Table 1 our findings are summarized.
Seven patients were affected by geotropic variant of LSCBPPV (5 on the right and 2 on the left side), whereas in five patient an apogeotropic LSC canalolithiasis was diagnosed (3 right-sided and 2 left-sided).
Figure 3.
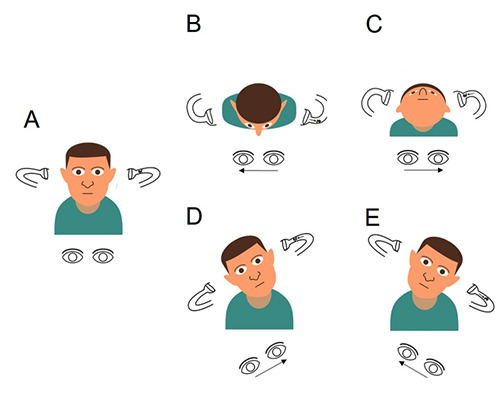
Schematic representation of diagnostic tests in upright position by taking as an example the clinical case of patient n.11 presenting with benign paroxysmal positional vertigo (BPPV) involving the ampullary arm of the left lateral semicircular canal (LSC) (left apogeotropic LSC-BPPV). Arrows within the canal represent the direction of endolymphatic flows, whereas arrows beneath the eyes represent the direction of the fast phase of nystagmus. A) Pseudo Spontaneous Nystagmus: absent. B) Head Pitch Test (HPT) with forward head bending eliciting right-beating nystagmus due to debris moving away from left LSC ampulla. C) HPT with backward head bending evoking ampullifugal endolymphatic flows, thus resulting in left-beating nystagmus. D) Upright Head Roll Test (UHRT) with rightward head tilting eliciting left-beating apogeotropic nystagmus as particles floats toward left LSC ampulla. E) UHRT with leftward head tilting generating right-beating apogeotropic nystagmus due to otoliths shifting away from left LSC ampulla.
Table 1.
Demographic and clinical records of patients enrolled in this preliminary study.
| Patient | Age | Sex | PSN | HPT-F | HPT-B | UHRT-R | UHRT-L | SST | HYT | Side and LSC arm involved | Onset time |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 55 | F | L | R | L | L | R | No | A-N | L-amp | 2-7 d |
| 2 | 60 | M | No | L | R | No | L | R | G-L | L-non-amp | > 7 d |
| 3 | 58 | M | L | R | L | R | L | L | G-R | R-non-amp | < 2 d |
| 4 | 50 | F | L | L | R | L | R | No | A-N | R-amp | 2-7 d |
| 5 | 52 | F | R | L | R | L | R | R | A-L | R-amp | < 2 d |
| 6 | 50 | F | No | L | R | R | L | R | G-L | L-non-amp | 2-7 d |
| 7 | 60 | F | L | R | L | R | L | L | G-R | R-non-amp | < 2 d |
| 8 | 35 | M | No | No | L | R | L | L | G-R | R-non-amp | > 7 d |
| 9 | 60 | M | R | R | L | R | L | L | G-R | R-non-amp | 2-7 d |
| 10 | 50 | F | No | L | R | L | R | No | A-N | R-amp | > 7 d |
| 11 | 62 | F | No | R | L | L | R | L | A-R | L-amp | > 7 d |
| 12 | 83 | M | No | R | No | R | L | L | G-R | R-non-amp | > 7 d |
A-L: apogeotropic nystagmus, more intense on the left side; A-N: apogeotropic nystagmus, no differences in intensity between right and left side; A-R: apogeotropic nystagmus, more intense on the right side; d: day(s); F: female; G-L : geotropic nystagmus; more intense on the left side; G-N: geotropic nystagmus; no differences in intensity between right and left side; G-R : geotropic nystagmus, more intense on the right side; HPTB: head pitch test backward; HPT-F: head pitch test forward; HYT: head yaw test; L: left-beating nystagmus; L-amp: ampullary arm of the left canal; L-non-amp: non-ampullary arm of the left canal; LSC: lateral semicircular canal; M: male; No: no nystagmus; PSN: pseudo-spontaneous nystagmus; R: right-beating nystagmus; R-amp: ampullary arm of the right canal; R-non-amp: non-ampullary arm of the right canal; SST: seated-supine test, UHRT-L: Upright Head Roll Test on the left side; UHRT-R: Upright Head Roll Test on the right side.
PSN could be detected in 6 patients (50% of cases, 3 with apogeotropic LSC-BPPV, 3 with geotropic form) and only in 4 of them it was directed toward the same side of the head pitch nystagmus with the head bent backward and in 3 of them it was in accordance with the SST nystagmus.
HPT elicited a direction-changing horizontal nystagmus with either head bending in 10 patients (83.3% of cases), whereas in two cases (both geotropic) it was incomplete, resulting in detectable nystagmus only with the head bent backward in a case and in forward head bending in another case.
SST evoked a horizontal nystagmus in 9 cases (75% of cases, all 7 geotropic forms and 2 apogeotropic variants). The direction of nystagmus always matched that in backward head bending at the HPT, except for a geotropic case lacking of detectable nystagmus in this latter position.
In all patients, the HYT elicited a direction-changing positional nystagmus to either side. Nevertheless, only 9 patients (75% of cases) exhibited difference in nystagmus amplitude between the two sides, whereas 3 patients affected by apogeotropic LSC-BPPV did not show asymmetric responses. Curiously, these 3 patients were those who did not exhibit nystagmus at the SST and one of them also lacked of PSN. In these cases, a proper diagnosis of side involvement could be achieved only by matching data from HYT and HPT. UHRT elicited a direction-changing positional nystagmus on either side in all patients, except for a case of geotropic canalolithiasis in which it was incomplete, eliciting nystagmus only by one positioning. The same patient did not show any PSN whereas both HPT and SST were positive and resulting data were in accordance. In all cases, the direction of nystagmus induced by the UHRT on either side matched that generated by the HYT.
Therefore, if the percentage of correct diagnosis made by matching data from all five tests (SPN + HPT + UHRT + SST + HYT) is compared with that achieved resorting only to diagnostic tests in the sitting position (SPN + HPT + UHRT), the same results are obtained as both test battery reached 100% of diagnostic accuracy. In other words, in our series the diagnosis of geotropic or apogeotropic variants of LSC-BPPV, as well as the identification of the affected side, could be obtained in the sitting position only by basing on upright diagnostic tests.
On the contrary, the percentage of proper diagnosis of side involvement only relying on diagnostic tests in the supine position was 75% as 3 patients neither exhibit difference in nystagmus amplitude at the HYT nor showed nystagmus at the SST.
As regards different onset times, 3 patients were diagnosed with LSC-BPPV within the first 48 hours (acute stage), 4 patients were evaluated between 2 days and one week from the onset of symptoms (sub-acute group) and 5 patients were evaluated after 1 week (post-acute group). Each diagnostic test elicited a clear nystagmus in all subjects in acute stage. All six patients lacking in PSN were in sub-acute or post-acute stage (1 case and 5 cases, respectively) and the 3 patients with negative SST and symmetric nystagmic responses to the HYT where either in sub-acute (2 cases) or in post-acute stage (1 case). Similarly, time between the onset of symptoms and the evaluation in subjects presenting with either incomplete HPT or incomplete UHRT was more than a week in all cases.
All patients were then successfully treated with the aforementioned physical therapy and all of them were symptoms free at the last clinical evaluation.
Discussion
The diagnosis of LSC-BPPV is traditionally entrusted to the HYT performed in the supine position, which allows to identify the form (geotropic or apogeotropic) and the affected side.1,4 The diagnosis of the involved ear relies on Ewald’s second law, saying that ampullipetal endolymphatic flows produce stronger responses than ampullifugal flows in LSC.11 Unfortunately, it may be sometimes difficult to determine the affected ear in LSC-BPPV using Ewald’s second law in clinical practice, that is comparing maximum slow phase velocity of nystagmus and symptoms between each side. In fact, intensity and amplitude of eye movements are not always so distinctly different between the two sides, especially in apogeotropic variants.13 On the other hand, repeating several times the HYT to confirm the diagnosis may result in impaired paroxysmal nystagmus due to a fatigue response27 and in significant discomfort to patients with acute vertigo and intense autonomic symptoms and/or in anxious subjects.12,15
A series of clinical signs integrating those obtained with the HYT, thus facilitating the identification of the affected side, have already been described in literature. The so-called “secondary signs of lateralization”13 include the PSN, the direction-changing nystagmus evoked by the HPT and the nystagmus provoked by the SST.12,13,15-21,28-32
PSN and the HPT are evaluated in upright position using Video-Frenzel goggles. Although data obtained by these tests do not allow clinicians to fully identify which LSC and canal arm is involved by lithiasis, diagnostic hypotheses are nevertheless reduced to only two options. Taking a hypothetical case with positional vertigo as a practical example, we can imagine to evaluate a patient in upright position presenting with left-beating horizontal PSN. Moreover, whereas at the HPT in backward bending PSN increases, by bending patient’s head forward it first progressively recedes and then reverses becoming right-beating. In a case like this, only two options are possible: i) The patient is affected by right geotropic LSC-BPPV, ii) The patient is affected by left apogeotropic LSC-BPPV.
The proposed diagnostic maneuver UHRT aims to solve these doubts by simply tilting the patient’s head sideways along the roll plane and observing the direction of nystagmus (geotropism). Taking the above-mentioned example, if tilting the head towards the right a left-beating nystagmus (apogeotropic) is elicited, we could identify debris within the ampullary arm of the left LSC and diagnose a left apogeotropic LSC-BPPV. We could also tilt the patient’s head towards the contralateral side to observe, again, an apogeotropic nystagmus (right-beating), confirming our diagnostic hypothesis. On the contrary, if we elicit bilaterally a geotropic nystagmus with the UHRT on either side, we could figure out that otoliths settle in the non-ampullary arm of the right LSC, thus diagnosing right geotropic LSC-BPPV. In order to facilitate the comprehension of the mechanism by which both the HPT and UHRT move debris along the LSC, a video showing video-oculographic findings in patient n.11 with schematic drawings depicting patient’s head, particles and their movements within the involved LSC is proposed (Video 1: Video-oculographic findings in patient n.11 presenting with Benign Paroxysmal Positional Vertigo (BPPV) involving the ampullary arm of the left Lateral Semicircular Canal (LSC) (left apogeotropic LSC-BPPV). In the lower-right quadrant, step-by-step schematic drawings depict patient’s head, particles and their movements within the involved LSC. Arrows within the canal represent the direction of endolymphatic flows, whereas arrows beneath the eyes represent the direction of the fast phase of nystagmus).
In this preliminary study, all reported tests were applied in each patient to identify the simplest way for an appropriate diagnosis of LSC-BPPV. According to our results, we could correctly identify the side and the canal arm involved by lithiasis in all cases by integrating results from the HPT with the UHRT, thus maintaining the patient upright without the need to perform the SST and the HYT. Therefore, the diagnostic approach based on the detection of nystagmus exclusively in upright position, in accordance with the MSS principles, showed the same maximal diagnostic sensitivity compared to the traditional approach.
The opportunity to diagnose LSC-BPPV only resorting to tests in upright position makes this diagnostic work-up less troublesome for patients, especially in the acute stage of the disease when they could be particularly susceptible to rotational movements and accelerations. Furthermore, this more comfortable protocol could also result in a less time-consuming management of LSC-BPPV as patients can directly receive appropriate CRM from the upright position, immediately after diagnosis. In fact, CRM proposed by Gufoni starts with the patient in the sitting position22,23 and diagnostic tests while supine are undue.
Although the UHRT is simple and easy to perform, it can be challenging in patients with a reduced cervical range of motion similarly to other therapeutic maneuvers for BPPV.33 Nevertheless, if patients exhibit difficulties to flex the head laterally due to neck stiffness, the whole trunk of the patient may be tilted about 30° toward both sides along the roll plane to attain the same head position with respect to gravity, keeping the diagnostic value of UHRT unchanged.
Both HPT and UHRT only employ inertia of debris moving along LSC. For this reason, they may evoke only impaired nystagmic responses, which can be preferably observed using video- Frenzel goggles. Furthermore, these tests may produce incomplete responses, as occurred in 3 patients of our series who presented at our attention more than 7 days form the onset of symptoms. Hence, tests sensitivity may decrease depending on the amount of time that has lapsed since the onset of BPPV, mainly because the otoconial mass may have dispersed in the meanwhile. In these cases, more than one sign may be lacking and UHRT sensitivity could be partially impaired. In case of lack of detectable nystagmus, however, clinicians may increase UHRT sensitivity imparting slight accelerations to the patient’s head by rotating it quickly from one side to the other in the roll plane. This way, inertial forces will likely help the gravity vector to generate endolymphatic flows, resulting in detectable nystagmus.
Another case in which the UHRT may theoretically lack to generate nystagmus could be whether the entire amount of debris stubbornly settle in the lumen portion exactly between the ampullary and the non-ampullary arm of the canal (genu of the membranous duct). In this condition, both gravity vector and imparted head accelerations in the roll plane would fail to move debris back-and-forth along the LSC, but they could at most shift otoliths transversely to the main canal diameter, without obtaining any endolymphatic flow capable of modifying ampullary receptors discharge. In these cases, it could be helpful to perform the UHRT with the head slightly bent backward or forward along the pitch plane in order to mobilize otoconia from the critical position.
Nevertheless, according to our findings, a proper diagnosis of LSC-BPPV could be achieved even with incomplete results at the HPT and UHRT. Therefore, in case of patient in acute stage with enhanced autonomic symptoms, clinicians may theoretically only resort on an incomplete HPT (i.e. performing the test either in backward or forward head hanging) and an incomplete UHRT (i.e. tilting the patient’s head only by one side) to properly diagnose side and canal arm involved and directly proceed to repositioning.
Conclusions
In conclusion, we propose a new diagnostic test (the UHRT) that integrates with the HPT within the decision-making algorithm to diagnose and treat LSC-BPPV aiming to cause as little discomfort as possible, thus improving the MSS. According to our findings, LSC-BPPV diagnosis can be obtained in the sitting position by only basing on upright diagnostic tests, sparing the patients unpleasant maneuvers while supine and allowing clinicians to proceed immediately to proper CRM. Nevertheless, a larger cohort of patients will be needed to evaluate the sensitivity of the UHRT combined with the HPT in detecting the involved side and the affected arm in LSC-BPPV.
Acknowledgments
The Authors would like to thank Mr. Livio Fania for the illustrations
References
- 1.Cipparrone L, Corridi G, Pagnini P. Cupulolitiasi. V Giornata Italiana di Nistagmografia Clinica. Nistagmografia e patologia vestibolare periferica. Milano: CSS Boots-Formenti; 1985. p. 36-53. [Google Scholar]
- 2.McClure A. Lateral canal BPV. Am J Otolaryngol 1985;14:30-5. [PubMed] [Google Scholar]
- 3.Cakir BO, Ercan I, Cakir ZA, et al. What is the true incidence of horizontal semicircular canal benign paroxysmal positional vertigo? Otolaryngol Head Neck Surg 2006;134:451-4. [DOI] [PubMed] [Google Scholar]
- 4.Pagnini P, Nuti D, Vannucchi P. Benign paroxysmal vertigo of the horizontal canal. ORL J Otorhinolaryngol Relat Spec 1989;51:161-70. [DOI] [PubMed] [Google Scholar]
- 5.Baloh RW, Jacobson KJ, Honrubia V. Horizontal semicircular canal variant of benign positional vertigo. Neurol 1993; 43:2542-9. [DOI] [PubMed] [Google Scholar]
- 6.Steddin S, Brandt T. Horizontal canal benign paroxysmal positioning vertigo (h-BPPV): transition of canalolithiasis to cupulolithiasis. Ann Neurol 1996;40:918–22. [DOI] [PubMed] [Google Scholar]
- 7.Nuti D, Vannucchi P, Pagnini P. Benign paroxysmal vertigo of the horizontal canal: a form of canalolithiasis with variable clinical features. J Vestib Res 1996;6:173-84. [PubMed] [Google Scholar]
- 8.Casani A, Vannucci G, Fattori B, Ghilardi PL. Positional vertigo and ageotropic bidirectional nystagmus. Laryngoscope 1997;107:807-13. [DOI] [PubMed] [Google Scholar]
- 9.von Brevern M, Bertholon P, Brandt T, et al. Benign paroxysmal positional vertigo: Diagnostic criteria Consensus document of the Committee for the Classification of Vestibular Disorders of the Bárány Society. Acta Otorrinolaringol Esp 2017;68:349-60. [DOI] [PubMed] [Google Scholar]
- 10.Bhattacharyya N, Gubbels SP, Schwartz SR, et al. Clinical Practice Guideline: Benign Paroxysmal Positional Vertigo (Update). Otolaryngol Head Neck Surg 2017;156:S1-S47. [DOI] [PubMed] [Google Scholar]
- 11.Ewald R. Physiologische Untersuchungen über das Endorgan des Nervous Octavus. Weisbaden: Bergmann, 1892. [Google Scholar]
- 12.Asprella Libonati G. Benign Paroxysmal Positional Vertigo and Positional Vertigo Variants. AIJOC 2012;4:25-40. [Google Scholar]
- 13.Califano L, Melillo MG, Mazzone S, Vassallo A. “Secondary signs of lateralization” in apogeotropic lateral canalolithiasis. Acta Otorhinolaryngol Ital 2010;30:78-86. [PMC free article] [PubMed] [Google Scholar]
- 14.Riga M, Korres S, Korres G, Danielides V. Apogeotropic variant of lateral semicircular canal benign paroxysmal positional vertigo: is there a correlation between clinical findings, underlying pathophysiologic mechanisms and the effectiveness of repositioning maneuvers? Otol Neurotol 2013; 34:1155-64. [DOI] [PubMed] [Google Scholar]
- 15.Asprella Libonati G. Diagnostic and treatment strategy of lateral semicircular canal canalolithiasis. Acta Otorhinolaryngol Ital 2005;25:277-83. [PMC free article] [PubMed] [Google Scholar]
- 16.Asprella Libonati G, Gagliardi G, Cifarelli D, et al. “Step by step” treatment of lateral semicircular canal canalolithiasis under videonystagmoscopic examination. Acta Otorhinolaryngol Ital 2003;23:10-5. [PubMed] [Google Scholar]
- 17.Asprella Libonati G. Pseudo-spontaneous nystagmus: a new sign to diagnose the affected side in lateral semicircular canal benign paroxysmal positional vertigo. Acta Otorhinolaryngol Ital 2008;28:73-8. [PMC free article] [PubMed] [Google Scholar]
- 18.Choung Y-H, Shin YR, Kahng H, et al. “Bow and Lean test” to determine the affected ear of horizontal canal benign paroxysmal positional vertigo. Laryngoscope 2006;116:1776-81. [DOI] [PubMed] [Google Scholar]
- 19.Bisdorff AR, Debatisse D. Localizing signs in positional vertigo due to lateral canal cupulolithiasis. Neurology 2001;57:1085–8. [DOI] [PubMed] [Google Scholar]
- 20.Nuti D, Vannucchi P, Pagnini P. Lateral canal BPPV: which is the affected side? Audiol Med 2005;3:16-20. [Google Scholar]
- 21.Koo JW, Moon IJ, Shim WS, et al. Value of lying-down nystagmus in the lateralization of horizontal semicircular canal benign paroxysmal positional vertigo. Otol Neurotol. 2006;27:367371. [DOI] [PubMed] [Google Scholar]
- 22.Gufoni M, Mastrosimone L. Repositioning maneuver in benign paroxysmal vertigo of horizontal semicircular canal. Acta Otorhinolaringol Ital 1998;18:363-7. [PubMed] [Google Scholar]
- 23.Mandalà M, Pepponi E, Santoro GP, et al. Double-blind randomized trial on the efficacy of the Gufoni maneuver for treatment of lateral canal BPPV. Laryngoscope. 2013;123:1782-6. [DOI] [PubMed] [Google Scholar]
- 24.Vannucchi P, Giannoni B, Pagnini P. Treatment of horizontal semicircular canal benign paroxysmal positional vertigo. J Vestib Res 1997;7:1-6. [PubMed] [Google Scholar]
- 25.Ciniglio Appiani G, Catania G, Gagliardi M, Cuiuli G. Repositioning maneuver for the treatment of the apogeotropic variant of horizontal canal benign paroxysmal positional vertigo. Otol Neurotol 2005;26:257-60. [DOI] [PubMed] [Google Scholar]
- 26.Vannucchi P, Asprella Libonati G, Gufoni M. The Physical Treatment of Lateral Semicircular Canal Canalolithiasis. Audiol Med 2005;3:52-66. [Google Scholar]
- 27.Boselli F, Kleiser L, Bockisch CJ, Hegemann SC, Obrist D. Quantitative analysis of benign paroxysmal positional vertigo fatigue under canalithiasis conditions. J Biomech 2014; 47:1853-60. [DOI] [PubMed] [Google Scholar]
- 28.Baloh RW, Yue Q, Jacobson KM, Honrubia V. Persistent direction- changing positional nystagmus: another variant of benign positional nystagmus? Neurology 1995;45:1297–301. [DOI] [PubMed] [Google Scholar]
- 29.Lee S-H, Choi K-D, Jeong S-H, et al. Nystagmus during neck flexion in the pitch plane in benign paroxysmal positional vertigo involving the horizontal canal. J Neurol Sci 2007;256:75-80. [DOI] [PubMed] [Google Scholar]
- 30.Han BI, Oh HJ, Kim JS. Nystagmus while recumbent in horizontal canal benign paroxysmal positional vertigo. Neurology 2006;66:706-10. [DOI] [PubMed] [Google Scholar]
- 31.Oh JH, Song SK, Lee JS, et al. Lying-down nystagmus and head-bending nystagmus in horizontal semicircular canal benign paroxysmal positional vertigo: are they useful for lateralization? BMC Ophthalmol 2014;14:136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Marcelli V. Nystagmus intensity and direction in bow and lean test: an aid to diagnosis of lateral semicircular canal benign paroxysmal positional vertigo. Acta Otorhinolaryngol Ital 2016;36:520-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Martellucci S, Attanasio G, Ralli M, et al. Does cervical range of motion affect the outcomes of canalith repositioning procedures for posterior canal benign positional paroxysmal vertigo? Am J Otolaryngol 2019;40:494-8. [DOI] [PubMed] [Google Scholar]


