Abstract
National evidence-based guidelines recommend offering hydroxyurea to patients with sickle cell anemia (SCA) 9 months of age and older using shared decision making, but offer no strategies to aid implementation. We developed a hydroxyurea multicomponent decision aid via a needs assessment, clinic observations, and iterative feedback to address parent decision needs and promote a discussion between clinicians and parents. A total of 75 parents and 28 clinicians participated across all phases. The decision aid was rated as useful. Hydroxyurea knowledge improved and decisional conflict decreased supporting the potential for use to facilitate shared decision making in pediatric SCA.
Keywords: pediatric, decision-making, decision aids, treatment preference, hydroxyurea
Introduction
Approximately 1 in 2500 U.S. babies has sickle cell disease, with highest incidence among African-Americans (1 in 400).1 Sickle cell anemia (SCA) is the most severe form, placing children at-risk for serious medical complications including stroke, and early morbidity and mortality. Hydroxyurea significantly reduces the frequency of pain, hospitalizations, transfusions, serious medical complications, and may improve quality of life.2,3 Despite substantial health and psychosocial benefits, widespread adoption of hydroxyurea in pediatrics has been slow due to a variety of factors at the systems, clinician and patient/parent level2. At the systems level, barriers such as non-FDA approval, label packaging as a chemotherapeutic agent, and limited access to hydroxyurea (particularly the liquid form), influence use.2,4 Clinicians report concerns about patient/family adherence with hydroxyurea and monitoring, safety of its use in young children, and the impact on fertility resulting in variations in prescribing.4 Some clinicians have also reported that not having enough time to explain fully the benefits and risks to patients/families as a barrier.4 From the parent perspective, feelings of uncertainty (decisional conflict) and concerns about efficacy, safety, and side-effects are influential.5,6 If these factors are not adequately addressed, parents may delay decision making about hydroxyurea for months or years.
National Heart, Lung, and Blood Institute (NHLBI) evidence-based guidelines recommend offering hydroxyurea to all patients 9 months old and older using shared decision making,7 but offer no specific strategies or tools to aid implementation. Shared decision making is a collaborative process in which clinicians and patients (and/or parents in the context of pediatric medical settings) come together to make health decisions based on best clinical evidence and patient/parent preferences and values.8 A first step to facilitating shared decision making, is to understand the decisional needs of parents and clinicians. Decision aids are educational tools to assist patients or parents in decision-making and have been found to increase patient/parent knowledge about treatment options, reduce decisional conflict, and improve patient/parent involvement in decision-making.9 Both anecdotal data reported by clinicians and the larger literature suggest that talking with other parents plays an influential role in decision-making.10 Recent studies have found that inclusion of patient stories in decision aids improves knowledge of treatment options,11 helps individuals make decisions based on trade-offs and personal values, facilitates individuals discussing the decision with others, and increases decision intentionality.12,13 The objective of the current study was to identify influential factors and support needs for parents of children with SCA facing the decision to initiate hydroxyurea with the goal of developing a tailored decision aid. This paper describes the needs assessment, development of the aid and its acceptability, feasibility and preliminary impact on parent decisional conflict and hydroxyurea knowledge.
Materials and Methods
Needs Assessment
Based on a literature review of 1) decision support needs and development of decision aids for parents of children with chronic diseases, 2) barriers and facilitators for hydroxyurea use, 3) shared decision making in SCA, and guided by empirically supported standards for decisional needs assessments14 and discussions with clinicians, we developed a semi-structured interview guide to understand hydroxyurea decision-making including influential motivations and beliefs and resources they found helpful or would be helpful for others. Parents were recruited by phone or in clinic after receiving a letter describing the study. Eligible parents had already made a decision about hydroxyurea initiation (n=52 CCHMC; n = 7 referred by hematologists participating in a national learning collaborative). After providing consent, 25 parents of children with SCA (20 local and 5 others) were interviewed. Research staff conducted interviews using the semi-structured interview guide, which lasted 30–45 minutes.
Concurrently, clinicians were surveyed to understand implementation barriers and facilitators for hydroxyurea shared decision making. Clinicians were identified through convenience sampling of local clinicians (n=5) and those participating in a Hemoglobinopathy Learning Collaborative (n=23). All clinicians invited to participate completed a survey developed based on the Ottawa Decision Support group recommendations and their data were included in analyses. 14. 14We obtained a waiver of consent for clinicians.
Decision Aid Development
Two authors (LC, AW) conducted independent content analysis of transcripts of parent interviews and observations of clinician-parent discussions about hydroxyurea initiation. Guided by social cognitive theory and the theory of planned behavior,15,16 transcripts were coded for issues that parents reported actively thinking about prior to decision making and strategies that facilitated decision making. Final themes were determined by consensus. Themes guided the development of prototypes of the different components of the decision aid (e.g. parent video narratives, in-visit issue card) which were refined using an iterative process. SCA experts identified parents who were good storytellers for the video narratives (i.e. told an engaging and memorable story that was easily understood).12,17 We completed twelve iterations of the other components of the decision aid before qualitative feedback from parents and clinicians indicated that the decision aid met needs and SCA experts agreed the aid met the majority of International Patient Decision Aid Standards (IPDAS).
Evaluation Plan
Parents were eligible for participation if 1) their child had a diagnosis of SCA and received care at one of the clinics, 2) the parent had not previously made a decision about hydroxyurea, and 3) they could read and speak English fluently. Clinicians had to agree that study participation would not interfere with the child’s medical treatment. Parents were excluded if they (or the medical team) reported experiencing high levels of acute stress.
The intervention group was made up of parents in pediatric SCA clinics in both a large academic medical center (Midwest – Cincinnati, OH) and a small academic medical center (Midwest – Peoria, IL). Both clinics start discussions with parents about hydroxyurea in the first year of life, and the clinics were shifting from offering hydroxyurea when children are 5 years of age to 9 months of age. These clinics also systematically identified patients eligible for hydroxyurea initiation and tracked whether it was offered. The control group was comprised of parents from a third site, a pediatric SCA clinic in a large academic medical center (West – Oakland, CA). This clinic also identifies patients eligible for hydroxyurea initiation and uses a patient brochure during discussions. Parents in the control and intervention group were determined based on clinic and were not randomized to groups. Control group parents completed measures without exposure to the decision aid. The Institutional Review Boards at all three sites approved the study.
Evaluation Measures
Decisional uncertainty was assessed using the 16-item decisional conflict scale (DCS).18 A 9-item survey specific to content on the decision aid was used to assess hydroxyurea knowledge (highest score 9; Cronbach alpha = 0.708).
We evaluated acceptability of the decision aids using a 10-item survey; the survey has been used in previous studies and includes likert and open-ended questions (Cronbach alpha = 0.669).19 Specifically, feedback was elicited about the content, complexity, balance, format, and usefulness of the decision aid. Open-ended questions probed what participants liked and disliked about the aid.
Evaluation Methods
For parents in the intervention group, research staff provided the pre-visit brochure and access to the parent video narratives (parents could watch one or more) via an iPad or computer. Clinicians gave parents the in-visit issue card and the after visit booklet, which parents could use to take notes during the discussion. Clinicians received training on asking parents to choose the first 2–3 issues to discuss. Parents in the control group received the informational brochure as a part of their usual care. Parents in both the control and intervention groups completed the DCS and the hydroxyurea knowledge questionnaire following their clinic visit. The first 11 parents recruited into the intervention group (n=11) completed written consent, a demographic survey, the DCS, and the hydroxyurea knowledges questionnaire prior to the clinic visit to allow for measurement of changes pre to post. Additionally, this group completed the 10-item survey of acceptability and provided qualitative feedback on content, format, and comprehensiveness of the decision aid.
Data Analysis
We conducted all quantitative analyses in SPSS Version 23 or Mplus (Version 7.4). Seven participants did not complete at least one item on the hydroxyurea knowledge survey; thus, we handled missing data via alternative model [HA:] multiple imputation with 34 auxiliary correlate variables to increase the plausibility of missing at random. Analyses did not identify any patterns for missing items. We examined changes in DCS scores and hydroxyurea knowledge with repeated measures ANOVAs for the intervention group (pre and post). To determine effect sizes (Cohen’s d ≤0.2 = small; ≤0.5 = medium; ≤ 0.8 = large) for hydroxyurea knowledge and DCS between parents who did or did not use decision aids, we conducted independent samples ANOVAs.
Results
Participants
Table 1 summarizes demographic information for all participants and feasibility and acceptability data for the multicomponent decision aid. In general, parents were African-American, non-Hispanic and mothers. The groups did not differ on age, race, gender, mother’s highest level of education, father’s highest level of education, or hemoglobin type as demonstrated by Chi-Squares and T-tests.
Table 1.
Demographic Characteristics
| Parent Interviews (n=25) | % (N) | M (SD) |
| Relationship to Patient | ||
| Mother | 80%(20) | |
| Father | 12% (3) | |
| Grandmother | 4% (1) | |
| Grandfather | 4% (1) | |
| Mothers Highest Level of Education | ||
| Graduate or professional degree | 24% (6) | |
| College Graduate | 24% (6) | |
| Some college or certification course | 32% (8) | |
| High school graduate | 8% (2) | |
| 9th– 12th grade or less | 12% (3) | |
| Fathers Highest Level of Education | ||
| Graduate or professional degree | 12% (3) | |
| College Graduate | 24% (6) | |
| Some college or certification course | 20% (5) | |
| High school graduate | 8% (2) | |
| 9th– 12th grade or less | 16% (4) | |
| 7th–9th grade or less | 4% (1) | |
| Unknown | 16% (4) | |
| Insurance | ||
| Private | 28% (7) | |
| Public | 52% (13) | |
| Unknown | 20% (5) | |
| Patient Age | 12.30 (3.49) | |
| Patient Gender | ||
| Female | 52% (13) | |
| Male | 48% (12) | |
| Patient Ethnicity | ||
| Black or African American | 100% (25) | |
| Patient SCD Genotype | ||
| HbSS | 84% (21) | |
| HbSC | 8% (2) | |
| HbS Beta 0 Thal | 4% (1) | |
| HbS Beta + Thal | 4% (1) | |
| Morisky Scale | Low adherence | |
| PedsQL Total Score | 75.74 (15.61) | |
| Provider Survey/ Interviews (n=28) | % (N) | M (SD) |
| Position | ||
| Physicians | 67.86% (19) | |
| Nurse Practitioners | 21.43% (6) | |
| Nurses | 7.14% (2) | |
| Psychologist | 3.57% (1) | |
| Practice Specialty | ||
| Pediatric Hematology | 78.57% (22) | |
| Adult Hematology | 10.71% (3) | |
| Primary Care Provider | 10.71% (3) | |
| Clinic Observations (n=5) | % (N) | M (SD) |
| Relationship to Patient | ||
| Mother | 80% (4) | |
| Father | 20% (1) | |
| Mothers Highest Level of Education | ||
| Graduate or professional degree | 20% (1) | |
| College Graduate | 20% (1) | |
| Some college or certification course | 40% (2) | |
| 9th– 12th grade or less | 20% (1) | |
| Fathers Highest Level of Education | ||
| Some college or certification course | 60% (3) | |
| High school graduate | 20% (1) | |
| 9th– 12th grade or less | 20% (1) | |
| Insurance | ||
| Private | 20% (1) | |
| Public | 80% (4) | |
| Patient Age | 6.89 (4.91) | |
| Patient Gender | ||
| Female | 60% (3) | |
| Male | 40% (2) | |
| Patient Ethnicity | ||
| Black or African American | 100% (5) | |
| Patient SCD Genotype | ||
| HbSS | 80% (4) | |
| HbSC | 20% (1) | |
| Parent Narratives (n=5) | % (N) | M (SD) |
| Relationship to Patient | ||
| Mother | 80% (4) | |
| Father | 20% (1) | |
| Mothers Highest Level of Education | ||
| Graduate or professional degree | 20% (1) | |
| College Graduate | 20% (1) | |
| Some college or certification course | 40% (2) | |
| High school graduate | 20% (1) | |
| Fathers Highest Level of Education | ||
| Graduate or professional degree | 40% (2) | |
| High school graduate | 40% (2) | |
| 9th–12th grade or less | 20% (1) | |
| Insurance | ||
| Private | 40% (2) | |
| Public | 40% (2) | |
| Unknown | 20% (1) | |
| Patient Age | 8.39 (5.91) | |
| Patient Gender | ||
| Female | 60% (3) | |
| Males | 40% (2) | |
| Patient Ethnicity | ||
| Black or African American | 100% (5) | |
| Patient SCD Genotype | ||
| HbSS | 100% (5) | |
| Intervention Group (n=27) | % (N) | M (SD) |
| Relationship to Patient | ||
| Mother | 74.10% (20) | |
| Father | 18.50% (5) | |
| Grandmother | 3.70% (1) | |
| Other | 3.70% (1) | |
| Mothers Highest Level of Education | ||
| College Graduate | 29.63% (8) | |
| Some college or certification course | 25.92% (7) | |
| High school graduate | 18.52% (5) | |
| 9th– 12th grade or less | 18.52% (5) | |
| Unknown | 7.41% (2) | |
| Fathers Highest Level of Education | ||
| Graduate or professional degree | 7.41% (2) | |
| College Graduate | 11.11% (3) | |
| Some college or certification course | 25.92% (7) | |
| High school graduate | 29.63% (8) | |
| 9th– 12th grade or less | 14.81% (4) | |
| Unknown | 11.11% (3) | |
| Insurance | ||
| Private | 14.81% (4) | |
| Public | 85.19% (23) | |
| Patient Age | 4.06 (4.60) | |
| Patient Gender | ||
| Female | 74.10% (20) | |
| Male | 25.90% (7) | |
| Patient Ethnicity | ||
| Black or African American | 100% (27) | |
| Patient SCD Genotype | ||
| HbSS | 96.29% (26) | |
| Sickle Cell Trait | 3.70% (1) | |
| Control Group (n=20) | % (N) | M (SD) |
| Relationship to Patient | ||
| Mother | 65% (13) | |
| Father | 15% (3) | |
| Grandmother | 5% (1) | |
| Guardian | 10% (2) | |
| Self | 5% (1) | |
| Mothers Highest Level of Education | ||
| College graduate | 40% (8) | |
| Some college or certification course | 25% (5) | |
| High school graduate | 5% (1) | |
| 9th–12th grade or less | 10% (2) | |
| Unknown | 20% (4) | |
| Fathers Highest Level of Education | ||
| Graduate or professional degree | 10% (2) | |
| College graduate | 15% (3) | |
| Some college or certification course | 10% (2) | |
| High school graduate | 25% (5) | |
| 9th–12th grade or less | 25% (5) | |
| Unknown | 15% (3) | |
| Insurance | ||
| Private | 30% (6) | |
| Public | 70% (14) | |
| Patient Age | 6.53 (5.44) | |
| Patient Gender | ||
| Female | 60% (12) | |
| Male | 40% (8) | |
| Patient Ethnicity | ||
| Black or African American | 75% (15) | |
| Hispanic | 10% (2) | |
| Multi-Racial | 15% (3) | |
| Patient SCD Genotype | ||
| HbSS | 95% (19) | |
| HbS Beta 0 Thal | 5% (1) | |
| Acceptability (n=11) | % (N) | M (SD) |
| Clear information | 90.9% (10) | |
| Right amount of information | 100% (11) | |
| Helpful information about side effects/risks | 90.9% (10) | |
| Helpful information about evidence of benefits | 90.9% (10) | |
| Useful when deciding | 100% (11) | |
| Balanced | 81.8% (9) | |
Clinicians were primarily physicians, specifically pediatric hematologists. Sites were chosen by convenience; site clinicians had > 10 years of experience taking care of patients with SCA.
Needs Assessment
Table 2 contains themes from the literature review, interviews, surveys and clinic observations revealed by parents and clinicians, and how addressed in the decision aid. Parents also identified key issues to discuss with clinicians: 1) how hydroxyurea works to treat SCA; 2) benefits; 3) side-effects/risks; 4) anticipated changes in daily life; 5) associated costs; and 6) frequently asked questions. Clinicians desired a shared decision aid and asked for talking points and training on use of the decision aids.
Table 2.
Parent and clinician decision support needs
| Parent/Clinician Need | Demonstrative Quote | Decision Aid Component |
|---|---|---|
| Parents felt unprepared to discuss hydroxyurea initiation. |
“That’s what’s scary when you don’t have the appropriate information, you just have to make a decision . . . don’t have the time or opportunity to get the information.” “Parents may not really understand everything . . . cause sometimes they may not know the correct answers . . . the correct questions to ask so they’re kind of left in the dark.” “[To overcome the barrier of lack of knowledge] it would help to supply the information ahead of time instead of just suggesting it at the clinic like during their treatment...So that they kind of have a heads up of what’s going on next.” |
Pre-visit brochure |
| Parents had difficulty accessing accurate information about SCA and hydroxyurea. |
“In the beginning I felt a little scared, it was as if I didn’t have enough information to really understand um the effects of the medicine what to expect from the medicine.” “All of our research on the drug itself, its relationship was to its use in the treatment of cancer and we didn’t really understand the correlation between that and how it’s being applied here.” “The only thing I wish was out there and it’s just not readily available right now would be is the long term information because right now, we’re just stepping out on faith.” |
All decision aid materials |
| Parents wanted to hear the experiences of other parents prior to making a decision. |
“We talked with the doctor and then one of the biggest influences, I think was just talking to another parent.” “Yeah, cause sometimes people have to look at information and see what other parents’ opinion and decision making is and how they deal and dealt with their child and situation.” “That would’ve been great to have people in the room, people who are on hydroxyurea and people who are starting you know, ... to know the process and how it works.” |
Video narratives |
| Parents desired a discussion that incorporated their values and preferences. |
“I know they’re doc- they’re the doctor, but ... that’s my child. . . . I don’t just take it just because that’s what they say. . . maybe personally for you, quality of life was important, so maybe that would affect [your decision}” “If there was another visit then they would be like ‘have you thought any’ you know ‘what do you think?’ it wasn’t ‘we want him to do this’ it was ‘well, what do you think?’” “Just sitting down to ask him a lot of questions. Just asking the doctor any questions to assure you that this doesn’t [seem like] the wrong decision.” |
Organization of the decision aids by issues important to parents (range of topics available on the issue card to discuss with clinicians). |
| Parents needed to have information to share with other family members who would help make the decision but may not be present at the visit. |
“The family has the decision, but if you go home like me; me and my husband make the decision.” “I looked [HU] up and I talked to my family about it, like all my family. And so we all basically just came up with a decision together...” “[I] decided with my mom. My mom is always there, . . . even if she is nine hours away from you, she still wanna know. . . she wants to be in that decision.” |
After-visit booklet |
| Parents may not make the decision after the first discussion with the clinician. |
“[I need] time, don’t rush me when making a decision like that.” “I kinda take my time getting information. I have a really great support system of both family members . . . and I ask a lot of questions and just deal with it until I’m comfortable with it, then I can make a decision because ultimately if the responsibility’s gonna rest on my shoulders, then I need to be comfortable with it.” “[After the] recommendation from the doctor, then me and my husband take time to talk about it and then we’ll talk about it with [our child with sickle cell anemia]; sometimes, I try and get opinions from others, you know adults with sickle cell or some parents of children with sickle cell that possibly have the same experience or in the same situation and then we’ll come back together and try to make the best informed decision that works for us.” |
After-visit booklet |
| Clinicians need more time to have a comprehensive discussion. |
“have enough of an appointment time to be able to explain clearly enough the how’s and why’s without having to rush to the next patient.” “I wish I had more time and literature specifically tailored for patient with sickle cell disease.” “The lack of time and resources to show patients.” “Lack of time during appointments.” |
Structured process – prioritize issues most important to parents, provider talking points |
| Clinicians desire sickle cell specific resources. |
“A better sickle cell focused hand out” “Visual aids explaining effects of HU” “Simple handout discussing data about efficacy and side effects in very simple terms, history of its use. importance and schedule for lab monitoring” |
After-visit booklet, resources and video narratives |
| Clinicians concerned that parents do not have access to accurate information. |
“New treatment, chemotherapy drug, hesitant when introduced because no technology to search in front of them” “It is very difficult when families without any knowledge feel that the medication is “experimental” . . . Also, when families want a 100% guarantee that this medication will cure their child (i.e. unrealistic expectations).” “Wrong information that the patient [parent] has received about hydroxyurea in the past.” “Conflicting and/or anecdotal information” “misinformation from other patients/families (“my child was fine until she took HU, then she got so much worse, don’t put your child on it”)” |
All decision aids, resources and the video narratives |
| Clinicians feel some parents are not ready for the discussion. |
“Lack of understanding . . . about seriousness of untreated SCD; unwillingness to make a decision that might result in unintended side effects; desire for a magical cure without any risks” “If I feel the patient [parent] does not truly understand the pros/cons of their choice . . . If patient [parent] cannot articulate why they have made a particular choice or are inconsistent in their preference, . . . I feel patient [parent] is making choice based on biased or inaccurate presentation of information” “They don’t see the need, a lot of info going on in visit (HU message may be lost)” ‘Fear of the unknown; difficulty in understanding the risks of their current disease state vs the possible risks of HU” |
Organization of the decision aids by issues important to parents (range of topics available on the issue card to discuss with parents). |
| Clinicians want parents to be active partners in decision making. |
“It is easy to support decision making when they ask insightful questions and seem to understand the information I am giving them.” “Family willing to be a partner in decision making and willing to weigh risks and benefits as objectively as possible.” ‘Parents thinking it through, opportunity to provide additional information.” “When they ask questions and wait for answers; when the meeting goes at least an hour and everyone is talking and listening---being open and honest.” |
Issue card |
| Clinicians feel talking with others parents would help with decision making. |
“Parent testimonials; educational materials in easy to grasp format.” “It helps if the patients/families talk to other patient/families that are on hydroxyurea and can share their experiences. This gives them a perspective that the medical provider cannot give them.” “More patient-oriented materials, audiovisuals.” “Parent testimonials would be a huge plus.” “I would like to have more first-person testimonials about HU that are accurate. We need them from all age groups, boys and girls and parents.” |
Video narratives |
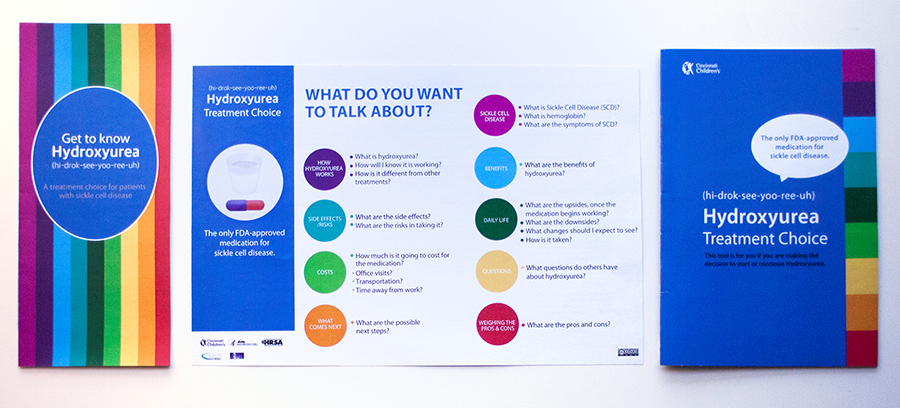
Multicomponent Decision Aid
We developed a multicomponent decision aid (Figure 1) consisting of a pre-visit brochure, five parent video narratives, a during-visit issue card, and an after-visit booklet. To ensure accuracy, hematologists reviewed and edited decision aid content. The pre-visit brochure describes how hydroxyurea works in SCA in an effort to prepare parents for their discussion with clinicians. Video narratives provide information about the decision making process. Parents on the videos provided narrative responses to stems or questions corresponding to themes from the needs assessment (e.g. tell us your thoughts about hydroxyurea’s side effects, short-term or long-term, during your decision making process). Videos feature the 1) mother of an infant, 2) mother of a teenager, 3) father of a young child, 4) mother of a school age child, and 3) a “young” mother (during acceptability testing, parents requested a mother who was in her twenties). Parent feedback on video narratives indicated that they were beneficial because they covered a wide range of issues, helped parents think of questions to discuss with clinicians, and increased confidence in decision-making. The during visit card and after-visit booklet are organized by issue, with each issue presented in a different color. Clinicians and parents use the issue card during the visit to promote a discussion. Clinicians asked for standardized information to discuss with parents, thus, the back of the issue card contains talking points for each issue. The after-visit booklet contains information on how hydroxyurea works for SCA, costs, benefits, side-effects, impact on daily life, frequently asked questions, resources, next steps and a decision making exercise. Parents can take notes in the booklet during the discussion. After the visit, parents leave with the booklet, which they can share with others who may help make the decision.
Figure 1:
Before-visit, during-visit, and after-visit components of the decision aid.
Evaluation Results
All parents using the decision aids reported that they were useful for decision-making (100%; see Table 1). Hydroxyurea knowledge increased and decisional conflict decreased pre to post with use of the decision aids (Table 3). The comparison of the post-test scores of parents who used the decision aid with the post-test scores of parents who did not use the decision aid revealed a significant difference in the DCS informed subscale (p = 046) and a large effect size (d=0.66). Analyses revealed medium effect sizes for the DCS total scale (d =0.41) and the DCS values clarification subscale (d = 0.51).
Table 3.
Hydroxyurea Knowledge and Decisional Conflict Scores
| Pre/Post Group (n=11) Pre-test M(SD) |
Intervention Group (N=27) Post-test M(SD) |
Pre/Post Group pre/post difference P value |
Within Intervention Group Cohen’s d of pre to post difference |
Control Group (N=20) Post-test M(SD) |
Between Groups comparison of post-test scores p value |
Between Groups Cohen’s d of post-test scores | |
|---|---|---|---|---|---|---|---|
| Hydroxyurea Knowledge | 6.5 (1.4) | 7.1 (1.3) | 0.001* | 0.68 | 7.2 (2.2) | 0.875 | 0.07 |
| Decisional conflict scale (DCS) | |||||||
| DCS total score | 22.5 (18.0) | 13.2 (13.1) | 0.002* | 0.69 | 18.9 (14.8) | 0.178 | 0.41 |
| DCS uncertainty | 25.3 (24.4) | 16.7 (18.9) | 0.001* | 0.45 | 22.5 (21.6) | 0.342 | 0.29 |
| DCS informed | 23.7 (18.6) | 11.4 (14.3) | 0.001* | 0.74 | 24.17 (24.5) | 0.046* | 0.66 |
| DCS values clarity | 25.9 (22.2) | 13.3 (13.3) | 0.004* | 0.65 | 20.4 (15.2) | 0.101 | 0.51 |
| DCS support | 16.7 (17.1) | 12.0 (13.7) | 0.079 | 0.36 | 12.5 (12.8) | 0.906 | 0.13 |
| DCS effective decision | 21.3 (21.1) | 12.7 (16.3) | 0.008* | 0.58 | 15.9 (16.9) | 0.518 | 0.19 |
statistically significant difference (p < .05)
Discussion
Sickle cell anemia (SCA) is a severe form of sickle cell disease that puts children at-risk for early mortality and morbidity in addition to other serious medical complications. Evidence-based guidelines developed by the National Heart, Lung, and Blood institute recommend clinicians offer hydroxyurea to all patients 9 months old and older using shared decision making with no implementation guidance. The goals of the current study were to develop a decision aid to facilitate shared decision making for hydroxyurea.
Needs Assessment and Decision Aid Development
Our needs assessment identified parental decision support needs consistent with those previously described in the literature including managing their emotional responses (feeling unprepared), balancing the child’s best interest with their personal values and preferences, getting accurate information about treatment outcomes, and having time to make the decision (not feeling pressured).20 Parents also wanted information to prepare for discussions. Moreover, clinicians and parents agreed that the decision to initiate hydroxyurea might take more than one discussion. The after-visit booklet was designed to meet this need. Allowing time for parents to deliberate outside of the clinic visit may lessen any pressure parents feel to say “yes” immediately.
Qualitative feedback gathered during decision aid development suggested that parents desire a decision aid that is comprehensive, evidence-based, tailored to their needs, in a question and answer format, and a consistent organizational scheme across the components (pre-visit brochure, after visit booklet).10 Parents also want information about trustworthy resources to conduct their own research. The video narratives were well-received by parents, viewed as influential in decision making, and complementary to discussions with clinicians. Parents desired a discussion with clinicians that included their values and experiences, but also wanted to take an active role in decision-making. Parents asked for support in weighing options and next steps in the decision-making process; in response, we included a decision making exercise and a next steps checklist in the after-visit booklet.
Evaluation, Limitations, and Future Directions
The data suggest that our multicomponent decision aid for hydroxyurea has potential for helping parents clarify their values, feel more informed, and decrease feelings of uncertainty (conflict) during decision-making. The aid may have also assisted clinicians with implementing hydroxyurea treatment guidelines for children with SCA; however, a randomized trial is needed to determine the acceptability (using a standardized measure) of the decision aid for a larger group of parents. The trial should also evaluate the impact of the decision aid on shared decision making (e.g. parental perception of and involvement in decision making) and clinical outcomes. Our study used a convenience sample and results should be interpreted with this in mind. Although the Flesch–Kincaid readability level of the decision aids was calculated to be seventh grade on average, studies are needed to determine if this level meets parent health literacy needs. In addition, we did not collect data on significant others involved in the decision making process (e.g. other family members). Although the overall decision aid was rated as balanced, future studies should evaluate whether parents perceived the video narratives as biased (nudging them toward initiating hydroxyurea). For example, did they feel parents used value-laden language rather than descriptive language?11 Did they feel parents left out important information about hydroxyurea?11 Additionally, this study’s findings may be limited by the inclusion of primarily parents with high levels of education; findings may also not be applicable for adult SCA populations. These materials would require adaptation for use with older populations.
Use of the hydroxyurea multicomponent decision aid showed potential for assisting parents of children with SCA in decision making. A review of data collected on parent decisions indicates that 70% of parents exposed to the decision aid decided to start their child on hydroxyurea after the discussion. Parents not making an immediate decision reported that they needed more time to deliberate and/or conduct their own research. It is possible that the decision aid helped parents take an active role in the decision making process and intentional about their decision. Ultimately, better parent engagement in the process may improve hydroxyurea uptake in children with SCA.21
Acknowledgments
The project described was supported in part by Agency for Healthcare Research and Quality’s (AHRQ) Centers for Education and Research in Therapeutics (CERTs) Grant number: 1U19HS021114. This project was also supported by the Health Resources and Services Administration (HRSA) Sickle Cell Disease Treatment Demonstration Program grant number: U1EMC27863. The Hemoglobinopathy Learning Collaborative was supported by funding from the Health Resources and Services Administration (HRSA) Sickle Cell Disease Treatment Demonstration Program Sickle Cell Disease Treatment Demonstration Program (HRSA Contract #HHSH25020100022C). The content is solely the responsibility of the authors and does not necessarily represent the official views of the AHRQ or HRSA. The authors would like to thank Suyao Chen a graduate student at the University of Cincinnati College of Design who contributed to the graphic design of the decision aid. The authors would like to acknowledge Dylan Rudy, Cami Mosley, and Ellen Manegold for their assistance with data collection, data preparation, and formatting. Finally, the authors wish to thank the parents, clinicians and other experts who contributed to the development and refinement of the decision aid.
Conflicts of Interest and Source of Funding: The project described was supported in part by Agency for Healthcare Research and Quality’s (AHRQ) Centers for Education and Research in Therapeutics (CERTs) Grant number: 1U19HS021114. This project was also supported by the Health Resources and Services Administration (HRSA) Sickle Cell Disease Treatment Demonstration Program grant number: U1EMC27863. The Hemoglobinopathy Learning Collaborative was supported by funding from the Health Resources and Services Administration (HRSA) Sickle Cell Disease Treatment Demonstration Program Sickle Cell Disease Treatment Demonstration Program (HRSA Contract #HHSH25020100022C). The content is solely the responsibility of the authors and does not necessarily represent the official views of the AHRQ or HRSA.
References
- 1.Brousseau DC, A Panepinto J, Nimmer M, Hoffmann RG. The number of people with sickle-cell disease in the United States: national and state estimates. American journal of hematology. 2010;85(1):77–78. [DOI] [PubMed] [Google Scholar]
- 2.Brawley OW, Cornelius LJ, Edwards LR, et al. National Institutes of Health Consensus Development Conference statement: hydroxyurea treatment for sickle cell disease. Ann Intern Med. 2008;148(12):932–938. [DOI] [PubMed] [Google Scholar]
- 3.McGann PT, Ware RE. Hydroxyurea therapy for sickle cell anemia. Expert opinion on drug safety. 2015;14(11):1749–1758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brandow AM, Jirovec DL, Panepinto JA. Hydroxyurea in children with sickle cell disease: practice patterns and barriers to utilization. American journal of hematology. 2010;85(8):611–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oyeku SO, Driscoll MC, Cohen HW, et al. Parental and other factors associated with hydroxyurea use for pediatric sickle cell disease. Pediatric blood & cancer. 2013;60(4):653–658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hankins J, Hinds P, Day S, et al. Therapy preference and decision-making among patients with severe sickle cell anemia and their families. Pediatric blood & cancer. 2007;48(7):705–710. [DOI] [PubMed] [Google Scholar]
- 7.Yawn BP, Buchanan GR, Afenyi-Annan AN, et al. Management of sickle cell disease: summary of the 2014 evidence-based report by expert panel members. Jama. 2014;312(10):1033–1048. [DOI] [PubMed] [Google Scholar]
- 8.Wyatt KD, List B, Brinkman WB, et al. Shared decision making in pediatrics: a systematic review and meta-analysis. Academic pediatrics. 2015;15(6):573–583. [DOI] [PubMed] [Google Scholar]
- 9.Stacey D, Légaré F, Col NF, et al. Decision aids for people facing health treatment or screening decisions. The Cochrane Library. 2014. [DOI] [PubMed] [Google Scholar]
- 10.Jackson C, Cheater FM, Reid I. A systematic review of decision support needs of parents making child health decisions. Health expectations. 2008;11(3):232–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bekker HL, Winterbottom AE, Butow P, et al. Do personal stories make patient decision aids more effective? A critical review of theory and evidence. BMC medical informatics and decision making. 2013;13(2):S9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kreuter MW, Holmes K, Alcaraz K, et al. Comparing narrative and informational videos to increase mammography in low-income African American women. Patient Educ Couns. 2010;81:S6–S14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jibaja-Weiss ML, Volk RJ, Granchi TS, et al. Entertainment education for breast cancer surgery decisions: a randomized trial among patients with low health literacy. Patient Educ Couns. 2011;84(1):41–48. [DOI] [PubMed] [Google Scholar]
- 14.Jacobsen M, O’Connor A, Stacey D. Decisional Needs Assessment in Populations. A workbook for assessing patients’ and practitioners’ decision making needs1999. 2013. [Google Scholar]
- 15.Makoul G, Clayman ML. An integrative model of shared decision making in medical encounters. Patient Educ Couns. 2006;60(3):301–312. [DOI] [PubMed] [Google Scholar]
- 16.Han H, Kim Y. An investigation of green hotel customers’ decision formation: Developing an extended model of the theory of planned behavior. International Journal of Hospitality Management. 2010;4(29):659–668. [Google Scholar]
- 17.Kreuter MW, Green MC, Cappella JN, et al. Narrative communication in cancer prevention and control: a framework to guide research and application. Ann Behav Med. 2007;33(3):221–235. [DOI] [PubMed] [Google Scholar]
- 18.O’Connor AM. Validation of a decisional conflict scale. Medical decision making. 1995;15(1):25–30. [DOI] [PubMed] [Google Scholar]
- 19.O’Connor A, Cranney A. User Manual - Acceptability [document on the internet]. 1996; http://decisionaid.ohrica/docs/develop/User_Manuals/UM_Acceptability.pdf. Accessed August, 2017.
- 20.Heath G, Abdin S, Begum R, Kearney S. Putting children forward for epilepsy surgery: A qualitative study of UK parents’ and health professionals’ decision-making experiences. Epilepsy Behav. 2016;61:185–191. [DOI] [PubMed] [Google Scholar]
- 21.Heeney MM, Ware RE. Hydroxyurea for children with sickle cell disease. Pediatric clinics of North America. 2008;55(2):483–501, x. [DOI] [PubMed] [Google Scholar]