Abstract
Background
Pulmonary hypertension (PH) causes increased morbidity and mortality in patients with interstitial lung diseases (ILD). Classification schemes, while well-characterised for the vasculopathy of idiopathic PH, have been applied, unchallenged, to ILD-related PH. We evaluated pulmonary arterial histopathology in explanted human lung tissue from patients who were transplanted for advanced fibrotic ILD.
Methods
Lung explants from 38 adult patients who underwent lung transplantation were included. Patients were divided into three groups: none, mild/moderate and severe PH by mean pulmonary artery pressure (mPAP) measured at pre lung transplantation right heart catheterisation (RHC). Grading of pulmonary vasculopathy according to Heath and Edwards scheme, and prelung transplantation evaluation data were compared between the groups.
Results
38 patients with fibrotic ILDs were included, the majority (21) with idiopathic pulmonary fibrosis. Of the 38 patients, 18 had severe PH, 13 had mild/moderate PH and 7 had no PH by RHC. 16 of 38 patients had severe pulmonary arterial vasculopathy including vascular occlusion with intimal fibrosis and/or plexiform lesions. There were no correlations between mPAP and lung diffusion with the severity of pulmonary arterial pathological grade (Spearman’s rho=0.14, p=0.34, rho=0.11, p=0.49, respectively).
Conclusions
Patients with end stage ILD had severe pulmonary arterial vasculopathy in their explanted lungs irrespective of the presence and/or severity of PH as measured by RHC. These findings suggest that advanced pulmonary arterial vasculopathy is common in patients with advanced fibrotic ILD and may develop prior to the clinical detection of PH by RHC.
Keywords: interstitial fibrosis, primary pulmonary hypertension, lung transplantation
Key messages.
What is the key question?
What is the pulmonary arterial vascular histopathology in patients with end stage fibrotic interstitial lung disease and does it correlate to measured pulmonary arterial pressure?
What is the bottom line?
One-fifth of patients with end stage fibrotic interstitial lung disease had severe pulmonary arterial vasculopathy including plexiform lesions in their explanted lungs.
Why read on?
This study provides direct evidence that WHO group 3 PH related to hypoxemic lung disease has histopathological similarities to WHO group 1 pulmonary arterial hypertension. These findings suggest that severe pulmonary arterial vasculopathy is more common than previously recognised and may develop in advanced fibrotic interstitial lung disease prior to the clinical detection of pulmonary hypertension.
Introduction
Pulmonary hypertension (PH) is a well-known cause of increased morbidity and mortality in patients with interstitial lung diseases (ILD).1–3 ILD-related PH, a subset of the WHO group 3 PH, is defined by a mean pulmonary artery pressure (mPAP) greater than 25 mm Hg on right heart catheterisation (RHC). The prevalence of PH in fibrotic ILD increases with the severity of the lung disease. PH occurs in 46% of end stage fibrotic lung disease awaiting lung transplantation and severe PH, defined as mPAP >35–40 mm Hg is observed in 5%–10%.2–9
The modern clinical classification of PH is five-group taxonomy based on the attributable cause and anticipated vascular histopathology. Group 1 is pulmonary arterial hypertension (PAH) (including idiopathic PAH (iPAH)) while groups 2–5 are aetiologically different and are thought not to derive from primary arterial vasculopathy. Plexiform vasculopathy is the defining pathological feature of iPAH.10 11 Abundant human necropsy tissue studies have demonstrated plexiform arterial lesions since iPAH was first described in 1891 by Ernst Von-Romberg.12–14 Therefore, it is generally assumed that the plexiform lesion is a marker of advance WHO group 1 PAH and a correlate of elevated pulmonary vascular resistance (PVR). The classification of PH related to lung disease outside of primary vasculopathy comes from an assumed causal role of hypoxemia as opposed to a plexiform vasculopathy.15 Human tissue studies from well characterised group 3 patients are rare and these historical assumptions and modern classification scheme have stood unchallenged.16 17
We sought to evaluate the pulmonary arterial histopathology in explanted human lung tissue from well characterised patients who were transplanted for advanced fibrotic ILD. We aimed to examine patient clinical characteristics including pulmonary haemodynamics and their relation to pulmonary arterial histopathology including the presence or absence of plexiform arterial vasculopathy.
Materials and methods
Study population
Data were obtained from 38 of the 133 (age≥18 years) patients with fibrotic ILD who received lung transplantation at Temple University Hospital (TUH), Philadelphia, USA, from 2011 to 2016. The patients were divided into three groups of measured mPAPs determined by pretransplant RHC (see below): none (n=66), mild-moderate (n=49) and severe PH (n=18). We included in the analysis all 18 patients with severe PH, 13 randomly selected patients with mild-moderate PH and 7 randomly selected patients without PH whose explanted lungs were available for pathological studies (figure 1). Clinical data were available as part of routine prelung transplantation evaluation included demographics, pulmonary function tests (PFTs), 6 min walk test, echocardiography, RHC and high-resolution CT.
Figure 1.
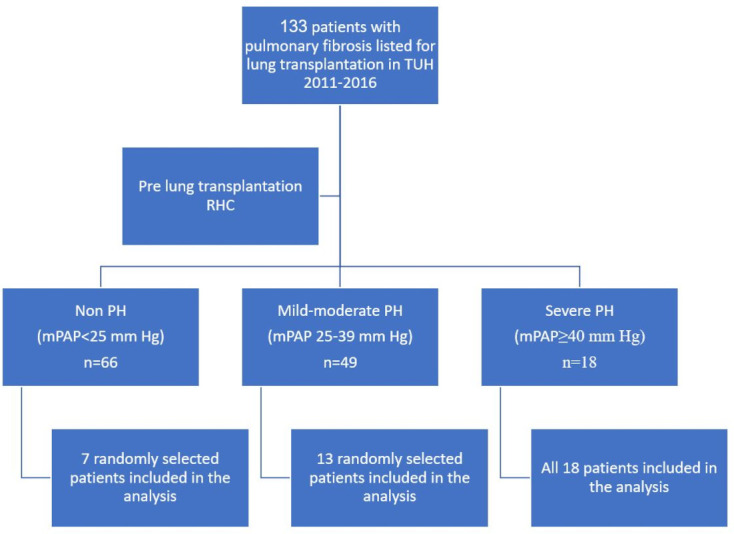
Study design. mPAP, mean pulmonary artery pressure; PH, pulmonary hypertension; RHC, right heart catheterisation; TUH, Temple University Hospital.
Grading of PH severity
PH was classified by pretransplantation RHC values—mPAP and pulmonary arterial wedge pressure (PAWP) according to the recent haemodynamic definitions and updated clinical classification of PH guidelines by the 6th World Symposium on Pulmonary Hypertension Task Force: Precapillary PH defined by mPAP>20 mm Hg and PVR ≥3 Wood units (WU) and PAWP≤15 mm Hg.18 PH severity was graded by mPAP: non-PH—patients with mPAP ≤20 mm Hg; mild/moderate PH—patients with 20<mPAP<40 mm Hg, PVR ≥3 WU and PAWP≤15 mm Hg and severe PH—patients with mPAP ≥40 mm Hg, PVR ≥3 WU and PAWP≤15 mm Hg.18 PVR was available (WU) but was not used for grading of PH severity.
Tissue acquisition procedure
All fixed and frozen tissues were obtained as part of the Lung Tissue Research Consortium (LTRC). The LTRC is sponsored by the American National Heart Lung and Blood Institute and TUH is one of the five clinical centres for LTRC in the USA. The tissues were preserved within 30 min of removal from the patients. Briefly, tissues were placed in liquid N2 and once completely frozen transferred to a container filled with dry ice or a −80°C freezer. Then, it was covered with RNAlater and totally immersed in fixative with 10% neutral buffered formalin. Slides were made with H&E and pentachrome staining from the formalin-fixed specimens from each lobe. All tissue specimens were sent to the Tissue Core Laboratory and stored as follows: RNAlater tissue was aliquoted and stored at −20°C and Flash (snap) frozen tissue was aliquoted and stored at −80°C.
Grading of hypertensive pulmonary vascular disease
Paraffin block specimens were prepared from lung tissue as described above. Sections were visually scored at 10× magnifications. Grading of the pulmonary vasculature was done blinded to the mPAP (author WH) according to Heath and Edwards’s scheme for hypertensive pulmonary vascular disease with progressive structural changes10 (table 1). All vessels seen on each slide were examined. However, vascular grading was applied only to pulmonary arterioles. Venules were examined to rule out signs of pulmonary veno-occlusive disease.
Table 1.
Heath and Edwards’s scheme for hypertensive pulmonary vascular disease with progressive structural changes10
| Grade | Pathology |
| 0 | Normal |
| 1 | Distal extension of muscle into distal arterioles and medial thickening of muscular arteries |
| 2 | Medial hypertrophy with cellular intimal proliferation in small muscular arteries |
| 3 | Progressive fibrous vascular occlusion, concentric intimal fibrosis |
| 4 | Progressive generalised arterial dilatation lesions, including plexiform lesions |
| 5 | Chronic dilatation with medial and intimal fibrosis, prominent plexiform lesions, angiomatoid lesions, pulmonary hemosiderosis |
| 6 | Necrotising arteritis |
Due to the high unexpected frequency of plexiform lesions, a second pathologist (author AA) reviewed all specimens, and only cases that were diagnosed by both pathologists as plexiform lesions were included in the study as such (8/11).
Statistical analysis
Data are presented as mean±SD for continuous variables or counts (percentages) for categorical variables. χ² was used for categorical data, and the paired or unpaired t-test was used for continuous data. The Spearman rank-order correlation coefficient was used to measure the strength and direction of association between continuous and ordinal variables. All data were analysed using SPSS V.12.0 (SPSS, Chicago, Illinois, USA) and Stata 14.0 (Stata, College Station, Texas, USA).
Patient and public involvement statement
Patients or the public were not involved in the design, or conduct, or reporting, or dissemination plans of our research.
This study was conducted in accordance with the amended Declaration of Helsinki. TUH review board approved the protocol, and written informed consent was obtained from all patients (protocol number 24556).
Results
Patients
A total of 38 patients with fibrotic end stage lung disease who had lung transplantation at TUH from 2011 to 2016 were included in the final analysis (figure 1). The average age of the patients was 65±8 years, 26 of them were males and 12 were females. The lung diseases of the patients were diverse, with 21 patients with idiopathic pulmonary fibrosis (IPF), 8 patients with combined pulmonary fibrosis and emphysema (CPFE), 3 patients with connective tissue disease related ILD, 2 patients with chronic hypersensitivity pneumonitis, 2 patients with interstitial pneumonia with autoimmune features, 1 patient with desquamative interstitial pneumonia) and 1 patient with pulmonary Langerhans cell histiocytosis. Their PFTs showed severe restrictive pattern with forced expiratory volume in the first second (FEV1) to forced vital capacity (FVC) ratio of 78%±14% and FVC 53%±19% of predicted, total lung capacity (TLC) 53+15% of predicted and lung diffusion for carbon monoxide (DLCO) of 22%±10% of predicted (table 2).
Table 2.
Patient characteristics grouped by PH severity
| Non-PH (n=7) | Mild-moderate PH (n=13) | Severe PH (n=18) | All patients (n=38) | |
| Age (years) | 67±5 | 67±8 | 61±8 | 65±8 |
| Gender (M/F) | 6/1 | 8/5 | 12/6 | 26/12 |
| FEV1/FVC (%) | 85±6 | 77±14 | 76±16 | 78±14 |
| FEV1* | 54±15 | 55±17 | 54±21 | 54±18 |
| FVC* | 47±11 | 55±19 | 56±22 | 53±19 |
| TLC* | 48±12 | 50±16 | 58±16 | 53±15 |
| RV* | 41±16 | 47±29 | 59±20 | 51±23 |
| DLCO* | 27±14 | 24±11 | 21±9 | 22±10 |
| mPAP (mm Hg) | 17±3† | 26±2† | 49±12† | 35±16 |
| PVR (WU) | 2.76±1.4 | 3.37±1.14 | 9.13±6.09‡ | 5.9±5.1 |
*Per cent of predicted.
†Statistically significant between all groups comparisons.
‡Statistically significant between none and mild/moderate to severe PH groups.
DLCO, lung diffusion of carbon monoxide; FEV1, forced expiratory volume in the first second; FVC, forced vital capacity; mPAP, mean pulmonary artery pressure; PH, pulmonary hypertension; PVR, pulmonary vascular resistance; RV, residual volume; TLC, total lung capacity; WU, Wood units.
Pulmonary hypertension data
All patients had prelung transplant RHC. Patients were grouped by pretransplant PH severity derived from RHC measurement: 18 patients had severe PH with mPAP of 49±12 mm Hg, 13 patients had mild/moderate PH with mPAP of 26±2 mm Hg and 7 patients did not have PH (non-PH group) with mPAP of 17±3 mm Hg (p<0.0001 for all between groups comparisons). Age, gender and PFTs of all three groups were not statistically different (table 2). PVR was 9.1±6 WU for the severe PH group, 3.4±1.1 WU for the mild/moderate PH group and 2.8±1.4 WU for the non-PH group (p<0.01 for comparison of severe to mild-moderate and non-PH groups).
Vasculature pathology grade
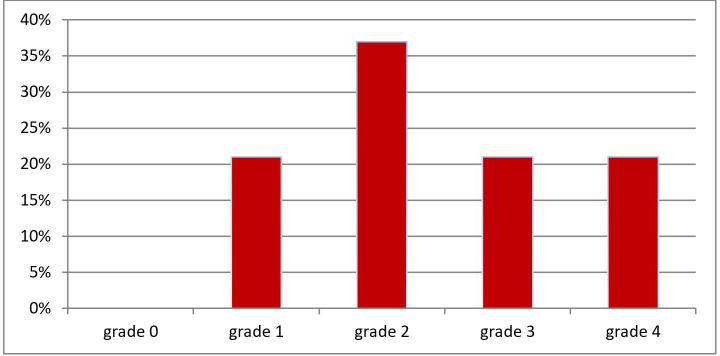
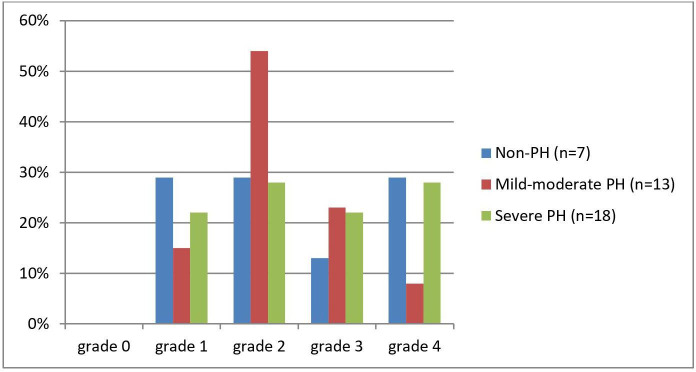
All 38 patients had pulmonary artery histopathological changes ranging from grade 1 (distal extension of muscle into distal arterioles and medial thickening of muscular arteries) to grade 4 (progressive generalised arterial dilatation lesions, including plexiform lesions) (figure 2). 14 of 38 (37%) had grade 2 (medial hypertrophy with cellular intimal proliferation in small muscular arteries). Sixteen of 38 (42%) had grade 3 (progressive fibrous vascular occlusion, concentric intimal fibrosis) and/or grade 4 changes (figure 3). The mean vasculature pathology grade was 2.42±1.05 with no significant difference between all three groups of PH severity. There was no correlation between the presence and severity of PH (mPAP and PVR) and the severity of the vasculature pathology grade (Spearman’s rho=0.14, p=0.34 and Spearman’s rho=0.018, p=0.91, respectively, figure 4). There was also no correlation between the DLCO and the severity of the vasculature pathology grade (Spearman’s rho=0.11, p=0.49). Pulmonary venules in each slides were examined for signs of veno-occlusive disease which were not seen in any patient.
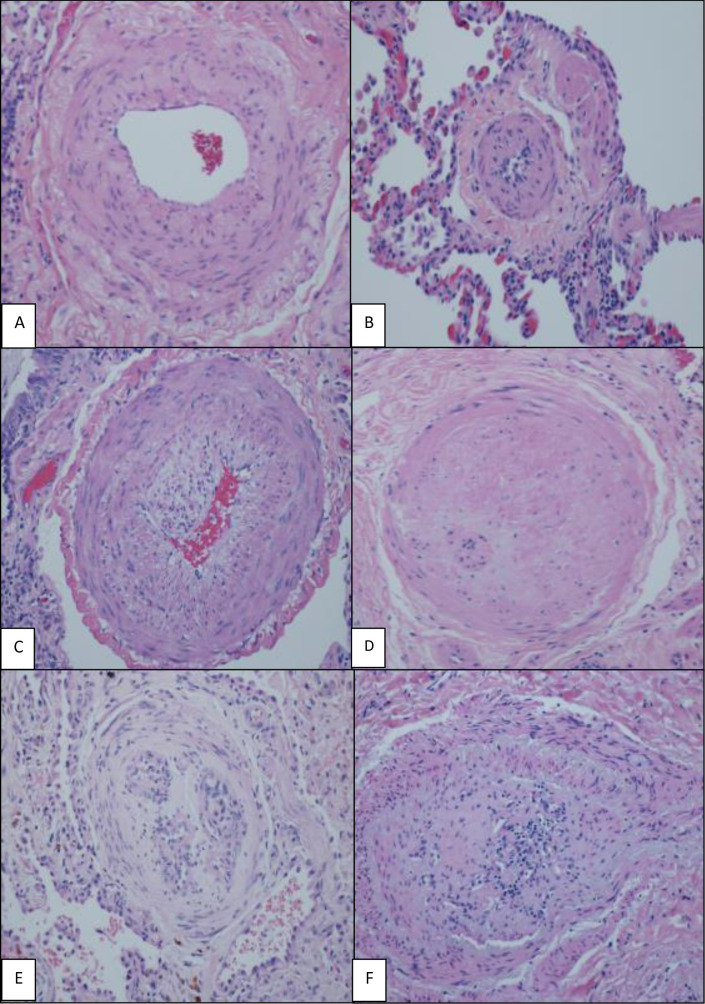
Figure 2.
H&E (×200), various grades of histological changes (A–F). (A) Muscular artery with medial hypertrophy (increased number of smooth muscle nuclei arranged in parallel around the lumen). (B) Muscularisation of arterioles (thick muscle layer in arterial wall composed of numerous smooth muscle cells with closely spaced nuclei). (C) Intimal proliferation and fibrosis in addition to medial hypertrophy. (D) Concentric intimal fibrosis resulting in circumferential luminal narrowing. (E, F) Plexiform lesions; concentric intimal fibrosis causing near luminal obliteration and multiple small vascular spaces and expansion and partial destruction of the arterial wall with extension of the lesion into the perivascular connective tissue.
Figure 3.
Pulmonary vasculopathy grades for all patients (n=38). Briefly, Grade 0—normal; Grade 1—medial thickening; Grade 2—medial hypertrophy; Grade 3—concentric intimal fibrosis; Grade 4—plexiform lesions (for full description, see Heath and Edwards scheme, table 1).
Figure 4.
Pulmonary vasculopathy grades by PH severity (none, mild-moderate and severe PH). Briefly, Grade 0—normal; Grade 1—medial thickening; Grade 2—medial hypertrophy; Grade 3—concentric intimal fibrosis; Grade 4—plexiform lesions (for full description, see Heath and Edwards scheme, table 1). PH, pulmonary hypertension.
Plexiform lesions
Eight of 38 (21%) patients had plexiform pulmonary arterial lesions. Plexiform lesions were evident in all three PH severity groups: 2 of 7 non-PH, 1 of 13 mild/moderate PH and 5 of 18 severe PH. A comparison of patients with plexiform lesions (n=8, grade 4) to patients without plexiform lesions (n=30, grades 1–3) showed no statistically significant differences in pulmonary haemodynamics or clinical data including age, gender, PFTs and RHC data (table 3).
Table 3.
Comparison of patients’ characteristics between patients with and without plexiform lesions
| Patients with plexiform lesions (n=8) | Patients without plexiform lesions (n=30) | |
| Age (years) | 65±7 | 63±11 |
| Gender (M/F) | 6/2 | 20/10 |
| Lung disease (IPF/non-IPF) | 2/6 | 13/17 |
| FEV1/FVC (%) | 78±15 | 81±13 |
| FEV1* | 55±18 | 53±22 |
| FVC* | 54±18 | 52±23 |
| TLC* | 53±17 | 56±12 |
| RV* | 50±24 | 59±21 |
| DLCO* | 21±9 | 28±14 |
| mPAP (mm Hg) | 33±12 | 43±25 |
| PVR (WU) | 5±3 | 9±10 |
| H&E vascular grade | 4 | 2±0.7† |
*Per cent of predicted.
†Statistically significant.
DLCO, lung diffusion of carbon monoxide; FEV1, forced expiratory volume in the first second; H&E, Heath and Edwards pulmonary vasculopathy grades; IPF, idiopathic pulmonary fibrosis; mPAP, mean pulmonary artery pressure; PVR, pulmonary vascular resistance; RV, residual volume; TLC, total lung capacity; WU, Wood units.
Pulmonary vasodilators and antifibrotic therapy data
Eight of 38 (21%) patients were taking pulmonary vasodilator medication prior to lung transplant. Therapy included phosphodiesterase-5 (PDE-5) inhibitor (n=7), combination PDE-5 and endothelin receptor antagonist (n=4) and 1 prostanoid +dual therapy. As expected, mPAP was significantly higher in the group on baseline PH therapy (51.5±15.2 vs 30.7±13.2 mm Hg, p=0.002) as was PVR (9.89±6.46 vs 4.76±4.08 WU, p=0.04). Ten patients (26%) were taking antifibrotic therapy prior to lung transplant: pirfenidone (7/10) and nintedanib (3/10). Those taking antifibrotics had significantly lower mPAP and PVR (25.7±8.4 vs 39.3±16.7 mm Hg, p=0.001 and 4.22±2.5 vs 6.69±5.9 WU, p=0.04, respectively).
Discussion
Our study showed that patients with end stage fibrotic ILD undergoing lung transplantation had significant and often severe pulmonary arterial vasculopathy in their explanted lungs. Unexpectedly, this arterial vasculopathy was present in lungs from patients with and without PH and had no correlation to the clinical severity of the underlying lung disease. To the best of our knowledge, this is the first study to describe a high frequency of severe vascular changes in advanced fibrotic ILD, with almost half of the patients showing vascular occlusion with intimal fibrosis and one-fifth showing plexiform lesions which are traditionally considered a hallmark only of WHO group 1 iPAH pathology.
Our patients with PH are classified as WHO Group 3, PH secondary to hypoxemic lung disease. One of the most important factors contributing to pulmonary arterial changes in patients with ILD is chronic hypoxia, which is a part of the terminology of WHO group 3 (PH due to lung diseases and/or hypoxia). Chronic hypoxia affects all three layers of the pulmonary vasculature: the intima, media and adventitia and their harbouring cells—the endothelial cells (EC), smooth muscle cells (SMC) and fibroblasts, respectively.19 However, hypoxia alone does not usually lead to high-grade vascular remodelling with intimal obliteration and plexiform lesions as seen in iPAH.20
Plexiform lesions are networks of vascular micro vessels that consist of two distinct populations of EC: normal phenotype that lines vessels and the proliferating, apoptosis-resistant phenotype at the core of the lesion.21 22 They are considered the hallmark of severe iPAH and were first described in 1927.12 23,12 In 1989, a landmark study by Pietra et al, of 48 patients with iPAH documented plexiform lesions in 52% of the total cohort.12 This study also demonstrated that presence of plexiform lesions portended a poorer prognosis. In 2012, Stacher et al evaluated explanted lungs from 62 patients with group 1 PAH and documented plexiform lesions in 90% overall and in all of 48 patients with idiopathic group 1 iPAH.11
Data obtained by computerised three-dimensional reconstructions of serial lung sections from patients with PH, suggested that a single plexiform lesion can occlude the entire length of an affected vessel, contributing to PH severity.21
Historically, pulmonary arterial vascular changes are less well documented and infrequently described in patients with fibrotic ILD. A Japanese lung necropsy study of 60 patients with emphysema, IPF or CPFE reported plexiform arterial lesions in 2 patients with CPFE and 1 patient with IPF and none in emphysema.16 In a similar study of explanted lungs of 70 patients transplanted for end stage COPD (chronic obstructive pulmonary disease), only 1 patient had plexiform lesions.17 Our data demonstrated much more common advanced vasculopathy including plexiform lesions in end stage fibrotic ILD lung explants obtained at time of transplantation.
Our hypothesis was that patients with severe PH would have more severe pulmonary arterial vascular changes but not plexiform lesions seen in group 1 PAH. We were expecting positive correlation between mPAP and pulmonary artery vasculopathy grade and only mild to moderate vascular changes. However, pretransplantation measured mPAP and DLCO failed to predict which patients had pulmonary arterial pathological changes. In addition, we found unexpectedly severe vascular change and a high prevalence of plexiform arterial lesions in patients with normal directly measured pulmonary pressures. We found that severe pulmonary arterial vasculopathy was common in patients with end stage fibrotic ILD and that these changes could not be predicted clinically before lung transplantation. The significance of these and our data is unclear. Is the presence of plexiform arterial lesions in fibrotic ILD an indicator a causal role for the pulmonary arterial vasculopathy in clinical ILD disease progression or if simply a morphological epimarker of the irreversible parenchymal distortion seen in end-stage fibrotic ILD?22 24–26 We speculate about possible explanations:
Geographic and temporal heterogeneity in pulmonary arterial vascular changes throughout the lung. Since the geographic distribution of parenchymal pathology is uneven within the lung, there might be significant heterogeneity in the distribution and severity of the vascular changes. In some patients, we may have found signs of severe local vasculopathy that had yet to cause a significant effect on the PVR as measured in RHC. This idea is supported by previous findings in iPAH histopathology regarding notable heterogeneity in the number and distribution patterns of plexiform lesions within a given PAH lung and between patients with PAH. This occurred without relation to other parameters of vascular remodelling or haemodynamics.11 25 Even if true, this does not account for advanced arterial vasculopathy and of plexiform lesions as a response to chronic hypoxia. Chronic hypoxic changes have been described to cause intimal fibrosis and medial and adventitial thickening, but not higher-grade vascular remodelling including plexiform lesions.27
Shared pathogenic mechanisms between fibrosis and pulmonary arterial vasculopathy. Many mediators including endothelin, VEGF (vascular endothelial growth factor), TGF-β (transfroming growth factor β), NO (nitric oxide), PGE2 (prostaglandin E2), BMPR2 (bone morphogenic protein receptor type 2) and IL-6 (interleukin 6) have been shown to play important roles in both the progression of fibrosis and the development of PH.28 The possibility of shared pathogenic mechanisms between IPF and PH was also demonstrated through microarray gene expression; patients with IPF patients, like patients with PH show an exaggerated expression of mediators of SMC and EC proliferation compared with controls, suggesting the existence of preclinical pulmonary vascular disease.29 The patients end stage fibrotic lung disease theoretically might have caused vascular changes unrelated to clinically measured PH by mPAP in RHC. In other words, the presence of the severe vascular changes might represent end stage lung disease rather than severe PH.
Interestingly, patients who were treated with antifibrotics before lung transplant had significantly lower mPAP and PVR. The role of pirfenidone and nintedanib in patients with IPF and PH is not clear since no data on these agents are currently available. Tyrosine kinase inhibitors such as Imatinib and nintedanib have shown to improve exercise capacity and haemodynamics in patients with advanced WHO group 1 PAH. Pirfenidone which combines antiproliferative and anti-inflammatory activity may have similar effects. However, no data currently support this hypothesis.30
There is no known effective therapy to prevent or treat PH in fibrotic ILD and treatment with pulmonary vasodilators is not recommended based on multiple clinical trials.31–44 Further molecular, biochemical and clinical characterisation subgroup of patients with ILD and high-grade vascular changes might have an important mechanistic, clinical and therapeutic significance. Clinical data including directly measured pulmonary haemodynamics failed to indicate patients at risk for pulmonary arterial vascular pathology. This highlights the challenges in identification of patients with fibrotic ILD who could potentially benefit from future therapeutic interventions.
Our study has several limitations. First, this is a retrospective study that has inherent limitations in patient selection. Second, despite our relatively large sample size as compared with other studies with explanted lungs, the size is still small with inherently reduced statistical power. Third, sampling error is possible and may underestimate the degree of significant vascular changes, especially with disease that is patchy in nature; however, we also view this as strength of our research as this may explain why plexiform pulmonary arterial vasculopathy has yet been better described in end stage ILD.
In summary, we found significant pulmonary arterial vasculopathy in patients with end stage ILD. The vasculopathy did not correlate with the clinical severity of the underlying lung disease and did not correlate with the presence and/or severity of PH as measured by RHC. We found a significant number of patients with end stage lung disease (21%) with plexiform lesions which are traditionally a hallmark of WHO group 1 PAH. The observed vasculopathy might be derived from severe and prolonged hypoxia in the complex biochemical environment of the diseased lung that involve mechanisms similar to those seen with WHO group 1 PAH. These findings indicate that advanced pulmonary arteriopathy is common and may develop in a heterogeneous regional pattern in advanced lung disease prior to the clinical detection of PH. Larger scales studies are needed to confirm our findings and conclusions.
Footnotes
Contributors: YD collected the data and is the guarantor of the article, taking responsibility for the integrity of the work as a whole from inception to published article. AG collected the data. JS and GD helped write the manuscript. HW, AA and BC reviewed the pathology studies. HZ conducted the statistical analysis. CD reviewed the imaging studies. NM, FCC, GC and AJM were the transplant pulmonologists for the patients included in the study, conducted the pretransplantation evaluation and treated the patients before and after lung transplantation. AJM was a primary coauthor, responsible for the study concept and helped write the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available on reasonable request. All data relevant to the study are included in the article or uploaded as supplementary information. All data relevant to the study are included in the article or uploaded as supplementary information. All data are deidentified participant data. Data are available on reasonable request from the corresponding author, Dr. Yaniv Dotan, at yaniv.dotan@sluhn.org.
References
- 1.Caminati A, Cassandro R, Harari S. Pulmonary hypertension in chronic interstitial lung diseases. Eur Respir Rev 2013;22:292–301. 10.1183/09059180.00002713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lettieri CJ, Nathan SD, Barnett SD, et al. Prevalence and outcomes of pulmonary arterial hypertension in advanced idiopathic pulmonary fibrosis. Chest 2006;129:746–52. 10.1378/chest.129.3.746 [DOI] [PubMed] [Google Scholar]
- 3.Minai OA, Chaouat A, Adnot S. Pulmonary hypertension in COPD: epidemiology, significance, and management: pulmonary vascular disease: the global perspective. Chest 2010;137:39S–51. [DOI] [PubMed] [Google Scholar]
- 4.Andersen KH, Iversen M, Kjaergaard J, et al. Prevalence, predictors, and survival in pulmonary hypertension related to end-stage chronic obstructive pulmonary disease. J Heart Lung Transplant 2012;31:373–80. 10.1016/j.healun.2011.11.020 [DOI] [PubMed] [Google Scholar]
- 5.Shorr AF, Wainright JL, Cors CS, et al. Pulmonary hypertension in patients with pulmonary fibrosis awaiting lung transplant. Eur Respir J 2007;30:715–21. 10.1183/09031936.00107206 [DOI] [PubMed] [Google Scholar]
- 6.Scharf SM, Iqbal M, Keller C, et al. Hemodynamic characterization of patients with severe emphysema. Am J Respir Crit Care Med 2002;166:314–22. 10.1164/rccm.2107027 [DOI] [PubMed] [Google Scholar]
- 7.Chaouat A, Bugnet A-S, Kadaoui N, et al. Severe pulmonary hypertension and chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2005;172:189–94. 10.1164/rccm.200401-006OC [DOI] [PubMed] [Google Scholar]
- 8.Harari S. Out of proportion pulmonary hypertension: a paradigm for rare disease. Chest 2012;142:1087–8. [DOI] [PubMed] [Google Scholar]
- 9.Seeger W, Adir Y, Barberà JA, et al. Pulmonary hypertension in chronic lung diseases. J Am Coll Cardiol 2013;62:D109–16. 10.1016/j.jacc.2013.10.036 [DOI] [PubMed] [Google Scholar]
- 10.Heath D, Edwards JE. The pathology of hypertensive pulmonary vascular disease; a description of six grades of structural changes in the pulmonary arteries with special reference to congenital cardiac septal defects. Circulation 1958;18:533–47. 10.1161/01.cir.18.4.533 [DOI] [PubMed] [Google Scholar]
- 11.Stacher E, Graham BB, Hunt JM, et al. Modern age pathology of pulmonary arterial hypertension. Am J Respir Crit Care Med 2012;186:261–72. 10.1164/rccm.201201-0164OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pietra GG, Edwards WD, Kay JM, et al. Histopathology of primary pulmonary hypertension. A qualitative and quantitative study of pulmonary blood vessels from 58 patients in the National heart, lung, and blood Institute, primary pulmonary hypertension registry. Circulation 1989;80:1198–206. 10.1161/01.CIR.80.5.1198 [DOI] [PubMed] [Google Scholar]
- 13.Romberg E. Über sklerose Der lungenarterie. Dtsch Arch Klin Med 1891;48:197–206. [Google Scholar]
- 14.Wagenvoort CA, Wagenvoort N. Primary pulmonary hypertension: a pathologic study of the lung vessels in 156 clinically diagnosed cases. Circulation 1970;42:1163–84. [Google Scholar]
- 15.Farkas L, Gauldie J, Voelkel NF, et al. Pulmonary hypertension and idiopathic pulmonary fibrosis: a tale of angiogenesis, apoptosis, and growth factors. Am J Respir Cell Mol Biol 2011;45:1–15. [DOI] [PubMed] [Google Scholar]
- 16.Awano N, Inomata M, Ikushima S, et al. Histological analysis of vasculopathy associated with pulmonary hypertension in combined pulmonary fibrosis and emphysema: comparison with idiopathic pulmonary fibrosis or emphysema alone. Histopathology 2017;70:896–905. 10.1111/his.13153 [DOI] [PubMed] [Google Scholar]
- 17.Carlsen J, Hasseriis Andersen K, Boesgaard S, et al. Pulmonary arterial lesions in explanted lungs after transplantation correlate with severity of pulmonary hypertension in chronic obstructive pulmonary disease. J Heart Lung Transplant 2013;32:347–54. 10.1016/j.healun.2012.11.014 [DOI] [PubMed] [Google Scholar]
- 18.Simonneau G, Montani D, Celermajer DS, et al. Haemodynamic definitions and updated clinical classification of pulmonary hypertension. Eur Respir J 2019;53:1801913 https://doi.org/ 10.1183/13993003.01913-2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pugliese SC, Poth JM, Fini MA, et al. The role of inflammation in hypoxic pulmonary hypertension: from cellular mechanisms to clinical phenotypes. Am J Physiol Lung Cell Mol Physiol 2015;308:L229–52. 10.1152/ajplung.00238.2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guignabert C, Dorfmuller P. Pathology and pathobiology of pulmonary hypertension. Semin Respir Crit Care Med 2013;34:551–9. 10.1055/s-0033-1356496 [DOI] [PubMed] [Google Scholar]
- 21.Cool CD, Stewart JS, Werahera P, et al. Three-Dimensional reconstruction of pulmonary arteries in plexiform pulmonary hypertension using cell-specific markers. Evidence for a dynamic and heterogeneous process of pulmonary enodthelial cell growth. Am J Pathol 1999;155:411–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jonigk D, Golpon H, Bockmeyer CL, et al. Plexiform lesions in pulmonary arterial hypertension composition, architecture, and microenvironment. Am J Pathol 2011;179:167–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moschcowitz Eli. Hypertension of the pulmonary circulation. Am J Med Sci 1927;174:388–405. 10.1097/00000441-192709000-00010 [DOI] [Google Scholar]
- 24.Abe K, Toba M, Alzoubi A, et al. Formation of plexiform lesions in experimental severe pulmonary arterial hypertension. Circulation 2010;121:2747–54. 10.1161/CIRCULATIONAHA.109.927681 [DOI] [PubMed] [Google Scholar]
- 25.Tuder RM, Stacher E, Robinson J, et al. Pathology of pulmonary hypertension. Clin Chest Med 2013;34:639–50. 10.1016/j.ccm.2013.08.009 [DOI] [PubMed] [Google Scholar]
- 26.St. Croix CM, Steinhorn RH. New thoughts about the origin of plexiform lesions. Am J Respir Crit Care Med 2016;193:484–5. 10.1164/rccm.201510-1959ED [DOI] [PubMed] [Google Scholar]
- 27.Stenmark KR, Meyrick B, Galie N, et al. Animal models of pulmonary arterial hypertension: the hope for etiological discovery and pharmacological cure. Am J Physiol Lung Cell Mol Physiol 2009;297:L1013–32. 10.1152/ajplung.00217.2009 [DOI] [PubMed] [Google Scholar]
- 28.Collum SD, Amione-Guerra J, Cruz-Solbes AS, et al. Pulmonary hypertension associated with idiopathic pulmonary fibrosis: current and future perspectives. Can Respir J 2017;2017:1–12. 10.1155/2017/1430350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Patel NM, Kawut SM, Jelic S, et al. Pulmonary arteriole gene expression signature in idiopathic pulmonary fibrosis. Eur Respir J 2013;41:1324–30. 10.1183/09031936.0084112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Harari S, Elia D, Humbert M. Pulmonary hypertension in parenchymal lung diseases: any future for new therapies? CHEST 2018;153:217–23. [DOI] [PubMed] [Google Scholar]
- 31.Stolz D, Rasch H, Linka A, et al. A randomised, controlled trial of bosentan in severe COPD. Eur Respir J 2008;32:619–28. 10.1183/09031936.00011308 [DOI] [PubMed] [Google Scholar]
- 32.Blanco I, Gimeno E, Munoz PA, et al. Hemodynamic and gas exchange effects of sildenafil in patients with chronic obstructive pulmonary disease and pulmonary hypertension. Am J Respir Crit Care Med 2010;181:270–8. 10.1164/rccm.200907-0988OC [DOI] [PubMed] [Google Scholar]
- 33.Idiopathic Pulmonary Fibrosis Clinical Research Network, Zisman DA, Schwarz M, et al. A controlled trial of sildenafil in advanced idiopathic pulmonary fibrosis. N Engl J Med 2010;363:620–8. 10.1056/NEJMoa1002110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Blacno I, Santos S, Gea J, et al. Sildenafil to improve respiratory rehabilitation outcomes in COPD: a controlled trial. Eur Respir J 2013;42:982–92. [DOI] [PubMed] [Google Scholar]
- 35.Goudie AR, Lipworth BJ, Hopkinson PJ, et al. Tadalafil in patients with chronic obstructive pulmonary disease: a randomised, double-blind, parallel-group, placebo-controlled trial. Lancet Respir Med 2014;2:293–300. 10.1016/S2213-2600(14)70013-X [DOI] [PubMed] [Google Scholar]
- 36.Lederer DJ, Bartels MN, Schluger NW, et al. Sildenafil for chronic obstructive pulmonary disease: a randomized crossover trial. COPD 2012;9:268–75. 10.3109/15412555.2011.651180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.King TE, Behr J, Brown KK, et al. BUILD-1: a randomized placebo-controlled trial of bosentan in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 2008;177:75–81. 10.1164/rccm.200705-732OC [DOI] [PubMed] [Google Scholar]
- 38.King TE, Brown KK, Raghu G, et al. BUILD-3: a randomized, controlled trial of bosentan in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 2011;184:92–9. 10.1164/rccm.201011-1874OC [DOI] [PubMed] [Google Scholar]
- 39.Raghu G, Behr J, Brown KK, et al. Treatment of idiopathic pulmonary fibrosis with ambrisentan: a parallel, randomized trial. Ann Intern Med 2013;158:641–9. [DOI] [PubMed] [Google Scholar]
- 40.Raghu G, Million-Rousseau R, Morganti A, et al. Macitentan for the treatment of idiopathic pulmonary fibrosis: the randomised controlled music trial. Eur Respir J 2013;42:1622–32. 10.1183/09031936.00104612 [DOI] [PubMed] [Google Scholar]
- 41.Corte TJ, Keir GJ, Dimopoulos K, et al. Bosentan in pulmonary hypertension associated with fibrotic idiopathic interstitial pneumonia. Am J Respir Crit Care Med 2014;190:208–17. 10.1164/rccm.201403-0446OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Badesch DB, Feldman J, Keogh A, et al. ARIES-3: ambrisentan therapy in a diverse population of patients with pulmonary hypertension. Cardiovasc Ther 2012;30:93–9. 10.1111/j.1755-5922.2011.00279.x [DOI] [PubMed] [Google Scholar]
- 43.Rietema H, Holverda S, Bogaard HJ, et al. Sildenafil treatment in COPD does not affect stroke volume or exercise capacity. Eur Respir J 2008;31:759–64. 10.1183/09031936.00114207 [DOI] [PubMed] [Google Scholar]
- 44.Shlobin OA, Brown AW, Nathan SD. Pulmonary hypertension in diffuse parenchymal lung diseases. Chest 2017;151:204–14. 10.1016/j.chest.2016.08.002 [DOI] [PubMed] [Google Scholar]