Abstract
Objective
To evaluate the clinical reliability and validity of the Chinese version of the Patient Health Questionnaire-9 (C-PHQ-9) in patients with psoriasis.
Design
Cross-sectional study.
Setting
Tertiary care centre.
Participants
Patients with psoriasis who have not been diagnosed with depression (n=148; mean age 43.37±17.46 years; 31.19% female).
Primary and secondary outcome measures
The primary outcome measures considered in this study were the C-PHQ-9 and the Hamilton Depression Scale (HAMD). The American Diagnostic and Statistical Manual of Mental Disorders Fifth Edition (DSM-V) was used as the gold standard for the diagnosis of depression. Cronbach’s α and test–retest reliability after 1 week were evaluated using reliability analysis, and criterion and structural validity were assessed using validity analysis. Receiver operating characteristic (ROC) analysis was performed to identify the best demarcation score and diagnostic accuracy.
Results
Compared with DSM-V (27.27%), both C-PHQ-9 (39.19%) and HAMD (31.01%) had higher rates for detecting depression. The mean completion time for C-PHQ-9 evaluation (2.02±0.84 min) was significantly less than that for HAMD (23.37±3.21 min, p<0.001). The Cronbach’s α coefficient for the C-PHQ-9 was 0.938. The correlation coefficients of the nine items with the total scale ranged from 0.540 to 0.854, and the mean inter-item correlation coefficients ranged from 0.376 to 0.933. After a week, the retest coefficient was 0.955 (p<0.01). Principal component factor analysis showed that C-PHQ-9 identified a unifactorial structure. The best cut-off point was 9 points, with a sensitivity of 98.00% and a specificity of 90.80%. The area under the ROC curve was 0.979 (95% CI 0.968 to 0.991).
Conclusion
C-PHQ-9 has good reliability and validity in patients with psoriasis and can be used for primary screening of patients with psoriasis and depression. This scale has obvious time and labour advantages over the HAMD and should be considered for use in clinical practice.
Keywords: C-PHQ-9, reliability, validity, psoriasis, depression
Strengths and limitations of this study.
The main strength of this study is that all patients with psoriasis were assessed using the gold standard tool (Diagnostic and Statistical Manual of Mental Disorders Fifth Edition) for evaluating depression.
The Chinese version of the Patient Health Questionnaire-9 (C-PHQ-9) was also innovatively applied to patients with psoriasis.
The time to complete the C-PHQ-9 and the Hamilton Depression Scale was also assessed.
The study was limited by its small sample size.
The study was also limited by its cross-sectional and single-centre design.
Introduction
Psoriasis is a chronic inflammatory systemic disease with a strong genetic predisposition and autoimmune pathogenic traits affecting about 2% of the population.1 Psoriasis is characterised by hyperproliferation of the epidermis, resulting in thick, red, scaly lesions.2 Itchiness, skin flaking, swelling, redness, pain and other manifestations frequently accompany the lesions, and the arthritic complications of the disease can cause pain and lead to loss of mobility and even disability.3 Although the pathogenesis of psoriasis is not clear, it is currently believed to be mainly related to genetics, immunity, oxidative stress, inflammatory response and environment.4 Psoriasis typically affects the skin, but may also affect the joints and has been associated with a number of diseases. A study revealed that depression is a common complication of psoriasis, with an incidence of about 22.1%.1 The impact of psoriasis on psychological and mental health is currently an important consideration due to the implications of the disease on social well-being and treatment. Patients with psoriasis have an increased prevalence of depression and anxiety and suicidal ideation. Interestingly, psoriasis treatment leads to improvement in symptoms of anxiety.5 6 Dantzer et al7 proposed a hypothesis on inflammatory cytokines for depression through a large number of animal experiments and clinical observations. Activated immune inflammatory pathways are now thought to be involved in the development of depression. Some proinflammatory factors such as interleukin-1, tumour necrosis factor-α and interferon-γ can cause psoriasis and also play an important role as neurotransmitters in depression.7 The inflammatory response may be a common pathway for depression in patients with psoriasis.
Currently, there are more than 10 kinds of assessment scales for clinical depression. Different studies have shown that different assessment scales have different detection rates for depression.8 The most widely used is the Hamilton Depression Scale (HAMD). However, due to its complexity and need for professional input, it requires more labour and time. The Chinese version of the Patient Health Questionnaire-9 (C-PHQ-9) is a self-evaluation tool for the diagnosis and assessment of depression based on the major disorder of the Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition) (DSM-IV).9
With the emergence of novel biological agents, most psoriasis can now be effectively controlled. However, because biological agents are expensive, most patients with psoriasis do not use biologics and so their symptoms are not effectively controlled. The symptoms of psoriasis have a profound impact on the patient’s quality of life, and patients often experience depression, anxiety and even suicidal behaviour. These adverse emotions can further aggravate the condition of patients with psoriasis, through the nervous-endocrine system and the nervous-immune system, forming a vicious circle. The ‘neurotransmitter hypothesis’ suggests that neurotransmitters such as norepinephrine and dopamine are abnormally expressed in patients with depression. These neurotransmitters are important components of the neuroendocrine-immunomodulatory system which can regulate the phagocytosis and proliferation activity of lymphocytes and macrophages and may promote the occurrence and development of psoriasis. Therefore, clinicians should screen and identify patients with psoriasis early and develop individualised psychosomatic treatment programmes to adapt to the biopsychosocial model under the new situation. However, in the dermatology clinic, the diagnosis of depression is difficult for healthcare practitioners who are not qualified psychiatrists. In particular, professional, complex and time-consuming survey scales make such diagnoses more difficult to achieve. Therefore, it is necessary to identify an accurate and simple depression screening tool. Considering these, this study aimed to evaluate the clinical reliability and validity of the Chinese version of the C-PHQ-9 in screening for depression in patients with psoriasis.
Methods
Study design
This is a cross-sectional study. Written consent for use of clinical data in aggregate form was obtained from all patients after they were informed about the study procedures. In this observational study, 148 patients with psoriasis were included from the outpatient and inpatient departments of the Affiliated Hospital of Southwest Medical University from January to February 2018. The diagnosis of depression was made by a psychiatrist using the American DSM-V, which is considered the gold standard for assessing depression. The psychiatrist determined each patient’s HAMD score. The PHQ-9 is a self-evaluation tool for the major disorder based on the criteria of the DSM-IV. Every patient from the sample group who had an additional previous diagnosis of depression completed a questionnaire we created, which aimed to evaluate the C-PHQ-9 score, sociological data and treatment satisfaction. The designated personnel received standardised training to follow specific instructions to guide patients in completing the questionnaire and assessment. After reading the questionnaire, the C-PHQ-9 was carefully and completely filled out by each patient. HAMD and DSM-V were assessed by two attending physicians. The psychiatrist completed the assessment and recorded the time it took to complete each questionnaire.
Measurements
The assessment range for C-PHQ-9 considers only the time period within the previous 2 weeks, with each symptom having a possible score of 0–3 points (0=no, 1=a few days, 2=more than half of the days, 3=almost every day). The total score of the scale is 27 points, with 0–4 points indicating absence of depression, 5–9 points mild depression, 10–14 points moderate depression, and 15–27 points severe depression.
A 17-item version of HAMD was used in this study, with a total score of 0–7 points indicative of no depression, 8–17 points mild depression, 18–24 points moderate depression, and >24 points severe depression.
As noted, DSM-V was used as the gold standard for the diagnosis of depression. These questionnaires were collected by the same trained physician to avoid selection bias.
Statistical analysis
In this cross-sectional study, data were processed and analysed using SPSS V.20.0. Listwise deletions were carried out to manage missing values. Subgroup analysis was used to control for confounding factors. Quantitative data are presented as mean±SD, and count data are expressed as percentages. To calculate the internal consistency of HAMD and C-PHQ-9, we used Cronbach’s α. To derive the optimal cut-off points for HAMD and C-PHQ-9, we performed receiver operating characteristic (ROC) analysis. We compared the areas under the ROC curves (AUCs) to determine the respective abilities of HAMD and C-PHQ-9 in diagnosing depression. In all tests, statistical significance was defined as p<0.05.
Patient and public involvement
Patients with psoriasis were included from the outpatient and inpatient departments of the Affiliated Hospital of Southwest Medical University from January to February 2018. Patients with psoriasis were evaluated by professional dermatologists and met the clinical diagnostic criteria for psoriasis. All subjects signed the informed consent form. The sample size was determined by retrieving previous studies.
Results
Patient characteristics
A total of 150 questionnaires were distributed in this study, and 148 valid questionnaires were collected (response rate 98.67%). Each patient met the diagnostic criteria for psoriasis, and there were no other confounding factors such as systemic diseases and mental illness with a clear diagnosis. The study sample comprised 90 male (60.81%) and 58 female (31.19%) patients, with a mean age of 43.37±17.46 (range 18–85) years. The mean disease course was 9.63±7.85 (range 0.5–43) years. Table 1 outlines the sociodemographic variables considered in the study and the rate of depression with respect to each of these variables.
Table 1.
Patient characteristics
| Variables | Patients with psoriasis (n) | C-PHQ-9(+) (n) | Positive rate (%) | X2 value | P value |
| Gender | 0.009 | 0.926 | |||
| Male | 90 | 35 | 38.89 | ||
| Female | 58 | 23 | 39.66 | ||
| Age (years) | 0.032 | 0.858 | |||
| ≤60 | 126 | 49 | 33.56 | ||
| >60 | 22 | 9 | 40.91 | ||
| Disease duration (years) | 8.984 | 0.003 | |||
| ≤10 | 91 | 27 | 29.67 | ||
| >10 | 57 | 31 | 54.39 | ||
| Marital status | 0.814 | 0.666 | |||
| Unmarried | 44 | 15 | 34.09 | ||
| Married | 100 | 41 | 41 | ||
| Divorced or widowed | 4 | 2 | 50 | ||
| Educational level | 1.334 | 0.248 | |||
| Junior high school and below | 91 | 39 | 42.86 | ||
| High school and above | 57 | 19 | 33.33 | ||
| Place of residence | 0.613 | 0.434 | |||
| City | 58 | 25 | 43.1 | ||
| Rural | 90 | 33 | 36.67 |
C-PHQ-9, Chinese version of the Patient Health Questionnaire-9.
Subanalyses with men and women
To help identify populations where C-PHQ-9 can be particularly useful, subanalyses based on disease duration were conducted in men and women. The results in tables 2 and 3 showed no statistically significant difference in the incidence of depression between men and women with the same disease duration (p>0.05).
Table 2.
Depression rate between men and women with disease duration ≤10 years
| Disease duration ≤10 years | ||||
| Patients with psoriasis | C-PHQ-9(+) (n) | X2 value | P value | |
| Male | 57 | 17 | 0.002 | 0.967 |
| Female | 34 | 10 | ||
C-PHQ-9, Chinese version of the Patient Health Questionnaire-9.
Table 3.
Depression rate between men and women with disease duration >10 years
| Disease duration >10 years | ||||
| Patients with psoriasis | C-PHQ-9(+) (n) | X2 value | P value | |
| Male | 33 | 18 | 0.001 | 0.977 |
| Female | 24 | 13 | ||
C-PHQ-9, Chinese version of the Patient Health Questionnaire-9.
Incidence of depression in patients with psoriasis
This study identified 30 (20.27%) patients who met the DSM-V criteria for the diagnosis of depression and 118 (79.73%) patients without depression. There was no significant difference between the C-PHQ-9 (39.19%) and HAMD (31.09%) detection rates for depression (X2=2.14, p=0.15) (table 4).
Table 4.
C-PHQ-9 and HAMD depression findings, n (%)
| Scale | Patients without depression | Mild depression | Moderate depression | Severe depression |
| C-PHQ-9 | 90 (60.81) | 37 (25.00) | 15 (10.14) | 6 (4.05) |
| HAMD | 102 (68.91) | 29 (19.59) | 10 (6.76) | 7 (4.73) |
C-PHQ-9, Chinese version of the Patient Health Questionnaire-9; HAMD, Hamilton Depression Scale.
Trust-level analysis
Homogeneity reliability
The internal consistency coefficient (Cronbach’s α coefficient) of the C-PHQ-9 scale was 0.938. The correlation coefficient between each item and the total score of the scale ranged from 0.540 to 0.854, and the correlation coefficient between each item ranged from 0.376 to 0.933, all of which demonstrated significant correlation (p<0.01) (table 5).
Table 5.
Correlation between items in C-PHQ-9 and each item and total score (r)
| Items | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 |
| Q1 | 1 | ||||||||
| Q2 | 0.608* | 1 | |||||||
| Q3 | 0.749* | 0.650* | 1 | ||||||
| Q4 | 0.661* | 0.788* | 0.561* | 1 | |||||
| Q5 | 0.702* | 0.606* | 0.589* | 0.634* | 1 | ||||
| Q6 | 0.625* | 0.508* | 0.591* | 0.567* | 0.680* | 1 | |||
| Q7 | 0.490* | 0.390* | 0.431* | 0.509* | 0.589* | 0.803* | 1 | ||
| Q8 | 0.501* | 0.376* | 0.438* | 0.527* | 0.573* | 0.804* | 0.858* | 1 | |
| Q9 | 0.499* | 0.376* | 0.436* | 0.543* | 0.589* | 0.804* | 0.868* | 0.933* | 1 |
| Total score | 0.840* | 0.839* | 0.839* | 0.854* | 0.761* | 0.683* | 0.573* | 0.575* | 0.540* |
Q1 refers to the first score, Q2 refers to the second score, and so on.
*P<0.01 (two-sided test).
C-PHQ-9, Chinese version of the Patient Health Questionnaire-9.
Test reliability
The initial score and the retested C-PHQ-9 total score after 1 week were analysed and the correlation coefficient was 0.955 (p<0.01).
Validity analysis
Validity
The consistency analysis between C-PHQ-9 and HAMD showed a kappa coefficient of 0.779. The two were divided into positive correlations and the correlation coefficient was 0.504 (p<0.01).
Structural validity
Principal component analysis showed that the Kaiser-Meyer-Olkin Measure of Sampling Adequacy (KMO) value was 0.877, and the Bartley spherical test statistics was 31 130.97 (p<0.05), indicating that there are common factors among the items, making them suitable for factor analysis. The principal component factor analysis was a one-factor structure, the extracted eigenvalue was 6.20, the variance of the factor was 68.88% of the total, and the factor load matrix coefficients of all the entries were greater than 0.572 (0.572–0.950).
ROC curve
A total of 148 subjects were evaluated using the DSM-V, including 30 patients with depression and 118 patients without depression. DSM-V was used as the standard for the ROC curve, with the maximum Youden index (sensitivity+specificity=1). The best cut-off point for C-PHQ-9 was 9 points, with a sensitivity of 98.00% and a specificity of 90.80%. The AUC of C-PHQ-9 was 0.979 (95% CI 0.968 to 0.991) (figure 1).
Figure 1.
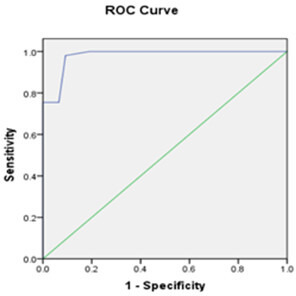
ROC curve of C-PHQ-9. The blue line represents the ROC curve of C-PHQ-9, and the green line represents the diagnostic reference line. C-PHQ-9, Chinese version of the Patient Health Questionnaire-9; ROC, receiver operating characteristic.
Comparison of the completion time of the two scales
In this study, the mean completion time for C-PHQ-9 evaluation (2.02±0.84 min) was significantly less than that for HAMD (23.37±3.21 min), and the difference was statistically significant (t=−78.37, p<0.001).
Discussion
About 300 million people worldwide are affected by depression,10 with different prevalence rates in different countries, including about 8.1% in the USA,11 8.7% in Argentina,12 14% in Brazil,10 5.9%–9.8% in Germany,13 5.5% in Singapore14 and 5.9%–13.2% in China.15 16 Psoriasis is a common chronic inflammatory skin disease that has a notable impact on the lives of patients. A study that employed different survey populations and screening tools found that 9%–55% of patients with psoriasis have depression.8 However, currently, dermatologists are not very aware of depression, resulting in undiagnosed depression in some patients with psoriasis and thus affecting the treatment of psoriasis. Screening for depression in patients with psoriasis is currently limited by three factors: (1) high variability of currently available questionnaires, (2) absence/lack of questionnaires designed and validated for patients with psoriasis, and (3) dermatologists’ limited use and non-familiarity with questionnaires.17 Therefore, it is necessary to find an evaluation scale for patients with psoriasis and depression that is both specific and sensitive, as well as economical and time-saving.
Screening for depression refers to the use of a depression screening questionnaire to identify patients who may have depression but have not been diagnosed with the condition. PHQ-9 has been recommended by DSM-V for investigating depression and has been shown to have good reliability and validity in different populations.18–20 However, there are no reports on its use in patients with psoriasis. In this study, 148 patients with psoriasis were investigated using the C-PHQ-9 scale. The rate of depression in patients with psoriasis using C-PHQ-9 scale was 39.19% and is consistent with the results of previous research.8 However, after controlling for disease duration, there was no difference in the prevalence of depression between men and women. In future work, we will focus on whether C-PHQ-9 is particularly useful to a specific population. The rate of depression was significantly higher in patients with disease duration >10 years. This finding is consistent with the results of other research and seems reasonable due to the long-standing adverse effects of psoriasis in these patients. Specificity in this study was similar to that in previous studies and across reference standards. Based on semistructured interviews, the standard cut-off score of 9 maximised combined sensitivity and specificity, which yielded values of 98.00% and 90.80%, respectively. In this study, we hoped to find a simpler, more convenient and efficient scale that dermatologists can use to evaluate the psychological state of patients with psoriasis in clinical work and to timely identify patients with depression, and the results show the best truncation. The cut-off point is 9 and the sensitivity and specificity can reach 98% and 90.8%, which are slightly different from previous studies.21 Martin et al22 found the best cut-off score is 10, and this part of patients always need psychological intervention by psychologists. Our results show that C-PHQ-9 can screen out some patients with early depression, including those who can take early psychological intervention to avoid serious consequences. The kappa coefficient between the C-PHQ-9 and HAMD scales was 0.779. The two scales were divided into positive correlations and the correlation coefficient was 0.504, which indicates good consistency. The identification of depression was higher using C-PHQ-9 and HAMD compared with DSM-V, which is consistent with previous studies, indicating that both have good false-positive rates. The time to complete C-PHQ-9 was less than the time taken to complete HAMD.
The main strength of this study is that all patients with psoriasis were assessed using the gold standard for evaluating depression. DSM-V and the C-PHQ-9 were innovatively applied to patients with psoriasis. Moreover, the time to complete C-PHQ-9 and HAMD was also assessed. However, the study was limited by its small sample size, as well as its cross-sectional and single-centre design. In the future, randomised controlled trials are needed to analyse factors related to psoriasis and assess the effect of C-PHQ-9 in patients with psoriasis and depression.
Conclusions
C-PHQ-9 has the advantages of fewer items, easier administration, better clarity, high screening efficiency and having nine diagnostic criteria for depression based on DSM-V. PHQ-9 not only provides value for screening but can also assess the severity of depression. Also, this scale has clear advantages over the HAMD with regard to time and effort in completing the questionnaire. Due to its simplicity, high sensitivity and high specificity, we believe C-PHQ-9 should be strongly considered for use in clinical setting to screen psoriasis patients with depression, with a recommended cut-off score of ≥9.
Supplementary Material
Footnotes
XY and H-LS contributed equally.
Contributors: XY and H-LS were involved in the study design, study coordination, data analysis and manuscript writing. XF, X-LZ and D-MX contributed to data analysis and manuscript writing. BY, W-YM and Z-QW were involved in patient recruitment coordination. C-QL was involved in the study design and critical revision of the manuscript.
Funding: The study of Neuroendocrine basis and comorbidity mechanism in psoriasis patients with depression (LuZhou Science and Technology Department-Southwest Medical University joint Project (090300021424)).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Patient consent for publication: Not required.
Ethics approval: The survey was approved by the Ethics Committee of the Affiliated Hospital of Southwest Medical University. The study was conducted in accordance with the tenets of the Declaration of Helsinki.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All data relevant to the study are included in the article or uploaded as supplementary information. No additional data are available.
References
- 1.Iskandar IYK, Ashcroft DM, Warren RB, et al. Demographics and disease characteristics of patients with psoriasis enrolled in the British association of dermatologists biologic interventions register. Br J Dermatol 2015;173:510–8. 10.1111/bjd.13908 [DOI] [PubMed] [Google Scholar]
- 2.Nevitt GJ, Hutchinson PE. Psoriasis in the community: prevalence, severity and patients' beliefs and attitudes towards the disease. Br J Dermatol 1996;135:533–7. 10.1111/j.1365-2133.1996.tb03826.x [DOI] [PubMed] [Google Scholar]
- 3.Rapp SR, Feldman SR, Exum ML, et al. Psoriasis causes as much disability as other major medical diseases. J Am Acad Dermatol 1999;41:401–7. 10.1016/S0190-9622(99)70112-X [DOI] [PubMed] [Google Scholar]
- 4.Rendon A, Schäkel K. Psoriasis pathogenesis and treatment. Int J Mol Sci 2019;20:E1475. 10.3390/ijms20061475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fleming P, Bai JW, Pratt M, et al. The prevalence of anxiety in patients with psoriasis: a systematic review of observational studies and clinical trials. J Eur Acad Dermatol Venereol 2017;31:798–807. 10.1111/jdv.13891 [DOI] [PubMed] [Google Scholar]
- 6.Sampogna F, Tabolli S, Abeni D. IDI multipurpose psoriasis research on vital experiences (improve) Investigators. living with psoriasis: prevalence of shame, anger, worry, and problems in daily activities and social life. Acta Derm Venereol 2012;92:299–303. [DOI] [PubMed] [Google Scholar]
- 7.Dantzer R, Wollman E, Vitkovic L, et al. Cytokines and depression: fortuitous or causative association? Mol Psychiatry 1999;4:328–32. 10.1038/sj.mp.4000572 [DOI] [PubMed] [Google Scholar]
- 8.Korman AM, Hill D, Alikhan A, et al. Impact and management of depression in psoriasis patients. Expert Opin Pharmacother 2016;17:147–52. 10.1517/14656566.2016.1128894 [DOI] [PubMed] [Google Scholar]
- 9.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. primary care evaluation of mental disorders. patient health questionnaire. JAMA 1999;282:1737–44. 10.1001/jama.282.18.1737 [DOI] [PubMed] [Google Scholar]
- 10.Saragoussi D, Christensen MC, Hammer-Helmich L, et al. Long-Term follow-up on health-related quality of life in major depressive disorder: a 2-year European cohort study. Neuropsychiatr Dis Treat 2018;14:1339–50. 10.2147/NDT.S159276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brody DJ, Pratt LA, Hughes JP. Prevalence of Depression Among Adults Aged 20and Over:United States, 2013-2016[J]. NCHS Data Brief 2018;303:1–8. [PubMed] [Google Scholar]
- 12.Cía AH, Stagnaro JC, Aguilar Gaxiola S, et al. Lifetime prevalence and age-of-onset of mental disorders in adults from the Argentinean study of mental health epidemiology. Soc Psychiatry Psychiatr Epidemiol 2018;53:341–50. 10.1007/s00127-018-1492-3 [DOI] [PubMed] [Google Scholar]
- 13.Silva MT, Galvao TF, Martins SS, et al. Prevalence of depression morbidity among Brazilian adults: a systematic review and meta-analysis. Braz J Psychiatry 2014;36:262–70. 10.1590/1516-4446-2013-1294 [DOI] [PubMed] [Google Scholar]
- 14.Grobe TG, Kleine-Budde K, Bramesfeld A, et al. [Prevalences of Depression Among Adults: Comparative Analysis of a Nationwide Survey and Routine Data]. Gesundheitswesen 2019;81:1011–7. 10.1055/a-0652-5424 [DOI] [PubMed] [Google Scholar]
- 15.Mythily S. Abdin Edimansyah, Sambasivam Rajeswari, et al. Prevalence of Depression among Older Adults-Results from the Well-being of the Singapore Elderly Study. J Ann Acad Med Singap 2016;45:123–33. [PubMed] [Google Scholar]
- 16.Liu H, He Y, Wang J, et al. Epidemiology of depression at traditional Chinese medicine hospital in Shanghai, China. Compr Psychiatry 2016;65:1–8. 10.1016/j.comppsych.2015.09.005 [DOI] [PubMed] [Google Scholar]
- 17.Zhou X, Bi B, Zheng L, et al. The prevalence and risk factors for depression symptoms in a rural Chinese sample population. PLoS One 2014;9:e99692. 10.1371/journal.pone.0099692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dowlatshahi EA, Wakkee M, Arends LR, et al. The prevalence and odds of depressive symptoms and clinical depression in psoriasis patients: a systematic review and meta-analysis. J Invest Dermatol 2014;134:1542–51. 10.1038/jid.2013.508 [DOI] [PubMed] [Google Scholar]
- 19.Grapp M, Terhoeven V, Nikendei C, et al. Screening for depression in cancer patients using the PHQ-9: the accuracy of somatic compared to non-somatic items. J Affect Disord 2019;254:74–81. 10.1016/j.jad.2019.05.026 [DOI] [PubMed] [Google Scholar]
- 20.Adekkanattu P, Sholle ET, DeFerio J, et al. Ascertaining depression severity by extracting patient health questionnaire-9 (PHQ-9) scores from clinical notes. AMIA Annu Symp Proc 2018;2018:147–56. [PMC free article] [PubMed] [Google Scholar]
- 21.Ahmad S, Hussain S, Akhtar F, et al. Urdu translation and validation of PHQ-9, a reliable identification, severity and treatment outcome tool for depression. J Pak Med Assoc 2018;68:1166–70. [PubMed] [Google Scholar]
- 22.Martin A, Rief W, Klaiberg A, et al. Validity of the brief patient health questionnaire mood scale (PHQ-9) in the general population. Gen Hosp Psychiatry 2006;28:71–7. 10.1016/j.genhosppsych.2005.07.003 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


