Abstract
Objectives:
Fecal microbiota transplantation (FMT) has emerged as an effective treatment option for Clostridioides difficile infection (CDI) and is considered an investigational therapy for a number of other diseases. Social media has facilitated widespread exposure of the public to the gut microbiome and FMT, ultimately acting as a catalyst for the Do-It-Yourself (DIY) FMT movement.
Aims:
The aims of this study were to identify factors that influenced willingness to pursue DIY-FMT including common indications, screening processes, sample preparation, and self-reported efficacy and safety outcomes.
Methods:
A twenty-five-point cross-sectional survey was posted online via the websites and social medial pages of The Peggy Lillis Foundation, Fecal Transplant Foundation, and Power of Poop. Responses were cataloged via the Research Electronic Data Capture tool and descriptive analyses were performed.
Results:
84 respondents completed the survey between January 2018 and February 2019. The majority were female (71%) and white (92%). Most (80%) reported performing FMT on themselves; 87% utilized internet resources to assist in the process and 92% knew their stool donor. Inflammatory bowel disease (35%) and irritable bowel syndrome (29%) were the two most common conditions that respondents attempted to treat. Only 12% reported adverse events while 82% reported improvement in their condition.
Discussion:
DIY-FMT is being used for many indications, including those for which there is little evidence. There was a high self-reported success rate among respondents with few adverse events. There is a need for increased awareness around DIY-FMT and research around this phenomenon, which may impact public health.
Keywords: Clostridioides difficile, C. difficile infection, fecal transplant, Do-It-Yourself fecal transplant, gut microbiome, microbiota transplant
Introduction:
Fecal microbiota transplantation (FMT) has emerged as an effective treatment option for individuals with Clostridioides difficile infection. Given that it has been shown to beneficially alter the recipient gut microbiome, some posit that FMT may be effective at treating other conditions associated with dysbiosis such as inflammatory bowel diseases (IBD), autoimmune disorders, irritable bowel syndrome (IBS), obesity/metabolic syndrome, and even neuropsychiatric conditions including depression or autism spectrum disorders 4–6. Although there is increasing awareness and interest in conducting clinical trials of FMT for these other indications, this has not rapidly translated into increased clinical delivery and access. This has become a source of consternation for the lay public, some of whom have begun to self-administer FMT outside of clinical settings in a practice known as “Do-It-Yourself” (DIY)-FMT--meaning lay individuals adopting FMT clinical techniques performed on and/or by themselves at home.
Social media has facilitated widespread exposure to and awareness of the relationship between the gut microbiome and human health. A Facebook search of “gut microbiome” yields numerous posts, articles, groups, and pages such as “Gut Microbiota News Watch” and “Gut Health Project” with close to 50,000 “likes” between these 2 pages alone. A brief Internet search for home-based or DIY-FMT generates a plethora of videos, blogs, discussion boards, and support groups. Sites such as “The Power of Poop” among others promote how to find and screen a stool donor, prepare a transplant sample, and conduct its transfer [5,7–9]. The availability of this knowledge propagates interest and enthusiasm around FMT as a promising and beneficial therapy. Although it is known that FMT is being performed in non-clinical settings by nonhealthcare providers, limited literature exists that explores factors influencing decisions to pursue DIY-FMT and associated outcomes. Our study aims to describe the scope of DIY-FMT including indications, methods, and self-reported outcomes and safety issues.
Methods:
A twenty-five-point cross-sectional English-language survey was designed to collect key information pertaining to DIY-FMT including demographics, motivations to perform, indications treated, donor identification and screening, efficacy outcomes, and reported safety events (Appendix 1). After approval by the Lifespan Institutional Review Board, the survey was posted online through the websites and related social media pages of the Peggy Lillis Foundation, The Fecal Transplant Foundation, and The Power of Poop. The Peggy Lillis Foundation gets about 120,000 unique visitors to their website and across social media annually, while the Facebook groups related to FMT where the link to the survey was posted reached another 8,000 users. Survey responses were captured and analyzed after 13 months of hosting on these servers. There were no incentives offered to induce participation, and no measures in place to mitigate repeat survey submissions from single respondents. Responses were cataloged through the Research Electronic Data Capture (REDCap) data-base tool hosted at Lifespan which also facilitated extraction of descriptive analyses.
Results:
A total of 84 respondents completed the survey between January 2018 and February 2019. The median age group of respondents was 40-49 years old. The majority were female (71%) and white (92%) (Table 1). Most (61%) respondents were from the United States, with the majority residing on the West Coast (27%) (Figures 1 and 2). Most had done FMT on themselves (80%), while the remainder performed FMT on their children (12%); a spouse (2%); another relative (2%), a friend (1%); or other (2%). Of the 67 respondents who responded to the question “How many stool transplants have you done on yourself?” the largest group (43%) had performed more than 10 transplants; 22% reported performing more than 1 but less than 5; 16% performed more than 5 but less than 10; and 18% reported having done only 1 transplant. Of the 16 respondents who reported having assisted someone else with stool transplant, half had assisted others more than 10 times.
Table 1:
Demographics
| Number (%) of Respondents | ||
|---|---|---|
| Gender | ||
| Female | 59 (71) | |
| Male | 22 (27) | |
| Other | 1 (1) | |
| Prefer not to say | 1 (2 | |
| Race/Ethnicity | ||
| Asian | 1 (1) | |
| Black or African American | 0 | |
| American Indian or Alaska Native | 0 | |
| White | 76 (92) | |
| Native Hawaiian or Other Pacific Islander | 0 | |
| Prefer Not to Say | 6 (7) | |
| Hispanic, Latino, or Spanish Origin | ||
| Yes | 3 (4) | |
| No | 74 (90) | |
| Prefer Not to Say | 5 (6) | |
| Age | ||
| < 18 | 1 (1) | |
| 18-29 | 7 (8) | |
| 30 – 39 | 29 (35) | |
| 40 – 49 | 12 (14) | |
| 50 – 59 | 23 (27) | |
| 60 – 69 | 9 (11) | |
| 70 – 79 | 1 (1) | |
| 80 – 89 | 1 (1) | |
| 90 or > | 0 | |
| Prefer Not to Say | 1 (1) |
Figure 1:
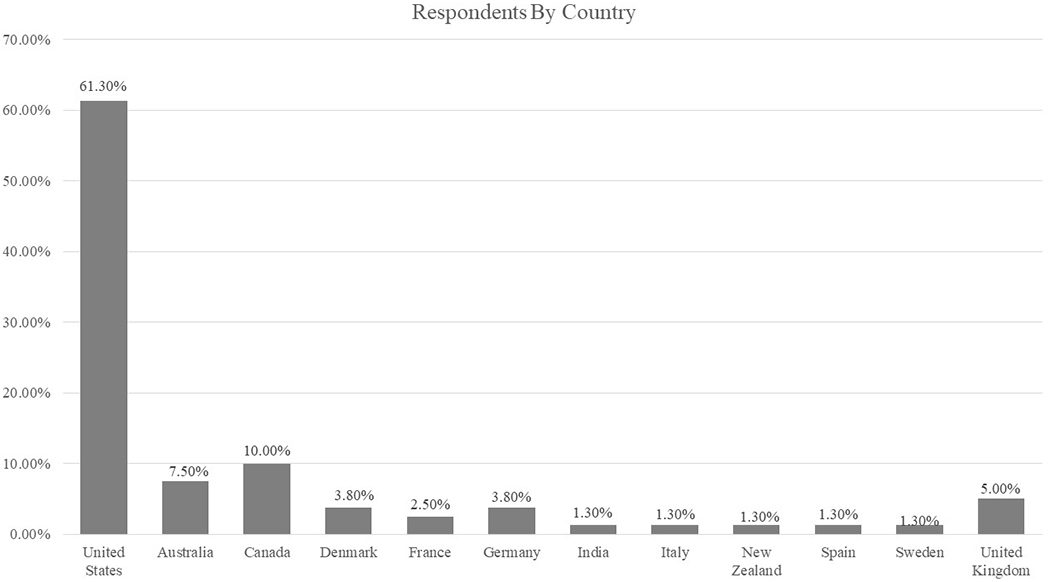
The countries respondents live in expressed in percentages.
Figure 2:
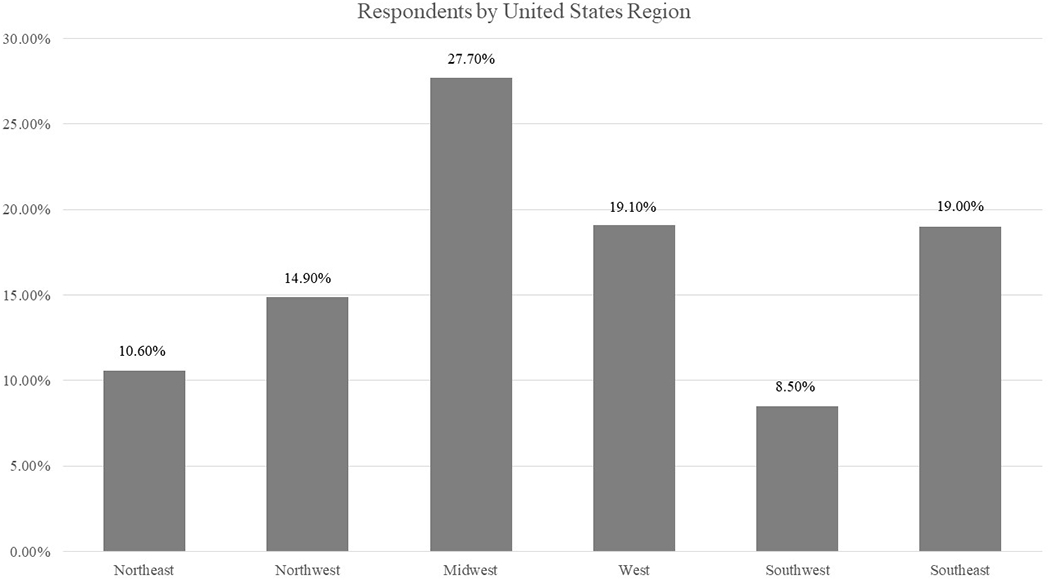
The regional distribution of respondents in the United States expressed in percentages.
Half (n=42) of all respondents reported receiving help or advice from a healthcare professional. The majority (87%) figured out how to do perform FMT through Internet support groups/ community boards/ YouTube/ other Internet video site; 6% became informed through a family member. Most reported using a stool donor known to them (92%), and 65% screened the donor in some way. Screening modalities included health questionnaire, blood tests, stool tests, or interviews. Of the respondents who used screening modalities, 20% used 2 screening modalities, 13% used 3 screening modalities, and 11% used all 4 screening modalities. Almost all performed FMT through enema (95%), 2 (2.4%) respondents performed FMT by enema and capsule ingestion, 1 performed by oral ingestion (1.2%) and 1 (1.2%) attempted capsule ingestion, but was unsuccessful.
The conditions respondents were trying to treat included IBD (35%), IBS (29%), CDI (26%), food allergies/intolerance or non-digestive autoimmune disorders (30%), small intestinal bacterial overgrowth (SIBO) (11%), autism (2%), and “other” (25%) (Table 2). Few (12%) reported any adverse events (AEs) (Table 3). Of the respondents who reported AEs, 70% had performed screening of the donor before FMT. Factors that influenced respondents’ decisions to try DIY-FMT included lack of access to healthcare providers offering FMT (33%); lack of insurance coverage for FMT (10%); and having tried other treatments that did not work (64%) (Table 4). A total of 68 respondents (82%) felt that DIY-FMT helped the condition they hoped to treat; 86% of respondents with CDI reported improvement in their condition, 90% of respondents with IBD reported improvement in their condition, 70% of respondents with IBS reported improvement in their condition, and 84% of respondents with food allergies/intolerance or nondigestive autoimmune disorders reported improvement in their condition. In addition, nearly all (96%) reported that they would do it again. Seventy-two respondents (86%) indicated that they would feel comfortable talking about FMT with a healthcare provider. Importantly, 57% of respondents indicated that they would have preferred to have it performed in a clinical setting or health center instead of at home.
Table 2:
Conditions Hoped to Treat Using FMT.
| N | % | |
|---|---|---|
| CDI | 22 | 26.2 |
| 1IBD | 29 | 34.5 |
| IBS | 24 | 28.6 |
| Food allergies, intolerance or non-digestive autoimmune disorders | 25 | 29.8 |
| SIBO | 9 | 10.7 |
| Autism | 2 | 2.4 |
| 2Other | 21 | 25 |
Of those reporting IBD: Crohn’s Disease N=7, 24.1%; Ulcerative colitis N=20, 69%; Other IBD/Unknown N=2, 6.9%.
Other reported conditions hoped to treat using FMT that were self-reported included: Immune dysfunction, allergies; Obesity; Damage from chemo; Chronic diarrhea 6-10 times daily after my c diff had been treated; Chronic Fatigue Syndrome; Multiple Sclerosis; Leaky gut; Depression and migraines; ME/CFIDS, Hashi’s, MCAS; Nonspecific Colitis; Postural Orthostatic Tachycardia (POTS); Bipolar 1; “ a whole range of serious and debilitating inflammatory symptoms”; fibromyalgia; anxiety/ADHD; Leaky gut and short temper; IBS; weight loss.
Table 3:
Adverse Events Reported.
| Adverse Events Reported | N | % |
|---|---|---|
| Fever | 2 | 20 |
| Abdominal pain | 5 | 50 |
| Gassiness, bloating | 5 | 50 |
| Infection | 1 | 10 |
| Hospitalization | 1 | 10 |
| Change in mood | 5 | 50 |
| 1,2New diagnosis | 2 | 20 |
“It altered my chronic inflammation in general. For example, blepharitis in my right eye is now worse. I have had changes in motility.”
“Used a low quality/risky donor out of desperation and developed a variety of new issues. Diarrhea from FODMAPS, unique foul body odor, cramps, various ear issues, brain feeling inflamed, light sensitive, eyes burning, red and dry under eyes, feeling incredibly ill. Red dots on various parts of body that look like busted red blood vessels. Low brain function, confusion, right eye droopy, some borderline stroke symptoms. I’ve mostly got these under control via saccharomyces boulardii + only eating plain white rice & fruit juice.”
Table 4:
Factors that influenced respondents’ decisions to try DIY-FMT.
| Factors of Influence | N | % |
|---|---|---|
| I read about it in medical papers or articles | 59 | 70 |
| Other treatments I tried have not worked | 54 | 64 |
| I found out about it from internet support groups/community boards | 51 | 61 |
| My healthcare provider does not offer stool transplant | 28 | 33 |
| I heard about it from the media | 25 | 30 |
| I heard about it from stories from other patients, family members or friends | 24 | 29 |
| Trying stool transplant in the privacy of my home was attractive | 20 | 24 |
| My doctor or other healthcare professional suggested it | 15 | 18 |
| I thought it would be cheaper than other medical treatments | 11 | 13 |
| My insurance provider does not cover stool transplant or only partially covers it | 8 | 10 |
| I felt embarrassed about getting a stool transplant in a public clinic | 0 | 0 |
| *Other factors not listed here | 22 | 26 |
FMT, fecal microbiota transplantation.
Other Factors of Influence to Try DIY-FMT:
-”Ridiculous costs associated with going out of country for it, utter unavailability of it in the US medical system.”
-“It seemed [my] last hope to live.”
-“Six months of C diff treatment with vancomycin and I got FMT from a doctor 8 [times] after to improve my gut bacteria and help heal gut and also fear of recurring C diff. It should have been offered to me before getting bedridden from antibiotics not working and causing more damage but insurance requires 3 failed treatments with meds.”
-“I needed to be intubated for colonoscopy because of issues with anesthesia in the past. My GI doesn’t do them I’d need to go through a different GI doctor.”
-“FMT for bipolar disorder is not yet medically approved.”
-“Not FDA approved [for something other than C diff].”
-“Less expensive than getting it in a clinic (as far as I know, no clinic offers it in my country).”
-“NOT ALLOWED IN US EXCEPT FOR C DIFF !!!”
Discussion:
In recent years, there has been an increase in do-it-yourself medical movements, meaning lay individuals adopting experimental clinical techniques performed on and/or by themselves at home [10–12]. This study provides the first systematic glimpse into the practices of DIY-FMT, elucidating how and why individuals turn to FMT. Like other DIY medical movements, lack of access and prohibitive costs, combined with frustration at the lack of effective treatment, are key factors that influenced participants’ decisions to try FMT at home [13–15]. Just as in other DIY medical movements, participants primarily learn how to perform the technique through the Internet [16]. Participants have used FMT both for treatments that are currently standard of care (i.e., CDI) as well as for indications that are currently under investigation (e.g., IBD) as well as others for which there is little evidence. Many reported treating themselves with 10 or more FMTs, which is interesting as serial FMT has commonly been reported for indications other than C. difficile, for which a single FMT is usually effective [17] Most common reported indications for multiple FMTs in this cohort were food allergies, nondigestive autoimmune conditions, and IBD.
One of riskiest aspects of DIY-FMT is that the donor is not typically screened according to the methods used in the clinic, where there is rigorous screening for communicable diseases such as human immunodeficiency virus, viral hepatitis, and enteric pathogens. Currently, in clinical settings, most FMT procedures are performed using stool from a donor that is unknown to the recipient. Strikingly, amongst this population of respondents, almost all reported using donor stool from an individual known to them. This may be because of a perception of decreased risk when using known donors or because obtaining fecal material from an anonymous volunteer donor outside of a clinical setting seems more challenging. Even more surprising is that more than half the respondents took the additional step of screening donor blood or stool through laboratory tests or reported guidance from healthcare professionals. However, the present survey did not tease out the level of guidance, which could have ranged from providing orders for stool screening to mere warning of risks. Known risks associated with FMT include infection, transmission of multidrug resistant organisms [18], or aspiration if instilled through the oro/nasopharyngeal route. That a portion of respondents are taking steps to screen indicates a level of safety concern or awareness among some individuals. Concerningly, however, is that a portion of respondents also did not perform any kind of donor screening. These observations are particularly disturbing in light of the fact that 10% of respondents performed FMT on children.
One of the most striking findings is the high level of self-reported success in treatment of both gastrointestinal and extraintestinal conditions. Although these outcomes are self-reported, they are in-line with the literature on the effectiveness of FMT for CDI in which studies report resolution of symptoms in 90% of cases [17]. Conversely, randomized controlled trials of FMT in IBD have reported efficacy rates far below the positive outcomes reported in this survey [6]. Reported success rates for other indications might be related to the placebo effect, which is as high as 43% in clinical trials for functional bowel disorders [19]. Respondents reported few AEs or complications associated with FMT, the vast majority of which were minor or moderate—which is consistent with previous systematic reviews exploring incidences of AEs after FMT [20]. On one hand, this is reassuring and suggests that there are relatively few side effects associated with FMT. Yet, the inherent selection bias associated with surveys such as this must always be considered with respect to likely under-reporting of side effects associated with FMT.
Other limitations include the inherent barriers to Internet-based surveys including access to the Internet or traffic impedance to the given servers on which they are hosted. Moreover, without stringent parameters to prohibit repeat submissions, duplication of particular respondents could also present as a confounder. This survey was hosted on 3 advocacy websites: Peggy Lillis Foundation, The Fecal Transplant Foundation, and The Power of Poop—which contributes to the aforementioned selection bias. Research has shown that there is a significant difference among racial or ethnic groups as well as based on education levels in web-based survey participation which again contributes to selection bias [21]. In our study, 91% of respondents identified as white, which may indicate that underrepresented populations are not performing DIY-FMT or that they are less likely to report doing so. Moreover, there may be an effect of class or socioeconomic status in the DIY medicine movement evident in real-world samples such as this, that is collapsed within discourses regarding selection bias.
The highly successful cure rates of CDI by FMT generated a robust expansion of scientific exploration to further investigate the implications of FMT on other disease states. Presently, there are more than 200 active clinical trials exploring the role of FMT in the treatment of a multitude of disease processes [22]. Under current US Food and Drug administration (FDA) policy, FMT is permissible for CDI recalcitrant to standard therapies, for other indications, however, submission of investigational new drug (IND) applications for review and oversight agency continues, which has limited the adoption of FMT for conditions outside of recalcitrant CDI in clinical settings [23,24]. This barrier does not, however, apply to lay individuals. Our work highlights the curiosity and interest among patients on the applicability of FMT for other conditions associated with alterations in the gut microbiome. This curiosity has manifest as individuals experimenting on themselves with the aim of achieving cure or healing. Put succinctly, the public’s desire has outpaced the rate of our clinical discovery in this domain, and this should prompt serious concerns regarding safety, harm, efficacy, and a fracturing of the trust that is paramount between patients and providers. The lay public is leveraging the Internet and social media to share resources and treat a wide array of diseases on their own. It is imperative that clinicians address this evolving gap between patients’ needs and medical knowledge around FMT in order to maintain trust and ensure safety and efficacy. The fact that more than half of respondents would have preferred to have FMT performed in a clinical setting is a hopeful sign that our patients have not abandoned conventional medicine in favor of Internet-guided self-care. In sum, DIY-FMT is an active phenomenon that the medical community must not ignore. There should be recognition that its use is a response to the mismatch between our evolving knowledge around the gut microbiome, FMT’s efficacy, and perceptions of the lay public. We must think critically about how this ascendant age of social media and the Internet impacts public safety and the doctor-patient relationship.
Supplementary Material
Appendix 1: The twenty-five-point cross-sectional English-language survey that was distributed by social medial to collect demographics, motivations to perform, indications treated, donor identification and screening, efficacy outcomes and reported safety events of DIY-FMT.
Study Highlights.
WHAT IS KNOWN
Fecal microbiota transplantation (FMT) is supported by guidelines for treatment for C difficile infections (CDI).
Although FMT is being investigated as a therapy for multiple diseases associated with alterations in the gut microbiome, the FDA does not permit use outside of clinical trials for non-CDI indications.
Many people seek health information online, and social media has increased the lay public’s awareness around the gut microbiome and FMT.
WHAT IS NEW HERE
Do-It-Yourself (DIY) FMT has gained popularity for treatment of a variety of diseases outside of CDI, including inflammatory bowel disease and irritable bowel syndrome.
Most participants performed FMT on themselves and utilized internet resources to assist in the process.
A majority of the participants knew their donor and reported improvement in their condition; there were few self-reported adverse events.
Acknowledgments
Financial support:
Author Conflict of Interest/Study Support
Guarantor of the article: Colleen R. Kelly, MD
Footnotes
Potential competing interests:
Dr. Kelly reported serving as a site investigator of a clinical trial for Finch Therapeutics and on the clinical advisory board for Openbiome. All other authors reported no conflicts of interest.
References:
- 1.Kelly CR, Ihunnah C, Fischer M, et al. Fecal microbiota transplant for treatment of Clostridium difficile infection in immunocompromised patients. The American Journal of Gastroenterology, 2014; 109(7): 1065–1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bakken JS, Borody T, Brandt LJ, et al. Fecal Microbiota Transplantation Workgroup. Treating Clostridium difficile infection with fecal microbiota transplantation. Clinical Gastroenterology and Hepatology, 2011; 9(12): 1044–1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cammarota G, Ianiro G, Gasbarrini A. Fecal microbiota transplantation for the treatment of Clostridium difficile infection: a systematic review. Journal of Clinical Gastroenterology, 2014; 48(8): 693–702. [DOI] [PubMed] [Google Scholar]
- 4.Matsuoka K, Mizuno S, Hayashi A, et al. Fecal microbiota transplantation for gastrointestinal diseases. The Keio Journal of Medicine, 2014; 63(4): 69–74. [DOI] [PubMed] [Google Scholar]
- 5.Goodman B The Rise of the Do-It-Yourself Fecal Transplant. WebMD; December 2015. [Google Scholar]
- 6.Paramsothy S, Paramsothy R, Rubin DT, et al. Faecal Microbiota Transplantation for Inflammatory Bowel Disease: A Systematic Review and Meta-analysis. J Crohns Colitis, 2017; October 1;11(10):1180–1199. [DOI] [PubMed] [Google Scholar]
- 7.Skwarecki B Why DIY fecal transplants are a thing (and the FDA is only part of the reason). PLOS Blogs: Public Health Perspectives; May 2013. [Google Scholar]
- 8.Jeffries A The World of Do-It-Yourself Fecal Transplants (Thanks YouTube!). Motherboard.Vice.Com. [Google Scholar]
- 9.The Power of Poop. Fecal Transplant At Home—DIY Instructions. www.thepowerofpoop.com.
- 10.Lee J, Hirschfeld E, Wedding J A Patient-Designed Do-It-Yourself Mobile Technology System for Diabetes: Promise and Challenges for a New Era in Medicine JAMA, 2016; 315(14), 1447–1448. [DOI] [PubMed] [Google Scholar]
- 11.Wexler A The practices of do-it-yourself brain stimulation: implications for ethical considerations and regulatory proposals Journal of Medical Ethics, 2016; 42(4), 211–215. [DOI] [PubMed] [Google Scholar]
- 12.Omer T Empowered citizen ‘health hackers’ who are not waiting BMC Medicine, 2016; 14(1), 118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rotondi N, Bauer G, Scanlon K, Kaay M, Travers R, Travers A (2013). Nonprescribed Hormone Use and Self-Performed Surgeries: “Do-It-Yourself” Transitions in Transgender Communities in Ontario, Canada American Journal of Public Health,2013; 103(10), 1830–1836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wexler A The Social Context of “Do-It-Yourself” Brain Stimulation: Neurohackers, Biohackers, and Lifehackers Frontiers in Human Neuroscience, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kaziunas E, Lindtner S, Ackerman M, Lee J (2017). Lived Data: Tinkering With Bodies, Code, and Care Work Human–Computer Interaction, 2017; 33(1), 49–92. [Google Scholar]
- 16.Wexler A Who Uses Direct-to-Consumer Brain Stimulation Products, and Why? A Study of Home Users of tDCS Devices Journal of Cognitive Enhancement, 2008; 2(1), 114–134. [Google Scholar]
- 17.Moayyedi P, Yuan Y, Baharith H, Ford AC. Faecal microbiota transplantation for Clostridium difficile associated diarrhea: a systemic review of randomized controled trials. The Medical Journal of Australia, 2017; 207(4): 166–172. [DOI] [PubMed] [Google Scholar]
- 18.Important Safety Alert Regarding Use of Fecal Microbiota for Transplantation and Risk of Serious Adverse Reactions Due to Transmission of Multi-Drug Resistant Organisms. June 13 2019. https://www.fda.gov/vaccines-blood-biologics/safety-availability-biologics/important-safety-alert-regarding-use-fecal-microbiota-transplantation-and-risk-serious-adverse
- 19.Lu CL, Chang FY. Placebo effect in patients with irritable bowel syndrome. J Gastroenterol Hepatol, 2011. Suppl 3:116–8. [DOI] [PubMed] [Google Scholar]
- 20.Baxter M, Colville A. Adverse events in faecal microbiota transplant: A review of the literature. J Hosp Infect, 2016. 92(2):117–27. [DOI] [PubMed] [Google Scholar]
- 21.Jang M, Vorderstrasse A. Socioeconomic Status and Racial or Ethnic Differences in Participation: Web-Based Survey. JMIR Res Protoc. 2019;8(4): e11865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.U.S. National Library of Medicine. (Clinicaltrials.gov) Accessed May 19, 2019.
- 23.Mole B FDA gets to grips with faeces. Nature 2013; 498(7453): 147–148. [DOI] [PubMed] [Google Scholar]
- 24.Food and Drug Administration. Guidance for Industry: Enforcement Policy Regarding Investigational New Drug Requirements for Use of Fecal Microbiota for Transplantation to Treat Clostridium difficile Infection Not Responsive to Standard Therapies. http://www.fda.gov/BiologicsBloodVaccines/GuidanceComplianceRegulatoryInformation/Guidances/Vaccines/ucm361379.htm Published 2013. Accessed November 22, 2018.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix 1: The twenty-five-point cross-sectional English-language survey that was distributed by social medial to collect demographics, motivations to perform, indications treated, donor identification and screening, efficacy outcomes and reported safety events of DIY-FMT.


