Abstract
Background
In December 2019, the outbreak of a disease subsequently termed COVID-19 occurred in Wuhan, China. The number of cases increased rapidly and spread to six continents. However, there is limited information on the chest computed tomography (CT) results of affected patients. Chest CT can assess the severity of COVID-19 and has sufficient sensitivity to assess changes in response to glucocorticoid therapy.
Objective
Analyze COVID-19 patients to determine the relationships of clinical characteristics, chest CT score, and levels of inflammatory mediators.
Methods
This retrospective, single-center case series of 108 consecutive hospitalized patients with confirmed COVID-19 at Tongji Hospital, Tongji Medical College of HUST (Wuhan, China) examined patients admitted from January 28 to February 20, 2020. Patient demographics, comorbidities, clinical findings, chest CT results, and CT scores of affected lung parenchyma were recorded. The relationships between chest CT score with levels of systemic inflammatory mediators were determined.
Results
All patients exhibited signs of significant systemic inflammation, including increased levels of C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), procalcitonin, chest CT score, and a decreased lymphocyte (LY) count. Chest CT score had positive associations with white blood cell (WBC) count, CRP, ESR, procalcitonin, and abnormal coagulation function, and a negative association with LY count. Treatment with a glucocorticoid increased the LY count, reduced the CT score and CRP level, and improved coagulation function.
Conclusions
COVID-19 infection is characterized by a systemic inflammatory response that affects the lungs, blood, digestive system, and circulatory systems. The chest CT score is a good indicator of the extent of systemic inflammation. Glucocorticoid treatment appears to reduce systemic inflammation in these patients.
Keywords: COVID-19, Chest CT score, Inflammation, Glucocorticoid, Treatment
Background
On Dec 8, 2019, there were reports of several cases of pneumonia of unknown etiology in Wuhan (Hubei Province, China). The disease (now termed COVID-19) spread rapidly from Wuhan to other areas. As of March 15, 2020, there were 80,860 confirmed cases in China, 72,469 cases in 143 other countries, and cases in 6 continents [1–5]. On January 3, 2020, this novel coronavirus (now termed SARS-CoV-2) was identified in samples of bronchoalveolar lavage fluid from a patient in Wuhan and confirmed as the cause of this disease [6]. During the early stages of this pneumonia, there were severe acute respiratory symptoms (SARS), and some patients rapidly developed acute respiratory distress syndrome (ARDS), acute respiratory failure, and other serious complications [7]. On Jan 7, the Chinese Center for Disease Control and Prevention (CDC) identified this novel coronavirus from the throat swab of a patient [8]. Other coronaviruses cause multiple system infections in various animals, and mainly respiratory tract infections in humans, such as severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS) [9, 10]. Most patients infected by SARS-CoV-2 have mild symptoms and good prognosis. However, some patients with COVID-19 progressed from severe pneumonia to pulmonary edema, acute respiratory distress syndrome, multiple organ failure, and death [11, 12].
A confirmed diagnosis of COVID-19 infection requires PCR identification of viral nucleic acid and lung imaging [13]. Most patients have lung imaging results indicating bilateral pulmonary parenchymal ground-glass and consolidative pulmonary opacities, sometimes with a rounded morphology and peripheral lung distribution. Notably, lung cavitation, discrete pulmonary nodules, pleural effusions, and lymphadenopathy are absent [13].
At present, there is little known about the relationship between imaging results indicative of pneumonia and the presence of systemic inflammatory mediators in patients with COVID-19. The purpose of this study is to evaluate the severity of COVID-19 infection by quantifying chest CT results and to determine the relationship between chest CT scores and systemic inflammatory mediators in an effort to identify factors that can be used against the COVID-19 pandemic.
Methods
Study design and participants
Ethical approval was received from the Ethics Committee of the Second Hospital of Jilin University.
A total of 108 patients with COVID-19 were enrolled in the Department of Respiratory and Critical Care Medicine of the Tongji Hospital Sino-French New Town, Tongji Medical College of HUST between January 28 and February 20, 2020. Oral consent was obtained from patients. All patients with COVID-19 were diagnosed using a PCR test and all patients met the requirements of Wuhan Health and Medical Commission for admission, all patients were general or severe according to the fourth edition of the treatment plan [14].
Chest CT imaging
Chest CT scores were the average of scores (range: 0 to 10) assigned by two independent radiologists, each with more than 5 years of experience in chest CT diagnosis. If the assigned scores differed by more than 1, then a senior radiologist, with more than 10 years of experience, arbitrated so that the final assigned scores differed by 1 or less.
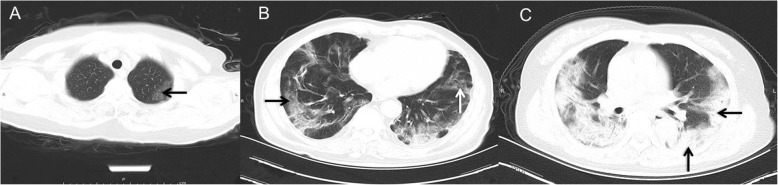
According to convention, the lung was divided into five levels, from the apex to the bottom: suprasternal notch, aortic arch, the tracheal carina, intermediate bronchus, and apex of diaphragm (Additional Figure 1A-E). The left and right lungs were scored separately, and each of the 5 lung zones in each patient was assigned a score according to distribution of affected parenchyma as previously described [15] (0, normal; 1, 10% abnormality; 2, 20% abnormality; etc.). The chest CT density was also graded (0, normal attenuation; 1, frosted glass density; 2, ground-glass attenuation; and 3, consolidation; Fig. 1). Then the lung parenchyma score was then multiplied by the square of the CT density score and points from all zones and added for a final total cumulative score that ranged from 0 to 900.
Fig. 1.
Representative lung CT images of patients who had frosted glass density (a), ground glass opacity (b), and consolidation (c)
Data collection
Demographic and clinical data were collected, including age, gender, medical history, smoking status, results from a physical examination, laboratory results, and chest CT results. Patients were divided into three subgroups based on chest CT score. The date of disease onset was defined as the day when symptoms were first noticed.
The validity of all data were checked by two physicians (BS and HD).
Statistical analysis
IBM SPSS Statistics 20.0 was used for data analysis. Data with normal distributions are presented as the means ± standard deviations (SDs) and analyzed by Student’s t-test, ANOVA, and a post hoc least significant difference (LSD) tests. Non-parametric data are expressed as medians and interquartile ranges (IQRs) and analyzed by the Kruskal-Wallis test with the Bonferroni correction or the Mann-Whitney U test. Correlations were determined using Spearman’s rank correlation coefficient. Categorical variables were analyzed using a Chi-square test. A P-value below 0.05 was defined as significant.
Results
Presenting characteristics
The study population consisted of 108 hospitalized patients with confirmed COVID-19 (Table 1). There were 25 patients (23%) under 50 years-old, 83 (77%) over 50 years-old, the median age was 66 years (interquartile range [IQR]: 51 to 72; range: 23 to 86), and 60 patients (55.6%) were men. The median duration from initial symptoms to dyspnea was 5 days (IQR: 0 to 7) and from first symptoms to admission was 10 days (IQR: 6 to 15). Forty-eight patients (44%) had an underlying disease, and the most common underlying diseases were hypertension (n = 44, 40.7%), diabetes (n = 18, 16.7%), and cardiovascular disease (n = 16, 14.8%). The most common symptoms at the onset of illness were fever (n = 93, 86%), cough (n = 78, 72.2%), and sputum production (n = 44, 40.7%), followed by diarrhea, fatigue, abdominal pain, headache, and vomiting. Sixty-five patients (60.2%) had dyspnea. In addition, one patient changed from severely ill to critically ill, and received endotracheal intubation and extracorporeal membrane oxygenation (ECMO), but eventually died (mortality rate: 1/108, 0.93%).
Table 1.
Demographic and baseline characteristics of patients (n = 108)
| Variable | Median (IQR) or n (%) |
|---|---|
| Age, years | |
| Median | 66(51, 72) |
| Range | 23, 86 |
| < 50 | 25(23%) |
| ≥ 50 | 83(77%) |
| Sex (male) | 60(55.6%) |
| Current smoking | 11(10.2%) |
| Comorbidities | |
| Hypertension | 44(40.7%) |
| Cardiovascular disease | 16(14.8%) |
| Diabetes | 18(16.7%) |
| Malignancy | 4(3.7%) |
| Cerebrovascular disease | 3(3.7%) |
| COPD | 5 (4.6%) |
| Chronic kidney disease | 3(2.8%) |
| Chronic liver disease | 5 (4.6%) |
| Signs and symptoms | |
| Fever | 93(86%) |
| Dry cough | 78(72.2%) |
| Sputum production | 44(40.7%) |
| Fatigue | 28(25.9%) |
| Myalgia | 15(13.9%) |
| Dyspnea | 65(60.2%) |
| Pharyngalgia | 9(8.3%) |
| Abdominal pain | 20(18.5%) |
| Diarrhea | 40(37%) |
| Nausea | 21(19.4%) |
| Dizziness | 9(8.3%) |
| Headache | 20(18.5%) |
| Vomiting | 19(17.6%) |
| Days from symptoms to first visit | 10(6, 15) |
| Days from onset to dyspnea | 5(0, 7) |
| Heart rate, bpm | 89(80,95) |
| Respiratory rate, per min | 20(20,21) |
| Mean arterial pressure, mmHg | 132(121,141) |
Data are indicated as n (%), n/N (%)
Laboratory parameters
The white blood cell counts of patients on admission were above the reference range in 10 patients (9.3%) and below the reference range in 10 patients (Table 2). Fifty-six patients (52%) had decreased LY counts, 62 patients (57%) patients had elevated D-dimer levels, 30 patients (28%) had elevated serum creatinine levels, 46 patients (43%) had elevated creatine kinase-MB (CK-MB) levels, 33 patients (31%) patients had increased procalcitonin levels, 87 patients (81%) had elevated CRP levels, and 76 patients (70%) had elevated levels of ESR.
Table 2.
Laboratory findings of patients upon admission
| Variable | Patients | P value | |||
|---|---|---|---|---|---|
| Chest CT score subgroup | |||||
| 0–100(group 1) | 101–200(group 2) | >200(group 3) | |||
| N | 108 | 50 | 23 | 11 | |
| Blood cells | |||||
| WBCs× 109/L, normal range: 3.5–9.5 | 5.7(4.5,7.8) | 5.9(4.4,7.8) △ | 5.5(4.6,6.1) △ | 5.4(4.4,9.5) *§ | 0.001 |
| Increased | 10 (9.3%) | 6(12%) | 0(0%) | 2(18%) | / |
| Decreased | 10(9.3%) | 5(10%) | 2(9%) | 1(9%) | / |
| Neutrophils×109/L, normal range: 1.8–6.3 | 4.1(2.9,5.9) | 4.4(2.7,6.1) △ | 3.5(3.1,4.3) △ | 3.8(2.9,7.4) *§ | < 0.001 |
| LYs × 109/L, normal range: 1.1–3.2 | 1.1(0.75,1.55) | 1.1(0.77,1.51) §△ | 1.15(0.67,1.73) * | 0.83(0.74,1.27) * | < 0.001 |
| Decreased | 56(52%) | 26(52%) | 11(48%) | 7(64%) | / |
| Platelets ×109/L, normal range: 125–350 | 266(174,340) | 265(156,338) | 268(160,363) | 261(211,342) | 0.251 |
| Haemoglobin, g/L, normal range: 115–150 | 129(114,143) | 130(111,144) | 129(117,136) | 127(114,147) | 0.410 |
| Coagulation parameters | |||||
| Activated partial thromboplastin time, s, normal range: 29–42 | 38.3(35.8,41.2) | 38.2(35.7,40.7) | 38.5(36.1,41.9) | 41.3(36.1,44) | 0.909 |
| Prothrombin time, s, normal range: 11.5–14.5 | 13.8 (13.3,14.3) | 13.9(13.6,14.5) | 13.7(13.2,14.6) | 13.6(13,14.3) | 0.076 |
| D-dimer, μg/mL, normal range: < 0.5 | 0.71 (0.40,1.58) | 0.64(0.31,1.67) &△ | 0.58(0.42,1.2) ▼ | 0.84(0.46,1.83) * | < 0.001 |
| Increased | 62(57%) | 20(40%) | 11(48%) | 5(46%) | / |
| Blood biochemistry | |||||
| Albumin, g/L, normal range: 35–52 | 35.3(32,39.4) | 36.3(31.8,40) | 37.2(32.4,40.2) | 33.3(31,37.7) | 0.183 |
| Alanine aminotransferase, U/L, normal range: ≤33 | 27(17,43) | 29(16.8,45) | 31(18,48) | 21(15,32) | 0.426 |
| Aspartate aminotransferase, U/L, normal range: ≤32 | 25 (21,39) | 24(21,37) | 32(23,47) | 25(19,38) | 0.778 |
| Total bilirubin, mmol/L, normal range: ≤21 | 9.5(7.2,13) | 8.9(6.9,12.1) | 11.6(7.9,15.1) | 9.8(7.1.,13.4) | 0.068 |
| Blood urea nitrogen, mmol/L, normal range: 1.7–8.3 | 4.8(3.6,6.1) | 5(3.6,6) &∫ | 4.7(3.7,5.3) ▼ | 4.7(3.6,7) ▼ | 0.022 |
| Serum creatinine, μmol/L, normal range: 45–84 | 71(57,86) | 70(57,86) | 81(67,87) | 68(55,78) | 0.538 |
| Increased | 30 (28%) | 14(28%) | 10(44%) | 1(9%) | / |
| CK–MB, ng/mL, normal range: ≤7.2 | 65.5(14,123) | 72(25,110) | 56(3116) | 101(15,182) | 0.493 |
| Increased | 46(43%) | 23(46%) | 6(26%) | 6(55%) | / |
| Lactate dehydrogenase, U/L, normal range: 135–214 | 262(228,333) | 261(226,325) §△ | 267(236,340) *△ | 264(225,328) *§ | < 0.001 |
| Troponin, pg/mL, normal range: ≤15.6 | 4.5(1.9,10) | 3.6(1.9,5.9) △ | 6.7(2.6,12.3) ∫ | 5.2(3.4,15.7) *& | 0.013 |
| Myoglobin, ng/mL, normal range: ≤154.9 | 59(41,113) | 49(40,72) | 74(36,127) | 59(24,132) | 0.072 |
| Glucose, mmol/L, normal range: 4.11–6·05 | 6.3 (5.6,8.3) | 6.1(5.4,8.2) | 7.4(5.7,11.7) | 7.9(6.4,9.7) | 0.108 |
| Infection-related biomarkers | |||||
| Procalcitonin, ng/mL, normal range: 0.02–0.05 | 0.04 (0.02,0.07) | 0.03(0.02, 0.05) §△ | 0.07(0.04, 0.16) * | 0.07(0.04, 0.19) * | < 0.001 |
| Increased | 33(31%) | 8(16%) | 13(57%) | 7(64%) | / |
| ESR, s, normal range: 0–20 | 40(20,66) | 36(18, 54) § | 68(35, 84) * | 58(42, 68) | 0.002 |
| Increased | 76(70%) | 36(72%) | 18(78%) | 9(82%) | / |
| CRP, mg/L, normal range: < 1 | 25(5,59) | 15(4,39) &△ | 77(30,103) ▼ | 35(20,57) * | < 0.001 |
| Increased | 87(81%) | 43(86%) | 18(78%) | 10(91%) | / |
| Serum ferritin, μg/L, normal range: 30–400 | 497 (234,975) | 376(182,709) §△ | 1202(513,1687) * | 1023(534,1509) * | 0.010 |
| IL-1β, pg/mL, normal range: < 5 | 5(5,5) | 5(5,5) | 5(5,5.3) | 5(5,5) | 0.335 |
| IL-2 receptor, U/mL, normal range: 223–710 | 613(398,918) | 607(428,765) | 628(371,1079) | 1316(424,1653) | 0.445 |
| IL-6, pg/mL, normal range: < 7 | 11(3.6,31.9) | 4.5(3.2, 16.2) | 29.3(15.1,60.3) | 11.7(5.5,79.1) | 0.103 |
| IL-8, pg/mL, normal range: < 62 | 12 (7.6,25.8) | 10.3(6.9,26.2) | 14.7(8,24.8) | 9.4(5.4,43.2) | 0.947 |
| IL-10, pg/mL, normal range: < 9.1 | 5(5,5.3) | 5(5,5) | 5.5(5,9.5) | 5(5,10) | 0.188 |
| TNF-α, pg/mL, normal range: < 8.1 | 7.9(5.6,9.4) | 8.4(5.4,9.5) | 7.2(5.6,9.7) | 7.5(5,8.8) | 0.624 |
Data are indicated as n (%), n/N (%), mean (SD), or median (IQR). Comparison of groups was determined using the Kruskall-Wallis test or the Mann-Whitney U test, as appropriate. IL, interleukin. TNF, tumor Necrosis Factor. *P < 0.01 vs. group 1; §P < 0.01 vs. group 2; △P < 0.01 vs. group 3; ▼P < 0.05 vs. group 1; &P < 0.05 vs. group 2; ∫P < 0.05 vs. group 3
Chest CT features
Chest CT images at admission were taken for 84 of 108 patients, and all CT images indicated abnormalities (Table 3). The typical findings were bilateral frosted glass density, ground-glass opacity (GGO), and consolidation (Fig. 1). Chest CT images showed that the diffuse density of both lungs increased, and the transparency of the lung field weakened. The lighter ones were frosted glass (Fig. 1a), with lower attenuation than the ground glass (Fig. 1b). GGO was present in 45 patients (53.6%), followed by frosted glass density (n = 38, 45.2%), and consolidation (n = 1, 0.93%). None of the patients had pleural effusion. Analysis of involved zones indicated that the base of the lung was most affected region (apex of diaphragm: n = 79, 94.1%), most patients had central and peripheral distribution (n = 81, 96.4%), and most patients had bilateral involvement (n = 78, 92.9%).
Table 3.
Chest CT features of patients (n = 84)
| Chest radiographic feature | Patients, n (%) or median (IQR) |
|---|---|
| Frosted glass density | 38(45.2%) |
| Ground glass opacity | 45(53.6%) |
| Consolidation | 1(1.2%) |
| Radiographic score | 59(12,148) |
| Pleural effusions | 0(0%) |
| Anatomic sides involved | |
| Unilateral | 6(7.1%) |
| Bilateral | 78(92.9%) |
| Predominant distribution | |
| Central | 2(2.3%) |
| Peripheral | 1(1.2) |
| Central and peripheral | 81(96.4%) |
| Involved zone | |
| Suprasternal notch | 37(44.1%) |
| Aortic arch | 67(79.8%) |
| Tracheal carina | 77(91.7%) |
| Intermediate bronchus | 76(90.5%) |
| Apex of diaphragm | 79(94.1%) |
Data are indicated as n (%), n/N (%)
Chest CT scores
We divided the patients into three subgroups based on the chest CT score (0 to 100, 101 to 200, and above 200), and then compared the characteristics of these subgroups (Table 2). Analysis of blood cell counts indicated that the WBC, neutrophil, and lymphocyte counts were significantly lower (P ≤ 0.001) in patients with higher CT scores. Patients in the three groups also had significant differences in D-dimer (P < 0.001), blood urea nitrogen (BUN, P = 0.022), lactate dehydrogenase (P < 0.001), troponin (P = 0.013), procalcitonin (P < 0.001), ESR (P = 0.002), CRP (P < 0.001), and serum ferritin (P < 0.010).
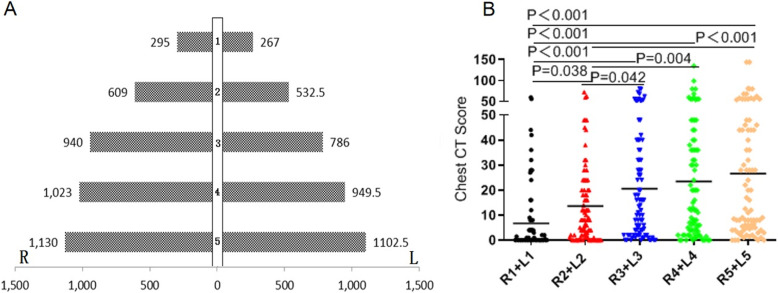
Comparison of the left and right lung layers indicated the right lung score was higher, but this was not statistically significant (P > 0.05) (Fig. 2a). A comparison of CT scores of the two lungs at different areas indicated that the chest CT score significantly increased from the top to the bottom of the lungs (Fig. 2b).
Fig. 2.
Chest CT scores of patients. a, Location of lung pathologies in the five levels of right and left (1: suprasternal notch; 2: aortic arch; 3: tracheal carina; 4: intermediate bronchus; 5: apex of diaphragm). The Kruskall-Wallis test indicated no significant differences (P > 0.05). b, Sum of the scores of the left and right lungs at 5 levels. The horizontal bars indicate medians and group comparisons using a t–test indicated significant differences
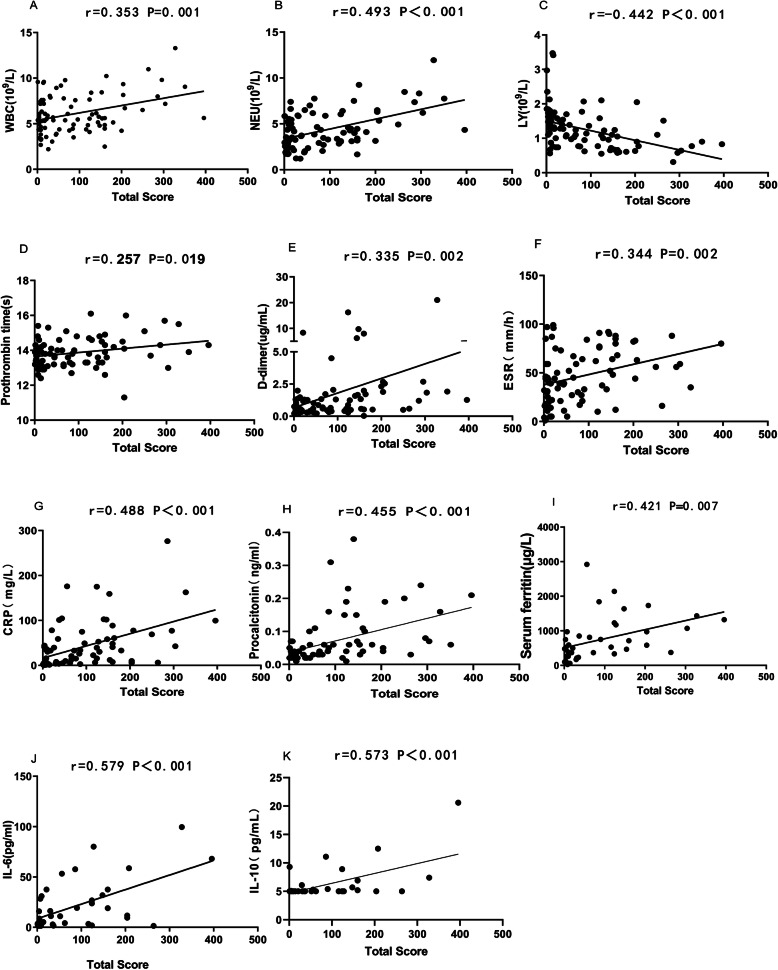
Association of chest CT score with inflammatory mediators
Correlation analysis (Fig. 3) indicated that chest CT score had significantly positive correlations with WBC count (P = 0.001), neutrophil count (P < 0.001); prothrombin time (PT, P = 0.019), the levels of D-dimer (P = 0.002), ESR (P = 0.002), CRP (P < 0 .001), procalcitonin (P < 0.001), serum ferritin (P < 0.007), IL-6 (P < 0.001), and IL-10 (P < 0.001); and a negative correlation with LY count (P < 0.001).
Fig. 3.
Correlation of chest CT score with different clinical parameters. WBC: white blood cells; NEU: neutrophils; LY: lymphocytes; ESR: erythrocyte sedimentation rate; CRP: C-reactive protein. The CT score is the product of the left and right 10 slice area scores and the square of the chest CT density score (range: 0 to 900)
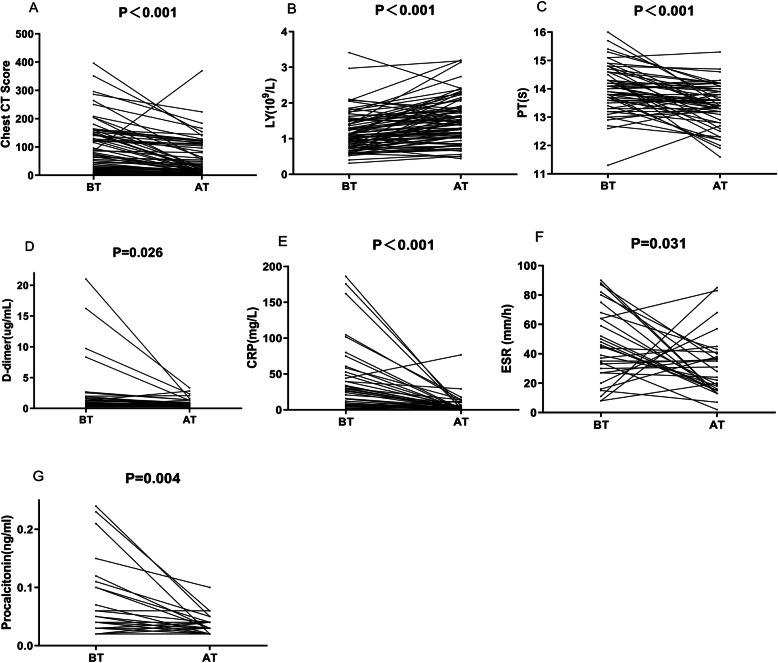
Chest CT score and laboratory parameters before and after treatment
After treatment, the chest CT score (P < 0.001), and the levels of ESR (P = 0.031), CRP (P < 0.001), and procalcitonin (P = 0.004) were significantly lower than before treatment, but the LY count (P < 0.001) was significantly greater (Fig. 4).
Fig. 4.
Changes of chest CT scores and levels of laboratory parameters from before treatment (BT) to after treatment (AT). P values are indicated for the Mann-Whitney test and the t-test for paired samples
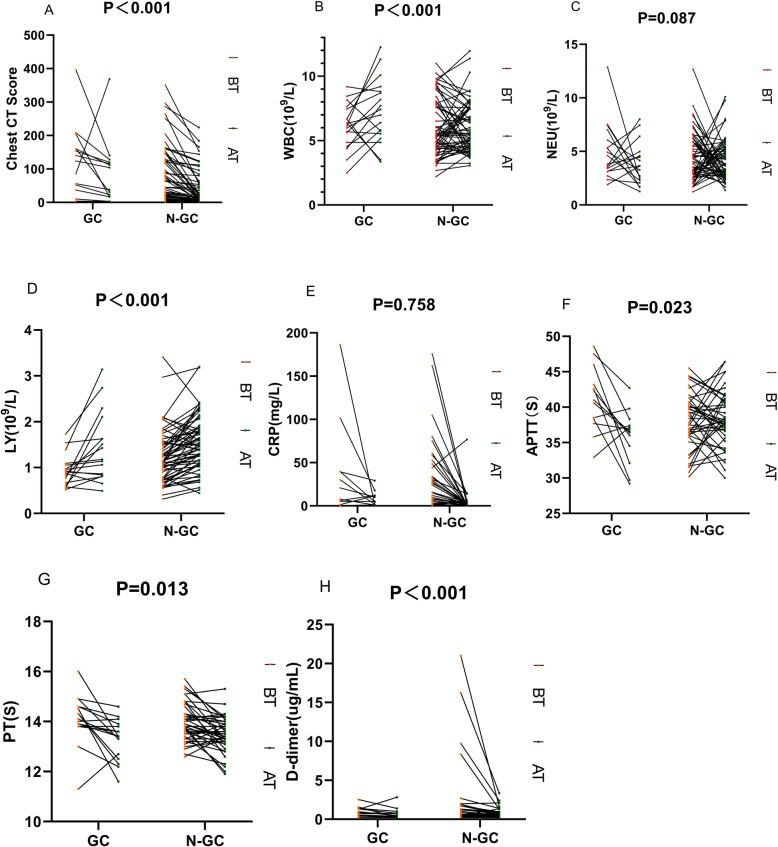
Association of glucocorticoid use with chest CT score and laboratory parameters
We also divided patients into a glucocorticoid group (n = 24, 22%) and a non-glucocorticoid group (n = 84, 78%) and compared their laboratory parameters and chest CT scores after treatment (Fig. 5). The results indicated that glucocorticoid use had significant positive relationships with WBC count (P < 0.001) and LY count (P < 0.001) and significant negative relationships with the levels of activated partial thromboplastin time (APTT, P = 0.023), and PT (P = 0.013). Notably, the CT score declined more in users than non-users of a glucocorticoid (P < 0.001).
Fig. 5.
Changes in 8 laboratory parameters from before treatment (BT) to after treatment (AT) for patients who received glucocorticoid therapy (GC) and did not receive glucocorticoid therapy (N-GC). P values are indicated for intergroup comparisons (GC vs. N-GC) of the amount of change in each variable
Correlations of changes in chest CT score with changes in other laboratory parameters
We further examined the correlation between the change in chest CT score from before to after treatment (ΔCT score) with changes in other laboratory parameters from before to after treatment (Table 4). The results indicated that ΔCT score had a positive correlation with ΔLY count (P = 0.048) and a negative correlation with ΔESR (P = 0.027).
Table 4.
Partial correlation analysis of change in chest CT score from before to after treatment (ΔCT score) with changes in different laboratory parameters (Δ) from before to after treatment
| Laboratory parameter | r | P |
|---|---|---|
| ΔWBC count | 0.171 | 0.184 |
| ΔNeutrophil count | −0.057 | 0.682 |
| ΔLY count | 0.251 | 0.048 |
| ΔESR | −0.451 | 0.027 |
| ΔCRP | 0.029 | 0.868 |
| ΔProcalcitonin | 0.204 | 0.288 |
| ΔD-dimer | −0.068 | 0.679 |
| ΔPT | 0.092 | 0.544 |
| ΔAPTT | 0.034 | 0.827 |
WBC white blood cell, LY lymphocyte, ESR erythrocyte sedimentation rate, CRP C-reactive protein, PT prothrombin time, APTT activated partial thromboplastin time
Discussion
This study indicated that patients who were hospitalized with COVID-19 tended to be older than those in the general population. Among all patients, 68% had one or more coexisting medical conditions, such as hypertension, cardiac disease, or chronic obstructive pulmonary disease. Our finding that COVID-19 is more common in older adults with coexisting chronic diseases is consistent with previous publications [11, 16, 17]. Indeed, elderly men with underlying diseases appear to have the highest risk for development of COVID-19 [18]. The most common symptoms at the onset of illness were fever, dry cough, myalgia, fatigue, dyspnea, and anorexia. The lung CT scans indicated that the most common manifestations were bilateral distribution of patchy shadows and ground glass opacity without pleural effusion. The lung CT results also indicated that the most severely affected patients were older.
Our analysis of laboratory data indicated the LY count was reduced in most patients, and that a greater chest CT score negatively correlated with LY count. This suggests that COVID-19 might act directly upon LYs, especially TLYs, as previously reported for SARS-CoV and MERS-CoV [19, 20]. Recent studies found that the severity of lymphopenia correlated with the severity of COVID-19 [21]. Our results indicated that the chest CT score had a positive correlation with the extent of lymphopenia. In agreement, a previous study reported that the semi-quantitative non-invasive chest CT score reliably predicted COVID-19 prognosis. As viruses spread through the respiratory mucosa and infect other cells, they induce a cytokine storm and a series of immune responses that cause changes in peripheral WBCs and immune cells. Coronviruses invade the lungs, as well as the blood, digestive system, and circulatory system [22–24]. Our analysis indicated that high chest CT score had a positive correlation with abnormal blood coagulation (based on measurements of PT and D-dimer), and severe cases are prone to fibrinolytic activation and excessive bleeding. This is consistent with the findings of Chen et al. [11]. Zhang et al. [25] found coagulation dysfunction and antiphospholipid antibodies in 3 patients with COVID-19; Antiphospholipid antibodies can occur in patients with infectious diseases, and function in the exogenous coagulation pathway. Combined with our research, which indicated no significant relationship of APTT level with chest CT score, we suggest that SARS-CoV-2 may mainly affect the exogenous coagulation pathway.
Our analysis of chest CT scores of patients with COVID-19 indicated that the lesions were mainly at level 5, suggesting that the virus is most abundant in the more active parts of the lung. We also found that the initial chest CT score was positively correlated with the levels of systemic inflammatory factors (CRP and ESR). The overall radiologic score is based on the severity of air-space disease and its distribution. Previous studies found that patients who had viral pneumonias with consolidations evident in lung CT had more severe clinical courses than those who presented with ground glass opacities [26, 27]. These abnormalities also correlated with diffuse alveolar damage [28]. Patients who have COVID-19 and bilateral consolidations tended to have severe systemic inflammation. Because COVID-19 is an extremely contagious and potentially fatal disease, risk stratification using the simple chest CT scoring that we used here may help to appropriately triage patients, so that patients with more severe disease can receive more aggressive treatment and closer monitoring. In other words, the chest CT score should be considered for risk stratification of patients with COVID-19. However, use of initial chest CT scores for prediction of clinical outcome of patients with COVID-19 requires confirmation.
Further genetic, clinical, epidemiological, and clinical studies are needed to examine the efficacy of this semi-quantitative chest CT grading system to predict outcome, evaluate disease phenotypes, monitor disease progression, and evaluate treatment response and efficacy for other forms of viral pneumonia or air space diseases.
Due to the serious adverse effects of glucocorticoids experienced by patients with SARS-CoV infections [29, 30], it is questionable whether glucocorticoids should be used to treat patients with SARS-CoV-2 infections [31, 32]. Our results showed that patients who received glucocorticoids had greater improvements of chest CT score and LY count. This suggests that moderate application of glucocorticoids may have a positive effect in these patients. Our regression analysis indicated that the change of chest CT score after treatment had a positive correlation with the change in LY count, indicating that the chest CT score is useful in assessing patient status before and after treatment.
There were several limitations in this study. First, this was retrospective study and included only relatively small number of cases. All patients were reported to the CDC from January 2020 to February 202,020 and required hospitalization, but were not admitted to the ICU. Therefore, the analysis was biased toward patients with more severe forms of COVID-19. However, the patients we examined were from the general ward, and none were admitted to the ICU. Therefore, many patients with COVID-19 have higher chest CT scores. Second, because we only examined five levels in the chest CT examinations, we may have missed some lesions. Last, because of time constraints, we only performed a cross-sectional study, and did not perform follow-up CT scans. All chest CT images were from patients at the time of admission and prior to treatment.
Some of the patients we examined progressed rapidly to ARDS, septic shock, and then multiple organ failure. Therefore, early identification and timely treatment of these critical cases is of crucial importance. The chest CT score is a non-invasive method that provides an actionable means for achieving this goal.
Conclusions
In conclusion, the chest CT score of patients with COVID-19 is associated the severity of the systemic inflammatory response. The damage from SARS-CoV-2 infection is greater in more active parts of the lung. Because COVID-19 is potentially fatal and highly contagious, risk stratification based on air-space disease may help to triage patients, guide treatment, and monitor disease progression and treatment.
Supplementary information
Additional file 1: Figure S1. A, suprasternal notch; B, aortic arch; C, tracheal carina; D, intermediate bronchus; E, apex of diaphragm.
Acknowledgements
Not applicable.
Abbreviations
- CT
Computed tomography
- CRP
C-reactive protein
- ESR
Erythrocyte sedimentation rate
- LY
Lymphocyte
- WBC
White blood cell
- SARS
Severe acute respiratory syndrome
- ARDS
Acute respiratory distress syndrome
- MERS
Middle East respiratory syndrome
- CK-MB
Creatine kinase-MB
- GGO
Ground-glass opacity
- NEU
Neutrophil
- PT
Prothrombin time
- APTT
Activated partial thromboplastin time
Authors’ contributions
JZ, GM and WL carried out the data collection, literature review and drafting of the manuscript. BS, HD contributed to the drafting of the manuscript and aided in the literature review. ZS, and QH participated in the data collection and the drafting of the manuscript. PG help to draft the manuscript and revised the final version of the manuscript. All authors read and approved the final manuscript.
Funding
Not applicable.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Ethics approval and consent to participate
Ethics Committee of the Second Hospital of Jilin University approved this study.
Consent for publication
Oral consent to publish was obtained from all patients in this study.
Competing interests
All authors have read and approved the content, and declare no conflicts of interest. There is no ethical/legal conflicts involved in the article.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Jie Zhang, Guangping Meng and Wei Li contributed equally to this work.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s12931-020-01440-x.
References
- 1.Wuhan Municipal Health Commission . Report of clustering pneumonia of unknown etiology in Wuhan City. 2019. [Google Scholar]
- 2.Lu H, Stratton CW, Tang YW. Outbreak of pneumonia of unknown etiology in Wuhan, China: the mystery and the miracle. J Med Virol. 2020;92:401–402. doi: 10.1002/jmv.25678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Health Commission of the People’s Republic of China . Report Aggregated pneumonia of unknown etiology China. 2020. [Google Scholar]
- 4.WHO . Novel coronavirus (2019-nCoV) 2020. [Google Scholar]
- 5.Hui DS, Azhar EI, Madani TA, Ntoumi F, Kock R, Dar O, Ippolito G, McHugh TD, Memish ZA, Drosten C, et al. The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health - the latest 2019 novel coronavirus outbreak in Wuhan, China. Int J Infect Dis. 2020;91:264–266. doi: 10.1016/j.ijid.2020.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, Zhao X, Huang B, Shi W, Lu R, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.WHO . Clinical management of severe acute respiratory infection when Novel coronavirus (nCoV) infection is suspected: interim guidance. 2020. [Google Scholar]
- 9.Yin Y, Wunderink RG. MERS, SARS and other coronaviruses as causes of pneumonia. Respirology. 2018;23:130–137. doi: 10.1111/resp.13196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cui J, Li F, Shi ZL. Origin and evolution of pathogenic coronaviruses. Nat Rev Microbiol. 2019;17:181–192. doi: 10.1038/s41579-018-0118-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pediatric Branch of Hubei Medical A, Pediatric Branch of Wuhan Medical A, Pediatric Medical Quality Control Center of H Recommendation for the diagnosis and treatment of novel coronavirus infection in children in Hubei (Trial version 1) Zhongguo Dang Dai Er Ke Za Zhi. 2020;22:96–99. doi: 10.7499/j.issn.1008-8830.2020.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pan Y, Guan H, Zhou S, Wang Y, Li Q, Zhu T, Hu Q, Xia L. Initial CT findings and temporal changes in patients with the novel coronavirus pneumonia (2019-nCoV): a study of 63 patients in Wuhan. Eur Radiol: China; 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.National Health Commission of the People’s Republic of China . Diagnosis and Treatment of Pneumonia Caused by New Coronavirus (Trial Version 4) 2020. [Google Scholar]
- 15.Feng F, Jiang Y, Yuan M, Shen J, Yin H, Geng D, Xu J, Hua Y, Shi J, Shi Y, Zhang Z. Association of radiologic findings with mortality in patients with avian influenza H7N9 pneumonia. PLoS One. 2014;9:e93885. doi: 10.1371/journal.pone.0093885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kui L, Fang YY, Deng Y, Liu W, Wang MF, Ma JP, Xiao W, Wang YN, Zhong MH, Li CH, et al. Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province. Chin Med J. 2020;133(9):1025–1031. doi: 10.1097/CM9.0000000000000744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Special Expert Group for Control of the Epidemic of Novel Coronavirus Pneumonia of the Chinese Preventive Medicine A An update on the epidemiological characteristics of novel coronavirus pneumoniaCOVID-19. Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41:139–144. doi: 10.3760/cma.j.issn.0254-6450.2020.02.002. [DOI] [PubMed] [Google Scholar]
- 19.Channappanavar R, Zhao J, Perlman S. T cell-mediated immune response to respiratory coronaviruses. Immunol Res. 2014;59:118–128. doi: 10.1007/s12026-014-8534-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chu H, Zhou J, Wong BH, Li C, Chan JF, Cheng ZS, Yang D, Wang D, Lee AC, Li C, et al. Middle East respiratory syndrome coronavirus efficiently infects human primary T lymphocytes and activates the extrinsic and intrinsic apoptosis pathways. J Infect Dis. 2016;213:904–914. doi: 10.1093/infdis/jiv380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, Wu Y, Zhang L, Yu Z, Fang M, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gambotto A, Barratt-Boyes SM, de Jong MD, Neumann G, Kawaoka Y. Human infection with highly pathogenic H5N1 influenza virus. Lancet. 2008;371:1464–1475. doi: 10.1016/S0140-6736(08)60627-3. [DOI] [PubMed] [Google Scholar]
- 23.Lau SK, Lau CC, Chan KH, Li CP, Chen H, Jin DY, Chan JF, Woo PC, Yuen KY. Delayed induction of proinflammatory cytokines and suppression of innate antiviral response by the novel Middle East respiratory syndrome coronavirus: implications for pathogenesis and treatment. J Gen Virol. 2013;94:2679–2690. doi: 10.1099/vir.0.055533-0. [DOI] [PubMed] [Google Scholar]
- 24.Wauquier N, Becquart P, Padilla C, Baize S, Leroy EM. Human fatal Zaire ebola virus infection is associated with an aberrant innate immunity and with massive lymphocyte apoptosis. PLoS Negl Trop Dis. 2010;4:e837. doi: 10.1371/journal.pntd.0000837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang Y, Xiao M, Zhang S, Xia P, Cao W, Jiang W, Chen H, Ding X, Zhao H, Zhang H, et al. Coagulopathy and Antiphospholipid antibodies in patients with Covid-19. N Engl J Med. 2020;382:e38. doi: 10.1056/NEJMc2007575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grinblat L, Shulman H, Glickman A, Matukas L, Paul N. Severe acute respiratory syndrome: radiographic review of 40 probable cases in Toronto, Canada. Radiology. 2003;228:802–809. doi: 10.1148/radiol.2283030671. [DOI] [PubMed] [Google Scholar]
- 27.Gattinoni L, Caironi P, Cressoni M, Chiumello D, Ranieri VM, Quintel M, Russo S, Patroniti N, Cornejo R, Bugedo G. Lung recruitment in patients with the acute respiratory distress syndrome. N Engl J Med. 2006;354:1775–1786. doi: 10.1056/NEJMoa052052. [DOI] [PubMed] [Google Scholar]
- 28.Marchiori E, Zanetti G, Fontes CA, Santos ML, Valiante PM, Mano CM, Teixeira GH, Hochhegger B. Influenza a (H1N1) virus-associated pneumonia: high-resolution computed tomography-pathologic correlation. Eur J Radiol. 2011;80:e500–e504. doi: 10.1016/j.ejrad.2010.10.003. [DOI] [PubMed] [Google Scholar]
- 29.Li N, Wang GF, Wu YF, Xie GQ, Xiao F, Chen BW, Wang YX. Han DM: [side effects of glucocorticosteroids in the management of 1291 patients of SARS] Beijing Da Xue Xue Bao. 2004;36:519–524. [PubMed] [Google Scholar]
- 30.Zhao R, Wang H, Wang X, Feng F. Steroid therapy and the risk of osteonecrosis in SARS patients: a dose-response meta-analysis. Osteoporos Int. 2017;28:1027–1034. doi: 10.1007/s00198-016-3824-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Xu K, Cai H, Shen Y, Ni Q, Chen Y, Hu S, Li J, Wang H, Yu L, Huang H, et al. Management of corona virus disease-19 (COVID-19): the Zhejiang experience. Zhejiang Da Xue Xue Bao Yi Xue Ban. 2020;49:0. doi: 10.3785/j.issn.1008-9292.2020.02.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ling Y, Xu SB, Lin YX, Tian D, Zhu ZQ, Dai FH, Wu F, Song ZG, Huang W, Chen J, et al. Persistence and clearance of viral RNA in 2019 novel coronavirus disease rehabilitation patients. Chin Med J. 2020;133(9):1039–1043. doi: 10.1097/CM9.0000000000000774. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Figure S1. A, suprasternal notch; B, aortic arch; C, tracheal carina; D, intermediate bronchus; E, apex of diaphragm.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.