Dear Editor,
Infectious disease outbreaks such as COVID-19, as well as other public health events, can cause emotional distress and anxiety even in people not at high risk of getting sick [1–3]. People with neurodegenerative diseases, particularly those associated with impaired respiratory function, are at risk of severe complications and more likely to report negative mental health outcomes. In this context, amyotrophic lateral sclerosis (ALS) patients are particularly vulnerable to either medical complications of infection or emotional distress in terms of anxiety and depression. Importantly, anxiety and depression have been already reported in 30% [4] and 44% [4] of these patients, respectively. The percentages of these psychiatric symptoms are above the rates of general population and are more severe in patients who present concomitant cognitive and behavioural dysfunctions or express a wish to die [5]. Additionally, studies have shown that emotional distress, such as anxiety and depression, seems to be strongly linked to inner bodily sensations, the so-called interoceptive awareness or self-awareness [6]. Lastly, ALS patients may also exhibit maladaptive coping strategies [7], which make them even more susceptible to detrimental neuropsychiatric effects of the outbreak.
On these bases, we aimed to investigate the emotional impact of COVID-19 outbreak in a sample of ALS by assessing anxiety, depression symptoms and self-awareness and comparing such results with those obtained by their caregivers.
This study was conducted on a group of patients with definite or probable diagnosis of ALS (n = 23; age (years) = 61.91 ± 2.08; sex (M/F) = 13/10; education level (years) = 11.30 ± 0.79; disease duration (years) = 2.99 ± 0.32), whose cognitive and psychopathological baseline data were collected before the outbreak (January and February 2020). During the outbreak, these patients completed a follow-up assessment between the 20th of March and 5th of April, by means of an online interview and with the same trained interviewers (F.P.A. and M.S.) of baseline data. Scales were sent to the patients in advance via mail to prepare them for the interviews and consisted of Hamilton Depression Scale (HDS) [8] and Beck Anxiety Inventory (BAI) [9] to identify clinically relevant depression and anxiety by measuring the severity of symptoms and the Self-Awareness Questionnaire (SAQ) to assess the experience and frequency of internal bodily feelings, evaluating both somatosensory and visceral sensations [10]. During the outbreak, these psychological scales were also applied to ALS patients’ caregivers as control group (n = 21, age (years) = 57.9 ± 3.42, sex (M/F) = 10/11, education (years) = 12.10 ± 0.76). Demographic data (age, sex and education) did not significantly differ between patients and caregivers (all p > 0.45). Neither patients nor caregivers got infected with the virus.
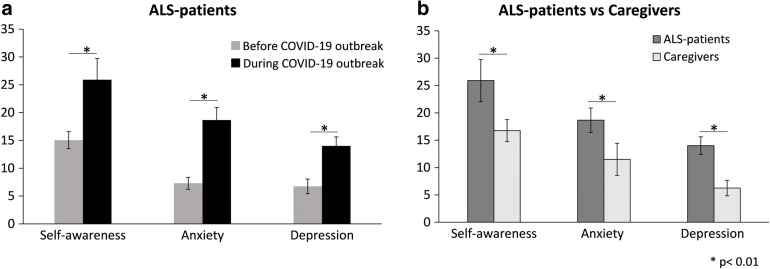
At baseline, cognitive assessment of patients showed mild cognitive impairment involving executive (ALS-eci) or non-executive (i.e. memory) functions (ALS-neci) in 73.91% (17/23) as assessed by the Edinburgh Cognitive and Behavioural ALS Screen (ECAS) [11]. Motor dysfunction evaluated with the Revised Amyotrophic Lateral Sclerosis Functional Rating Scale (ALSFRS-R) did not significantly worsen during the follow-up (before outbreak, average ± standard deviation: 32.35 ± 7.38, range 21–45; during outbreak, average ± standard deviation: 31.83 ± 8.53, range 16–45, p = 0.47). Moreover, a paired t test showed that in patients’ sample scores on depression, anxiety and self-awareness tests were significantly higher during the outbreak respect to the baseline data (all p < 0.01) (Fig. 1a). A multivariate analysis of variance showed that during outbreak, patients scored significantly poorer than caregivers on depression (p < 0.001), anxiety (p < 0.001) and self-awareness (p < 0.001) tests, F(3, 38) = 4.224, Wilks’ lambda = 0.75, p = 0.01 (Fig. 1b). Interestingly, caregivers during the outbreak exhibited scores over the pathological cut-off at HDS and BAI in 28.57% (6/21) of cases, reaching the highest scores corresponding to severe symptoms of anxiety in 19.05% of cases (4/21) and depression in 9.52% of cases (2/21). As expected, ALS patients, compared to caregivers, showed higher percentages of pathological scores at both scales during the pandemic, reaching 65.22% (15/23) of cases for depression symptoms and 78.26% (18/23) for anxiety. Moreover, these percentages were significantly higher with respect to the baseline condition (HDS: 30.43% vs 65.22%, p = 0.018; BAI: 34.78% vs 78.26%, p = 0.003), suggesting that clinically relevant anxiety and depression developed due to the situational distress of the outbreak.
Fig. 1.
Panel a shows the worsening of self-awareness, anxiety and depression symptoms in ALS population during the COVID-19 outbreak with respect to the pre-COVID phase. Panel b shows that the three parameters of emotional burden were significantly worse in ASL patients with respect to their caregivers during the outbreak. Bar represents the mean value; error bars indicate standard error. *p < 0.01
This small survey was an opportunity to explore how patients with ALS and their caregivers cope with an emerging challenge to global healthcare systems and a situation that strikes symptoms related to depression and anxiety within the general population about an unknown disease. We showed that patients with ALS exhibited a worsening of depressive and anxiety symptoms associated to altered interoceptive awareness during the outbreak, and this emotional burden was much more pronounced in patients with respect to caregivers. Caregivers displayed a high level of anxiety and depression in a significant percentage of cases, suggesting that outbreak had a significant impact on them as well, and in line with the previous literature [12].
We should, anyway, acknowledge that a major limitation of our study is the lack of a healthy subject group; therefore, we cannot be entirely sure that our findings are specific for ALS patients and their caregivers. Future studies enrolling a larger ALS population together with caregivers’ and healthy subjects’ groups are warranted to address this issue.
Considering the rapid worldwide spread of the COVID-19 outbreak, ALS specialists should consider to adopt strategies to monitor the psychopathological complications of the pandemic. Importantly, when planning support strategies (i.e. online psychological consultation, antidepressant and anxiolytic medications), special attention should be paid on patients at higher risk to develop cognitive and neuropsychiatric complications.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
The protocol was approved by the local ethics committee, and the research was conducted in accordance with the 1964 Declaration of Helsinki.
Footnotes
Natascia De Lucia and Francesco Pio Ausiello equally contributing as first authors
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, Ho RC. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17:1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatry. 2020;33:e100213. doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, Rubin GJ. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kurt A, Nijboer F, Matuz T, Kübler A. Depression and anxiety in individuals with amyotrophic lateral sclerosis: epidemiology and management. CNS Drugs. 2007;21:279–291. doi: 10.2165/00023210-200721040-00003. [DOI] [PubMed] [Google Scholar]
- 5.Rabkin J, Goetz R, Murphy JM, Factor-Litvak P, Mitsumoto H, ALS COSMOS Study Group Cognitive impairment, behavioral impairment, depression, and wish to die in an ALS cohort. Neurology. 2016;87:1320–1328. doi: 10.1212/WNL.0000000000003035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Paulus MP, Stein MB. Interoception in anxiety and depression. Brain Struct Funct. 2010;214:451–463. doi: 10.1007/s00429-010-0258-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hecht M, Hillemacher T, Gräsel E, et al. Subjective experience and coping in ALS. ALS Other Mot Neuron Disord. 2002;4:225–231. doi: 10.1080/146608202760839009. [DOI] [PubMed] [Google Scholar]
- 8.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56:893–897. doi: 10.1037/0022-006X.56.6.893. [DOI] [PubMed] [Google Scholar]
- 10.Longarzo M, D’Olimpio F, Chiavazzo A, et al. The relationships between interoception and alexithymic trait. The self-awareness questionnaire in healthy subjects. Front Psychol. 2015;6:1149. doi: 10.3389/fpsyg.2015.01149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Abrahams S, Newton J, Niven E, Foley J, Bak TH. Screening for cognition and behaviour changes in ALS. Amyotroph Lateral Scler Front Degener. 2014;15:9–14. doi: 10.3109/21678421.2013.805784. [DOI] [PubMed] [Google Scholar]
- 12.Prasad S, Holla VV, Neeraja K, Surisetti BK, Kamble N, Yadav R, Pal PK. Parkinson’s disease and COVID-19: perceptions and implications in patients and caregivers. Mov Disord. 2020;35:1–4. doi: 10.1002/mds.28088. [DOI] [PMC free article] [PubMed] [Google Scholar]