Dear Editor,
Previous studies demonstrated that a combination of hydrocortisone, vitamin C, and thiamine (HVT) is a promising adjuvant treatment for sepsis and septic shock, with decreased mortality and improved resolution of disease [1]. However, recently published prospective, randomized controlled trials (RCTs) did not support this finding [2]. Therefore, we performed a meta-analysis to evaluate the efficacy of HVT treatment for patients with sepsis or septic shock.
This meta-analysis was performed strictly following the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) statement [3]. The primary outcomes were mortality, decrease of sequential organ failure assessment score from baseline (Delt SOFA), and time of vasopressors use. Relative risk (RR) with 95% confidence intervals (CIs) and weighted mean differences (WMDs) with 95% CIs were used. Meta-analyses were performed using a random-effects model by RevMan version 5.1.
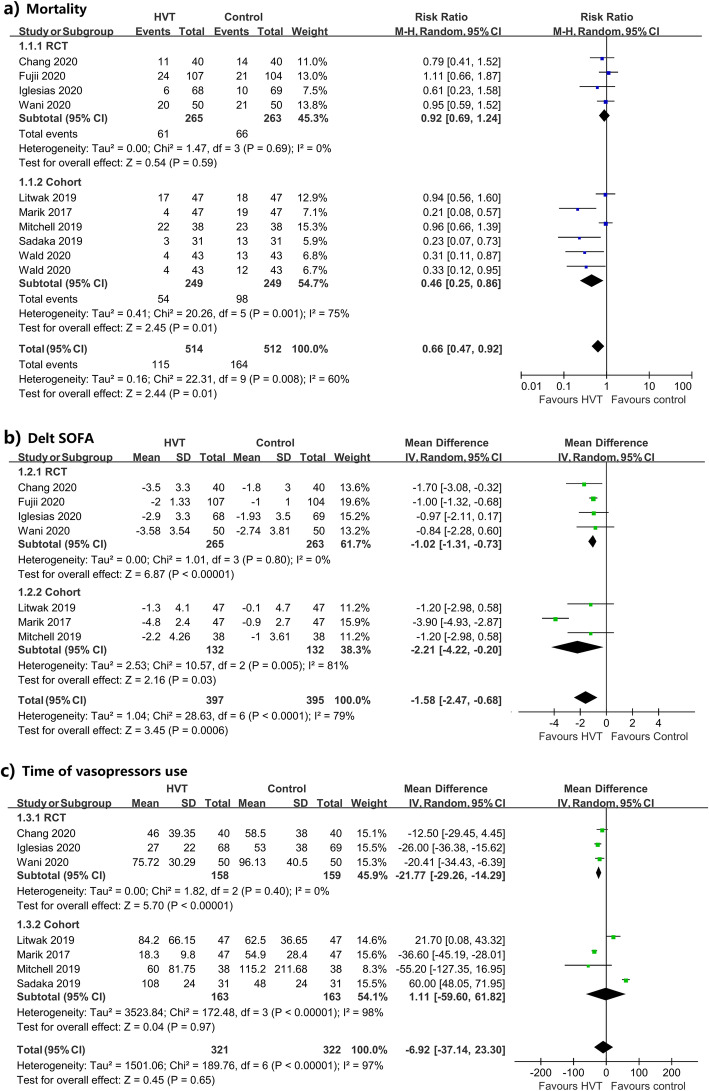
Four RCTs with 528 patients and five cohorts involving 412 patients were included, as described in Table 1. As shown in Fig. 1, pooled results from RCTs showed that HVT has no benefit on mortality (RR 0.92, 95%CI 0.69 to 1.24, p = 0.59; I2 = 0%, PH = 0.69), while it was associated with a significant decrease of SOFA (Delt SOFA: WMD − 1.02, 95%CI − 1.31 to − 0.73, p < 0.001; I2 = 0%, PH = 0.80) and reduction in time of vasopressors use (WMD − 21.77 h, 95%CI − 29.26 to − 14.29, p < 0.001; I2 = 0%, PH = 0.4). Overall results from cohorts revealed that HVT could significantly reduce mortality (RR0.46, 95%CI 0.25 to 0.86, p = 0.01; I2 = 75%, PH = 0.001) and SOFA score (Delt SOFA: WMD − 2.21, 95%CI − 4.22 to − 0.20, p = 0.03; I2 = 81%, PH = 0.005), but not the duration of vasopressors use (WMD 1.11 h, 95%CI − 59.60 to 61.82, p = 0.97; I2 = 98%, PH < 0.001). No differences in intensive care unit (ICU) length of stay and hospital length of stay between the HVT and the control group were observed.
Table 1.
Baseline characteristics of the included studies
| Study ID | Country | Study design | No. (HVT/Con) | Patient | Intervention | |
|---|---|---|---|---|---|---|
| HVT group | Control | |||||
| Chang 2020, PMID: [32243943] | China | Single-blinded RCT | 40/40 | Adult patients with sepsis or septic shock and procalcitonin PCT ≥ 2 ng/mL |
- IV hydrocortisone (50 mg every 6 h for 7 days) - IV vitamin C (1.5 g every 6 h for 4 days) - IV thiamine (200 mg every 12 h for 4 days) - Standard care |
- Placebo (normal saline) - Standard care |
| Fujii 2020, PMID: [31950979] | Australia, New Zealand, Brazil | Multicenter, open-label RCT | 107/104 | Adult patients with septic shock |
- IV hydrocortisone (50 mg every 6 h for a maximum of 7 days) - IV vitamin C (1.5 g every 6 h for a maximum of 10 days) - IV thiamine (200 mg every 12 h for a maximum of 10 days) - Standard care |
- IV hydrocortisone (50 mg every 6 h) - Standard care |
| Igelesia 2020, PMID: [32194058] | USA | Double-blinded RCT | 68/69 | Adult patients with sepsis or septic shock |
- IV hydrocortisone (50 mg every 6 h) - IV vitamin C (1.5 g every 6 h) -IV thiamine (200 mg every 12 h) for a maximum of 4 days - Standard care |
- Placebo (normal saline) - Standard care |
| Wani 2020, PMID: [31990246] | India | Open-label RCT | 50/50 | Adult patients with sepsis or septic shock and serum lactate level of > 2 mmol/L |
- IV hydrocortisone (50 mg q 6 hourly for 7 days or until ICU discharge) - IV vitamin C (1.5 g every 6 h for 4 days or until discharge) - IV thiamine (200 mg q 12 hourly for 4 days or until discharge) - Standard care |
- Standard care alone |
| Litwak 2019, PMID [30970560] | USA | Retrospective cohort study | 47/47 | Adult patient with septic shock |
- IV hydrocortisone (200–300 mg every day) - IV vitamin C (1.5 g every 6 h) - IV thiamine (200 mg every 12 h) for 4 days - Standard care |
- Standard care and/or IV hydrocortisone |
| Marik 2017, PMID: [27940189] | USA | Retrospective cohort study | 47/47 | Adult patients with severe sepsis or septic shock and PCT > 2 ng/mL |
- IV hydrocortisone (50 mg every 6 h for 7 days or until ICU discharge) - IV vitamin C (1.5 g every 6 h for 4 days or until ICU discharge) - IV thiamine (200 mg every 12 h for 4 days or until ICU discharge) |
- IV hydrocortisone (50 mg every 6 h) - Standard care |
| Mitchell 2019, PMID: [31469984] | USA | Retrospective cohort study | 38/38 | Adult patients with severe sepsis or septic shock |
- IV hydrocortisone (50 mg every 6 h, 100 mg every 8 h, or 10 mg per h for 7 days) - IV vitamin C (1.5 g every 6 h for 4 days) - IV thiamine (200 mg IV every 1 for 4 days) - Standard care |
- IV hydrocortisone - Standard care |
| Sadaka 2019, PMID: [31315499] | USA | Retrospective cohort study | 31/31 | Adult patients with septic shock |
- IV hydrocortisone (50 mg every 6 h for 7 days) - IV vitamin C (1.5 g every 6 h for 4 days) - IV thiamine (200 mg every 12 h for 4 days) - Standard care |
- Standard care alone |
| Wald 2020, PMID: [31916841] | USA | Retrospective cohort study | 43/43(a)/43(b) | Pediatric patients with septic shock |
- IV hydrocortisone (50 mg/m2/day divided every 6 h) - IV vitamin C (30 mg/kg/dose every 6 h for 4 days; maximum 1.5 g/dose) - IV thiamine (4 mg/kg/day for 4 days; maximum 200 mg/dose) - Standard care |
a) Hydrocortisone only; b) standard care alone |
PMID PubMed unique identifier; RCT randomized controlled trial; HVT hydrocortisone, vitamin C, and thiamine; Con control; PCT procalcitonin; IV intravenous; h hour
Fig. 1.
Forest plots for the primary outcome. a Mortality. b Delt SOFA. c Time of vasopressors use
Our study suggested that HVT has potential beneficial effects. A significant reduction in SOFA score was observed, although no benefit of mortality in the pooled effect of RCTs. Since it is a valuable end-point reflecting the disease process and also a surrogate marker for mortality, our meta-analysis of the four small RCTs might be inadequate to detect a mortality benefit. Additionally, the improved resolution of shock from RCTs also supports HVT use.
A generally recognized concept is that the HVT could synergistically restore the dysregulated immune system, oxidative mitochondrial function, and energy production [4]. However, current clinical practice regarding the HVT strategy is still debating. Besides the potential synergistic beneficial effects, the arguments supporting the use of HVT include low risk, low cost, and easy availability. Minor clinical side effects, such as hyperglycemia, hypertension, and hypernatremia induced by hydrocortisone [5], might occur but are insignificant and easily managed in ICU.
Some limitations merit consideration. Sample sizes in RCTs are small, and pooled effects on different outcomes are inconsistent. Though potential bias in cohort studies, the pooled result of cohort studies in our study supported and consolidated the findings from RCTs. Additionally, hydrocortisone was not systematically used for control groups in RCTs and cohorts. It is thus questionable to determine the benefit is from the synergistic effect of HVT or corticosteroid only, since the beneficial effect of corticosteroid sole has been well established [6]. Besides, other clinical heterogeneities, such as the timing of HVT and severity of the disease, should also be regarded. However, the data sparseness of included studies limited our subgroup analysis for further exploration.
In conclusion, the beneficial findings of our study support that HVT remains an attractive choice for sepsis and septic shock, while results from large-scale RCTs are still expected before a definite conclusion, especially in terms of the timing of HVT and the severity of sepsis.
Acknowledgements
None.
Abbreviations
- HVT
Hydrocortisone, vitamin C, and thiamine
- RCTs
Randomized controlled trials
- WMDs
Weighted mean differences
- RR
Relative risks
- CIs
Confidence intervals
Authors’ contributions
RS and HTT conceived the study, participated in the design, and collected the data. HTT performed the statistical analyses. RS drafted the manuscript. HTT revised the manuscript critically for important intellectual content. All authors read and approved the final manuscript.
Authors’ information
HTT is now working as a cardiothoracic surgeon in the Department of Cardiothoracic Surgery, The First Affiliated Hospital of Chongqing Medical University.
Funding
None.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Rui Shi, Email: shiruidingding@hotmail.com.
Hongtao Tie, Email: hongtaotie@163.com.
References
- 1.Marik PE, Khangoora V, Rivera R, Hooper MH, Catravas J. Hydrocortisone, vitamin C, and thiamine for the treatment of severe sepsis and septic shock: a retrospective before-after study. Chest. 2017;151(6):1229–1238. doi: 10.1016/j.chest.2016.11.036. [DOI] [PubMed] [Google Scholar]
- 2.Fujii T, Luethi N, Young PJ, et al. Effect of vitamin C, hydrocortisone, and thiamine vs hydrocortisone alone on time alive and free of vasopressor support among patients with septic shock: the VITAMINS Randomized Clinical Trial. JAMA. 2020;323(5):423–431. doi: 10.1001/jama.2019.22176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moher D, Liberati A, Tetzlaff J, et al. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 4.Marik PE. Hydrocortisone, ascorbic acid and thiamine (HAT therapy) for the treatment of sepsis. Focus on Ascorbic Acid Nutrients. 2018;10(11):1762. doi: 10.3390/nu10111762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Briegel J, Huge V, Möhnle P. Hydrocortisone in septic shock: all the questions answered? J Thorac Dis. 2018;10(Suppl 17):S1962–S1965. doi: 10.21037/jtd.2018.04.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rygard SL, Butler E, Granholm A, et al. Low-dose corticosteroids for adult patients with septic shock: a systematic review with meta-analysis and trial sequential analysis. Intensive Care Med. 2018;44(7):1003–1016. doi: 10.1007/s00134-018-5197-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.