Abstract
Study Design:
Retrospective cohort study.
Objective:
Screw loosening in spinal fusion is poorly defined. Accordingly, its prevalence rates range from 1% to 60%, and its risk factors remain undefined. The goal of this study was to assess the prevalence of screw loosening, according to precise definitions, and to identify factors associated with it.
Methods:
We retrospectively reviewed records for 166 patients who underwent a posterior spinal fusion in our institution between 2011 and 2016. We recorded demographic data, osteoporosis, pelvic balance, surgery-related information, and postoperative radiographic data at a minimum follow-up of 6 months. Univariable and multivariable logistic regression models were used. Significance was defined by P < .05.
Results:
When loosening was defined by partial pull-out, its prevalence was 9.6% (95% CI 5.6-15); thoracic localization, the use of CrCo (chromium-cobalt) rods, osteoporosis, PI/LL (pelvic incidence/lumbar lordosis) mismatch (preoperative), and frontal imbalance (preoperative) were significant risk factors. When loosening was defined by osteolysis (radiolucent rim) >1 mm around at least 1 screw, its prevalence was 40.4% (95% CI 33-48) and age, scoliosis as indication for fusion, ASA (American Society of Anesthesiologists) 2 or 3, the use of CrCo rods, more than 5 levels fused, no circumferential arthrodesis, postoperative bracing, and sacrum or ilium as the inferior level of instrumentation were also significant risk factors.
Conclusions:
A clear definition of screw loosening seems essential for a useful analysis of the literature. Osteoporosis, sagittal imbalance, and rigid material appear to be risk factors, regardless of the definition.
Keywords: pedicle screw, osteoporosis, fusion, loosening, spine surgery
Introduction
As populations age, spine surgeons see ever more patients with degenerative spine diseases, such as discopathy, articular destabilization and spinal static disorders. These affect patients’ quality of life substantially.1 When medical treatment is no longer effective, surgery is needed, often vertebral fusion by the placement of pedicular implants combined with a bone graft.2-6 Since the 2000s, the rate of long spinal fusions among patients older than 65 years has increased exponentially.7 Moreover, the population of that age is predicted to double by 2050.8 This increasingly older population, however, has comorbidities that affect the prognosis of spinal fusion surgery. In particular, bone quality is crucial for holding vertebral implants in place, but bone mass is known to diminish by as much as 50% in elderly women and 30% in elderly men.9 This reduction causes a decrease of primary fixation of pedicle implants and risks the early loosening of arthrodesis, which may in turn lead to pseudarthrosis, chronic pain, and the need for reoperation, sometimes associated with high patient morbidity.10
Although the complication of loosening is recurrent in clinical practice for spinal fusion, especially among patients with osteoporosis, it is poorly defined in the literature. Although it is a frequent secondary outcome of clinical studies, its definition varies from one article to another. Some authors define it as the appearance of a radiolucent rim >1 mm around at least one screw on radiography or computed tomography (CT) scan, with or without related symptoms; although others define it as a complete pull-out of implants, symptomatic and requiring surgical revision.11-13 Although it has been shown that the appearance of a rim >1 mm around screws decreases the extraction torque of implants significantly, no conclusion can be reached about its clinical significance.14 Moreover, the prevalence of loosening (ranging from 1% to 60% in the literature) and its functional prognosis both remain unclear.15
The aim of this study was to define the prevalence of screw loosening in spinal fusion, according to whether it is defined as a pulled-out screw or a radiolucent rim ≥1 mm around it.
The secondary goal was to determine the risk factors associated with this complication.
Materials and Methods
We retrospectively reviewed all patients who underwent a posterior spinal fusion during the 28-month period between January 1, 2011 and May 1, 2016, in our orthopedic center specialized in spine surgery.
The exclusion criteria were as follows: age <18 years, surgery for causes related to trauma, tumors or primary infection, the use of cemented screws, an anterior-only approach, a follow-up of less than 1 year, or the lack of radiographic (anteroposterior [AP] and lateral full-spine pre- and postoperative radiographs) or clinical data.
The preoperative data collected was demographic (age, gender, American Society of Anesthesiologists [ASA] score, body mass index [BMI], tobacco/alcohol use), clinical (related to poor bone quality: menopause, level of physical activity, corticosteroid treatment, neurodegenerative disease, osteoporosis treatment and its duration), and the indication for surgery (degenerative/scoliosis/spondylolisthesis). The surgical data included surgeon’s status (junior/senior); number of fused levels and their upper and lower limits, any associated spine liberation, pelvic fusion, instrumentation at each level); type of implants (chromium-cobalt [CrCo]/titanium, diameter of rods, cross links, hooks, circumferential); and the postoperative course (infection, type and duration of immobilization, release from the hospital to home, rehabilitation center).
With the preoperative radiography, we assessed the sagittal balance data (pelvic incidence [PI], lumbar lordosis [LL], and PI/LL match), Singh classification,16 and C7 plumb line. On the final follow-up radiographs, we assessed sagittal and frontal balance with the same measurements. LL was defined as the L1-S1 angle on sagittal radiography and measured by Cobb’s method.17 The PI was measured as described by Marty et al.18
The primary outcome was the prevalence of “screw loosening” as a complication based on each of 2 definitions: radiolucent rim >1 mm around a screw or a pulled-out screw on the last follow-up radiography. Two independent spine surgeons used PACS software (AGFA Healthcare) for the radiographic measurements.
No institutional review board approval was needed for this study.
Univariable and multivariable logistic regression models were computed to look for variables associated with a radiolucent rim; because of the limited number of events observed, univariable models only were used to predict pulled-out screws. Variables with a relevant effect (P < .1) on the primary outcome in univariable models were fitted into a multivariable model; a final model was developed using a stepwise selection based on Akaike information criteria (stepwise backward and forward model selection).19
Results
The cohort comprised 116 women and 50 men (sex ratio 0.43). Their mean age was 67 years (Q1-Q3 58-73), and their mean BMI 26 kg/m2.
Table 1 summarizes the other preoperative demographic and clinical data.
Table 1.
Cohort’s Preoperative Demographic and Clinical Data.
| Characteristic | n | % |
|---|---|---|
| Sex | ||
| Male | 50 | 30.1 |
| Female | 116 | 60.9 |
| Indication | ||
| Degenerative | 86 | 51.8 |
| Scoliosis | 52 | 31.3 |
| Spondylolisthesis | 28 | 16.9 |
| ASA (American Society of Anesthesiologists) | ||
| 1 | 50 | 30.1 |
| 2 | 100 | 60.2 |
| 3-4 | 16 | 9.6 |
| Addiction | ||
| Alcohol | 16 | 9.6 |
| Tobacco | 67 | 40.4 |
| Singh classification | ||
| 1 | 1 | 0.6 |
| 2 | 14 | 8.4 |
| 3 | 35 | 21.1 |
| 4 | 42 | 25.3 |
| 5 | 51 | 30.7 |
| 6 | 23 | 13.9 |
| Osteoporosis treatment (yes) | 25 | 15.1 |
| Menopause/andropause (yes) | 105 | 63.3 |
| Corticosteroid treatment (yes) | 16 | 9.6 |
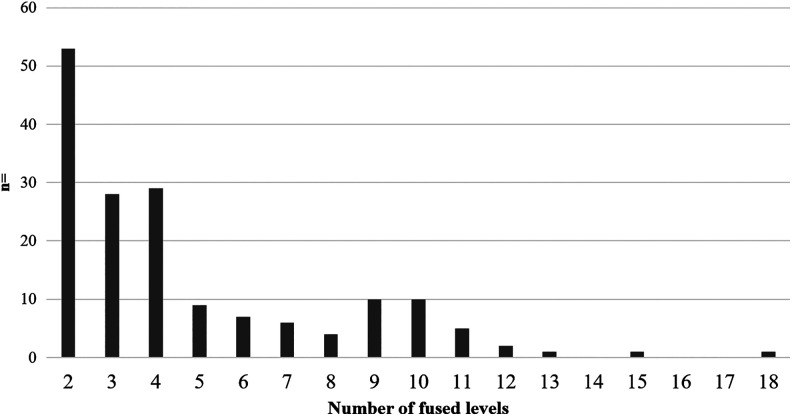
The surgical data showed a mean number of fused levels of 4.7 (2; 18), with 31.9% patients having a 2-level fusion, 39.8% fusion between 3 and 5 levels, and 28.3% fusion of more than 5 levels (Figure 1).
Figure 1.
Histogram showing the number of levels fused.
The prevalence of loosening was 9.6% (95% CI 5.6-15) when it was defined as implant pullout and 40.4% (95% CI 33-48) when defined as a radiolucent rim >1 mm.
The significant risk factors for loosening defined by pullout assessed radiologically were a thoracic localization (odds ratio [OR] 4.56), osteoporosis (OR 7.49), preoperative PI/LL mismatch (OR 1.04), the use of CrCo rods (OR 3.33), and preoperative frontal imbalance (OR 5.88) (Table 2).
Table 2.
Risk Factors for Pull-Out With Odds Ratios (ORs) and Confidence Interval Minimum and Maximum [CImin-CImax] and the Associated P Value.
| Pull-Out Univariable Regression | ||
|---|---|---|
| Variables | OR [CImin-CImax] | P |
| Age | 1.02 [0.97-1.07] | .420 |
| Pathology (scoliosis) | 2.95 [0.91-9.55] | .072 |
| Pathology (spondylolisthesis) | 1.94 [0.43-8.71] | .390 |
| Localization (thoracic) | 4.56 [1.58-13.17] | .005a |
| ASA (2) | 1.00 [0.32-3.10] | 1.000 |
| ASA (3) | 0.60 [0.06-5.55] | .650 |
| Menopause—hypogonadism | 4.54 [1.00-20.7] | .051 |
| Osteoporosis | 7.49 [1.64-34.09] | .009a |
| Titanium rods | 0.30 [0.11-0.87] | .026a |
| PI/LL mismatch (preoperative) | 1.04 [1.01-1.08] | .025a |
| Frontal balance (preoperative) | 0.17 [0.05-0.61] | .007a |
| Senior surgeon | 1.74 [0.47-6.42] | .400 |
| Number of levels fused (>5) | 1.14 [0.99-1.30] | .069 |
| Inferior level of instrumentation (thoracolumbar) | 0.44 [0.15-1.34] | .150 |
| All levels fused | 0.61 [0.12-3.00] | .540 |
| Circumferential arthrodesis | 0.40 [0.13-1.20] | .100 |
| Postoperative immobilization (brace) | 1.60 [0.56-4.56] | .380 |
Abbreviation: ASA, American Society of Anesthesiologists; PI, pelvic incidence; LL, lumbar lordosis.
aStatistically significant P values (P < .05).
The risk factors significantly associated with loosening defined by a rim >1 mm were age (OR 1.04), a fusion indication for scoliosis (OR 2.68), a thoracic localization (OR 3.29), ASA score 2 (OR 2.24) or 3 (OR 4.74), osteoporosis (OR 3.18), the use of CrCo rods (OR 2.33), a preoperative PI/LL mismatch (OR 1.05), preoperative frontal imbalance (OR 4.0), more than 5 levels fused (OR 1.21), sacrum or ilium as the inferior level of instrumentation (OR 2.70), the absence of circumferential arthrodesis (OR 2.08), and postoperative bracing (OR 2.86) (Table 3).
Table 3.
Risk Factors for Rim >1 mm Around Screws With Odds Ratios (ORs) and Confidence Interval Minimum and Maximum [CImin-CImax and the Associated P Values in Univariate Analysis and Multivariate Final Model.
| Univariable Regression | Multivariate Final Model | |||
|---|---|---|---|---|
| Variables | OR [CImin-CImax] | P | OR [CImin-CImax] | P |
| Age | 1.04 [1.01-1.07] | .005a | 1.03 [1.00-1.07] | 0.065* |
| Pathology (scoliosis) | 2.68 [1.32-5.45] | .006a | — | — |
| Pathology (spondylolisthesis) | 0.79 [0.31-2.00] | .610 | — | — |
| Localization (thoracic) | 3.29 [1.59-6.80] | .001a | — | — |
| ASA (2) | 2.24 [1.06-4.71] | .034a | — | — |
| ASA (3) | 4.74 [1.44-15.64] | .011a | — | — |
| Menopause—hypogonadism | 1.86 [0.96-3.62] | .067 | — | — |
| Osteoporosis | 3.18 [1.65-6.11] | .001a | 1.96 [0.91-4.22] | .085 |
| Titanium rods | 0.43 [0.21-0.86] | .0180a | — | — |
| PI/LL mismatch (preoperative) | 1.05 [1.02-1.08] | .001a | — | — |
| Frontal balance (preoperative) | 0.25 [0.13-0.48] | .00004a | 0.44 [0.21-0.93] | .032a |
| Senior surgeon | 2.08 [1.00-4.33] | .052 | — | — |
| Number of levels fused (>5) | 1.21 [1.09-1.35] | .0003a | — | — |
| All levels fused | 0.34 [0.11-1.07] | .066 | — | — |
| Circumferential arthrodesis | 0.48 [0.25-0.90] | .022a | 0.44 [0.21-0.91) | .027a |
| Postoperative immobilization (brace) | 2.86 [1.47-5.55] | .002a | 2.20 [0.99-4.87] | .053 |
| Inferior level of instrumentation (thoracolumbar) | 0.37 [0.19-0.70] | .002a | 0.45 [0.22-0.94] | .035a |
Abbreviation: ASA, American Society of Anesthesiologists; PI, pelvic incidence; LL, lumbar lordosis.
aStatistically significant P values (P < .05).
None of the other factors analyzed were statistically significant.
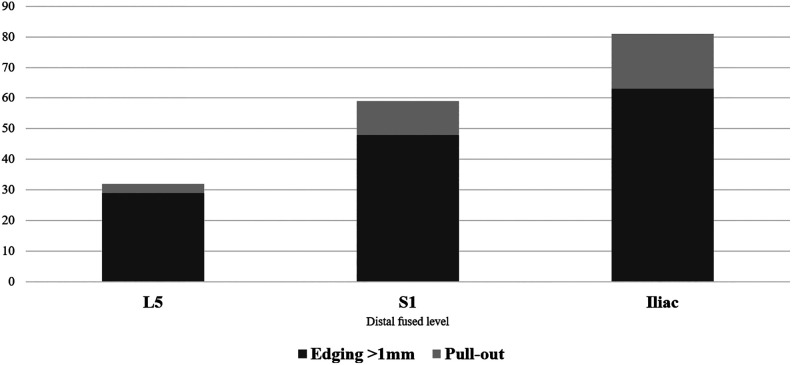
Investigating the incidence of loosening when pelvic joint fusion was performed, we found that the rate of loosening, regardless of its definition, was higher when the distal level involved the iliac spine rather than the sacrum (Figure 2).
Figure 2.
Rate of loosening for both definitions (rim >1 mm around at least 1 screw and screw pull-out) according to the distal level of the fusion.
Discussion
This study found that the incidence of screw loosening was more than 4 times higher when defined by a radiolucent rim >1 mm than by screw pull-out.
The risk factors in common for both definitions were osteoporosis, preoperative PI/LL mismatch, thoracic localizations and preoperative frontal imbalance. These risk factors were consistent with the literature. Among others, Scheyerer et al,20 using CT imaging, found osteoporosis and age to be significant risk factors for loosening in spine instrumentation.
The finding that CrCo rods are a risk factor for loosening suggests that failure by loosening is most likely in rigid constructions. Certainly, it has long been known that CrCo is more rigid than other materials.21 Similarly, the adjunction of an anterior support was associated with a decrease of loosening risk (OR 0.44 [0.21-0.91]; P = .027 in multivariate analysis), which may be explained by the improved fusion rates by anterior lumbar interbody fusion, compared with posterior arthrodesis only, that may more than compensate the stiffness of the construct.22,23 The key associated factor seems to be sagittal imbalance (PI/LL >10°), which was associated with a negative prognosis for implant anchorage in the bone under both definitions. The strong correlation of sagittal balance with postoperative patient satisfaction is further evidence of its importance.24
Among the other risk factors observed, the higher incidence of rims around the screws when the distal level of the fusion was the sacrum or the ileum, compared with L5 is consistent with other studies.25,26 On the other hand, the relative increased loosening when constructs stopped at the ilium in our study compared with the literature may be explained by the complexity of the cases requiring extension of distal fixation.25,26 Osteoporosis was strongly associated (OR 7.49 and 3.18 for pull-out and osteolysis, respectively) with loosening, as expected. The data was insufficient to allow us to assess the effect of osteoporotic treatment by dosage or duration.
The study’s principal limitation was its retrospective design, with the standard forms of potential bias it entails, including, among others, selection and recall bias. Moreover, the measurements were made on plain radiograms, and only a minority of patients had postoperative CT. We chose to assess loosening by either a rim >1 mm or a pulled-out screw, because these are the most commonly used criteria in the literature and enabled us to compare the series. Although it might have been interesting to test the method described by Benneker et al,27 the size of the cohort was sufficient to identify several clear risk factors and make progress in defining loosening in spine instrumentation.
In conclusion, loosening affected 1 in 10 patients when defined by screw pull-out, and more than 4 in 10 developed a radiolucent rim >1 mm around at least one screw. The risk factors that seemed most important were osteoporosis, sagittal imbalance (PI/LL >10°), and the use of CrCo rods. These findings underline the importance of preoperative screening of patients for risk factors. Indeed, osteoporosis treatment before surgery or the use of cemented screws should help prevent some loosening.28,29 Reducing the length of the fusion if possible and paying special attention to sagittal balance when instrumenting deformations should decrease the rate of screw loosening in posterior spinal fusions.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Laura Marie-Hardy, MD, MSc  https://orcid.org/0000-0001-5142-2658
https://orcid.org/0000-0001-5142-2658
References
- 1. Bydon M, Abt NB, De la Garza-Ramos R, et al. Impact of age on short-term outcomes after lumbar fusion: an analysis of 1395 patients stratified by decade cohorts. Neurosurgery. 2015;77:347–354. [DOI] [PubMed] [Google Scholar]
- 2. Smith JS, Shaffrey CI, Berven S, et al. Improvement of back pain with operative and nonoperative treatment in adults with scoliosis. Neurosurgery. 2009;65:86–94. [DOI] [PubMed] [Google Scholar]
- 3. Smith JS, Shaffrey CI, Berven S, et al. Operative versus nonoperative treatment of leg pain in adults with scoliosis: a retrospective review of a prospective multicenter database with two-year follow-up. Spine (Phila Pa 1976). 2009;34:1693–1698. [DOI] [PubMed] [Google Scholar]
- 4. Glassman SD, Carreon LY, Shaffrey CI, et al. The costs and benefits of nonoperative management for adult scoliosis. Spine (Phila Pa 1976). 2010;35:578–582. [DOI] [PubMed] [Google Scholar]
- 5. Bridwell KH, Glassman S, Horton W, et al. Does treatment (nonoperative and operative) improve the two-year quality of life in patients with adult symptomatic lumbar scoliosis: a prospective multicenter evidence-based medicine study. Spine (Phila Pa 1976). 2009;34:2171–2178. [DOI] [PubMed] [Google Scholar]
- 6. Cho KJ, Kim YT, Shin SH, Suk SI. Surgical treatment of adult degenerative scoliosis. Asian Spine J. 2014;8:371–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Andersen T, Bünger C, Søgaard R. Long-term health care utilisation and costs after spinal fusion in elderly patients. Eur Spine J. 2013;22:977–984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Social Security Administration. The 2001 annual report on the Board of Trustees of the Federal Old-Age and Survivors Insurance and Disability Insurance Trust Funds. https://www.ssa.gov/OACT/TR/TR01/tr01.pdf. Published March 19, 2001 Accessed July 9, 2019.
- 9. Fehlings MG, Tetreault L, Nater A, et al. The aging of the global population: the Changing epidemiology of disease and spinal disorders. Neurosurgery. 2015;77(suppl 4):S1–S5. [DOI] [PubMed] [Google Scholar]
- 10. Wittenberg RH, Shea M, Swartz DE, Lee KS, White AA, 3rd, Hayes WC. Importance of bone mineral density in instrumented spine fusions. Spine (Phila Pa 1976). 1991;16:647–652. [DOI] [PubMed] [Google Scholar]
- 11. Abul-Kasim K, Ohlin A. Evaluation of implant loosening following segmental pedicle screw fixation in adolescent idiopathic scoliosis: a 2-year follow-up with low-dose CT. Scoliosis. 2014;9:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Esses SI, Sachs BL, Dreyzin V. Complications associated with the technique of pedicle screw fixation. A selected survey of ABS members. Spine (Phila Pa 1976). 1993;18:2231–2239. [DOI] [PubMed] [Google Scholar]
- 13. McAfee PC, Weiland DJ, Carlow JJ. Survivorship analysis of pedicle spinal instrumentation. Spine (Phila Pa 1976). 1991;16(8 suppl):S422–S427. [PubMed] [Google Scholar]
- 14. Sandén B, Olerud C, Petrén-Mallmin M, Johansson C, Larsson S. The significance of radiolucent zones surrounding pedicle screws. Definition of screw loosening in spinal instrumentation. J Bone Joint Surg Br. 2004;86:457–461. [DOI] [PubMed] [Google Scholar]
- 15. Galbusera F, Volkheimer D, Reitmaier S, Berger-Roscher N, Kienle A, Wilke HJ. Pedicle screw loosening: a clinically relevant complication? Eur Spine J. 2015;24:1005–1016. [DOI] [PubMed] [Google Scholar]
- 16. Hicks GE, George SZ, Nevitt MA, Cauley JA, Vogt MT. Measurement of lumbar lordosis: inter-rater reliability, minimum detectable change and longitudinal variation. J Spinal Disord Tech. 2006;19:501–506. [DOI] [PubMed] [Google Scholar]
- 17. Singh M, Nagrath AR, Maini PS. Changes in trabecular pattern of the upper end of the femur as an index of osteoporosis. J Bone Joint Surg Am. 1970;52:457–467. [PubMed] [Google Scholar]
- 18. Legaye J, Duval-Beaupère G, Hecquet J, Marty C. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 1998;7:99–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Akaike H. A new look at the statistical model identification. IEEE Trans Autom Control. 1974;19:716–723. [Google Scholar]
- 20. Bredow J, Boese CK, Werner CM, et al. Predictive validity of preoperative CT scans and the risk of pedicle screw loosening in spinal surgery. Arch Orthop Trauma Surg. 2016;136:1063–1067. [DOI] [PubMed] [Google Scholar]
- 21. Lamerain M, Bachy M, Delpont M, Kabbaj R, Mary P, Vialle R. CrCo rods provide better frontal correction of adolescent idiopathic scoliosis treated by all-pedicle screw fixation. Eur Spine J. 2014;23:1190–1196. [DOI] [PubMed] [Google Scholar]
- 22. Flouzat-Lachaniette C-H, Ratte L, Poignard A, et al. Minimally invasive anterior lumbar interbody fusion for adult degenerative scoliosis with 1 or 2 dislocated levels. J Neurosurg Spine. 2015;23:739–746. [DOI] [PubMed] [Google Scholar]
- 23. Pateder DB, Kebaish KM, Cascio BM, Neubaeur P, Matusz DM, Kostuik JP. Posterior only versus combined anterior and posterior approaches to lumbar scoliosis in adults: a radiographic analysis. Spine (Phila Pa 1976). 2007;32:1551–1554. [DOI] [PubMed] [Google Scholar]
- 24. Yamada K, Abe Y, Yanagibashi Y, Hyakumachi T, Satoh S. Mid- and long-term clinical outcomes of corrective fusion surgery which did not achieve sufficient pelvic incidence minus lumbar lordosis value for adult spinal deformity. Scoliosis. 2015;10(suppl 2):S17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Yasuda T, Hasegawa T, Yamato Y, et al. Lumbosacral junctional failures after long spinal fusion for adult spinal deformity—which vertebra is the preferred distal instrumented vertebra? Spine Deform. 2016;4:378–384. [DOI] [PubMed] [Google Scholar]
- 26. Cho KJ, Suk SI, Park SR, et al. Risk factors of sagittal decompensation after long posterior instrumentation and fusion for degenerative lumbar scoliosis. Spine (Phila Pa 1976). 2010;35:1595–1601. [DOI] [PubMed] [Google Scholar]
- 27. Aghayev E, Zullig N, Diel P, Dietrich D, Benneker LM. Development and validation of a quantitative method to assess pedicle screw loosening in posterior spine instrumentation on plain radiographs. Eur Spine J. 2014;23:689–694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Tu CW, Huang KF, Hsu HT, Li HY, Yang SS, Chen YC. Zoledronic acid infusion for lumbar interbody fusion in osteoporosis. J Surg Res. 2014;192:112–116. [DOI] [PubMed] [Google Scholar]
- 29. Pesenti S, Blondel B, Peltier E, Adetchessi T, Dufour H, Fuentes S. Percutaneous cement-augmented screws fixation in the fractures of the aging spine: is it the solution? Biomed Res Int. 2014;2014:610675. [DOI] [PMC free article] [PubMed] [Google Scholar]