Abstract
Objectives
The objective of the study was to assess if patients with epilepsy (PWE) experienced an increase in seizure frequency and self-reported stress during the COVID-19 pandemic.
Methods
This is a cross-sectional study conducted in Saudi Arabia in April 2020. An electronic self-administered questionnaire was distributed to PWE via their treating neurologist. The variables included were demographic and baseline clinical characteristics (age, gender, living situation, occupational status, type of epilepsy, duration of epilepsy, number of antiepileptic medications (AEDs), presence of known psychiatric illness, and use of psychiatric medications), their seizure control in the month prior to the pandemic, perceived stress during this period of time, sleep changes, compliance changes, and change in seizure control during the pandemic.
Results
A total of 156 patients completed the questionnaire, with 29.5% reporting an increase in seizure frequency. Additionally, 59.4% reported an increase in self-reported stress and 71.2% experienced a significant change in their sleep during this period. Higher baseline seizure frequency, more AEDs, noncompliance, increase in self-reported stress, and sleep changes are the significant factors associated with increase in seizure frequency during the pandemic.
Conclusion
Identifying high-risk patients for seizure recurrence is important in order to provide them with adequate support to reduce such risk.
Keywords: Epilepsy, Seizure recurrence, COVID-19, Self-reported stress, Pandemic
Highlights
-
•
Poorly controlled epilepsy at baseline, more AEDs at baseline, medication non-compliance, increase in self-reported stress and altered sleep patterns are risk factors for increase in seizure frequency during the pandemic
-
•
Students, duration of epilepsy less than 5 years, history of psychiatric illness and use of psychiatric medications are risk factors for increase self-reported stress in PWE
1. Introduction
Epilepsy is one of the most common chronic neurological diseases, characterized by recurrent episodes of unprovoked seizure. Patients with epilepsy (PWE) are at risk of recurrent seizures despite medical therapy and intervention. Seizures can be triggered by both physical and psychological factors, including missing antiepileptic medication (AED) (40.9%), emotional stress (31.3%), sleep deprivation (19.7%), fatigue (15.3%), missing meals (9.1%), fever (6.4%), and smoking (6.4%) [1].
Stress plays a strong role in the recurrence of epileptic attacks. A study conducted on patients with focal epilepsy found that 5 out of 1000 patients experienced seizures in relation to significant life events [2]. Another study looking at risk of seizure recurrence in patients with single unprovoked seizure and in newly diagnosed epilepsy found that markers of stress (i.e., low collective efficacy, lifetime mood disorder, and lifetime generalized anxiety disorder) were associated with an increased risk of seizure recurrence in those patients [3]. Stress, whether acute or chronic, is a common reported trigger for seizure recurrence [4].
In December 2019, a novel coronavirus was reported in Wuhan, China [5]. Subsequently, the virus was identified and named COVID-19 in January 2020, before being declared as a global pandemic by the World Health Organization on March 11, 2020. Globally significant protective measures have been taken to help reduce the spread of infection, and Saudi Arabia is no exception. The first case of COVID-19 was diagnosed in the country on March 2, and since then, the number of new cases has increased. Protective measures taken by the country include the suspension of school, work, and travel, and on March 23, a partial curfew commenced. Subsequently, various degrees of curfew were taken in different cities depending on the extent of disease spread. With all of these measures in place, healthcare support to patients with preexisting chronic diseases, including PWE, might be affected. Most hospitals moved to telemedicine in order to reduce clinic attendance and thus mitigate patient exposure to COVID-19.
Patients have also been advised to avoid emergency room visits unless for life-threatening conditions. Different concerns regarding epilepsy and COVID-19 have been raised, yet current evidence suggests that PWE are not more likely to become infected with the virus and nor are they at higher risk of complications [6,7]. The concern, however, is that seizures may result in emergency room or clinical visits, and so better control of seizures is required. Further, identification of high-risk PWEs is helpful to provide adequate support for them. The aim of this study was to assess if PWE experienced an increase in their seizure frequency and self-reported stress during this period of the pandemic.
2. Methods
2.1. Study design and population
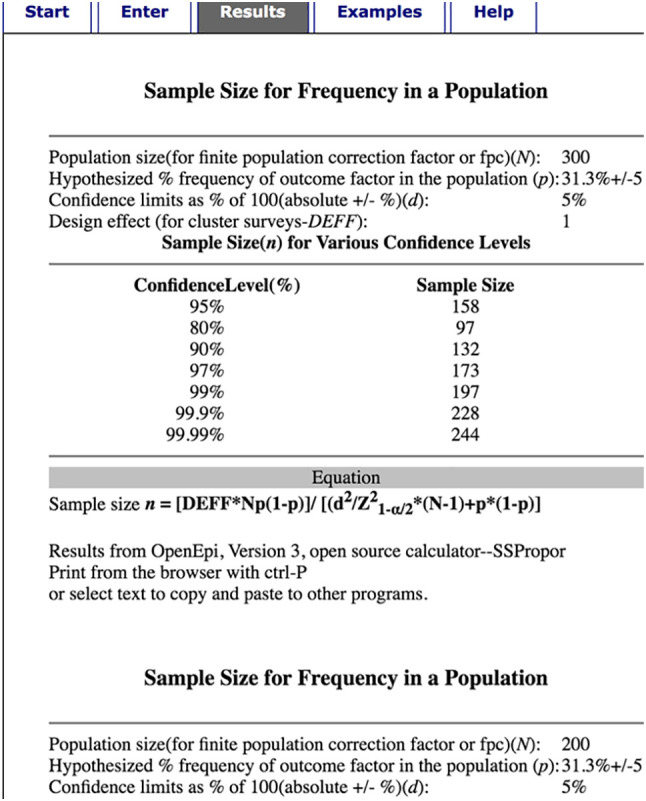
Focused on PWE in Saudi Arabia, this current study is a cross-sectional questionnaire-based research project. An electronic self-administered questionnaire with a cover letter explaining the purpose of the study was written in English then translated into Arabic, before being back translated to English to check for discrepancies. The questionnaire was also reviewed by two independent physicians and pretested on 10 PWE for validation. The questionnaire was distributed later to treating neurologists in different Saudi Arabian institutes. Finally, it was redistributed electronically to patients through the treating physician in the month of April 2020. Complete forms were included, and all incompletely filled forms were rejected. The sampling technique was nonprobability convenient sampling, and the sample size calculated was 158 based on exposure-induced epilepsy as 31.3%. We calculated sample sizes for various characteristics and finally chose the maximum sample size to accommodate all comparisons. For the variables where cell had expected value less than 5 while applying test of significance, we dropped from the result and were not included in final report. The p value chosen was for the likelihood ratio and does not require any change. The level of significance was 5%, and there was a 95% confidence interval. The expected number of patients was around 300 (please see Appendix A).
2.2. Data collection
The variables included were demographic and baseline clinical characteristics, such as age, gender, living situation, occupational status, type of epilepsy, duration of epilepsy, number of AEDs, presence of known psychiatric illness, and use of psychiatric medications. Further assessed was PWE's seizure control in the month prior to the pandemic, along with perceived stress during this period of time, sleep changes, compliance changes, and change in seizure control after the pandemic. The data were collected and recorded on an Excel sheet, and for each response, the frequency and percentage were calculated.
2.3. Data analysis
Data collected were converted to SPSS format and presented as mean ± standard deviation (SD). Statistical significance was established using analysis of variance (ANOVA) with the help of statistical software SPSS, v25 (IBM, USA), with the level of significance defined as p < 0.05.
2.4. Ethical considerations
Ethical approval was obtained from Umm Al-Qura University's ethics and research committee, and consent was acquired from all participants via an electronic self-administered questionnaire with a cover letter explaining the purpose of the study, written in Arabic.
3. Results
3.1. Demographic and patient characteristics
All 156 patients' responded to the questionnaire, completing it fully, and thus none were excluded from the study. Table 1 shows the demographic and baseline characteristics for the responders. Sixty-two percent of our responders were female patients, 99% were living with family, 38% had generalized seizures, 47% were on single medications, and 48.1% had been seizure-free for the past three months prior to the start of the pandemic. Most of the patients (93.6%) complied with their treatment plan, while 40% had one of the following comorbid psychiatric diseases: anxiety (15.4%), depression (7.1%), and obsessive or mixed disorders (16.5%). However, only 23.1% were receiving medical therapy.
Table 1.
Demographic data and baseline clinical characteristics.
| Characteristics | Categories | Gender |
Total | Likelihood ratio | p-Value | |
|---|---|---|---|---|---|---|
| Female | Male | |||||
| Age | Less than 20 | 18 | 5 | 23(14.7%) | 6.450 | 0.092 |
| 20–40 | 66 | 38 | 104(66.7%) | |||
| 40–60 | 11 | 13 | 24(15.4%) | |||
| More than 60 | 2 | 3 | 5(3.2%) | |||
| Living situation | Live alone | 0 | 2 | 2(1.3%) | 3.932 | 0.047 |
| Live with family | 97 | 57 | 154(98.7%) | |||
| Employment status | Employed | 16 | 29 | 45(28.8%) | 19.028 | 0.000 |
| Student | 31 | 13 | 44(28%) | |||
| Unemployed | 50 | 17 | 67(43%) | |||
| Duration of epilepsy | Less than 5 years | 22 | 17 | 39(25%) | 5.016 | 0.0810 |
| 5–10 years | 34 | 11 | 45(28.8%) | |||
| More than 10 years | 41 | 31 | 72(46%) | |||
| Type of epilepsy | Generalized | 37 | 22 | 59(37.8%) | 0.382 | 0.826 |
| Focal | 33 | 18 | 51(32.7%) | |||
| Focal with secondary generalization | 27 | 19 | 46(29.5%) | |||
| Number of medications | One | 51 | 23 | 74(47.4%) | 5.927 | 0.052 |
| Two | 27 | 14 | 41(26.3%) | |||
| More than two | 19 | 22 | 41(26.3%) | |||
| Seizure frequency (per month) | Less than one | 43 | 32 | 75(48%) | 2.238 | 0.525 |
| One | 7 | 2 | 9(5.8%) | |||
| Two | 27 | 13 | 40(25.6%) | |||
| More than two | 20 | 12 | 32(20.5%) | |||
| Medication compliance | Yes | 89 | 57 | 146(93.5%) | 1.576 | 0.209 |
| No | 8 | 2 | 10(6.4%) | |||
| Known psychiatric diagnosis | Yes | 43 | 19 | 62(39.8%) | 2.280 | 0.131 |
| No | 54 | 40 | 94(60%) | |||
| Use of psychiatric medications | Yes | 24 | 12 | 36(23%) | 0.406 | 0.524 |
| No | 73 | 47 | 120(77%) | |||
| Number of psychiatric medications | One | 18 | 6 | 24(15.4%) | 7.785 | 0.051 |
| Two | 6 | 3 | 9(5.8%) | |||
| More than two | 0 | 3 | 3(1.9%) | |||
3.2. Effect of the pandemic on PWE
Table 2 shows the effect of the pandemic on PWE. In this study, 29.5% of the patients experienced an increase in their seizure frequency as a result of COVID-19, although the majority of these PWE had < 50% increase in frequency. Compliance to medication was not affected by the situation in 94% of the patients.
Table 2.
Effect of pandemic on PWE.
| Increase in seizure frequency | |
| Yes | 46 (29.5%) |
| No | 110 (70.5%) |
| < 50% increase | 32 (20.5%) |
| > 50% increase | 14 (9%) |
| Change medication compliance | |
| Yes | 8 (5.1%) |
| No | 148 (94.9%) |
| Increase in self-reported stress | |
| Yes | 85 (54.4%) |
| No | 71 (45.5%) |
| Causes of increase in self-reported stress | |
| Afraid from getting infection | 30 (19.2%) |
| Social reasons | 44 (28.2%) |
| Financial reasons | 11 (7.05%) |
| Change in sleep patterns | |
| Yes | 111 (71.2%) |
| No | 45 (28.8%) |
| Sleep pattern changes | |
| Intermittent sleep | 1 (0.6%) |
| Reverse sleep pattern | 91 (58%) |
| Sleep less than usual | 4 (2.6%) |
| Sleep more than usual | 15 (9.6%) |
A total of 59.4% of patients reported an increase in self-reported stress during this period, while the majority of patients (71.2%) experienced a significant change in their sleep.
3.3. Factors associated with increase in self-reported stress
Table 3 shows the relation of increase in self-reported stress and demographic/clinical characteristics. In patients who had an increase in self-reported stress, occupational status was significantly related to this development. Students reported a significant difference (with a likelihood ratio of 6.48 and p-value less than 0.039). Patients with less than five years duration of epilepsy significantly had an increase in their stress (with a likelihood ratio of 6.65 and p-value less than 0.036). Patients with a psychiatric disease (with a likelihood ratio of 12.5 and p-value less than 0.000) and on medication for this illness (with a likelihood ratio of 4.33 and p-value less than 0.037) had a significant increase in their self-reported stress.
Table 3.
Effect of pandemic on self-reported stress in relation to demographic and baseline characteristic.
| Characteristic | Categories | Increase in self-reported stress |
Test of significance Likely hood ratio |
p-Value | |
|---|---|---|---|---|---|
| No | Yes | ||||
| Age | < 20 years | 6 | 17 | 7.5 | 0.053 |
| 20–40 | 52 | 52 | |||
| 40–60 | 9 | 15 | |||
| > 60 | 4 | 17 | |||
| Male | Male | 29 | 30 | 0.506 | 0.477 |
| Female | 42 | 55 | |||
| Occupational status | Students | 13 | 31 | 6.483 | 0.039 |
| Employed | 23 | 22 | |||
| Nonemployed | 35 | 23 | |||
| Living situation | Alone | 0 | 2 | 2.451 | 0.117 |
| With family | 71 | 83 | |||
| Duration of epilepsy | < 5 years | 11 | 28 | 6.651 | 0.036 |
| 5–10 years | 22 | 23 | |||
| > 10 years | 38 | 34 | |||
| Type of epilepsy | Generalized | 28 | 31 | 3.4 | 0.183 |
| Focal | 27 | 24 | |||
| Focal with generalization | 16 | 30 | |||
| Number of AED | 1 | 31 | 43 | 0.754 | 0.689 |
| 2 | 20 | 21 | |||
| > 2 | 20 | 21 | |||
| Seizure frequency (per month) | Less than one | 41 | 34 | 6.342 | 0.096 |
| 1 | 5 | 4 | |||
| 2 | 14 | 26 | |||
| More than 2 | 11 | 21 | |||
| Known psychiatric diagnosis | Yes | 40 | 45 | 12.5 | 0.000 |
| No | 50 | 18 | |||
| Use of psychiatric medications | Yes | 60 | 25 | 4.333 | 0.037 |
| No | 60 | 11 | |||
| Number of psychiatric medications | 1 | 8 | 16 | 4.742 | 0.192 |
| 1–2 | 2 | 7 | |||
| > 2 | 1 | 2 | |||
3.4. Factors associated with increase in seizure frequency
Table 4, Table 5 show the relation between increase in seizure frequency and different demographic/clinical characteristics. Patients who were taking more drugs (with a likelihood ratio of 7.28 and p-value less than 0.026) and those with more seizures at baseline experienced significant worsening of seizure frequency during the pandemic (with a likelihood ratio of 18.73 and p-value less than 0.000). Also, we found noncompliance to medication to be another cause of the increase in seizure frequency (with a likelihood ratio of 11.79 and p-value less than 0.001). Change in sleep (with a likelihood ratio of 4.42 and p-value less than 0.035) and increase in self-reported stress (with a likelihood ratio of 18.82 and p-value less than 0.000) were also significantly associated with increase in seizure frequency.
Table 4.
Seizure control in relation to demographic and baseline characteristic during the COVID pandemic.
| Characteristic | Categories | The effect of curfew on seizure |
Test of significance Likely hood ratio |
p-Value | |
|---|---|---|---|---|---|
| Seizure is not affected | Increase in seizure | ||||
| Age | < 20 years | 14 | 9 | 3.854 | 0.278 |
| 20–40 | 78 | 26 | |||
| 40–60 | 14 | 10 | |||
| > 60 | 4 | 1 | |||
| Gender | Male | 43 | 16 | 0.2580 | 0.612 |
| Female | 67 | 30 | |||
| Occupational status | Students | 32 | 12 | 4.094 | 0.129 |
| Employed | 36 | 9 | |||
| Nonemployed | 42 | 25 | |||
| Living situation | Alone | 2 | 0 | 1.408 | 0.235 |
| With family | 108 | 46 | |||
| Duration of epilepsy | < 5 years | 25 | 15 | 4.515 | 0.105 |
| 5–10 years | 37 | 8 | |||
| > 10 years | 48 | 24 | |||
| Type of epilepsy | Generalized | 40 | 19 | 5.954 | 0.051 |
| Focal | 42 | 9 | |||
| Focal with generalization | 28 | 18 | |||
| Number of AED | 1 | 57 | 17 | 7.277 | 0.026 |
| 2 | 31 | 10 | |||
| > 2 | 22 | 19 | |||
| Seizure frequency (per month) | Less than one | 59 | 16 | 18.734 | 0.00 |
| 1 | 9 | 0 | |||
| 2 | 28 | 12 | |||
| More than 2 | 14 | 18 | |||
| Medication compliance after curfew | Compliant | 108 | 38 | 11.79 | 0.001 |
| Noncompliant | 2 | 8 | |||
Table 5.
Effect of self-reported stress and sleep changes on seizure control.
| Seizure is not affected | Increase in seizure | Likelihood ratio p-Value |
p-Value | |
|---|---|---|---|---|
| Change in sleep | ||||
| Yes | 73 | 38 | 4.442 | 0.035 |
| No | 37 | 8 | ||
| Self-reported stress | ||||
| Increased | 48 | 37 | 18.821 | 0.000 |
| Not affected | 62 | 9 |
4. Discussion
Because in part of the risk to public health, pandemics lead to significant increases in stress. This impacts not only the affected patients and their families but also the general population [[8], [9], [10]]. In the case of COVID-19, several causes contribute to this, including the high infectivity of the virus and its rapid spread, along with extensive media coverage on the pandemic. Most countries adopted strict preventive measures to decrease the spread of the virus, all of which increased social isolation of individuals and had a significant financial and economic impact at both the personal and global level. In a review of studies looking at psychological stress among individuals during the early COVID-19 pandemic, it was found that anxiety and depression (16–28%) and self-reported stress (8%) are common and may be associated with disturbed sleep [8].
Patients with epilepsy are a vulnerable group, and our study found that 54.4% of participants reported an increase in their stress as a result of the pandemic. We found that students were more stressed than other patients, in part due to the suspension of school during the critical pre-exam period, the transition to remote learning (a new experience for the majority of students and staff), and the uncertainty surrounding examinations. Other factors reported by patients experiencing heightened stress include social reasons (28.2%), fear of infection (19.2%), and financial reasons (7.05%). Social issues mainly involve curfew-related isolation and the inability to visit family members and friends, while financial problems generally refer to the global economic crisis.
Another significant contribution to self-reported stress was found to be epilepsy duration. People with more recent onset of diagnosis (less than five years) were also at higher risk of increase in self-reported stress. Further, patients with a preexisting diagnosis of psychiatric illness were more likely to report an increase in self-reported stress, as well as those who were taking psychiatric medications. A study by Hao et al. shows that 13% of the observed PWE had severe psychological stress, compared with 2% in the matched control group. This suggests that PWE are at higher risk of mental diseases. Hao and colleagues reported that patients with drug-resistant epilepsy and the heighted media exposure were significantly related to increases in psychological stress [11]. In our study, we observed no significant relation of increase in self-reported stress to the number of AEDs and baseline seizure frequencies. However, we did not look at the relationship between self-reported stress and the time spent watching the news.
In our study, we found seizures increased in frequency during the month of the pandemic and curfew in Saudi Arabia. Patients with more severe epilepsy (manifested by higher baseline seizure rate and more AED) were more likely to experience increased seizure frequency regardless of their level of stress. Noncompliance to medications is a well-known trigger of seizure recurrence, and some patients were noncompliant for no specific reason (e.g., unrelated to drug availability, as no patients reported difficulties in obtaining drugs). Although there were curfews throughout Saudi Arabia, most hospitals adopted a system of medication delivery to patients' homes. Thus, patients with chronic illness were able to access their medications without visiting hospitals. Patients who were noncompliant to medication before the pandemic continued to have problems with compliance later.
Another major finding in our study was the change in sleep pattern in most of the patients. The most frequent change in sleep was a reversal of the sleep pattern in 58% of the respondents (sleep after sunrise), followed by more sleep than usual in 9.6%, less sleep in 2.6%, and intermittent sleep in 0.6%. Good sleep hygiene is recommended to all PWE, as strict compliance results in a reduction of seizure frequency. During this period, the majority of works were suspended and moved into the virtual mode. Patients and their families were staying at home with no routine daily activities, which most likely affected their sleep patterns, as reported by the patients. Even unemployed patients (43%) affected by cessation of work as the majority of our patients are living with their families. Their sleep is affected by the change in whole family routine. It is not uncommon in our society to reverse sleep patterns during holidays. During summer time, the majority of people will sleep after sunrise. Most of the activities will start at night giving the extreme heat during the daytime. Those with such changes experienced significant increases in their seizure frequency. Change in sleep–wake rhythm and sleep quality has also been described in an Italian cross-sectional study of the lockdown period [12]. The Task Force of the European CBT-I Academy published various recommended measures for different groups of people (e.g., women, children, and healthcare providers) to maintain good sleep hygiene [13]. Avoidance of sedatives in favor of a behavioral approach is recommended. Patient with epilepsy are a specific group whose quality of life is highly affected by sleep disturbance due to the impact this has on seizure frequency, and so vigilance is necessary to reduce increased instances.
Stress is one of the major contributors to the failure of epilepsy control. An increase in self-reported stress among our responders was also significantly related to the increase in their seizure frequencies. It is vital to identify patients who are more vulnerable to worsening seizure control during this period of time. Although there is a global trend to decrease protective measures, the pandemic is not yet over. Further, stress levels are likely to persist in view of economic prognostications. A consensus statement published on April 23, 2020 recommended that PWE adhere to adequate sleep routines where possible, engage in regular exercise and healthy eating where appropriate, and avoid alcohol and recreational drugs [6]. It is necessary for epilepsy clinics and foundations to stress the importance of medication compliance, adherence to good sleep, hygiene, and providing psychological support to the patients. Such measures may reduce the chance of worsening seizures for PWE and limit the risk of them requiring hospital or clinical treatment during the COVID-19 pandemic.
5. Limitation
We did not assess whether stress was related to living in communities with patients with infection or with a high rate of positive cases.
6. Conclusion
Patients with poorly controlled epilepsy, noncompliance to medications, altered sleep pattern, and an increase in self-reported stress are more susceptible to increased seizure frequency during the pandemic. Education of the importance of all risk factors is vital in order to keep PWE seizure-free.
Declaration of competing interest
All authors disclose no conflict of interest related to this study.
Acknowledgments
We thank all of the neurologists who contributed to this study by recruiting their patients.
Appendix A.
References
- 1.Balamurugan E., Aggarwal M., Lamba A., Dang N., Tripathi M. Perceived trigger factors of seizures in persons with epilepsy. Seizure. 2013;22(9):743–747. doi: 10.1016/j.seizure.2013.05.018. [DOI] [PubMed] [Google Scholar]
- 2.Gelisse P., Genton P., Coubes P., Tang N.P., Crespel A. Can emotional stress trigger the onset of epilepsy? Epilepsy Behav. 2015;48:15–20. doi: 10.1016/j.yebeh.2015.05.010. [DOI] [PubMed] [Google Scholar]
- 3.Baldin E., Hauser W.A., Pack A., Hesdorffer D.C. Stress is associated with an increased risk of recurrent seizures in adults. Epilepsia. 2017;58(6):1037–1046. doi: 10.1111/epi.13741. [DOI] [PubMed] [Google Scholar]
- 4.Privitera M., Walters M., Lee I., Polak E., Fleck A., Schwieterman D. Characteristics of people with self-reported stress-precipitated seizures. Epilepsy Behav. 2014;41:74–77. doi: 10.1016/j.yebeh.2014.09.028. [DOI] [PubMed] [Google Scholar]
- 5.Guan W.J., Ni Z.Y., Hu Y., Liang W.H., Ou C.Q., He J.X. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.French J.A., Brodie M.J., Caraballo R., Devinsky O., Ding D., Jehi L. Keeping people with epilepsy safe during the Covid-19 pandemic. Neurology. 2020;94(23):1032–1037. doi: 10.1212/WNL.0000000000009632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kuroda N. Epilepsy and COVID-19: associations and important considerations. Epilepsy Behav. 2020;108:107122. doi: 10.1016/j.yebeh.2020.107122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rajkumar R.P. COVID-19 and mental health: a review of the existing literature. Asian J Psychiatr. 2020;52:102066. doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tian F., Li H., Tian S., Yang J., Shao J., Tian C. Psychological symptoms of ordinary Chinese citizens based on SCL-90 during the level I emergency response to COVID-19. Psychiatry Res. 2020;288:112992. doi: 10.1016/j.psychres.2020.112992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang Y., Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 2020;288:112954. doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hao X., Zhou D., Li Z., Zeng G., Hao N., Li E. Severe psychological distress among patients with epilepsy during the COVID-19 outbreak in southwest China. Epilepsia. 2020;61(6):1166–1173. doi: 10.1111/epi.16544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cellini N., Canale N., Mioni G., Costa S. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J Sleep Res. 2020:e13074. doi: 10.1111/jsr.13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Altena E., Baglioni C., Espie C.A., Ellis J., Gavriloff D., Holzinger B. Dealing with sleep problems during home confinement due to the COVID-19 outbreak: practical recommendations from a task force of the European CBT-I Academy. J Sleep Res. 2020:e1. doi: 10.1111/jsr.13052. [DOI] [PubMed] [Google Scholar]


