The role of chest computed tomography (CT) in COVID-19 remains to be defined. Chest CT was applied early and locally in the outbreak in China and, at the peak of the COVID-19 outbreak, was used alongside of reverse transcription polymerase chain reaction (RT-PCR) testing, to diagnose patients upon acute presentation to fever clinics in and around Wuhan in Hubei Province, China (1). It has recently become clear that one of the main challenges of COVID-19 containment is the prevalence of patients who are asymptomatic, but are infectious and transmitting the virus (2). The rapid transmission of SARS-CoV-2 is partly because peak viral shedding occurs near the onset of symptoms, which means patients are unknowingly infectious well before clinical presentation (3). This is compounded by the fact that most patients with SARS-CoV-2, and therefore many people who transmit the virus have mild or no symptoms at all. A broad population testing program to limit the spread of the virus could consider the use of chest CT in addition to RT-PCR. Chest CT has been demonstrated to be even more sensitive than RT-PCR (4, 5), but has not been widely used for early COVID-19 detection in the United States and Europe. Limited availability of diagnostic methods for COVID-19 infection are a contributing factor to delayed diagnosis or incomplete information about prevalence. Delays in definitive diagnosis likely translate to incomplete isolation, due to reduced patient compliance with strict isolation slowing the mitigation process.
In some parts of China with high prevalence, COVID-19 was diagnosed despite RT-PCR negativity, with a positive CT plus high-risk travel or exposure history (6). Furthermore, in a study of 1040 patients, CT was shown to be more sensitive than PCR in their acute epidemic setting (4). Sensitivity of CT would go down in the absence of a severe epidemic with high prevalence, and likewise specificity of CT would go down in the presence of other viruses, such as influenza. However, the acceptance of positive exposure and CT-defined diagnosis may have captured a larger portion of the early COVID-19 population, than RT-PCR alone. In Hubei Province, such CT-positive patients were immediately isolated, which may have contributed in part to successful containment and relatively less mortality than in other parts of the world. In US and Europe, CT has been used less frequently and typically only in the progression of the disease and its complications. Some US guidelines have recommended against using CT as a “screening” tool (7). These patterns of diagnosis should be carefully studied for associations between CT use, early detection rates, transmission rates, prevalence, and outcomes.
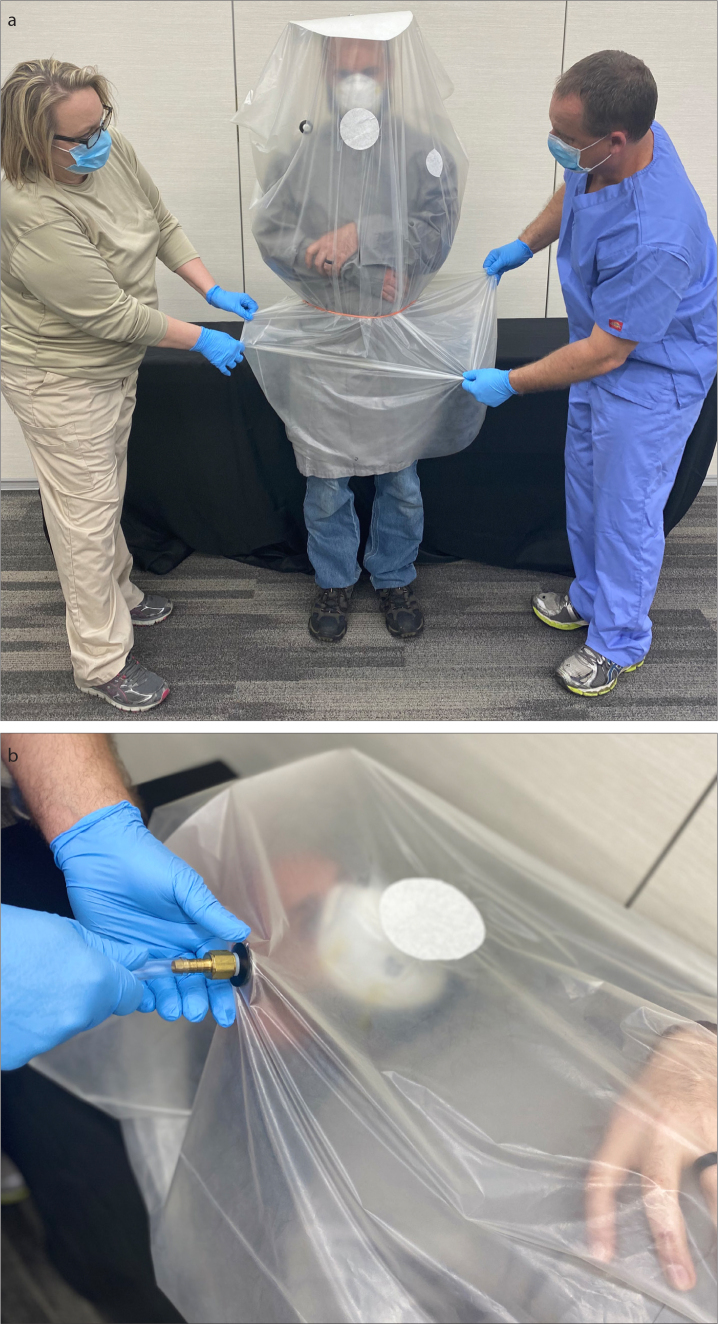
CT currently requires 30–60 minutes turnover time after the image acquisition for decontamination and passive air exchange between patients (8). This results in many fewer patients per hour than in normal operations. The issue of passive air exchange time in between CT exams is critical for effective use of CT early in presentation or as a screening tool for PCR test negative individuals with persistent suspicion of COVID-19. The decontamination time can be potentially reduced or dismissed with use of custom enhanced containment devices. During the Chinese outbreak, in addition to an N-95 mask, a large air-tight protective plastic bag was placed temporarily over the patient’s head with tape around the waist in order to reduce the aerosolization of SARS-CoV-2 from infectious patients (Figs. 1, 2) (9). Such an approach could reduce room turnover time significantly without having to wait for 30–60 minutes of ventilation or ultraviolet sterilization. This could not only enable CT efficiency, but also could make utilization of targeted CT for COVID-19 screening more cost-effective.
Figure 1.
CT contamination reduction equipment placed outside the N-95 mask to reduce the room turnover time. Reproduced with permission from reference 9.
Figure 2. a, b.
Upright (a) and supine (b) depictions show prototype patient isolation drape/bag device with elastic waistband being donned by 2 staff (a), and oxygen intake nipple for oxygen and integrated exit filter (N-95/FFP2 grade). The flat “hat” top maintains the bag material away from the face while upright (a) or supine (b). The patient wears an N-95 or FFP2 to further reduce air and surface exposures in CT, and to minimize the risk of airway obstruction from bag. Photo courtesy Civco Medical Solutions Inc., Coralville, Iowa, USA and NIH Center for Interventional Oncology, Bethesda, MD.
The additional relative cost of CT in this setting could go down by using a protective bag device, where 3–8 patients might theoretically be scanned per hour, instead of less than one with the current passive ventilation decontamination recommendations. In an outbreak hotspot, the total healthcare cost of targeted early CT use is certainly less, by orders of magnitude, than not using CT. Although the exact impact of testing with both CT and RT-PCR is speculative, early diagnosis across an outbreak is fundamental to containment. Ignoring early use of CT could send undiagnosed COVID-19 pneumonia patients home or out into the community to further spread the virus. Not all of these patients may be symptomatic enough to self-quarantine strictly. Although PCR sensitivity has likely improved since the referenced study, let’s assume a 98% sensitivity for CT and 71% sensitivity for PCR in an acute setting (4). In this case, 27% more patients with early COVID-19 pneumonia would potentially be diagnosed with CT. Thus, CT would miss 2/100 patients while PCR would miss 29/100 patients. Therefore, 27 of 100 patients would be misled by a false-negative PCR during the serial interval, which is when contact tracing occurs. Assuming a 35% noncompliance rate for strict isolation behaviors (10), 9 of 27 patients would further spread the virus unknowingly. Assuming a reproduction number of 2.2 (transmission rate per person), approximately 20 additional infections would quickly expand in number. These 20 newly infected patients will go on to infect 44 others after another 4 days, and so on. Finally, these undiagnosed COVID-19 pneumonia cases could benefit from earlier care and monitoring, especially if and when an early therapy proves helpful.
In this example, the additional cost of targeted CT for tracing would be far outweighed by the cost of not isolating new infections and the subsequent generations of infections. Any tool that can diagnose asymptomatic people who are shedding SARS-CoV-2 viral particles should be strongly considered, given the downstream global economic impact of ineffective mitigation methods. CT does not have to be broadly applied to a population to be an effective tool. There are approximately 15 000 CT scanners in the USA and nearly 100 million CT scans are performed per year. Utilization is low at present. Targeted CT may augment current tracing and prevalence gathering efforts. Any use of CT comes with added risks of exposures by bringing infected people together with non-infected people, so strict isolation is key, with dedicated access routes defined. Chest x-ray remains more widely available, and the role of imaging may depend upon local practices, resources, and access (11).
With the current disinfection recommendations, CT with a mandatory 1-hour disinfection interval in between patients might not be fiscally viable nor efficient. However, with custom bags and aggressive CT use with expedited throughput, chest CT in the pre-symptomatic and early onset COVID-19 patients might ultimately prove both ethical and cost-effective. Over 85% of COVID-19 infections went undocumented early on in China prior to implementation of aggressive CT and PCR testing (12). More use of CT early in the disease might decompress testing bottlenecks due to staffing or supplies. “Stay at home” orders may also make CT more accessible. Additionally, characterization of viral shedding dynamics and identification of asymptomatic patients through CT scans could provide increased prevalence data for modeling pandemic mitigation, reopening or exit strategies. Clinical trials with CT correlates may arrive at useful drugs sooner, and early diagnosis with CT may lead to better outcomes for any anti-viral drugs that might shorten the disease course when given early (like influenza antivirals). CT may also classify the ventilated critical patient into two distinct phenotypes of physiology and outcomes, which merits further examination (13). One recent experience in high prevalence northern Italy reported the benefits of CT over chest x-ray, in terms of more confidently ruling out and ruling in COVID-19 (14). No consensus exists on the integrated use of chest x-ray or CT for assessment, triage or management of symptomatic or asymptomatic patients suspected to have COVID-19 pneumonia, although practices vary widely by location and resources (11, 15).
In light of these insights, professional societies, advocacy groups, epidemiologists, and public health experts might consider CT as part of an early diagnostic array of testing tools when formulating or revising recommendations. The exact role of CT remains unclearly defined and may depend upon prevalence. Further research may prove targeted CT to be a cost-effective epidemiological tool that could play an important role in more effective containment or mitigation of COVID-19 outbreaks or triage of the critical patient.
Acknowledgements
Funded in part by the National Cancer Institute, National Institutes of Health, under Contract No. HHSN261200800001E. The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. Government.
Footnotes
Conflict of interest disclosure
The authors declared no conflicts of interest.
References
- 1.Liang T. Handbook of COVID-19 prevention and treatment: the First Affiliated Hospital, Zhejiang University School of Medicine. Available at: https://www.alibabacloud.com/universal-service/pdf_reader?spm=a3c0i141383008102420620dreadnow6df3647fp3w1Sj&cdnorigin=video-intl&pdf=Read%20Online-Handbook%20of%20COVID-19%20Prevention%20and%20Treatmentpdf.
- 2.Inui S, Fujikawa A, Jitsu M, et al. Chest CT findings in cases from the cruise ship “Diamond Princess” with coronavirus disease 2019 (COVID-19) Radiol Cardiothorac Imaging. 2020;2:e200110. doi: 10.1148/ryct.2020200110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zou L, Ruan F, Huang M, et al. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020;382:1177–1179. doi: 10.1056/NEJMc2001737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ai T, Yang Z, Hou H, et al. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 2020;0:200642. doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liu J, Yu H, Zhang S. The indispensable role of chest CT in the detection of coronavirus disease 2019 (COVID-19) Eur J Nucl Med Mol Imaging. 2020 Apr 3; doi: 10.1007/s00259-020-04795-x. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.China NHCotPsRo. Diagnosis and treatment protocols of pneumonia caused by a novel coronavirus (trial version 5) 2020. Available at: http://www.nhc.gov.cn/yzygj/s7653p/202002/3b09b894ac9b4204a79db5b8912d4440.shtml.
- 7.ACR Recommendations for the use of Chest Radiography and Computed Tomography (CT) for Suspected COVID-19 Infection. Mar 22, 2020. Available at: https://www.acr.org/Advocacy-and-Economics/ACR-Position-Statements/Recommendations-for-Chest-Radiography-and-CT-for-Suspected-COVID19-Infection.
- 8.Mossa-Basha M, Meltzer CC, Kim DC, Tuite MJ, Kolli KP, Tan BS. Radiology department preparedness for COVID-19: radiology scientific expert panel. Radiology. 2020 Mar;16:200988. doi: 10.1148/radiol.2020200988. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.An P, Ye Y, Chen M, Chen Y, Fan W, Wang Y. Management strategy of novel coronavirus (COVID-19) pneumonia in the radiology department: a Chinese experience. Diagn Interv Radiol. 2020 Mar 25; doi: 10.5152/dir.2020.20167. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baum A, Newman S, Weinman J. Cambridge Handbook of Psychology, Health and Medicine. 1st ed. Cambridge, UK: Cambridge University Press; 1997. [Google Scholar]
- 11.Rubin GD, Ryerson CJ, Haramati LB, et al. The role of chest imaging in patient management during the COVID-19 pandemic: a multinational consensus statement from the Fleischner Society. Radiology. 2020 Apr 7; doi: 10.1148/radiol.2020201365. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li R, Pei S, Chen B, et al. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV2) Science. 2020 Mar 16; doi: 10.1126/science.abb3221. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gattinoni L, Chiumello D, Caironi P, et al. COVID-19 pneumonia: different respiratory treatment for different phenotypes? Intensive Care Medicine. 2020 doi: 10.1007/s00134-020-06033-2. [In press] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sverzellati N, Milanese G, Milone F, Balbi M, Ledda RE, Silva M. Integrated radiologic algorithm for COVID-19 Pandemic. J Thorac Imaging. 2020 Apr 7; doi: 10.1097/RTI.0000000000000516. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sverzellati N, Milone F, Balbi M. How imaging should properly be used in COVID-19 outbreak: an Italian experience. Diagn Interv Radiol. 2020 Mar 31; doi: 10.5152/dir.2020.30320. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]