Abstract
PURPOSE
We aimed to evaluate whether tears of the posterior horn of the medial meniscus root ligament (PHMM RL) are associated with osteoarthritis of the far posterior femoral condyles (FPFC).
METHODS
Retrospective review of 1158 patients who underwent arthroscopy identified 49 patients with confirmed tears of the medial meniscus posterior root ligament attachment. Preoperative magnetic resonance imaging (MRI) studies were reviewed to identify advanced osteoarthritis involving the medial and lateral FPFC. Control patients (n=48) had no meniscal tears confirmed by arthroscopy. Cases and controls were age- and sex-matched exactly 1:1. One case patient was excluded since there was no age- and sex-matched control available. The International Cartilage Research Society (ICRS) MRI cartilage grade was recorded for the medial and lateral FPFC. Associations were evaluated using univariate and multivariable conditional logistic regression analyses.
RESULTS
There were 48 case and 48 control patients (10 men in each group, 20.8%) with median age 53 years (range, 21–67). Medial FPFC ICRS Grade 2 or higher lesions were present in 34 (70.8%) of case patients and 16 (33.3%) of control patients. Lateral FPFC ICRS Grade 2 or higher lesions were present in 24 (50%) of case patients and 14 (28.2%) of control patients. Increased body mass index (BMI) was associated with PHMM RL tears (OR=1.11, 95% CI [1.01, 1.22], P = 0.020). MRI was 81.2% (39/48) sensitive and 91.2% (44/48) specific for detection of PHMM RL tears. PHMM RL tears were associated with Grade 2 or higher medial FPFC osteoarthritis (OR=10.00, 95% CI (2.34, 42.78), P < 0.001). This association remained after adjusting for BMI (OR=11.79, 95% CI [2.46, 56.53], P = 0.002). There was also an association between PHMM RL tears and lateral FPFC osteoarthritis, which persisted after adjusting for BMI (OR =3.00, 95% CI [1.07, 8.37], P = 0.036).
CONCLUSION
PHMM RL tears are associated with advanced osteoarthritis of the FPFC. Radiologists identifying FPFC osteoarthritis should look carefully for PHMM RL tears.
Knee arthroscopy requires placement of portals for the evaluation and treatment of intra-articular knee disease (1, 2). Each arthroscopic portal has a potential blind spot that limits evaluation (1, 2). Evaluation of the posteromedial compartment and in particular the posterior horn of the medical meniscus and far posterior femoral condyle (FPFC) cartilage are limited when using routine anterior portals (1–3). More recent research has confirmed that the FPFC cartilage is a potential blind spot during routine arthroscopy (4). Posteromedial, posterolateral and posterior trans-septal portals can be used to better visualize the FPFC cartilage and posterior root ligaments of the menisci; however, these are generally only utilized if the clinical presentation or magnetic resonance imaging (MRI) findings suggest FPFC osteoarthritis or posterior meniscal pathology (1, 5).
MRI has been shown to be an accurate predictor of knee osteoarthritis (6,7); however, MRI has a limited sensitivity and positive predictive value for detecting posterior horn root ligament (PHRL) tears (8, 9). LaPrade et al. (8) have shown that 3.0 T MRI has a sensitivity of 77% and a specificity of approximately 73% for detecting PHRL tears, whereas Ozkoc et al. (9) have estimated the sensitivity of MRI to detect PHRL tears at around 72%. Therefore, almost one-third of PHRL tears are not identified by MRI (8, 9). Identifying an imaging sign that could increase diagnostic confidence in detecting PHRL tears would be of significant clinical importance. Biomechanical studies have shown that PHRL tears are associated with decreased contact area between the femur and tibia, and increased pressure between the tibia and femur at increased flexion angles (9–11). In flexion, the femur is posteriorly translated and externally rotated with increased contact between the FPFC cartilage and the tibial cartilage (11–13). Additional longitudinal data from the Multicenter Osteoarthritis Study suggest that PHRL tears of the medial meniscus result in increased osteoarthritis in the medial tibiofemoral compartment and increased meniscal extrusion (14, 15). A prior study by Guermazi et al. (16) found that PHRL tears of the medial meniscus were associated with development and worsening of medial tibiofemoral osteoarthritis; however, this study evaluated tears identified by a radiologist that were not confirmed by arthroscopy, which is the gold standard for the evaluation and detection of tears. Based on these findings, we hypothesized that PHRL tears, in particular tears of the posterior horn of the medial meniscus root ligament (PHMM RL), would be associated with joint degeneration especially at the FPFC. Therefore, the aim of this study is to evaluate whether FPFC advanced osteoarthritis is associated with PHMM RL tears.
Methods
This retrospective study was performed at a single tertiary care academic healthcare center. The study protocol was reviewed and approved (protocol #828674) by the local institutional review board /ethics committee and the need for signed informed consent from each patient was waived.
The surgical and medical records of 1158 patients who underwent knee arthroscopy by two orthopedic surgeons with 24 and 28 years of experience, respectively, were reviewed. Of these 1158 patients, 49 had arthroscopically confirmed tears of the PHMM RL and one had an arthroscopically confirmed tear of the posterior horn of the lateral meniscus root ligament (PHLM RL) while satisfying the study inclusion and exclusion criteria. To assess whether PHMM RL tears were associated with FPFC osteoarthritis, a cohort of 48 patients with arthroscopically confirmed tears were directly matched 1:1 by age and sex to control patients (patients with arthroscopically confirmed intact PHMM RL and PHLM RL). We were unable to find an age and sex matched control for one of the patients with a PHMM RL tear (a 64-year-old man), so this individual was excluded from the analysis.
Inclusion and exclusion criteria
Patients had to have arthroscopy of the knee confirming tears of the PHMM RL as well as a pre-operative MRI of the knee of diagnostic quality to evaluate the FPFC (Fig. 1). Knees were included in the study if preoperative MRI images and radiologists’ reports within 1 month prior to arthroscopy were available in the picture archiving and communication systems (PACS) at our institution. Control patients also had to have arthroscopic confirmation of no RL tears.
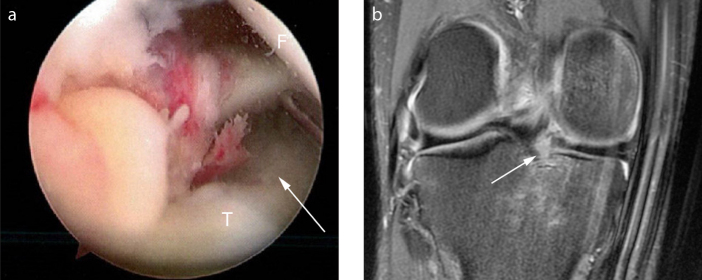
Figure 1. a, b.
Arthroscopic image (a) of the right knee in an 18-year-old male demonstrates a PHMM RL radial tear (white arrow) with surrounding edema and hemorrhage (T, medial tibial plateau; F, medial femoral condyle). Coronal fat-suppressed proton density-weighted image (b) of the same patient shows the PHMM RL radial tear (white arrow) with bone marrow edema like signal and contusion in the medial tibial plateau.
Patients were excluded if a pre-operative (pre-arthroscopy) MRI of diagnostic quality was not present, if they had history of prior infection, an inflammatory arthropathy involving the knee (including gout, rheumatoid arthritis, systemic lupus erythematosus), prior surgery/arthroscopy or fracture of the knee (femur, tibia or patella), prior anterior cruciate ligament (ACL) and/or posterior cruciate ligament tears. Patients underwent treatment at our institution between January 1, 2006 and January 1, 2019.
Clinical and demographic data
Clinical and demographic data at the time of the MRI including patient age, sex, height, weight, and body mass index (BMI) were collected from the electronic medical record. Arthroscopy reports were used to confirm diagnoses of PHRL tears and to identify normal controls.
MRI protocol
Patients were imaged using either 1.5 T or 3.0 T MRI systems (GE Medical Systems or Siemens Medical Solutions) by using routine clinical protocols and dedicated knee coils. All sequences were utilized for interpretation. Pulse sequences included: a) axial fat-suppressed proton-density (PD)-weighted sequence with echo time (TE) of 2000–4000 ms and repetition time (TR) of 20–40 ms, slice thickness of 3 mm, and interslice gap of 1 mm; b) coronal fat-suppressed PD-weighted sequence with TE of 2000–4000 ms and TR of 20–40 ms, slice thickness of 3 mm, and interslice gap of 1 mm; c) coronal T1-weighted sequence with TE of 400–800 ms and TR of 8–20 ms, slice thickness of 3 mm, and interslice gap of 1 mm; d) sagittal fat-suppressed PD-weighted sequence with TE of 2000–4000 ms and TR of 20–40 ms, slice thickness of 3 mm, and interslice gap of 1 mm; and e) sagittal T2-weighted sequence with TE of >4000 ms and TR of 75–120 ms, slice thickness of 3 mm, and interslice gap of 1 mm. Images were evaluated using Sectra PACS.
MRI measurements
Patients and control patients were randomly mixed and evaluated in a blinded fashion. FPFC osteoarthritis was graded using the International Cartilage Repair Society (ICRS) classification as 0, none; 1, surface fraying/irregularity; 2, mild cartilage loss involving less than 50% of the adjacent cartilage thickness (Fig. 2); 3, moderate cartilage loss involving greater than 50% of the adjacent cartilage thickness (Fig. 3); and 4, severe with involvement of the subchondral bone including any subchondral cyst like change/edema like change (Fig. 4) (17). We chose to study only the FPFC osteoarthritis, because this was the pattern we have noted anecdotally in clinical practice. Two fellowship trained musculoskeletal radiologists evaluated magnetic resonance images from each patient in the dataset and graded FPFC osteoarthritis using the ICRS criteria. Discrepancies were solved by consensus. Radiologists were blinded to whether there was a PHRL tear or not. PHMM RL tears were analyzed separately from PHLM RL tears.
Figure 2.
Sagittal fat-suppressed proton density-weighted image from MRI study of the left knee of a 52-year-old woman with a PHMM RL tear demonstrates ICRS Grade 2 chondral lesion of the medial FPFC. The white arrow shows an area of cartilage signal heterogeneity and fissuring with less than 50% cartilage depth involving the medial FPFC consistent with an ICRS Grade 2 cartilage lesion.
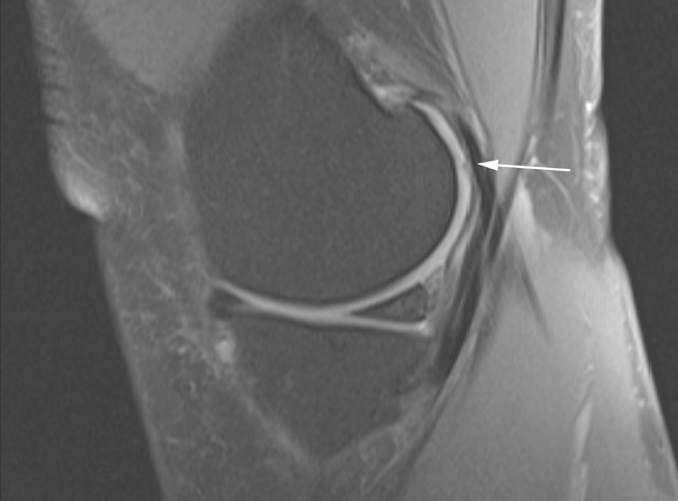
Figure 3.

Sagittal fat-suppressed proton density-weighted image from MRI study of the right knee of a 43-year-old woman with a PHMM RL tear demonstrates ICRS Grade 3 chondral lesion of the medial FPFC. The white arrow shows an area of cartilage delamination with greater than 50% cartilage depth involving the medial FPFC consistent with an ICRS Grade 3 cartilage lesion.
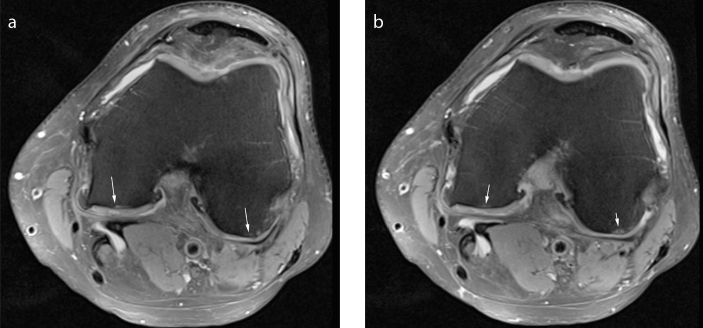
Figure 4. a, b.
Consecutive axial fat-suppressed proton density-weighted images (a) and (b) from MRI study of the right knee of a 49-year-old woman with a PHMM RL tear demonstrates ICRS Grade 4 chondral lesions of the medial and lateral FPFC. The white arrows show subchondral cyst like and edema-like lesion in the medial and lateral FPFC. There are ICRS Grade 4 cartilage lesions noted. The cartilage is severely abnormal extending down through the subchondral bone.
Prospective diagnostic accuracy of MRI to detect PHRL tears
All MRI scans were interpreted by a musculoskeletal fellowship trained and board-certified diagnostic radiologist. The radiologists’ reports from all of the pre-operative MRI studies were evaluated for both patients and control patients to assess whether the radiologist prospectively suspected a tear of the PHMM RL or PHLM RL. This method was chosen as it faithfully mirrors daily clinical practice. The type of meniscal tear was also recorded. A horizontal tear was defined as a tear parallel to the tibial plateau that separates the root into upper and lower parts (18). A longitudinal tear was defined as a vertical tear (perpendicular to the tibial plateau) that extends parallel to the main axis of the root (18). A radial tear was defined as a vertical tear that extends perpendicular to the main axis (18). An oblique tear was defined as a vertical tear that extends obliquely to the main axis of the root (18). A complex tear was defined as a tear with ≥2 of the previously described tears (18).
Statistical analysis
The Shapiro-Wilks test determined non-normal distribution for age, height, weight, and BMI. The analyses were performed using the untransformed and transformed predictor variables (log transformation for height, weight, BMI, and a power transformation to the power 3 for age). These transformations made all variables (age, height, weight and BMI) normal.
Descriptive statistics of the data are presented with n (%) and, for the non-normalized variables are shown as median (range). Because of the matched design, Wilcoxon signed rank test was used to compare quantitative variables between the two matched groups. McNemar’s test was used to compare categorical variables between the two matched groups.
Because only one patient had a PHLM RL tear, no association analyses with PHLM RL could be performed. The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy of MRI to detect PHMM RL tears were calculated.
Univariate conditional logistic regression models were used to evaluate the association between medial FPFC osteoarthritis and PHMM RL tears; and to evaluate the association between lateral FPFC osteoarthritis and PHMM RL tears. Multivariable conditional logistic regression models including BMI were used to evaluate whether the associations detected were mediated by BMI. The analyses were performed evaluating patients with advanced osteoarthritis (at least mild osteoarthritis of ICRS Grade 2 or higher), since these can be reliably detected by MRI (17).
We repeated both the univariate and multivariable conditional logistic regression models using the variables transformed to achieve normality to show that the inference and conclusions are unchanged. The likelihood ratio test statistic was used to assess the joint significance of both variables in the multivariable conditional logistic regression models. The R-squared value was provided to evaluate the goodness of fit of the multivariable conditional logistic regression models.
A priori, we hypothesized that approximately 30% of control patients would have medial FPFC ICRS 2, 3, or 4 lesions, that 75% of patients with PHMM RL tears would have medial FPFC ICRS 2, 3, or 4 lesions, and that the ratio of control patients to patients with PHRL tears would be 1:1. A sample size of 67 patients (28 with no meniscal tears and 39 with PHRL tears) would have 80% power with a Type I error rate, a=0.05 to detect a risk ratio of 2.33. Statistical significance of results was set at α=0.05, and all statistical tests were two-sided. R statistical software v3.4 (19) was utilized for the statistical analyses.
Results
There were 1158 patients who underwent arthroscopy in the study period. Approximately 4.3% (n=50) had tears of the PHRL: 49 with tears of the PHMM RL and one with a tear of the PHLM RL. One patient with PHMM RL tear was excluded due to the inability to find an age- and sex-matched control. Patient demographics and clinical characteristics are shown in Table 1. Median BMI was higher in patients with PHMM RL tears than in control patients (P = 0.022) (Table 1). All 48 control patients had arthroscopically confirmed normal menisci. Because patients were matched by age and sex, no association analyses with age and sex were performed. Only one patient had a PHLM RL tear, so no association analyses with PHLM RL could be performed.
Table 1.
Summary of clinical and demographic statistics
| Variable | PHMM RL tear (n=48) | Control (n=48) | P |
|---|---|---|---|
| Age (years), median (range) | 53 (21–67) | 53 (21–67) | 1.000a |
|
| |||
| Height (m), median (range) | 1.68 (1.47–1.83) | 1.66 (1.52–1.98) | 0.519a |
|
| |||
| Weight (kg), median (range) | 85.8 (54.40–180.40) | 80.30 (45.2–123.8) | 0.100a |
|
| |||
| BMI (kg/m2), median (range) | 31.36 (21.2–62.3) | 27.82 (17.4–42.6) | 0.022a |
|
| |||
| Male, n (%) | 10 (20.8) | 10 (20.8) | 1.000b |
|
| |||
| Medial FPFC ICRS grades, n (%) | <0.001b | ||
| Grade 0 or 1 | 14 (29.2) | 32 (66.7) | |
| Grade 2 or higher | 34 (70.8) | 16 (33.3) | |
|
| |||
| Lateral FPFC ICRS grades, n (%) | 0.033b | ||
| Grade 0 or 1 | 24 (50) | 34 (70.8) | |
| Grade 2 or higher | 24 (50) | 14 (29.2) | |
PHMM RL, posterior horn of the medial meniscus root ligament; BMI, body mass index; FPFC, far posterior femoral condyle; ICRS, International Cartilage Regeneration and Joint Preservation Society.
Wilcoxon signed rank test;
McNemar test.
MRI had a sensitivity of 81.2% (39/48), specificity of 91.2% (44/48), PPV of 90.7% (39/43), NPV of 83% (44/53) and accuracy of 86.5% (83/96) for detecting PHMM RL tears. The patient with the PHLM RL tear was prospectively identified as having a tear by the radiologist. Of the 39 patients with arthroscopically confirmed PHMM RL tears that were prospectively identified radiographically, 5 (12.8%) were complex tears, 1 (2.6%) was a horizontal tear and 33 (84.6%) were radial tears. Of the 9 patients with arthroscopically confirmed PHMM RL tears that were not prospectively confirmed radiographically, 1 (11.1%) was a horizontal tear and 8 (88.9%) were small radial tears. Of the 4 control patients that were misclassified as having PHMM RL tears, 2 (50%) had horizontal tears of the body and posterior horns of the MM, 1 (25%) had a radial tear of the PHMM (1) and 1 (25%) had a complex tear of the lateral meniscus.
Univariate conditional logistic regression analysis showed that higher BMI was associated with PHMM RL tears (OR=1.11, 95% CI [1.01, 1.22], P = 0.020) (Table 2). PHMM RL tears were associated with medial FPFC ICRS Grade 2 or higher lesions (OR=10.00, 95% CI [2.34, 42.78], P < 0.001), and associated with lateral FPFC ICRS Grade 2 or higher (OR=2.67, 95% CI [1.04, 6.82], P = 0.033). There was no association between PHMM RL tears and height (OR=0.15, 95% CI [0.01, 25.99], P = 0.473) or weight (OR=1.02, 95% CI [1.00, 1.05], P = 0.076). These results were unchanged when using the transformed predictor variables that were transformed for normality, as expected. We found no association between PHMM RL tears and transformed height (OR=0.05, 95% CI [0.00, 301.1], P = 0.503) or transformed weight (OR=9.98, 95% CI [0.878, 118.8], P = 0.068).
Table 2.
Univariate association with PHMM RL tears
| Variable | β (95% CI) | OR (95% CI) | Conditional logistic regression score test P |
|---|---|---|---|
| Height (m) | −1.87 (−6.99, 3.26) | 0.15 (0.00, 25.99) | 0.473 |
| Weight (kg) | 0.02 (0.00, 0.05) | 1.02 (1.00, 1.05) | 0.076 |
| BMI (kg/m2) | 0.10 (0.01, 0.19) | 1.11 (1.01, 1.22) | 0.020 |
| Medial FPFC osteoarthritis (ICRS Grade 2 or higher) | 2.30 (0.85, 3.76) | 10.00 (2.34, 42.78) | <0.001 |
| Lateral FPFC osteoarthritis (ICRS Grade 2 or higher) | 0.98 (0.04, 1.92) | 2.67 (1.04, 6.82) | 0.033 |
PHMM RL, posterior horn of the medial meniscus root ligament; CI, confidence interval; OR, odds ratio; BMI, body mass index; FPFC, far posterior femoral condyle; ICRS, International Cartilage Regeneration and Joint Preservation Society.
The association between PHMM RL tears and medial FPFC ICRS Grade 2 or higher lesions remained in the multivariable conditional logistic regression analysis after adjusting for BMI (OR=11.79, 95% CI [2.46, 56.53], P = 0.002) (Table 3). There was also an association between PHMM RL tears and lateral FPFC ICRS Grade 2 or higher lesions (OR=3.00, 95% CI [1.07, 8.37], P = 0.036). Both multivariable conditional logistic regression models were significant, showing that both BMI and PHMM RL tears were jointly associated with medial FPFC osteoarthritis (Joint model likelihood ratio test, P < 0.001) and lateral FPFC osteoarthritis (Joint model likelihood ratio test, P = 0.004).
Table 3.
Multivariable association with PHMM RL tears after adjusting for BMI
| Variable | β (95% CI) | OR (95% CI) | Conditional logistic regression Wald test P |
Overall model R2 |
Model likelihood ratio test P* |
|---|---|---|---|---|---|
| Medial FPFC osteoarthritis (ICRS Grade 2 or higher) | 2.47 (0.90, 4.03) | 11.79 (2.46, 56.53) | 0.002 | 0.21 | <0.001 |
| Lateral FPFC osteoarthritis (ICRS Grade 2 or higher) | 1.10 (0.07, 2.12) | 3.00 (1.07, 8.37) | 0.036 | 0.11 | 0.004 |
PHMM RL, posterior horn of the medial meniscus root ligament; BMI, body mass index; CI, confidence interval; OR, odds ratio; FPFC, far posterior femoral condyle; ICRS, International Cartilage Regeneration and Joint Preservation Society.
Model Likelihood Ratio Test P value evaluates the joint simultaneous significance of BMI and PHMM RL tears for predicting osteoarthritis.
These multivariable conditional logistic regression results were unchanged when using the transformed predictor variables. The association between PHMM RL tears and medial FPFC ICRS Grade 2 or higher lesions remained after adjusting for transformed BMI (OR=12.39, 95% CI [2.55, 60.19], P = 0.002) and the association between PHMM RL tears and lateral FPFC ICRS Grade 2 or higher lesions remained after adjusting for transformed BMI (OR=3.12, 95% CI [1.11, 8.77], P = 0.018). Both multivariable conditional logistic regression models remained significant showing that both transformed BMI and PHMM RL tears were jointly associated with medial FPFC osteoarthritis (P < 0.001) and lateral FPFC osteoarthritis (P = 0.004).
Discussion
Our results show that tears of the PHMM RL tears are more common in patients with higher BMI. Tears of the PHMM RL are also associated with osteoarthritis of the medial FPFC and the lateral FPFC. These findings have important clinical ramifications. The FPFC can be a hidden area on arthroscopy, but is better visualized by MRI. We have confirmed an association between FPFC osteoarthritis and PHMM RL tears. Clinicians identifying FPFC osteoarthritis should look carefully for PHRL tears. Similarly, if a PHRL tear is identified, then the clinician should look carefully for FPFC osteoarthritis.
The Apley’s grind test is a common clinical test used to detect meniscal pathology (20–22). The patient is usually in the prone position on an examination table, with the knee flexed to approximately 90 degrees (20, 21). The patient’s thigh is immobilized by the clinician, while the tibia is medially and laterally rotated with compression by the clinician (20, 21). Meniscal tears can be detected because the patient usually complains of increased pain with compression and rotation during the Apley grind test (20, 21). In 90 degrees of flexion, the FPFC has more contact with the tibia and is under more pressure with compression (10–12, 20, 21). Based on the association noted, we hypothesized that the development of osteoarthritis in the FPFC may contribute to a positive Apley grind test. Biomechanical studies have shown that tears of the PHMM RL result in increased tibiofemoral contact pressure with the knee in flexion (10–12), which may explain our finding.
The meniscus has been shown to be a biomechanically integral structure that prevents the development of osteoarthritis (10, 11, 14–16, 23). Meniscal tears have been associated with development of osteoarthritis of the knee (14–16, 24–27). Patients undergoing large meniscectomies are also at increased risk of development of osteoarthritis of the knee (26, 27). This study confirms the PHMM RL tear is associated with osteoarthritis of the FPFC. Crema et al. (14) hypothesized that meniscal extrusion may be indicative of loss of the meniscal function, and showed that the varus alignment of the knee, medial tibiofemoral compartment cartilage damage and other medial meniscal tears are associated with meniscal extrusion. Crema et al. (14) have posited that meniscal tears may affect the complex interactions among joint tissues and mechanical stresses involved in the osteoarthritis process, and our study suggests that this hypothesis may be correct.
Other studies have also shown that the risk of development of osteoarthritis increases with age (28, 29) and higher BMI (29, 30). Finally, other groups have shown an association between posterior medial meniscal root tears and osteoarthritis of the knee (31–33), similar to our findings; however, these prior studies did not specifically evaluate how the FPFC was affected by PHMM RL tears. This association is supported by the results from previously published biomechanical studies (10–12).
Our study also confirms that MRI is not perfect for detection of meniscal root tears. Approximately one-third of PHMM RL tears are thought to be undetected by radiologists (8, 9); however, in our series, the sensitivity was somewhat better, at almost 80%. Studies evaluating the effects of meniscal root tears should therefore have arthroscopic correlation and confirmation since MRI evaluation even by experienced musculoskeletal radiologists is not perfect.
This study had a few limitations. First, the study is retrospective and performed at a single tertiary care academic center and subject to ascertainment bias. Osteoarthritis was not confirmed arthroscopically, in part due to the fact that osteoarthritis of the FPFC are difficult to visualize arthroscopically from standard arthroscopic portals (1–3). The study population all underwent arthroscopy, so patient selection bias may result in overestimation of FPFC osteoarthritis prevalence relative to the general population. Nonetheless, the study was adequately powered to detect a robust association between PHMM RL tears and osteoarthritis of the FPFC. There are other areas in the tibiofemoral compartment that are potentially at risk for the development of osteoarthritis with PHMM RL tears (14–16). We did not investigate these areas because the association with the FPFC was the one we anecdotally observed most frequently in clinical practice, and therefore was the main driving factor in our hypothesis. Our study could be underpowered to evaluate these other areas given the sample size. FPFC osteoarthritis was also a feature that we thought could be used to help the radiologists identify occult tears of the PHMM. Future research could be done to evaluate how PHMM RL tears specifically influence the development of osteoarthritis in other areas of the tibiofemoral and patellofemoral compartments. While we found an association between FPFC osteoarthritis and PHMM RL tears, several of the control patients had FPFC osteoarthritis and several of the case patients with PHMM RL tears had no FPFC osteoarthritis. This suggests that other factors besides PHMM RL tears contribute to FPFC osteoarthritis, including knee alignment and morphology (14). The PHMM RL tear may need to be more chronic before FPFC osteoarthritis develops. Further research is required to confirm this assertion.
In conclusion, this study shows that there is an association between advanced FPFC osteoarthritis and PHMM RL tears. Patients with increased BMI were more likely to have FPFC osteoarthritis.
Main points.
MRI was 81.2% sensitive and 91.2% specific for detection of posterior horn of the medial meniscus root ligament tears.
Increase in BMI is associated with posterior horn of the medial meniscus root ligament tears.
Tears of the posterior horn of the medial meniscal root ligament are associated with advanced osteoarthritis of the medial and lateral far posterior femoral condyle (non-weight bearing posterior femoral condyle).
Radiologists identifying far posterior femoral condyle cartilage lesions should look carefully at the posterior horn of the medial meniscus root ligament attachment to exclude occult tears.
Footnotes
Conflict of interest disclosure
The authors declared no conflicts of interest.
References
- 1.Ahn J, Lee DH, Lee YS, Wang JH, Ha HC. Clearing a blind spot in knee arthroscopy: popliteal bursa. Knee Surg Sports Traumatol Arthrosc. 2008;16:549–552. doi: 10.1007/s00167-008-0488-z. [DOI] [PubMed] [Google Scholar]
- 2.Tolin BS, Sapega AA. Arthroscopic visual field mapping at the periphery of the medial meniscus: a comparison of different portal approaches. Arthroscopy. 1993;9:265–271. doi: 10.1016/S0749-8063(05)80420-7. [DOI] [PubMed] [Google Scholar]
- 3.Sando MJ, Rajaee SS, Liu JP, Banffy M, Limpisvasti O, Crues JV., 3rd identifying hidden zones of the far posterior cartilage of the femoral condyles not visible during knee arthroscopy. AJR Am J Roentgenol. 2017;208:W121–W126. doi: 10.2214/AJR.16.17080. [DOI] [PubMed] [Google Scholar]
- 4.Ogino S, Huang T, Watanabe A, Iranpour-Boroujeni T, Yoshioka H. Magnetic resonance imaging of articular cartilage abnormalities of the far posterior femoral condyle of the knee. Acta Radiol. 2010;51:52–57. doi: 10.3109/02841850903307566. [DOI] [PubMed] [Google Scholar]
- 5.Pace JL, Wahl CJ. Arthroscopy of the posterior knee compartments: neurovascular anatomic relationships during arthroscopic transverse capsulotomy. Arthroscopy. 2010;26:637–642. doi: 10.1016/j.arthro.2009.09.009. [DOI] [PubMed] [Google Scholar]
- 6.Bredella MA, Tirman PF, Peterfy CG, et al. Accuracy of T2-weighted fast spin-echo MR imaging with fat saturation in detecting cartilage defects in the knee: comparison with arthroscopy in 130 patients. AJR Am J Roentgenol. 1999;172:1073–1080. doi: 10.2214/ajr.172.4.10587150. [DOI] [PubMed] [Google Scholar]
- 7.Potter HG, Linklater JM, Allen AA, Hannafin JA, Haas SB. Magnetic resonance imaging of articular cartilage in the knee. An evaluation with use of fast-spin-echo imaging. J Bone Joint Surg Am. 1998;80:1276–1284. doi: 10.2106/00004623-199809000-00005. [DOI] [PubMed] [Google Scholar]
- 8.LaPrade RF, Ho CP, James E, Crespo B, LaPrade CM, Matheny LM. Diagnostic accuracy of 3.0 T magnetic resonance imaging for the detection of meniscus posterior root pathology. Knee Surg Sports Traumatol Arthrosc. 2015;23:152–157. doi: 10.1007/s00167-014-3395-5. [DOI] [PubMed] [Google Scholar]
- 9.Ozkoc G, Circi E, Gonc U, Irgit K, Pourbagher A, Tandogan RN. Radial tears in the root of the posterior horn of the medial meniscus. Knee Surg Sports Traumatol Arthrosc. 2008;16:849–854. doi: 10.1007/s00167-008-0569-z. [DOI] [PubMed] [Google Scholar]
- 10.Geeslin AG, Civitarese D, Turnbull TL, Dornan GJ, Fuso FA, LaPrade RF. Influence of lateral meniscal posterior root avulsions and the meniscofemoral ligaments on tibiofemoral contact mechanics. Knee Surg Sports Traumatol Arthrosc. 2016;24:1469–1477. doi: 10.1007/s00167-015-3742-1. [DOI] [PubMed] [Google Scholar]
- 11.Allaire R, Muriuki M, Gilbertson L, Harner CD. Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Joint Surg Am. 2008;90:1922–1931. doi: 10.2106/JBJS.G.00748. [DOI] [PubMed] [Google Scholar]
- 12.Vedi V, Williams A, Tennant SJ, Spouse E, Hunt DM, Gedroyc WM. Meniscal movement. An in-vivo study using dynamic MRI. J Bone Joint Surg Br. 1999;81:37–41. doi: 10.1302/0301-620X.81B1.0810037. [DOI] [PubMed] [Google Scholar]
- 13.Chen HN, Yang K, Dong QR, Wang Y. Assessment of tibial rotation and meniscal movement using kinematic magnetic resonance imaging. J Orthop Surg Res. 2014;21:65–68. doi: 10.1186/s13018-014-0065-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Crema MD, Roemer FW, Felson DT, et al. Factors associated with meniscal extrusion in knees with or at risk for osteoarthritis: the multicenter osteoarthritis study. Radiology. 2012;264:494–503. doi: 10.1148/radiol.12110986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Crema MD, Guermazi A, Li L, et al. The association of prevalent medial meniscal pathology with cartilage loss in the medial tibiofemoral compartment over a 2-year period. Osteoarthritis Cartilage. 2010;18:336–343. doi: 10.1016/j.joca.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 16.Guermazi A, Hayashi D, Arraya M, et al. Medial posterior meniscal root tears are associated with development or worsening of medialtibiofemoral cartilage damage: the multicenter osteoarthritis study. Radiology. 2013;268:814–821. doi: 10.1148/radiol.13122544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Reed ME, Villacis DC, Hatch GF, 3rd, et al. 3.0-Tesla MRI and arthroscopy for assessment of knee articular cartilage lesions. Orthopedics. 2013;36:e1060–1064. doi: 10.3928/01477447-20130724-24. [DOI] [PubMed] [Google Scholar]
- 18.Lee YG, Shim JC, Choi YS, Kim JG, Lee GJ, Kim HK. Magnetic resonance imaging findings of surgically proven medial meniscus root tear: tear configuration and associated knee abnormalities. J Comput Assist Tomogr. 2008;32:452–457. doi: 10.1097/RCT.0b013e31812f4eb0. [DOI] [PubMed] [Google Scholar]
- 19.R Development Core. Team R: A language and environment for statistical computing. R Foundation for Statistical Computing; Vienna, Austria: 2008. Available at: http://www.R-project.org. [Google Scholar]
- 20.Fowler PJ, Lubliner JA. The predictive value of five clinical signs in the evaluation of meniscal pathology. Arthroscopy. 1989;5:184–186. doi: 10.1016/0749-8063(89)90168-0. [DOI] [PubMed] [Google Scholar]
- 21.Agresti D, Jeanmonod R. StatPearls [Internet] Treasure Island (FL): StatPearls Publishing; 2018. Apley Grind Test. [PubMed] [Google Scholar]
- 22.Kurosaka M, Yagi M, Yoshiya S, Muratsu H, Mizuno K. Efficacy of the axially loaded pivot shift test for the diagnosis of a meniscal tear. Int Orthop. 1999;23:271–274. doi: 10.1007/s002640050369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wojtys EM, Chan DB. Meniscus structure and function. Instr Course Lect. 2005;54:323–330. [PubMed] [Google Scholar]
- 24.Englund M. The role of the meniscus in osteoarthritis genesis. Rheum Dis Clin North Am. 2008;34:573–579. doi: 10.1016/j.rdc.2008.05.009. [DOI] [PubMed] [Google Scholar]
- 25.Englund M, Guermazi A, Lohmander SL. The role of the meniscus in knee osteoarthritis: a cause or consequence? Radiol Clin North Am. 2009;47:703–712. doi: 10.1016/j.rcl.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 26.Weber J, Koch M, Angele P, Zellner J. The role of meniscal repair for prevention of early onset of osteoarthritis. J Exp Orthop. 2018;5:10. doi: 10.1186/s40634-018-0122-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Meredith DS, Losina E, Mahomed NN, Wright J, Katz JN. Factors predicting functional and radiographic outcomes after arthroscopic partial meniscectomy: a review of the literature. Arthroscopy. 2005;21:211–223. doi: 10.1016/j.arthro.2004.10.003. [DOI] [PubMed] [Google Scholar]
- 28.Slemenda CW. The epidemiology of osteoarthritis of the knee. Curr Opin Rheumatol. 1992;4:546–551. [PubMed] [Google Scholar]
- 29.Felson DT. The course of osteoarthritis and factors that affect it. Rheum Dis Clin North Am. 1993;19:607–615. [PubMed] [Google Scholar]
- 30.Felson DT. Weight and osteoarthritis. Am J Clin Nutr. 1996;63(Suppl 3):S430–432. doi: 10.1093/ajcn/63.3.430. [DOI] [PubMed] [Google Scholar]
- 31.Choi JY, Chang EY, Cunha GM, Tafur M, Statum S, Chung CB. Posterior medial meniscus root ligament lesions: MRI classification and associated findings. AJR Am J Roentgenol. 2014;203:1286–1292. doi: 10.2214/AJR.14.12559. [DOI] [PubMed] [Google Scholar]
- 32.Carreau JH, Sitton SE, Bollier M. Medial meniscus root tear in the middle aged patient: a case based review. Iowa Orthop J. 2017;37:123–132. [PMC free article] [PubMed] [Google Scholar]
- 33.Choi ES, Park SJ. Clinical evaluation of the root tear of the posterior horn of the medial meniscus in total knee arthroplasty for osteoarthritis. Knee Surg Relat Res. 2015;27:90–94. doi: 10.5792/ksrr.2015.27.2.90. [DOI] [PMC free article] [PubMed] [Google Scholar]