Abstract
Purpose
There is limited information regarding the prevalence and predictors of cost-related non-utilization (CRNU), while there is increasing attention to the rising out-of-pocket cost of health services including prescription medications. Prior studies have not quantified the role of perceived racism despite its documented relationship with health services utilization. We examine perceptions of reactions to race and quantify their relationship with CRNU.
Methods
This retrospective cross-sectional study utilized data from the 2014 Behavioral Risk Factor Surveillance System (BRFSS) public use file, an annual, state-based telephone survey of US adults aged 18 and older. We utilized data for four states that provided responses to five Reactions to Race items, including information about the self-perceived quality of the respondent’s health care experience compared with people of other races (worse vs same or better) and whether the respondent experienced physical symptoms because of treatment due to their race. The three binary outcomes were: 1) did not visit a physician; 2) did not visit a physician due to cost; 3) did not fill a prescription due to cost. We estimated covariate-adjusted odds ratios associated with each outcome using logistic regression models.
Results
The BRFSS sample consisted of 20,366 respondents of whom 8% were African American non-Hispanic, 12% were Hispanic and 73% were White. Three percent of respondents considered their experience to be worse than people of other races. Three percent of individuals reported physical symptoms because of treatment due to their race while 5% of respondents reported becoming emotionally upset because of treatment due to their race. The proportions for the three study outcomes were 11%, 13% and 7%, respectively. In covariate-adjusted models, a worse experience with the health care system was statistically significantly associated with CRNU (physician visit: 2.6 [95% CI: 1.6 – 4.3]). The experience of physical symptoms because of treatment due to race was statistically significantly associated with CRNU (physician visit: 2.6 [95% CI: 1.7 – 4]; prescription fills: 2.1 [1.2 – 3.6]). No Reactions to Race items were associated with general non-utilization.
Conclusions
Negative perceptions of reactions to race during the time of health services utilization is positively associated with CRNU, ie, foregoing physician visits and prescription fills due to cost.
Keywords: Cost-Related Non-Utilization, Behavioral Risk Factor Surveillance System, Reactions to Race
Introduction
Health care affordability for families remains a source of financial strain for millions of families in the United States. The Affordable Care Act increased rates of health care coverage for millions of previously uninsured adults and increased patient protections in health care coverage through mandated coverage for mental health services, coverage of essential preventive care services, and creating a maximum out-of-pocket limit for individuals and families.1 Despite these progressions, evidence demonstrates that combined health care out-of-pocket and premium expenses among middle- and high-income families have not significantly declined since 2013.2
Substantial out-of-pocket expenses in the forms of cost-sharing, premiums, and deductibles for families are associated with delayed or missed medical and pharmaceutical care, defined as cost-related non-utilization (CRNU).3-10 Fifty-one percent of US adults reported that a household family member or themselves postponed or avoided medical, pharmaceutical, or dental care in the last 12 months due to concerns regarding health care cost.8 Factors associated with CRNU can be assessed using an inverted Behavioral Healthcare Model which is a conceptual framework of health care utilization.11,12 This model was developed in an effort to define and measure the complex, multi-faceted factors associated with health care access and health care utilization.12 Early versions of the model have been criticized for not having sufficient focus on social resources13 or the influence of race across multiple domains of utilization.14 In 2000, the Gelberg-Andersen Behavioral Model for Vulnerable Populations (BMVP), a conceptual model of health care utilization among vulnerable groups, was published.15 The BMVP specifies that traditional, in combination with, predisposing, enabling, and need factors explain variation in health care among vulnerable populations. The BMVP does not include racial discrimination as a factor. Yet racism significantly impacts health care utilization.16-20
In a meta-analysis of 52 studies, experiencing racism was associated with a delay in health care utilization and decreased uptake of prescriber recommended treatments and pharmaceutical care.16 To date, there has not been a systematic analysis of the impact of perceived discrimination on CRNU and it is unclear whether prior results related to health care utilization apply to CRNU.
Figure 1 illustrates the nature of the relationship between perceived discrimination and CRNU. We examine CRNU as a unique component of non-utilization (NU) given that CRNU is focused on cost-related barriers to utilization. As illustrated in Figure 1, the conceptualization of cost in CRNU may include perceived costs of engagement with the health care system. Figure 1 indicates that a decision to forgo utilization occurs when the perceived cost of an encounter outweighs the perceived benefit. The perceived cost of the encounter may play a larger role in the CRNU decision compared with its role in the NU decision. Perceived discrimination may increase the opportunity cost (ie, the value of the foregone benefit of the next best alternative action) of a health care encounter by making the next best alternative (eg, seeking care outside the health care system) more desirable to the patient. A negative experience (eg, gendered racism) during a health encounter has been conceptualized in prior work21 as a predisposing factor that could reduce the likelihood of seeking traditional health care22 and increase the use of alternative health care services. We expect to disentangle and clarify the role of perceived discrimination by considering CRNU and NU outcomes in the same sample.
Figure 1. Relationship between perceived discrimination and cost-related non-utilization.
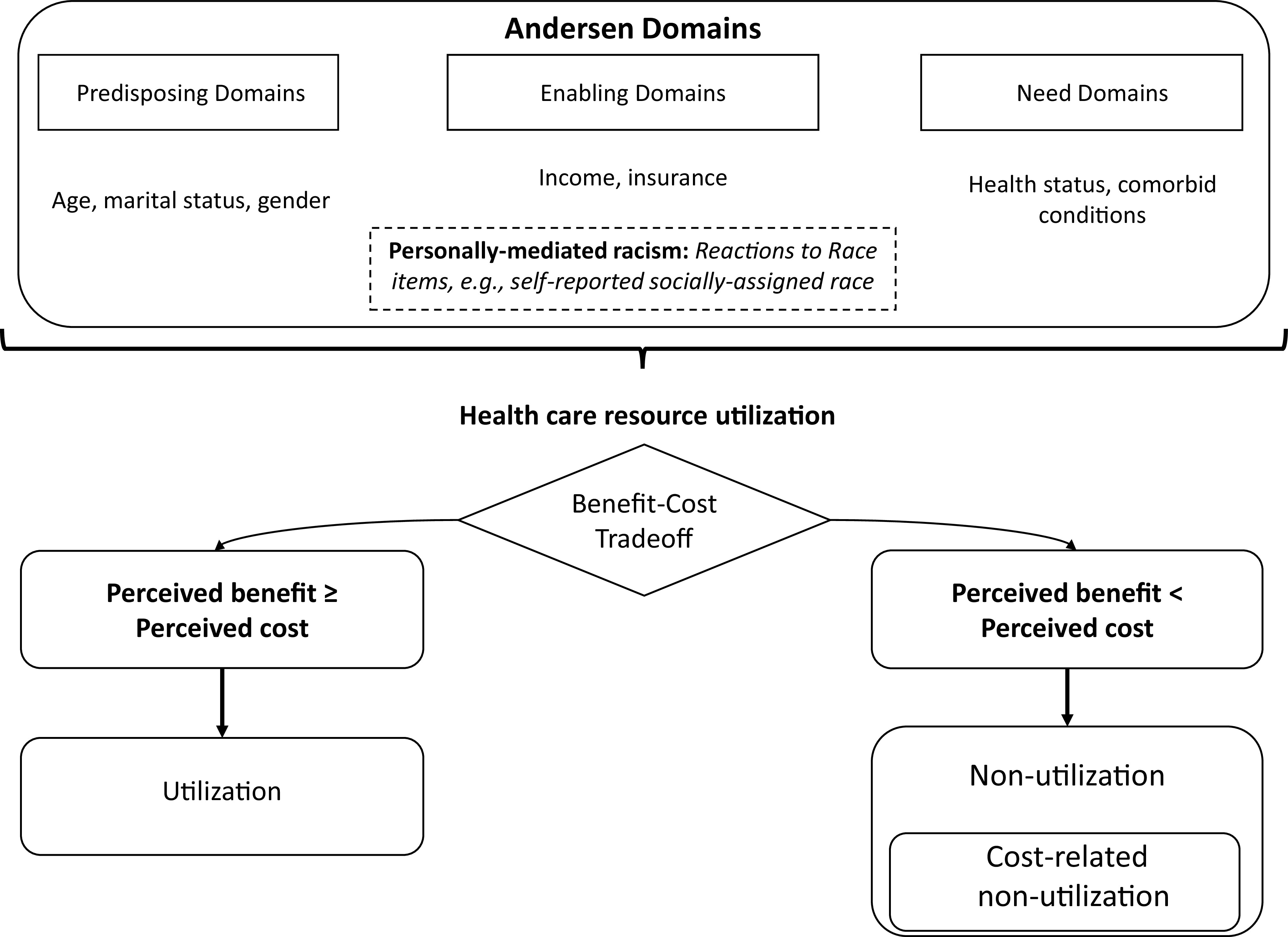
To examine the association between perceived discrimination and the CRNU and NU outcomes, we included measures of perceived discrimination in models of CRNU and NU and then qualitatively compared the association with the dependent variable across the three models. If opportunity cost considerations are relevant to CRNU outcomes, the implication is that we cannot examine certain utilization decisions in isolation and should consider the role of experiences that increase the perceived foregone value. In this study, we systematically examine the influence of perceived racism on variation in CRNU. We conceptualize negative perceptions of race as an enabling factor. Similar to the approach adopted to study non-utilization of health services where the key factors depended on the utilization category, we submit that different domains of the behavioral model will be important for CRNU compared with non-utilization of health services.
The objective of this work was to explore the association between self-reported reactions to race and CRNU alongside common predisposing, enabling, and need factors included in the BMVP. Given the focus on cost as the single reason for non-utilization, we expect that enabling factors such as annual household income will be important explanatory factors in a model of CRNU and will be less important in a model of general non-utilization. Furthermore, we submit that there may be additional differences between CRNU as it relates to physician visits foregone and CRNU as it relates to unfilled prescriptions due to the potential for higher out-of-pocket expenditure associated with prescription medications.
Methods
Study Population and Data Source
This cross-sectional study utilized data from the 2014 Behavioral Risk Factor Surveillance System (BRFSS) public use file. The BRFSS is an ongoing state-based telephone survey of non-institutionalized adults aged ≥18 years and residing in the United States. The BRFSS is a serial cross-sectional study and has been coordinated by the Centers for Disease Control and Prevention (CDC) on an annual basis since 1984. States have the option to field optional modules, such as the Reactions to Race module. In 2014, four states fielded this module. This study utilizes pooled data from these four states (Arizona, Minnesota, Mississippi and New Mexico) to conduct a cross-sectional analysis. The response rates for Arizona, Minnesota, Mississippi and New Mexico were: 41.6%, 54.4%, 41% and 52.8%.23 These response rates are comparable with expected response rates for the BRFSS which range from 48.7% for land line administration to 40.5% for cell-phone based outreach.23
Measures
Outcomes
We defined two measures of CRNU: no physician visit due to cost (CRNU_physician visit); no prescription filled due to cost (CRNU_prescription fill). We defined CRNU_physician visit as an affirmative response to the following question: “Was there a time in the past 12 months when you needed to see a doctor but could not because of cost?”.24 Similarly, we defined CRNU_prescription fill as an affirmative response to the following question: “Was there a time in the past 12 months when you did not take your medication as prescribed because of cost? Do not include over-the-counter (OTC) medication.” We do not expect negative perceptions of race to impact general non-utilization of health services since there is no defined role for cost as the single reason for non-utilization. We employ a falsification testing framework and test the relationship between Reactions to Race variables and general non-utilization of health services. We defined general non-utilization of health services as a response of “none” to the following question: “How many times have you been to a doctor, nurse, or other health professional in the past 12 months?”
Key Independent Variables
The Reactions to Race module was first piloted in 2002 and has been examined extensively in population-based research25; details are available elsewhere.26 The 2014 version utilized in this study represents the most recent year for which Reactions to Race data are available in the BRFSS file. The module includes six items assessing socially assigned race, degree of race consciousness, perceptions of differential treatment at work based on race, perceptions of differential experience based on race when seeking health care, and reports of negative emotional or physical symptoms resulting from treatment due to the respondent’s race. We captured respondents’ perceptions of a differential, race-based experience when seeking health care using responses to the following question: “Within the past 12 months when seeking health care, do you feel your experiences were worse than, the same as, or better than for people of other races?” We categorized responses as: 1) worse; 2) same or better. We captured the degree of race consciousness based on responses to the following question: “How often do you think about your race? Would you say never, once a year, once a month, once a week, once a day, once an hour, or constantly?” We categorized the responses as follows: 1: hardly = never or once a year; 2: often = monthly, weekly; 3: frequently = daily, hourly or constantly. We identified the presence of physical symptoms based on treatment due to race using responses to the following question: “Within the past 30 days, have you experienced any physical symptoms, for example, a headache, an upset stomach, tensing of your muscles, or a pounding heart, as a result of how you were treated based on your race?” We identified the presence of emotional reactions based on treatment due to race using responses to the following question: “Within the past 30 days, have you felt emotionally upset, for example angry, sad, or frustrated, as a result of how you were treated based on your race?”
We based the race/ethnicity groupings on the self-reported socially assigned race. This information was captured using the question: “How do other people usually classify you in this country? Would you say White, Black or African American, Hispanic or Latino, Asian, Native Hawaiian or Other Pacific Islander, American Indian or Alaska Native, or some other group?” Using the responses, we developed four race/ethnicity categories as: White non-Hispanic (WnH), African American non-Hispanic (AAnH), Hispanic, and Other.
Covariates
We identified potential confounding variables for inclusion in the model to represent pre-disposing, enabling, and need factors. The pre-disposing factors included: age, educational level, marital status, and a composite proxy indicator to account for healthy adherer behaviors. We compared the 35-44, 45-54, 55-64, 65-74, 75+ age groups with those in the 18- to 34-year old group (reference).We consolidated marital status categories into married (referent category), not married (“divorced”, “widowed”, “separated”), and never married (“never married”, “a member of an unmarried couple”) categories. For education, we considered ‘did not complete high school’ as the reference category. The composite measure to capture healthy adherer behavior took on a value of 1 if there was any indication of the following behaviors, some of which have been used in prior work27,28: flu shot (past 12 months), mammography (ever), pap test (ever), sigmoidoscopy or colonoscopy (ever), pneumoccocal vaccine (ever). We also included state indicators to identify respondents from each of the four states: Minnesota, Mississippi, New Mexico, and Arizona.
The enabling factors included: insured status, income, employment status, personal physician, and ongoing medical bills. Based on responses to the question about “annual household income from all sources,” we defined income groups as <$15,000; $15,000 to <$25,000; $25,000 to <$35,000; $35,000 to <$50,000; ≥$50,000. The ≥$50,000 group was the reference group. We identified access to a personal physician based on the responses to the question: “Do you have one person you think of as your personal doctor or health care provider?” Individuals who responded “Yes, only one” formed the reference group. We included “more than one personal physician” and “no personal physician” as model covariates. We also included a binary measure of ongoing medical bills based on responses to the question: “Do you currently have any health care bills that are being paid off over time?”
The need factors included: number of unhealthy days based on physical health, number of unhealthy days based on mental health, body mass index. We categorized the number of unhealthy days as zero (reference group), moderate or high. Similar to prior work27 and based on our data distribution, we utilized 15 as the cut point for defining ‘high number of unhealthy days’ and in response to the questions about physical health and mental health. We categorized the respondent’s BMI as normal (reference), overweight or obese. One and a half percent of respondents were underweight and they were grouped with the respondents in the ‘normal’ group.
Analytic Strategy
We utilized descriptive statistics and outcome group comparisons to describe the sample based on predisposing, enabling and need factors. We provided descriptive statistics for the subgroups defined by the Reactions to Race variables in order to provide more information about underlying relationships. We examined bivariate associations between race/ethnicity groups and key enabling and need factors using χ2 tests. We reported unweighted sample totals and weighted proportions for all descriptive results. We utilized the appropriate weighting, sampling unit, and stratifying variables in descriptive analyses and multivariable logistic regression models.29 In post-hoc analyses, we examined the sensitivity of the results to the use of self-reported race instead of self-reported socially assigned race. Statistical analyses were performed using SAS software, version 9.4 (SAS Institute, Inc., Cary, NC).
Following review (HP-00088388), the institutional review board (IRB) of the University of Maryland Baltimore determined that this analysis does not constitute human subjects research and did not require IRB oversight.
Results
After application of the study inclusion criteria, the final study sample included 20,366 respondents (the sampling flowchart is available from the lead author). Twelve percent and 16% of respondents thought frequently or often about their race, while 3% of respondents considered their experience when seeking health care to be worse than people of other races. Three percent of individuals reported physical symptoms because of treatment due to their race while 5% of respondents reported becoming emotionally upset because of treatment due to their race. Table 1 provides descriptive statistics for the study sample and for subgroups defined by selected Reactions to Race measures. We did not include the Reactions to Race item specific to workplace experience due to a high proportion (51%) of missing values. Fifty-one percent of the sample were male and over half of the sample were aged 55 years or younger. The race/ethnicity distribution for the sample was 73%, 8%, 12%, and 6% for WnH, AAnH, Hispanic, and Other, respectively. For comparison purposes, among those who reported experiencing physical symptoms due to treatment based on their race, this proportion was 37%, 19%, 26.5% and 17%. Among those who perceived that their experience seeking health care was worse in comparison to other races, the race/ethnicity proportion was 47%, 18%, 21% and 13.5%. The distribution of respondents according to the state of residence was: Arizona = 37.7%, Minnesota = 34.9%, Mississippi = 15.9%, and New Mexico = 11.5%.
Table 1. Demographics for the full sample and among subgroups defined by Reactions to Race (N=20,366).
| Full Sample | Experienced physical symptomsa because of treatment due to race | Quality of experience while seeking health care, in comparison with other races | ||||||||
| No, N=19,955 | Yes, N=411 | Better or same, N=19,904 | Worse, N=462 | |||||||
| Nb | %c | Nb | %c | Nb | %c | Nb | %c | Nb | %c | |
| Race | ||||||||||
| White | 16552 | 73.3 | 16366 | 74.3 | 186 | 37.2 | 16299 | 74 | 253 | 47.1 |
| African American | 1092 | 8.3 | 1027 | 8 | 65 | 19.2 | 1016 | 8 | 76 | 18.2 |
| Hispanic | 1688 | 12.3 | 1599 | 11.9 | 89 | 26.5 | 1616 | 12.1 | 72 | 21.2 |
| Other | 1034 | 6.1 | 963 | 5.8 | 71 | 17.1 | 973 | 4.7 | 61 | 13.5 |
| Sex | ||||||||||
| Female | 11151 | 49.3 | 10909 | 49.1 | 242 | 56.9 | 10907 | 49.2 | 244 | 53.3 |
| Male | 9215 | 50.7 | 9046 | 50.9 | 169 | 43.1 | 8997 | 50.8 | 218 | 46.7 |
| Age, years | ||||||||||
| 18-34 | 2813 | 27.7 | 2724 | 27.3 | 89 | 41.9 | 2722 | 27.6 | 91 | 32.9 |
| 35 - 44 | 2533 | 17.1 | 2464 | 17 | 69 | 19.2 | 2441 | 17 | 92 | 22 |
| 45 - 54 | 3468 | 17.1 | 3366 | 17.1 | 102 | 17.9 | 3363 | 17 | 105 | 22.3 |
| 55 - 64 | 4496 | 16.8 | 4411 | 16.8 | 85 | 13.6 | 4404 | 16.8 | 92 | 13.6 |
| 65 - 74 | 4268 | 12.9 | 4230 | 13.1 | 38 | 4.5 | 4213 | 13.1 | 55 | 6.1 |
| ≥75 | 2788 | 8.5 | 2760 | 8.6 | 28 | 2.9 | 2761 | 8.6 | 27 | 3.2 |
a. For example, a headache, an upset stomach, tensing of muscles, or a pounding heart.
b. Unweighted frequency.
c. Weighted proportion; column percents.
The descriptive statistics in Table 2 provide information regarding the prevalence of the three outcomes, ie, no physician visit, CRNU_physician visit (ie, did not visit physician due to cost concerns) and CRNU_prescription fill (ie, did not fill prescription due to cost concerns) in the full sample and among baseline factors. In the full sample, 11.4% of the sample did not visit a physician for any reason, CRNU_physician visit was reported for 12.7% of the sample and CRNU_prescription fill was reported for 7.4% of the sample over a 12-month period. The proportion of the sample reporting no physician visit over the 12-month period was highest among those in the Hispanic group (18.7%). Hispanics reported the highest (25.7%) for the CRNU_physician visit outcome. Lastly, the proportion reporting CRNU_prescription fill was highest among AAnH (13.8%).
Table 2. Descriptive statistics for the study sample, stratified by types of non-utilization, N=20,366.
| No physician visit | No physician visit due to cost | No prescription due to cost | ||||
| No | Yes | No | Yes | No | Yes | |
| %a | %a | %a | %a | %a | %a | |
| Full sample | 88.6 | 11.4 | 87.3 | 12.7 | 92.6 | 7.4 |
| Self-reported socially assigned race | ||||||
| White | 90.4 | 9.6 | 90.6 | 9.4 | 94.2 | 5.8 |
| African American | 88.0 | 12.0 | 81.5 | 18.5 | 86.2 | 13.8 |
| Hispanic | 81.3 | 18.7 | 74.3 | 25.7 | 87.1 | 12.9 |
| Other | 82.3 | 17.7 | 81.8 | 18.2 | 92.3 | 7.7 |
| Sex | ||||||
| Female | 92.1 | 7.9 | 85.6 | 14.4 | 91.4 | 8.6 |
| Male | 85.2 | 14.8 | 89.0 | 11.0 | 93.7 | 6.3 |
| Age, years | ||||||
| 18-34 | 82.3 | 17.7 | 82.4 | 17.6 | 90.9 | 9.1 |
| 35 - 44 | 85.3 | 14.7 | 85.6 | 14.4 | 91.7 | 8.3 |
| 45 - 54 | 88.9 | 11.1 | 84.7 | 15.3 | 90.9 | 9.1 |
| 55 - 64 | 92.1 | 7.9 | 89.3 | 10.7 | 92.4 | 7.6 |
| 65 - 74 | 96.3 | 3.7 | 95.2 | 4.8 | 96.2 | 3.8 |
| ≥75 | 96.6 | 3.4 | 96.3 | 3.7 | 97.7 | 2.3 |
| Education | ||||||
| Less than high school | 84.6 | 15.4 | 74.1 | 25.9 | 87.1 | 12.9 |
| High school graduate | 86.0 | 14.0 | 85.5 | 14.5 | 91.7 | 8.3 |
| Some college | 89.1 | 10.9 | 88.2 | 11.8 | 92.8 | 7.2 |
| College | 91.8 | 8.2 | 92.8 | 7.2 | 95.1 | 4.9 |
| Marital status | ||||||
| Married | 90.2 | 9.8 | 90.5 | 9.5 | 94.0 | 6.0 |
| Not married | 90.3 | 9.7 | 84.8 | 15.2 | 89.8 | 10.2 |
| Never married | 83.7 | 16.3 | 82.0 | 18.0 | 91.4 | 8.6 |
| Insurance | ||||||
| Insured | 90.8 | 9.2 | 90.8 | 9.2 | 93.9 | 6.1 |
| Uninsured | 69.6 | 30.4 | 57.3 | 42.7 | 81.5 | 18.5 |
| Income, annual | ||||||
| >$50,000 | 90.8 | 9.2 | 94.6 | 5.4 | 96.7 | 3.3 |
| $35,000 - 50,000 | 87.9 | 12.1 | 88.3 | 11.7 | 93.0 | 7.0 |
| $25,000 - <35,000 | 90.1 | 9.9 | 81.4 | 18.6 | 89.1 | 10.9 |
| $15,000 - <25,000 | 84.6 | 15.4 | 77.2 | 22.8 | 87.2 | 12.8 |
| <$15,000 | 82.8 | 17.2 | 71.5 | 28.5 | 83.1 | 16.9 |
| Health statusb | ||||||
| Excellent - good | 87.9 | 12.1 | 89.3 | 10.7 | 94.3 | 5.7 |
| Fair - poor | 92.9 | 7.1 | 74.6 | 25.4 | 81.5 | 18.5 |
| Medical billsc | ||||||
| No medical bills | 87.6 | 12.4 | 91.2 | 8.8 | 95.3 | 4.7 |
| Medical bills | 92.8 | 7.2 | 71.9 | 28.1 | 81.8 | 18.2 |
a. Weighted proportion; row percent for each outcome
b. Health status: Respondents were asked the following question, “Would you say that in general your health is: (excellent – poor).”
c. Medical bills: Respondents were asked the following question, “Do you currently have any health care bills that are being paid off over time?
The covariate-adjusted odds ratios (AOR) based on the logistic regression model are presented in Table 3 for each of the study outcomes and include pre-disposing, enabling and need factors. We report on enabling factors in the text, given the study hypothesis. Enabling factors include the Reactions to Race measures as well as insured status, income, employment status, personal physician, and ongoing medical bills. Considering the model of no physician visit, the odds of reporting no physician visit during the 12-month period did not differ based on the five Reactions to Race items namely, self-reported socially assigned race, degree of race consciousness, respondent’s perception about the quality of their health care experience compared with other races, physical response due to treatment based on race, or emotional response due to treatment based on race. The AOR of CRNU_physician visit during the 12-month period was 2.59 times higher (95% CI: 1.57-4.26) among respondents who reported that the quality of their health care experience was worse than other races. The AOR of CRNU_physician also was higher (2.58; 1.65-4.03) among those who reported experiencing physical symptoms because of treatment due to their race, compared with those who did not report symptoms. There was also a statistically significant difference (AOR: 1.47; 1.02-2.11) between those who became emotionally upset because of treatment due to race, compared with those who did not.
Table 3. Covariate-adjusted odds ratios from logistic regression models of non-utilization, N=20,366.
| No physician visit | No physician visit due to cost | Did not fill prescription due to cost | |
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Self-reported socially assigned race (ref: White) | |||
| African American | 1.16 (.73, 1.82) | .66 (.48, .92)b | .95 (0.63, 1.43) |
| Hispanic | 1.31 (.90, 1.89) | 1.24 (.88, 1.76) | 1.13 (.78, 1.64) |
| Other | 1.27 (.87, 1.84) | 1.11 (.74, 1.67) | .78 (.47, 1.30) |
| How often you think of your race (ref: hardly) | |||
| Often | .85 (.65, 1.11) | .89 (.68, 1.17) | 1.15 (.87, 1.52) |
| Frequent | .88 (.62, 1.25) | 1.06 (.77, 1.44) | 1.34 (.93, 1.93) |
| Quality of experience while seeking health care, in comparison to other races (ref: same or better) | |||
| Worse | 1.07 (.65, 1.78) | 2.59 (1.57, 4.26) b | 1.52 (.88, 2.61) |
| Physical symptomsa because of treatment due to race (ref: No) | |||
| Yes | 1.16 (.66, 2.03) | 2.58 (1.65, 4.03) b | 2.1 (1.24, 3.58) b |
| Emotionally upset because of treatment due to race (ref: No) | |||
| Yes | .75 (.44, 1.27) | 1.47 (1.02, 2.11) b | 1.37 (.92, 2.04) |
| Insurance status (ref: insured) | |||
| Uninsured | 2.63 (1.98, 3.49) b | 4.02 (3.11, 5.21) b | 1.78 (1.31, 2.41) b |
| Income (ref: >$50,000) | |||
| $35,000 - 50,000 | 1.41 (1.06, 1.87) b | 1.80 (1.32, 2.44) b | 1.94 (1.40, 2.68) b |
| $25,000 - <35,000 | .93 (.62, 1.41) | 3.02 (2.26, 4.04) b | 3.13 (2.15, 4.58) b |
| $15,000 - <25,000 | 1.47 (1.07, 2.01) b | 2.81 (2.07, 3.80) b | 3.07 (2.23, 4.23) b |
| < $15,000 | 1.71 (1.16, 2.52) b | 3.86 (2.68, 5.57) b | 4.38 (2.98, 6.42) b |
| Employment status (ref: employed) | |||
| Not employed | .86 (.67, 1.09) | .87 (.69, 1.11) | .82 (.63, 1.06) |
| No. of personal physicians (ref: 1 physician) | |||
| >1 personal physician | .91 (.61, 1.36) | 1.46 (1.04, 2.05) b | 1.42 (.98, 2.05) |
| No personal physician | 3.62 (2.91, 4.50) b | 1.27 (1.00, 1.62) b | 1.03 (.80, 1.35) |
| Medical bills (ref: no medical bills) | |||
| Medical bills | .45 (.34, .59) b | 3.13 (2.57, 3.82) b | 2.63 (2.38, 3.69) b |
a. For example, a headache, an upset stomach, tensing of muscles, or a pounding heart.
b. Values are statistically significant at an alpha <.05.
Models also included the following covariates: sex, age, education, married status, preventive health services utilization, body mass index, days in poor physical health, days in poor mental health. The results for these covariates are available from the authors upon request.
The odds of CRNU_prescription fill did not differ based on self-reported socially assigned race, degree of race consciousness, or based on the quality of their health care experience. The odds of CRNU_prescription fill were 2.1 (1.24-3.58) times higher among respondents who reported that they experienced physical symptoms because of treatment due to their race compared with those who did not report physical symptoms. Uninsured status was associated with statistically significantly higher odds of non-utilization whether defined as no physician visit (2.63; 1.98 – 3.49), CRNU_physician visit (4.02; 3.11 – 5.21), or CRNU_prescription fill (1.78; 1.31 – 2.41).
Lower annual household income (across all levels) was positively associated with both measures of CRNU. Lower annual household income was statistically significantly associated with no physician visit for most, but not all, income categories. The presence of ongoing medical bills was associated with a statistically significant lower odds of foregoing a physician visit for any reason (.45; .34 – .59). The presence of ongoing medical bills was associated with a statistically significant higher odds of CRNU_physician visit (AOR: 3.13; 2.57 – 3.82) and CRNU_prescription fill (2.63; 2.38 – 3.69).
In post-hoc analysis, we used self-reported race instead of self-reported socially assigned race and found no difference for AAnH or ‘Other’ across the three models. We also found no difference between Hispanic ethnicity and WnH for both CRNU_prescription_fill and NU. For CRNU_physician_visit, the result with self-reported socially assigned Hispanic ethnicity was (OR: 1.24; .88 – 1.76, P=.22) while the result with self-reported Hispanic ethnicity was (OR: 1.35; .98 – 1.87, P=.07).
Discussion
The current study provides a novel look at CRNU using a large sample of respondents to the BRFSS 2014 survey. The BRFSS survey is unique among available surveys in that it provides responses for two measures of CRNU along with responses to Reactions to Race measures. We conceptualized race-based perceptions as an enabling factor because it functions as a facilitator or barrier to health care utilization. If prior experiences with the health care system are positive, the individual may be more likely to engage with the health care system (facilitator role) while the opposite is true (barrier role) if the individual’s experience was negative. Reactions to Race items including the perceived quality of the health care experience, physical symptoms in response to treatment received due to race, and emotional reactions in response to treatment received due to race were used to identify the occurrence of a negative experience.
We hypothesized that enabling factors, including Reactions to Race items, would be more important in models of CRNU compared with a model of general non-utilization (ie, not tied to cost concerns). The regression results provide support for this hypothesis. Specifically, we found that a poorer perception of the quality of their health care experience in comparison with other races was statistically significantly positively associated with CRNU but not with general non-utilization. Studies have examined implicit bias and perceived discrimination in the health care system and found that perceived discrimination was associated with a poorer health care experience (eg, longer wait time, less time with the provider, reduced opportunities for shared decision making) and reduced use of health care services.30
Our results across the three models indicate that reactions to race, as enabling factors, may be uniquely relevant to CRNU outcomes. Furthermore, it suggests that CRNU may not be defined strictly by financial considerations (eg, out-of-pocket expenditures) and may also include economic costs, in particular, opportunity costs. The individual’s negative experiences (eg, worse experience when seeking health care, physical symptoms as the result of treatment due to race) compared with other races may increase the opportunity cost of engagement with the health care system, where opportunity cost is the value (foregone) of the next best alternative available to the individual. A negative perception (or expectation) regarding the quality of the health care experience may increase the value of the next best alternative, eg, seek advice from a trusted relative or secure medications through informal channels.
This study pools data across four states represented in the BRFSS to identify the factors associated with CRNU. To the authors’ knowledge, it represents the largest sample of respondents used to study the relationship between Reactions to Race items and CRNU. Prior work using the Reactions to Race items has examined health outcomes and health services utilization patterns, but not the decision to forego health care services. Using 2012 to 2014 BRFSS for MN, “reports of emotional and physical reactions to perceived discrimination were highest among Spanish-language preference Latinos. Both Spanish- and English-language preference Latinos were more likely to report poor self-rated health in comparison to whites.”27 One study examined perceived discrimination and the use of preventive health services and found that there was no relationship in covariate-adjusted models between negative discrimination and use of preventive services.25 Using 2004 BRFSS, researchers reported that “Hispanics who always thought about their race were 73% (OR = .27; 95% CI: .13-.57) less likely to receive [fecal occult blood testing]”.18 Others, using 2002 and 2004 BRFSS found that “Reactions to race-based treatment did not impact the odds of black women receiving Pap tests or mammograms.”31
The results from prior studies are mixed and focus on general non-utilization. Taken together with our findings using CRNU as an outcome, our results suggest that Reactions to Race items, conceptualized as enabling factors, are more relevant to utilization outcomes that are linked to cost barriers. Our findings suggest that the Gelberg-Andersen framework, as currently conceptualized, may not fully capture all the factors associated with CRNU despite the fact that CRNU is a component of NU. Our study suggests a role for future research to develop foundational constructs as they apply to CRNU among diverse populations. Being conservative, we used socially assigned race as it is correlated with large and statistically significant advantages in health status, regardless of the self-identified race/ethnicity.25 Using the 2014 BRFSS, one study found that, compared with minority patients perceived as such, being perceived as White was protective against workplace discrimination.32 We propose that socially assigned race/ethnicity is an enabling factor because it functions either as a facilitator or barrier, depending on the pre-existing (and evolving) social structures.
Study Limitations
There are a few limitations to consider. This study utilized a cross-sectional design that does not provide a causal interpretation. There may be opportunities for a reverse association since the Reactions to Race items (eg, the items focused on physical or emotional reactions were defined over a 30-day period while the outcome was defined over a 12-month period). However, we feel that the Reactions to Race items as a group, defined within the context of prior actual engagement with the health care system, could more reasonably be used to infer an association with downstream disengagement represented as CRNU as opposed to a situation where disengagement with the health care system leads to engagement. This study was focused on establishing foundational concepts and did not systematically explore interactions among covariates. For example, given prior work33 documenting racism and discrimination at higher income levels among minorities, it will be important to consider interactions between income and Reactions to Race items in future models of CRNU. Lastly, we did not investigate either perceived privilege or positive discrimination while both factors have been associated with health services utilization.34,35
Conclusion
Negative perceptions of reactions to race during the time of health services utilization is positively associated with cost-related non-utilization, ie, foregoing physician visits and prescription fills due to cost. These results suggest important directions for future work related to research (eg, examine additional factors related to race and privilege, test for multi-way and multi-level interactions) and associated tools (eg, surveys that examine race perceptions, out-of-pocket vs opportunity cost, and health).
References
- 1. Obama B. United States Health Care Reform: progress to date and next steps. JAMA. 2016;316(5):525-532. 10.1001/jama.2016.9797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Goldman AL, Woolhandler S, Himmelstein DU, Bor DH, McCormick D. Out-of-pocket spending and premium contributions after implementation of the Affordable Care Act. JAMA Intern Med. 2018;178(3):347-355. 10.1001/jamainternmed.2017.8060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Doshi JA, Li P, Ladage VP, Pettit AR, Taylor EA. Impact of cost sharing on specialty drug utilization and outcomes: a review of the evidence and future directions. Am J Manag Care. 2016;22(3):188-197. [PubMed] [Google Scholar]
- 4. Gleason PP, Starner CI, Gunderson BW, Schafer JA, Sarran HS. Association of prescription abandonment with cost share for high-cost specialty pharmacy medications. J Manag Care Pharm. 2009;15(8):648-658. 10.18553/jmcp.2009.15.8.648 10.18553/jmcp.2009.15.8.648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Heidari P, Cross W, Crawford K Do out-of-pocket costs affect medication adherence in adults with rheumatoid arthritis? A systematic review. Semin Arthritis Rheum. 2018;48(1):12-21. https://doi.org/ 10.1016/j. semarthrit.2017.12.010 PMID:29496225 [DOI] [PubMed]
- 6. Hopson S, Saverno K, Liu LZ, et al. . Impact of out-of-pocket costs on prescription fills among new initiators of biologic therapies for rheumatoid arthritis. J Manag Care Spec Pharm. 2016;22(2):122-130. 10.18553/jmcp.2016.14261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kim YA, Rascati KL, Prasla K, Godley P, Goel N, Dunlop D. Retrospective evaluation of the impact of copayment increases for specialty medications on adherence and persistence in an integrated health maintenance organization system. Clin Ther. 2011;33(5):598-607. 10.1016/j.clinthera.2011.04.021 [DOI] [PubMed] [Google Scholar]
- 8. Kirzinger A, Munana C, Wu B, Brodie M. Data Note: Americans’ Challenges with Health Care Costs. Menlo Park, CA: Henry J. Kaiser Family Foundation; 2019. [Google Scholar]
- 9. Starner CI, Alexander GC, Bowen K, Qiu Y, Wickersham PJ, Gleason PP. Specialty drug coupons lower out-of-pocket costs and may improve adherence at the risk of increasing premiums. Health Aff (Millwood). 2014;33(10):1761-1769. 10.1377/hlthaff.2014.0497 [DOI] [PubMed] [Google Scholar]
- 10. Streeter SB, Schwartzberg L, Husain N, Johnsrud M. Patient and plan characteristics affecting abandonment of oral oncolytic prescriptions. J Oncol Pract. 2011;7(3)(suppl):46s-51s. 10.1200/JOP.2011.000316 10.1200/JOP.2011.000316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1-10. 10.2307/2137284 [DOI] [PubMed] [Google Scholar]
- 12. Andersen RM. National health surveys and the behavioral model of health services use. Med Care. 2008;46(7):647-653. 10.1097/MLR.0b013e31817a835d [DOI] [PubMed] [Google Scholar]
- 13. Bass DM, Noelker LS. The influence of family caregivers on elder’s use of in-home services: an expanded conceptual framework. J Health Soc Behav. 1987;28(2):184-196. 10.2307/2137131 [DOI] [PubMed] [Google Scholar]
- 14. Bradley EH, McGraw SA, Curry L, et al. . Expanding the Andersen model: the role of psychosocial factors in long-term care use. Health Serv Res. 2002;37(5):1221-1242. 10.1111/1475-6773.01053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gelberg L, Andersen RM, Leake BD. The Behavioral Model for Vulnerable Populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000;34(6):1273-1302. [PMC free article] [PubMed] [Google Scholar]
- 16. Ben J, Cormack D, Harris R, Paradies Y. Racism and health service utilisation: A systematic review and meta-analysis. PLoS One. 2017;12(12):e0189900. 10.1371/journal.pone.0189900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Burgess DJ, Ding Y, Hargreaves M, van Ryn M, Phelan S. The association between perceived discrimination and underutilization of needed medical and mental health care in a multi-ethnic community sample. J Health Care Poor Underserved. 2008;19(3):894-911. 10.1353/hpu.0.0063 [DOI] [PubMed] [Google Scholar]
- 18. Crawford ND, Jones CP, Richardson LC. Understanding racial and ethnic disparities in colorectal cancer screening: Behavioral Risk Factor Surveillance System, 2002 and 2004. Ethn Dis. 2010;20(4):359-365. [PubMed] [Google Scholar]
- 19. Rhee TG, Marottoli RA, Van Ness PH, Levy BR. Impact of perceived racism on healthcare access among older minority adults. Am J Prev Med. 2019;56(4):580-585. 10.1016/j.amepre.2018.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Slaughter-Acey JC, Sneed D, Parker L, Keith VM, Lee NL, Misra DP skin tone matters: racial microaggressions and delayed prenatal care. Am J Prev Med. 2019;57(3):321-329. https://doi.org/ 10.1016/j. amepre.2019.04.014 PMID:31353164 [DOI] [PMC free article] [PubMed]
- 21. Oser CB, Bunting AM, Pullen E, Stevens-Watkins D. African American female offender’s use of alternative and traditional health services after re-entry: examining the behavioral model for vulnerable populations. J Health Care Poor Underserved. 2016;27(2A):120-148. 10.1353/hpu.2016.0052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Corbie-Smith G, Thomas SB, Williams MV, Moody-Ayers S. Attitudes and beliefs of African Americans toward participation in medical research. J Gen Intern Med. 1999;14(9):537-546. 10.1046/j.1525-1497.1999.07048.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Centers for Disease Control and Prevention 2014 Summary Data Quality Report with Response Rates. 2015. Last accessed August 31, 2019 from https://www.cdc.gov/brfss/annual_data/annual_2014.html.
- 24. Centers for Disease Control and Prevention 2014Behavioral Risk Factor Surveillance System Survey Questionnaire. Last accessed May 4, 2020 from https://www.cdc.gov/brfss/questionnaires/index.htm
- 25. Jones CP, Truman BI, Elam-Evans LD, et al. . Using “socially assigned race” to probe white advantages in health status. Ethn Dis. 2008;18(4):496-504. [PubMed] [Google Scholar]
- 26. Jones CP. Confronting institutionalized racism. Phylon. 2002;50(1/2):7-22. 10.2307/4149999 [DOI] [Google Scholar]
- 27. White K, Lawrence JA, Cummings JL, Fisk C. Emotional and physical reactions to perceived discrimination, language preference, and health-related quality of life among Latinos and Whites. Qual Life Res. 2019;28(10):2799-2811. 10.1007/s11136-019-02222-9 [DOI] [PubMed] [Google Scholar]
- 28. Zuckerman RB, Tinsley LJ, Hawk H, Cohen B. Perceived reactions to race and health status in the Massachusetts Behavioral Risk Factor Surveillance System Survey. Ethn Dis. 2012;22(4):492-496. [PubMed] [Google Scholar]
- 29. Centers for Disease Control and Prevention Behavioral Risk Factor Surveillance System: Module Data for Analysis for 2014 BRFSS. Technical Appendix 2015. Last accessd May 4, 2020 from https://www.cdc.gov/brfss/annual_data/2014/pdf/2014ModuleAnalysis.pdf.
- 30. Hall WJ, Chapman MV, Lee KM, et al. . Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: A systematic review. Am J Public Health. 2015;105(12):e60-e76. 10.2105/AJPH.2015.302903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Crawford ND, Jones CP, Richardson LC. Understanding the role of reactions to race-based treatment in breast and cervical cancer screening. J Natl Med Assoc. 2008;100(2):188-196. 10.1016/S0027-9684(15)31207-4 [DOI] [PubMed] [Google Scholar]
- 32. Jemal A, Gardiner M, Bloeser K. Perceived race as variable: moderating relationship between perceived discrimination in the workplace and mentally unhealthy days. J Racial Ethn Health Disparities. 2019;6(2):265-272. 10.1007/s40615-018-0521-y [DOI] [PubMed] [Google Scholar]
- 33. Hastert TA. All dollars are not created equal: health disparities persist even among the highest income Americans. Prev Med. 2017;96:154-155. https://doi.org/ 10.1016/j ypmed.2016.10.008 PMID:27729260 [DOI] [PubMed]
- 34. Hausmann LR, Jeong K, Bost JE, Ibrahim SA. Perceived discrimination in health care and use of preventive health services. J Gen Intern Med. 2008;23(10):1679-1684. 10.1007/s11606-008-0730-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Stepanikova I, Oates GR Perceived discrimination and privilege in health care: the role of socioeconomic status and race. Am J Prev Med. 2017;52(1S1):S86-S94. https://doi. org/ 10.1016/j.amepre.2016.09.024. [DOI] [PMC free article] [PubMed]


