Abstract
A number of studies have evaluated the variable courses of facial artery. However, the results of these differed substantially from each other so not consistent relationships have yet been established. There has also yet to be a relevant study using conventional angiography.
We assessed the variant branching pattern of the facial artery and its branches using conventional angiography.
Two radiologists retrospectively reviewed 284 cases of angiographies of the external carotid artery in 198 patients. The courses of the facial artery and infraorbital branch of the maxillary artery were classified into 4 types and 2 types, according to the end branch.
Among 284 cases of facial artery, type 1 (angular branch) made up 104 cases (36.6%), type 2 (lateral nasal branch) made up 138 cases (48.6%), type 3 (superior labial branch) made up 24 cases (8.5%), and type 4 (inferior labial branch) made up 18 cases (6.3%).
Regarding the 284 total cases of maxillary artery, 163 cases (57.4%) had anastomosis with the angular artery or extended to the territory of the angular artery. In addition, 121 cases (42.6%) had nothing done in regard to the angular artery.
The results may be helpful for avoiding complications related to facial and maxillary arteries during facial surgeries and cosmetic procedures.
Keywords: facial artery, infraorbital artery, maxillary artery
1. Introduction
As interest in physical appearance continues to grow, the demand for cosmetic procedures has rapidly increased. In the field of dermatology, dermal filler injection and neurotoxin injection are generally performed for facial contouring and rejuvenation as a minimally invasive method.[1,2] As the number of these cosmetic procedures performed has increased, several complications have been reported. In particular, tissue necrosis due to direct arterial occlusion by the injected filler particles is the most severe associated side effect.[3]
The main blood supply of the face is provided by the facial, transverse facial, and infraorbital arteries.[4] Among them, the facial artery plays a major role in supplying blood to the face.[5] Unfortunately, facial artery has different interindividual variations. Previous studies, most of which were limited to cadaveric studies, showed discrepancies between each other in the proportion of branches of the facial artery, especially in the angular branch.[6–14] Understanding the detailed anatomy of the facial artery is very important for performing facial surgery or cosmetic procedure in terms of avoiding complications associated with the facial artery.[1,2,12] Another artery, the infraorbital artery, is derived from the maxillary artery and supplies the infraorbital area of the face.[4] The infraorbital artery also shows variations in its end branch and anastomosis with the angular branch of the facial artery or the distal ophthalmic artery.[4,15] Additional knowledge of variations in the infraorbital artery will also be helpful to understanding the arterial supply of the face and to minimizing complications during facial surgery and cosmetic procedures.[16–18]
In this study, conventional angiography was used as evaluation tool for the assessment of variations of the facial and infraorbital artery. Conventional angiography is the gold standard for evaluating small vascular anatomy and related diseases because of its excellent depiction of vascular anatomy and its excellent spatial resolution.[19,20] In addition, because angiography occurs in real time, the operator can evaluate the dominant artery of the vessel territory during the procedure.[13] Digital subtraction angiography technique of conventional angiography also overcomes metal artifact compared with ultrasonography and CT angiography. Most importantly, this is the first study assessing the variant branching pattern of the facial artery and its branches using conventional angiography.
2. Methods
The institutional review board approved this study (IRB number: 2019–09–013–001), and the requirement for informed consent was waived because of the retrospective study design. From January 2008 to August 2018, the facial and infraorbital arterial anatomies were analyzed in patients who underwent external carotid angiography for the evaluation of cerebral vascular malformation, congenital anomaly, or intra-arterial procedures such as cerebral arterial thrombolysis, internal carotid arterial stent graft, brain tumoral embolization, and coil embolization of the cerebral arterial aneurysm at the Gyeongsang National University Hospital (center A) and Gyeongsang National University Changwon Hospital (center B). Biplane angiography (Artis Zee Biplane; Siemens, Erlangen, Germany or Allura Xper; Philips Healthcare, Best, The Netherlands) was used for external carotid angiography.
2.1. Patient
A total of 268 patients underwent external carotid angiography. Among them, 224 patients underwent angiography in center A and 44 patients did in center B. Seventy patients were excluded from analysis because the qualities of their images were too poor to evaluate the anatomy of the facial or infraorbital arteries, and their images did not include enough field to properly discriminate the types of the facial and infraorbital arteries. For 86 of the remaining 198 patients, external carotid angiography was performed bilaterally. Thus, a total of 284 external carotid angiographies which showed intact facial arteries without any abnormalities were obtained in 198 patients (Fig. 1).
Figure 1.

Flowchart of the selected cases.
2.2. Image analysis
Two radiologists (S.E. Park and S.J. Hong) retrospectively reviewed the external carotid angiographies. Two reviewers made the final decisions by consensus for discordant cases. The courses of the facial artery were classified into 4 types (Fig. 2A–F) according to the final branch: Type 1, facial artery that has angular branch beyond the midline of the orbit for its final branch (Fig. 3); Type 2, facial artery that has lateral nasal artery with or without alar branch for its final branch (Fig. 4); Type 3, facial artery that has superior labial branch for its final branch (Fig. 5); Type 4, facial artery that has only inferior labial branch (Fig. 6). We further classified type 1 facial arteries into type 1a, 1b, and 1c: Type 1a, angular branch running along only the conventional course without supratrochlear branch or duplex of the angular artery; Type 1b, angular branch that has supratrochlear branch extending to the frontal bone (Fig. 7); Type 1c, angular branch that is divided into 2 angular arteries (duplex) at proximal facial artery (Fig. 8).
Figure 2.

Types of facial artery (A-F) and infraorbital artery (G, H) according to the final branching pattern.
Figure 3.

Angiography of the external carotid artery in a 43-year-old female with cerebral infarction: AP view (A) and lateral view (B). Angular (black arrow) branch of the facial artery is seen without duplex or supratrochlear branch. This facial artery was classified as type 1a.
Figure 4.

Angiography of the external carotid artery in a 39-year-old female with moyamoya disease: AP view (A) and lateral view (B). Lateral nasal branch (black arrow) of the facial artery is seen without angular branch, classified as type 2.
Figure 5.

Angiography of the external carotid artery in a 38-year-old female for evaluating carotid cavernous fistula: AP view (A) and lateral view (B). Superior labial branch (black arrow) of the facial artery is the end branch in this patient, classified as type 3.
Figure 6.

Angiography of the external carotid artery in a 55-year-old female with dural arteriovenous fistula: AP view (A) and lateral view (B). Only inferior labial artery branches (black arrow) of the facial artery are seen, without other branches, classified as type 4.
Figure 7.
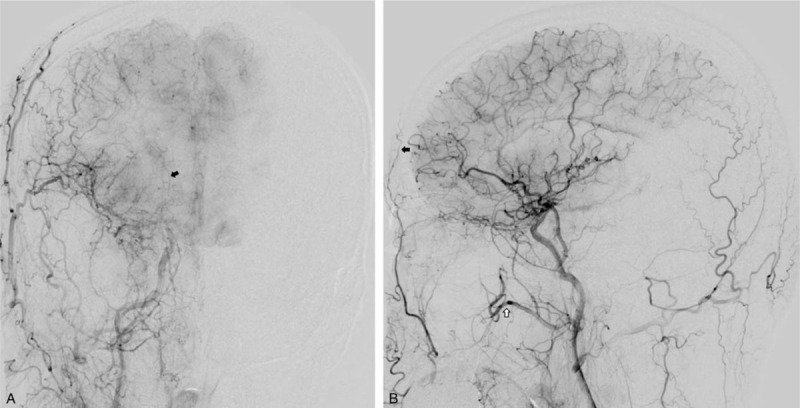
Angiography of the external carotid artery in a 53-year-old male with cerebral infarction: AP view (A) and lateral view (B). Supratrochlear branch of the angular artery (black arrow) extends to the frontal bone, classified as type 1b. The infraorbital artery (white arrow) ends before reaching the territory of the angular artery, classified as type 2.
Figure 8.

Angiography of the external carotid artery in a 61-year-old female for evaluating spontaneous intracranial hemorrhage: AP view (A) and lateral view (B). Duplex of the angular artery (black arrow) is separated from the lateral nasal branch of the facial artery (white arrow), classified as type 1c.
We also characterized the symmetry of the facial artery. Having the same type of facial artery bilaterally was regarded as having symmetric pattern and having arteries of different types is regarded as having asymmetric pattern.
We additionally classified the courses of infraorbital artery into 2 types (Fig. 2G, H): Type A, infraorbital artery that anastomoses with the angular artery or extends to the anterior portion of the orbit, which is the territory of the angular artery (Fig. 9); Type B, infraorbital artery that does not anastomose with angular branch and terminates before extending to the territory of the angular artery (Fig. 7B).
Figure 9.

Angiography of the external carotid artery in a 69-year-old male with moyamoya disease: AP view (A) and lateral view (B). Maxillary artery shows infraorbital branch extending to the territory of the angular artery (black arrow), classified as type 2.
3. Results
3.1. Facial artery
The branching pattern of the facial artery is shown in Table 1. Of the 284 cases of facial arteries in 198 patients, 104 cases (36.6%) were classified as type 1, which were facial arteries that terminated at the angular branch. Another 138 cases (48.6%) were classified as type 2, which were facial arteries that terminated at the lateral nasal artery, with or without alar branch. Still, 24 cases (8.5%) were type 3, which terminated at the superior labial branch, while 18 cases (6.3%) had only inferior labial branch and were thus classified as type 4. Among the 104 cases of type 1 facial artery, 34 cases (12.0%) had supratrochlear branch (type 1b) that extended to the frontal bone, and 14 cases (4.9%) had duplex of the angular artery (type 1c). The rest, total of 56 cases (19.7%), had the conventional course of the angular artery (type 1a) without supratrochlear branch or duplex of the angular artery.
Table 1.
Branching patterns of the facial artery.

Eighty six patients underwent bilateral external carotid angiography. Of these 86 patients, 60 patients (69.8%) had symmetric types of facial arteries and 26 patients (30.2%) had asymmetric types. Of the symmetric types, 19 cases (31.7%) were type 1, 34 cases (56.7%) were type 2, 5 cases (8.3%) were type 3, and 2 cases (3.3%) were type 4.
3.2. Infraorbital artery
Of the 284 cases of infraorbital artery, 163 cases (57.4%) were classified as type A, which had anastomosis with the angular artery or extended to the territory of the angular artery (Fig. 2G). In addition, 121 cases (42.6%) were classified as type B, or as having nothing to do with the angular artery (Fig. 2H, Table 2).
Table 2.
Anastomosis patterns of the infraorbital branch of the maxillary artery.

4. Discussion
As the frequency of cosmetic procedures increases, complications that range from temporary and mild to permanent and severe have been reported, including erythema, bruising, local swelling, infection, nodular masses, tissue necrosis, and even visual loss due to direct arterial occlusion by the injected filler particles.[16,21] (Visual loss has been identified to occur due to the mechanism of retrograde arterial occlusion into the ophthalmic artery from the supratrochlear or dorsal nasal artery.[22,23]) To minimize the risk of complications, physicians need to know detailed anatomy such as exact course, location, and variation of the facial artery before performing any cosmetic procedures.[1,2] Although there have been many previous studies on the detailed anatomy of the facial artery regarding its course and location, the results significantly differ from each other and consensus is yet to be established.[1] Additionally, most of these studies are limited as they are cadaveric studies.[6–12]
A comparison of the branching patterns of the facial artery indicated by previous studies is shown in Table 3. In 1960, Aratani et al[6] studied branching distributions of the facial artery in Japan and found that the facial artery ended as the angular artery in 15.8% and as the lateral nasal artery in 64.4%. Afterwards, Mitz et al[7] conducted similar research through dissection of adult French cadavers. According to this research, the facial artery ended as the angular artery only in 4% and as the lateral nasal artery in 78%. Contrastingly, Niranjan et al,[8] who conducted relevant research using British specimens, reported that the facial artery ended as the angular artery in 68% of cases and as the lateral nasal artery in 26% of cases. In 2003, Koh et al[9] conducted cadaveric study using Korean specimens that found that 40.7% of arteries terminated as the angular artery and 44% as the lateral nasal artery. Pinar, Loukas, and Lohn et al[10–12] also studied variations in the branching distribution of the facial artery and all found that the ratio of facial artery that ended as the angular artery was 22%, 51.3%, and 20%, respectively.
Table 3.
Comparison of the branching pattern of facial artery in previous studies.

There are several possible causes of the significant variations in facial artery anatomy among the previous studies. Previously, these discrepancies were considered to be due to racial differences.[24] However, the diverse patterns of the facial artery distribution did not reflect racial differences because it had been found that the distribution pattern of the facial artery of Koreans and Japanese, both mongoloids, was quite different.[9] However, the results of this study were similar to those of Koh et al, using the same Korean specimen compared to other Japanese, French, and British studies. Apart from racial differences, we also speculate about the possibility that the environmental aspects of lifestyles have an effect. In addition, our angiography-based study is technically different from the previous studies using cadaveric dissection. The cadaveric study is static and limited to surface anatomy, while angiography-based study is the method of viewing the enhanced inner lumen of the artery through intravenous injection of contrast agent.[13] Therefore angiography could detect superficial and deep branches of the artery and contrast reveals small vessels which have too small diameter to distinguish with the naked eye. Anatomic cadaver dissection cannot accurately reflect physiologic blood flow and vascular status. During liquid dye injection, vessel occlusion due to existing clots or air bubbles may not correspond. In addition, the force of the injection can change the vessel diameter, and the findings can also be altered due to the thickness of the liquid dye.[23]
In 2013, Furukawa et al[13] evaluated the branch of facial artery using noninvasive imaging tool, computed tomographic angiography, and the results were significantly different from those of the existing cadaveric studies. The proportion of the facial artery that ended as the angular branch including the lateral nasal branch was relatively low (26.1%), while 73.8% terminated as the superior and inferior labial branches, which was much higher than that indicated by any previous studies. In 2019, Mateusz et al[14] studied similar research using computed tomographic angiography. In this study, proportion of the facial artery terminated as the angular branch is higher (44.0%) than that of Furukawa et al and lower percentage (56.1%) of the facial arteries ended as the superior and inferior labial branches.
Different proportion of type of facial artery between this article and the researches using CT angiography is due to different classification. Furukawa et al[13] and Mateusz et al[14] did not separate lateral nasal artery but counted it with angular branch while current study separated lateral nasal artery from angular branch as previous cadaveric studies did.[6–12] And this variation could be affected by the different sensitivities and specificities for evaluating peripheral vessels between conventional angiography and CT angiography.[25,26] Because of the higher accuracy and spatial resolution for detecting peripheral vessel diseases in conventional angiography compared to CT angiography, conventional angiography has been used as reference standard in the assessment of peripheral vessels with variable radiologic tools including CT angiography.[13,25–27]
Most the previous studies had simultaneously studied the symmetry of the facial artery. Sixty eight percent were found to be symmetrical in study by Niranjan et al and Pinar et al, and 54.5%, 53%, and 52.7% were found to be symmetrical in Koh et al, Lohn et al, and Furukawa et al, respectively. In our specimens, symmetric distribution of the facial artery was observed similarly, in 69.8% of cases. In Kohs study, 50% of the symmetric facial arteries ended as angular artery and 45.8% ended as lateral nasal artery. In the case of asymmetry, it was most common that 1 side ended with lateral nasal artery and the other side ended with superior labial artery. In the cases of asymmetric facial arteries, the most common case ended as lateral nasal artery with contralateral superior labial artery on the other side. These results are consistent with the findings of Lohn et al, suggesting that individual developmental differences might have affected the patterns of facial arteries.[9,12]
The maxillary artery and its branches mainly supply arterial blood to various soft tissue organs and muscles in the head and neck.[15] Some branches, infraorbital and masseter branches, sometimes anastomose with the angular branch of the facial artery.[28] In addition, the infraorbital branch of the maxillary artery is occasionally connected to the distal ophthalmic artery.[29] In our study, 163 cases (57.4%) of infraorbital branch in the maxillary artery share supplying territory or anastomose with the angular artery among the 284 cases of external carotid angiography. In this type of the infraorbital branch partially compensated blood supply from the maxillary artery could be expected under the situation in which the facial artery is injured during procedure such as dermal filler injection. On the other hand, the infraorbital branch of the maxillary artery can be potential route causing ophthalmic artery occlusion by dermal filler particles.[30] Furthermore, because there is differential variation in the angular artery itself, not only the infraorbital area but also the angular area could be dangerous zones of ophthalmic artery occlusion through variable anastomotic sites of the facial artery with retrograde flow.[22,23,31]
This study had 2 limitations. First, this study used retrospective design. Second, readers may not have been able to detect very small-sized vessels which were not supplied with enough contrast media from the facial artery. However, sufficient performance time of angiography, carried out until the venous phase when the operator can see the draining veins of the external carotid artery, could minimize the underestimation of these results.
In conclusion, we performed the first study to identify variant branching patterns of facial and maxillary artery using conventional angiography, and obtained meaningful results. These data will help physicians avoid severe vascular complications during procedures. In addition, we believe that this study becomes a cornerstone for artery research using various tools such as color Doppler ultrasonography and MRI, as well as CT angiography in the future.
Acknowledgments
The authors would like to thank “Harrisco Language Editing Service” for the English language review and editing; http://www.harrisco.net.
Author contributions
All authors have reviewed and approved the final version of the manuscript.
Conceptualization: Seok Jin Hong, Sung Eun Park, Do Seon Jeong.
Data curation: Seok Jin Hong, Sung Eun Park, Dae Seob Choi.
Formal analysis: Seok Jin Hong, Sung Eun Park, Jeong Won, Dae Seob Choi, Minhee Hwang.
Investigation: Seok Jin Hong, Dae Seob Choi.
Methodology: Seok Jin Hong, Sung Eun Park, Do Seon Jeong, Minhee Hwang, Chi Yeon Kim.
Project administration: Seok Jin Hong, Do Seon Jeong.
Resources: Seok Jin Hong, Dae Seob Choi.
Software: Seok Jin Hong.
Supervision: Sung Eun Park, Jeong Won, Do Seon Jeong, Dae Seob Choi, Chi Yeon Kim.
Validation: Seok Jin Hong, Dae Seob Choi.
Visualization: Seok Jin Hong, Jung Ho Won.
Writing – original draft: Seok Jin Hong, Jeong Won.
Writing – review & editing: Seok Jin Hong, Sung Eun Park, Do Seon Jeong, Dae Seob Choi, Jung Ho Won, Minhee Hwang, Chi Yeon Kim.
Footnotes
Abbreviations: CT = computed tomography, MRI = magnetic resonance imaging.
How to cite this article: Hong SJ, Park SE, Jo JW, Jeong DS, Choi DS, Won JH, Hwang M, Kim CY. Variant facial artery anatomy revisited: Conventional angiography performed in 284 cases. Medicine. 2020;99:28(e21048).
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
The institutional review board approved this study (IRB file No. 2019-09-013-001).
The authors have declared that no competing interests exist.
The authors received no specific funding for this work.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- [1].Kim SK. New anatomical insights on the course and branching patterns of the facial artery: clinical implications of injectable treatments to the nasolabial fold and nasojugal groove. Plast Reconstr Surg 2014;134:847e–8e. [DOI] [PubMed] [Google Scholar]
- [2].Phumyoo T, Tansatit T, Rachkeaw N. The soft tissue landmarks to avoid injury to the facial artery during filler and neurotoxin injection at the nasolabial region. J Craniofac Surg 2014;25:1885–9. [DOI] [PubMed] [Google Scholar]
- [3].Lee SH, Gil YC, Choi YJ, et al. Topographic anatomy of the superior labial artery for dermal filler injection. Plast Reconstr Surg 2015;135:445–50. [DOI] [PubMed] [Google Scholar]
- [4].Soikkonen K, Wolf J, Hietanen J, et al. Three main arteries of the face and their tortuosity. Br J Oral Maxillofac Surg 1991;29:395–8. [DOI] [PubMed] [Google Scholar]
- [5].Lasjaunias P, Berenstein A, Doyon D. Normal functional anatomy of the facial artery. Radiology 1979;133:631–8. [DOI] [PubMed] [Google Scholar]
- [6].Aratani R. Anatomical study of the external carotid artery of Japanese. Oral Anat Res 1960;15:145–64. [Google Scholar]
- [7].Mitz V, Ricbourg B, Lassau J. Les branches faciales de l’artère faciale chez l’adulte. typologie, variations et territoires cutanés respectifs. Ann Chir Plast 1973;18:339–50. [PubMed] [Google Scholar]
- [8].Niranjan NS. An anatomical study of the facial artery. Ann Plast Surg 1988;21:14–22. [DOI] [PubMed] [Google Scholar]
- [9].Koh K, Kim H, Oh C, et al. Branching patterns and symmetry of the course of the facial artery in koreans. Int J Oral Maxillofac Surg 2003;32:414–8. [DOI] [PubMed] [Google Scholar]
- [10].Pinar YA, Bilge O, Govsa F. Anatomic study of the blood supply of perioral region. Clin Anat 2005;18:330–9. [DOI] [PubMed] [Google Scholar]
- [11].Loukas M, Hullett J, Louis RG, et al. A detailed observation of variations of the facial artery, with emphasis on the superior labial artery. Surg Radiol Anat 2006;28:316–24. [DOI] [PubMed] [Google Scholar]
- [12].Lohn JW, Penn JW, Norton J, et al. The course and variation of the facial artery and vein: Implications for facial transplantation and facial surgery. Ann Plast Surg 2011;67:184–8. [DOI] [PubMed] [Google Scholar]
- [13].Furukawa M, Mathes DW, Anzai Y. Evaluation of the facial artery on computed tomographic angiography using 64-slice multidetector computed tomography: implications for facial reconstruction in plastic surgery. Plast Reconstr Surg 2013;131:526–35. [DOI] [PubMed] [Google Scholar]
- [14].Mateusz K, Marek T, Mateusz H, et al. Anatomical map of the facial artery for facial reconstruction and aesthetic procedures. Aesthet Surg J 2019;39:1151–62. 15. [DOI] [PubMed] [Google Scholar]
- [15].William Allen, E. Leon Kier, Stephen LG Rothman. The maxillary artery: normal arteriographic anatomy. Am J Roentgenol 1973;118:517–27. [DOI] [PubMed] [Google Scholar]
- [16].Cohen JL. Understanding, avoiding, and managing dermal filler complications. Dermatol Surg 2008;34. [DOI] [PubMed] [Google Scholar]
- [17].Hirsch RJ, Carruthers JD, Carruthers A. Infraorbital hollow treatment by dermal fillers. Dermatol Surg 2007;33:1116–9. [DOI] [PubMed] [Google Scholar]
- [18].Grunebaum LD, Allemann IB, Dayan S, et al. The risk of alar necrosis associated with dermal filler injection. Dermatol Surg 2009;35:1635–40. [DOI] [PubMed] [Google Scholar]
- [19].Sugahara T, Korogi Y, Nakashima K, et al. Comparison of 2D and 3D digital subtraction angiography in evaluation of intracranial aneurysms. AJNR Am J Neuroradiol 2002;23:1545–52. [PMC free article] [PubMed] [Google Scholar]
- [20].Firouzian A, Manniesing R, Flach ZH, et al. Intracranial aneurysm segmentation in 3D CT angiography: method and quantitative validation with and without prior noise filtering. Eur J Radiol 2011;79:299–304. [DOI] [PubMed] [Google Scholar]
- [21].Daines SM, Williams EF. Complications associated with injectable soft-tissue fillers: a 5-year retrospective review. JAMA Facial Plast Surg 2013;15:226–31. [DOI] [PubMed] [Google Scholar]
- [22].Carle MV, Roe R, Novack R, et al. Cosmetic facial fillers and severe vision loss. JAMA Ophalmo 2014;132:637–9. [DOI] [PubMed] [Google Scholar]
- [23].Saban Y, Amodeo CA, Bouaziz D, et al. Nasal arterial vasculature: medical and surgical applications. Arch Facial Plast Surg 2012;14:429–36. [DOI] [PubMed] [Google Scholar]
- [24].Nakajima H, Imanishi N, Aiso S. Facial artery in the upper lip and nose: anatomy and a clinical application. Plast Reconstr Surg 2002;109:855–61. [DOI] [PubMed] [Google Scholar]
- [25].Bash S, Villablanca JP, Jahan R, et al. Intracranial vascular stenosis and occlusive disease: evaluation with CT angiography, MR angiography, and digital subtraction angiography. AJNR Am J Neuroradiol 2005;26:1012–21. [PMC free article] [PubMed] [Google Scholar]
- [26].Kaatee R, Beek FJ, de Lange EE, et al. Renal artery stenosis: detection and quantification with spiral CT angiography versus optimized digital subtraction angiography. Radiology 1997;205:121–7. [DOI] [PubMed] [Google Scholar]
- [27].Willmann JK, Baumert B, Schertler T, et al. Aortoiliac and lower extremity arteries assessed with 16–detector row CT angiography: Prospective comparison with digital subtraction angiography. Radiology 2005;236:1083–93. [DOI] [PubMed] [Google Scholar]
- [28].Tanoue S, Kiyosue H, Mori H, et al. Maxillary artery: functional and imaging anatomy for safe and effective transcatheter treatment. Radiographics 2013;33:e209–24. [DOI] [PubMed] [Google Scholar]
- [29].Geibprasert S, Pongpech S, Armstrong D, et al. Dangerous extracranial-intracranial anastomoses and supply to the cranial nerves: vessels the neurointerventionalist needs to know. AJNR Am J Neuroradiol 2009;30:1459–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Cohen E, Yatziv Y, Leibovitch I, et al. A case report of ophthalmic artery emboli secondary to calcium hydroxylapatite filler injection for nose augmentation-long-term outcome. BMC Ophthalmol 2016;16:98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Lee JG, Yang HM, Choi YJ, et al. Facial arterial depth and relationship with the facial musculature layer. Plast Reconstr Surg 2015;135:437–44. [DOI] [PubMed] [Google Scholar]


