Abstract
Context:
Endotracheal intubation of pediatric patients is challenging, especially in the pre-hospital emergency setting and if performed by less experienced providers. Securing an airway should be achieved with a single intubation attempt, as each intubation attempt contributes to morbidity and mortality. A new airway device, the VieScope, was recently introduced into clinical market, but efficacy to reduced intubation attempts remains unclear thus far.
Objective:
We aimed to compare endotracheal intubation by paramedics using the Vie Scope in different pediatric airway simulation conditions.
Methods:
We conducted a randomized, cross-over simulation study. Following a theoretical and practical training session, paramedics performed endotracheal intubation in 3 different pediatric emergency scenarios: normal airway; tongue edema; cardiopulmonary resuscitation using the VieScope. Overall intubation success rate was the primary outcome. Secondary outcomes included number of intubation attempts, time to intubation, Cormack-Lehane grade, POGO score, and ease of use (using 1–100 scale).
Results:
Fifty-five paramedics with at least 2 years of clinical experience and without any previous experience with the VieScope participated in this study. The overall intubation success rate was 100% in all 3 scenarios. The median intubation time was 27 (24–34) versus 27 (25–37) versus 29 (25–40) s for scenarios A, B, and C, respectively. In scenario A, all paramedics performed successful intubation with 1 single intubation attempt, whereas 2% of the paramedics had to perform 2 intubation attempts in scenario B and 9% in scenario C.
Conclusions:
Results of this simulation study indicate preliminary evidence, that the VieScope enables adequate endotracheal intubation in the pediatric setting. Further clinical studies are needed to confirm these results.
Keywords: airway management, pediatric, endotracheal intubation, medical simulation, paramedic
1. Introduction
Securing the airway is a fundamental skill in the treatment of critically ill or injured patients.[1,2] Endotracheal intubation is widely considered the standard of care but requires high level of experience and regular re-training.[3,4] The out-of-hospital emergency setting is even more challenging, especially if dealing with pediatric patients. Unanticipated difficulties during endotracheal intubation has been reported in up to 25% in pediatric and up to 10% in adult patients.[3,5–7] Difficulties during endotracheal intubation is critical, as prolonged and/ or multiple intubation attempts are clearly associated with potentially deleterious consequences like desaturation, bradycardia or even death.[8,9]
Videolaryngoscopy was introduced into clinical practice to ultimately ease endotracheal intubation more than a decade ago. Videolaryngoscopy is considered an acceptable alternate technique compared to direct laryngoscopy, but clinical evidence is mostly based on clinical studies performed in adult patients.[10–12] Results of studies performed in adults cannot extrapolate into the pediatric population, as pediatric patients are much more challenging due to their more challenging airway anatomy and physiology.[13,14] Videolaryngoscopy in pediatric patients is generally believed to provide favorable airway visualization, but it remains unclear whether better visualization reduces intubation failures or reduces time to intubation.[15,16]
Airway management in the pediatric out-of-hospital emergency setting is challenging, especially if performed by relatively unexperienced airway providers like paramedics.[4,10,17] Airway assistance tools like bougies have been reported to be beneficial, especially if used by paramedics.[18] Once the bougie is placed between the vocal cord, an endotracheal tube can be inserted via the bougie into the trachea. Although placement of the bougie is considered easier than endotracheal intubation, it is still sometimes challenging, mostly due to limited airway visualization. A newly developed airway device, called VieScope (Adroit Surgery, Oklahoma City, OK), was introduced into clinical market to combine the advantages of better airway visualization and introducing a bougie into the patient's airway. The VieScope is a self-contained, battery powered, disposable scope. The VieScope takes advantage of a closed circular tube with a beveled end to visualize the vocal cords. Light is transmitted through the side wall of the tube from end to end as well as within the lumen. Hereby, visualization of the target tissue should be optimized by reducing the chance of light obstruction by secretions or blood. Endotracheal intubation by the VieScope involves a 2-step process. First, the device is inserted orally and visualizing of glottis through the clear cylindrical lumen of the intubation channel is obtained. Second, a bougie is inserted into patient's trachea and the VieScope removed. Afterwards, a conventional endotracheal tube is railroaded over the bougie. Once the endotracheal tube is placed, the bougie is removed.
The aim of this study was to identify potential advantages of using the VieScope for intubation of pediatric patients. Specifically, we tested the clinical efficacy of the VieScope for endotracheal intubation during 3 different airway scenarios in a pediatric manikin setting.
2. Methods
This study was designed as a randomized, cross-over simulation study. This manuscript reports in accordance with the CONsolidated Standards of Reporting Trials (CONSORT) statement.[19] The study protocol was approved by the Institutional Review Board of the Polish Society of Disaster Medicine (Approval no.: 21.08.2019.IRB). Paramedics with at least 2 years of experience in the out-of-hospital emergency setting were invited to participate in this study. Paramedics with less experience or any previous training in the VieScope were excluded. Written voluntary informed consent was obtained from each paramedic before the study.
2.1. Study design
All paramedics completed a brief questionnaire consisting of demographic information and prior clinical experience with any kind of laryngoscopes including VieScope (Table 1). All paramedics attended a 30-minute lasting lecture, covering basic principles of endotracheal intubation of pediatric patients and the modified intubation technique using the VieScope laryngoscope (Fig. 1).
Table 1.
Baseline characteristics.
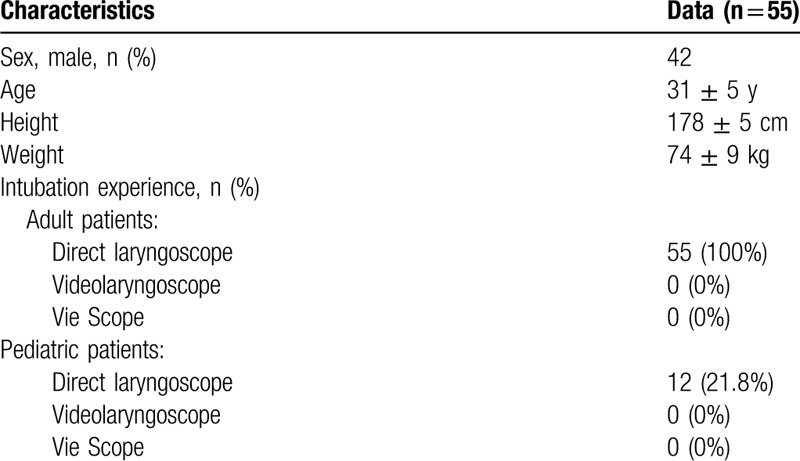
Figure 1.

Vie Scope laryngoscope.
After the lecture, all paramedics had a 10-minute practice period to familiarize themselves with the VieScope and perform endotracheal intubation on the Laerdal Airway Management Trainer (Laerdal, Stavanger, Norway). Once the training was completed, paramedics were guided to a separate testing area. The Pediatric HAL S3005 Advanced Simulator (Gaumard, Miami, FL), representing a 5-year-old child, was used to simulate the pediatric patient. The simulator was placed on a flat floor in neutral position. Paramedics were asked to perform endotracheal intubation using the VieScope in 3 separate airway scenarios in a randomized sequence using the Research Randomizer program (Fig. 2):
Figure 2.
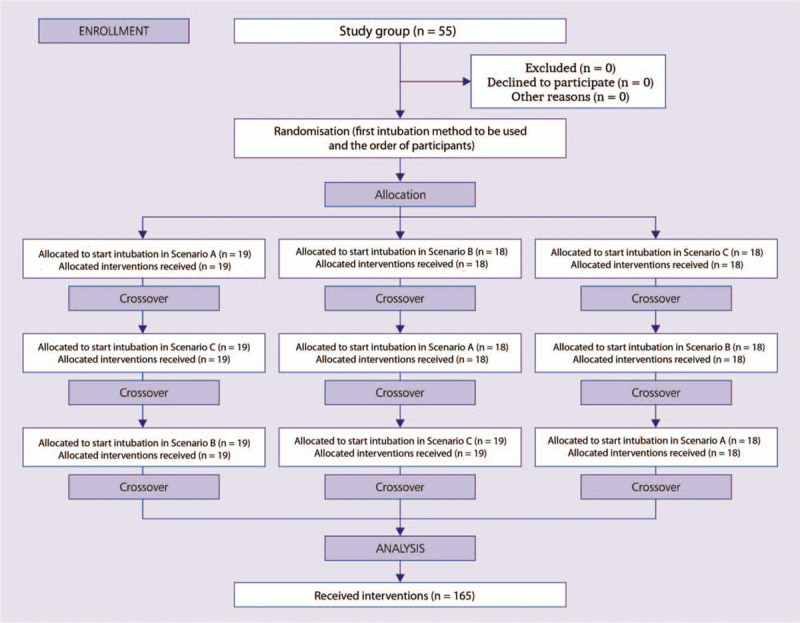
Randomization flow chart.
Scenario A—Normal airway scenario.
Scenario B—Tongue edema: The tongue edema was simulated by inflating the tongue using the simulator's software.
Scenario C—Cardiopulmonary resuscitation (CPR): endotracheal intubation was performed during ongoing external chest compression. To standardize the chest compressions, the mechanical chest compression system LUCAS3 was used (Stryker, Richmond, VA).
Once intubation was achieved, an anesthesia bag (producer) was connected with the endotracheal tube and a breath was given.
In adult patients, a bougie size 15Fr is primarily used with VieScope. For this study, the guide was replaced by a smaller diameter (mean 3.3 mm–10CH) guide adapted to the pediatric size of the endotracheal intubation tubes.
Each airway scenario was limited to a maximum of 60 seconds up to 3 intubation attempts. Between each airway scenarios, paramedics were having a break lasting for 20 minutes.
2.2. Measurements
The primary endpoint of the study was success rate of intubation. Successful intubation was confirmed by adequate ventilation of the lungs using the manikin software.
Time to intubation, defined as the time between insertion of the VieScope between the teeth until successful manual ventilation of the manikin's lungs, and number of intubation attempts served as the secondary outcomes. Additionally, after each attempt, paramedics were asked to rate airway visualization according to the Cormack-Lehane classification and the percentage of glottic opening (POGO) view.[20] A 100% POGO score indicates visualization of entire glottis from the anterior commissure to the interarytenoid notch. A POGO score of 0 indicates that the interarytenoid notch cannot be visualized. Ease of use was assessed with a visual analogue scale score ranging 1 to 100, where 1 meant “extremely easy" and 100 stood for “extremely difficult."
2.3. Statistical analysis
Sample size was calculated with G∗Power 3.1 using a 2-tailed t test. A minimum of 39 paramedics were necessary to achieve a Cohen d = 0.8, alpha error = 0.05, power = 0.95). To compensate for potential dropouts, we decided to enroll up to 55 paramedics into this study.
All statistical analyses were performed with the use of the Statistica 13.3 EN for Windows software (Tibco Inc.; Tulsa, OK). Data are presented as number (percentage), mean ± standard deviation (SD), or median (interquartile range [IQR]), as appropriate. Nonparametric tests were used for the data that did not have a normal distribution, which was tested with the Lilliefors test and the Shapiro–Wilk test. All statistical tests were 2-sided. The 1-way analysis of variance on ranks was applied to compare the different times and to determine the statistical difference for each group (post-hoc Bonferroni correction was used to counteract the problem of multiple comparisons). P value of <.05 was assumed statistically significant.
3. Results
Fifty-five paramedics participated in this study. Demographics and previous intubation experience are reported in Table 1. None of the paramedics had any previous training with the VieScope. Results are presented in Table 2.
Table 2.
Intubation parameters.
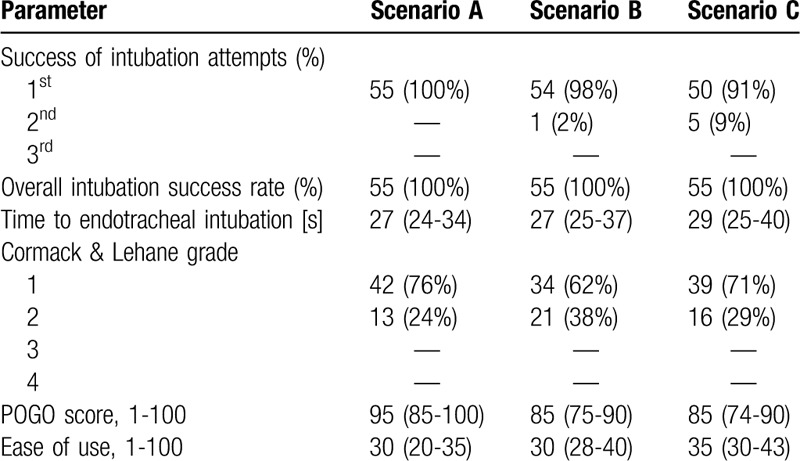
In scenario A, all paramedics were able to intubate with the first intubation attempt. Two percent of the paramedics required a second intubation attempt in scenario B and 9% in scenario C. Overall success rate was 100% in all 3 airway scenarios.
The median time to intubation was 27 seconds (24–34 seconds) in scenario A, 27 seconds (25–37 seconds) in scenario B, and 29 (25–40 seconds) in scenario C.
4. Discussion
Our study revealed novel and promising findings for the new airway device VieScope. First, we report consistent 100% overall first pass intubation success rate by all paramedics, even in difficult airway scenarios. Second, the time to achieve intubation was almost similar in all 3 scenarios. Third, the data confirms reasonably well laryngeal visualization by VieScope as determined by Cormack and Lehane score and POGO score.
Time to secure the airway is crucial in the emergency setting. Pediatric advance life support recommendations suggest that total intubation time should not exceed 30 seconds.[21] In our analysis, all paramedics achieved relatively quicker successful intubation (averaged 27–29 seconds) with the VieScope. In contrast, previous publications in the pediatric difficult airway manikin setting suggest prolonged intubation time exceeding the 30 seconds time limit using Miller and Macintosh laryngoscopes. Scenarios such as ongoing chest compressions during CPR increase time to intubation even more.[22–25] The mean intubation time with VieScope during chest compressions was noted to be 29 seconds–interestingly, similar to normal airways scenario.
Previous studies investigating several videolaryngoscopes including the McGrath and the Trueview demonstrated relatively shorter time to intubation during CPR.[26,27] This relatively longer time to intubation for the VieScope is based on the technique, as the VieScope includes 2 separate steps—introducing the bougie between vocal cords and the endotracheal tube vie the bougie into the trachea. However, our intubation times are broadly in keeping with a recent randomized clinical trial, comparing intubation with bougie and endotracheal tube with stylet in adult emergency settings.[28]
Multiple intubation attempts substantially increase risk of overall adverse events and leads to prolonged intubation.[9,29] Previous work suggests that an additional intubation attempt in pediatrics population exponentially increases the risk of severe desaturation (below 80%).[9,30] Notably, we found very few instances requiring another attempt. For example, second intubation attempt was noted in only 2% of the tongue edema scenario and only 9% in the CPR scenario. A similar study comparing Macintosh laryngoscope and McGrath videolaryngoscope during ongoing CPR demonstrated comparable first-time success rate (91% vs 98%) by paramedics.[31] Importantly, our paramedics were not previously trained to use VieScope and achieved reassuring first pass success rate of >90%, in difficult scenarios.
We also analyzed laryngeal visualization as another outcome and found that VieScope provides better visualization and superior laryngoscopic view, as shown by better Cormack-Lehane classification and POGO score. Likewise, participants rated VieScope as relatively easy to intubate device, consistently in all 3 scenarios.
Endotracheal intubation using different kinds of bougies is a simple, inexpensive technique first described in 1949. This technique is mostly reserved primarily for patients with poor laryngeal views or as a rescue device, if initial intubation attempt failed.[32] In adult patients, several studies in a wide range of different settings indicate a higher intubation success rate and lower intubation-related adverse events.[28,29,33,34] Intubation success rate with a bougie is reported to be up to 96% in the emergency setting, if performed by physicians.[28]
Our analysis has several limitations. First, it is worth noting that our study is a preliminary manikin study, the results of which are often difficult to extrapolate to the general human population. However, we tried to simulate the clinical practice scenario as closely as possible with strict standardization, but they can never fully translate actual clinical scenarios. Second, to provide more reliable evaluation and reduce bias, we recruited paramedics who had previous experience with direct laryngoscopy, but the results may be different in novice hands. Furthermore, no comparisons were made with other devices and the manikin morphological anatomy may favor a specific airway device which may distort the results. Lastly, our manikin study design did not allow us to evaluate VieScope and its bougie-related complications such as airway trauma, although bougies are generally considered safe devices.[35,36]
5. Conclusions
Based on preliminary manikin study, our results emphasized that VieScope may be helpful to achieve quicker, favorable first pass success rate in normal and difficult airways scenarios, with minimum learning curve. It appears that VieScope may be a useful addition to already available airway devices for difficult airway scenarios. However, future comparative manikin and clinical studies will be needed to ascertain the advantages of VieScope over another airway device while including the clinical as well as practical aspects in prehospital settings.
Author contributions
Conceptualization: Maciej Maslanka, Lukasz Szarpak.
Data curation: MaciekjMaslanka, Lukasz Szarpak.
Formal analysis: Lukasz Szarpak, Maciej Maslanka.
Investigation: Maciej Maslanka, Lukasz Szarpak.
Methodology: Maciej Maslanka, Jacek Smereka.
Project administration: Lukasz Szarpak.
Resources: Lukasz Szarpak, Maciej Maslanka, Jacek Smereka.
Supervision: Lukasz Szarpak.
Validation: Maciej Maslanka, Kurt Ruetzler.
Visualization: Lukasz Szarpak, Maciej Maslanka.
Writing – original draft: Maciej Maslanka.
Writing – review & editing: all authors.
Footnotes
Abbreviations: CONSORT = CONsolidated Standards of Reporting Trials, CPR = cardiopulmonary resuscitation, IRB = institutional review board, IQR = interquartile range, POGO = percentage of glottic opening, SD = standard deviation.
How to cite this article: Maslanka M, Szarpak L, Ahuja S, Ruetzler K, Smereka J. Novel airway device Vie Scope in several pediatric airway scenario- a randomized simulation pilot trial. Medicine. 2020;99:28(e21084).
This study was supported by the Polish Society of Disaster Medicine.
The authors report no conflicts of interest.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- [1].Ruetzler K, Smereka J, Abelairas-Gomez C, et al. Comparison of the new flexible tip bougie catheter and standard bougie stylet for tracheal intubation by anesthesiologists in different difficult airway scenarios: a randomized crossover trial. BMC Anesthesiol 2020;20:90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Smereka J, Czyzewski L, Szarpak L, et al. Comparison between the TrueView EVO2 PCD and direct laryngoscopy for endotracheal intubation performed by paramedics: preliminary data. Am J Emerg Med 2017;35:789–90. [DOI] [PubMed] [Google Scholar]
- [3].Goliasch G, Ruetzler A, Fischer H, et al. Evaluation of advanced airway management in absolutely inexperienced hands: a randomized manikin trial. Eur J Emerg Med 2013;20:310–4. [DOI] [PubMed] [Google Scholar]
- [4].Ruetzler K, Roessler B, Potura L, et al. Performance and skill retention of intubation by paramedics using seven different airway devices--a manikin study. Resuscitation 2011;82:593–7. [DOI] [PubMed] [Google Scholar]
- [5].Ruetzler K, Guzzella SE, Tscholl DW, et al. Blind intubation through self-pressurized, disposable supraglottic airway laryngeal intubation masks: an international, multicenter prospective cohort study. Anesthesiology 2017;127:307–16. [DOI] [PubMed] [Google Scholar]
- [6].Thoeni N, Piegeler T, Brueesch M, et al. Incidence of difficult airway situations during prehospital airway management by emergency physicians—a retrospective analysis of 692 consecutive patients. Resuscitation 2015;90:42–5. [DOI] [PubMed] [Google Scholar]
- [7].Vilke GM, Steen PJ, Smith AM, et al. Out-of-hospital pediatric intubation by paramedics: the San Diego experience. J Emerg Med 2002;22:71–4. [DOI] [PubMed] [Google Scholar]
- [8].Walas W, Aleksandrowicz D, Kornacka M, et al. The management of unanticipated difficult airways in children of all age groups in anaesthetic practice—the position paper of an expert panel. Scand J Trauma Resusc Emerg Med 2019;27:87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Fiadjoe JE, Nishisaki A, Jagannathan N, et al. Airway management complications in children with difficult tracheal intubation from the Pediatric Difficult Intubation (PeDI) registry: a prospective cohort analysis. Lancet Respir Med 2016;4:37–48. [DOI] [PubMed] [Google Scholar]
- [10].Ruetzler K, Szarpak L, Smereka J, et al. Comparison of direct and video laryngoscopes during different airway scenarios performed by experienced paramedics: a randomized cross-over manikin study. Biomed Res Int 2020;2020:5382739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Ruetzler K, Imach S, Weiss M, et al. [Comparison of five video laryngoscopes and conventional direct laryngoscopy: Investigations on simple and simulated difficult airways on the intubation trainer]. Anaesthesist 2015;64:513–9. [DOI] [PubMed] [Google Scholar]
- [12].Jaber S, De Jong A, Pelosi P, et al. Videolaryngoscopy in critically ill patients. Crit Care 2019;23:221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Park R, Peyton JM, Fiadjoe JE, et al. The efficacy of GlideScope(R) videolaryngoscopy compared with direct laryngoscopy in children who are difficult to intubate: an analysis from the paediatric difficult intubation registry. Br J Anaesth 2017;119:984–92. [DOI] [PubMed] [Google Scholar]
- [14].Sunder RA, Haile DT, Farrell PT, et al. Pediatric airway management: current practices and future directions. Paediatr Anaesth 2012;22:1008–15. [DOI] [PubMed] [Google Scholar]
- [15].Abdelgadir IS, Phillips RS, Singh D, et al. Videolaryngoscopy versus direct laryngoscopy for tracheal intubation in children (excluding neonates). Cochrane Database Syst Rev 2017;5:CD011413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Sun Y, Lu Y, Huang Y, et al. Pediatric video laryngoscope versus direct laryngoscope: a meta-analysis of randomized controlled trials. Paediatr Anaesth 2014;24:1056–65. [DOI] [PubMed] [Google Scholar]
- [17].Bielski A, Rivas E, Ruetzler K, et al. Comparison of blind intubation via supraglottic airway devices versus standard intubation during different airway emergency scenarios in inexperienced hand: Randomized, crossover manikin trial. Medicine (Baltimore) 2018;97:e12593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Prekker ME, Kwok H, Shin J, et al. The process of prehospital airway management: challenges and solutions during paramedic endotracheal intubation. Crit Care Med 2014;42:1372–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Turner L, Shamseer L, Altman DG, et al. Consolidated standards of reporting trials (CONSORT) and the completeness of reporting of randomised controlled trials (RCTs) published in medical journals. Cochrane Database Syst Rev 2012;11:MR000030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Biro P, Ruetzler K. The reflective intubation manoeuvre increases success rate in moderately difficult direct laryngoscopy: A prospective case-control study. Eur J Anaesthesiol 2015;32:406–10. [DOI] [PubMed] [Google Scholar]
- [21].Duff JP, Topjian AA, Berg MD, et al. 2019 American Heart Association focused update on pediatric advanced life support: an update to the American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Pediatrics 2020;145: [DOI] [PubMed] [Google Scholar]
- [22].Xanthos T, Stroumpoulis K, Bassiakou E, et al. Glidescope((R)) videolaryngoscope improves intubation success rate in cardiac arrest scenarios without chest compressions interruption: a randomized cross-over manikin study. Resuscitation 2011;82:464–7. [DOI] [PubMed] [Google Scholar]
- [23].Szarpak L, Czyzewski L, Kurowski A. Can BONFILS intubation endoscope be an alternative to direct laryngoscopy for pediatric tracheal intubation during resuscitation? Am J Emerg Med 2015;33:293–4. [DOI] [PubMed] [Google Scholar]
- [24].Szarpak L, Czyzewski L, Kurowski A. Comparison of the Pentax, Truview, GlideScope, and the Miller laryngoscope for child intubation during resuscitation. Am J Emerg Med 2015;33:391–5. [DOI] [PubMed] [Google Scholar]
- [25].Koyama J, Iwashita T, Okamoto K. Comparison of three types of laryngoscope for tracheal intubation during rhythmic chest compressions: a manikin study. Resuscitation 2010;81:1172–4. [DOI] [PubMed] [Google Scholar]
- [26].Szarpak L, Kurowski A, Czyzewski L, et al. Comparison of infant intubation through the TruView EVO2, TruView PCD, and Miller laryngoscope by paramedics during simulated infant cardiopulmonary resuscitation: a randomized crossover manikin study. Am J Emerg Med 2015;33:872–5. [DOI] [PubMed] [Google Scholar]
- [27].Madziala M, Smereka J, Dabrowski M, et al. A comparison of McGrath MAC(R) and standard direct laryngoscopy in simulated immobilized cervical spine pediatric intubation: a manikin study. Eur J Pediatr 2017;176:779–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Driver BE, Prekker ME, Klein LR, et al. Effect of use of a Bougie vs endotracheal tube and stylet on first-attempt intubation success among patients with difficult airways undergoing emergency intubation: a randomized clinical trial. JAMA 2018;319:2179–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Mort TC. Emergency tracheal intubation: complications associated with repeated laryngoscopic attempts. Anesth Analg 2004;99:607–13. table of contents. [DOI] [PubMed] [Google Scholar]
- [30].Lee JH, Turner DA, Kamat P, et al. The number of tracheal intubation attempts matters! A prospective multi-institutional pediatric observational study. BMC Pediatr 2016;16:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Szarpak L, Truszewski Z, Czyzewski L, et al. A comparison of the McGrath-MAC and Macintosh laryngoscopes for child tracheal intubation during resuscitation by paramedics. A randomized, crossover, manikin study. Am J Emerg Med 2016;34:1338–41. [DOI] [PubMed] [Google Scholar]
- [32].Combes X, Le Roux B, Suen P, et al. Unanticipated difficult airway in anesthetized patients: prospective validation of a management algorithm. Anesthesiology 2004;100:1146–50. [DOI] [PubMed] [Google Scholar]
- [33].Sakles JC, Chiu S, Mosier J, et al. The importance of first pass success when performing orotracheal intubation in the emergency department. Acad Emerg Med 2013;20:71–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Rognas L, Hansen TM, Kirkegaard H, et al. Pre-hospital advanced airway management by experienced anaesthesiologists: a prospective descriptive study. Scand J Trauma Resusc Emerg Med 2013;21:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Rai MR. The humble bougie. Forty years and still counting? Anaesthesia 2014;69:199–203. [DOI] [PubMed] [Google Scholar]
- [36].Hodzovic I, Latto IP, Henderson JJ. Bougie trauma—what trauma? Anaesthesia 2003;58:192–3. [DOI] [PubMed] [Google Scholar]


