Supplemental Digital Content is available in the text
Keywords: China, dental care for children, dental caries, risk factors
Abstract
An effective prevention policy for dental caries is absent in Jilin, China because of outdated and insufficient data. Therefore, this study aimed to investigate dental caries status and related risk indicators among 12-year-old students in Jilin Province.
We conducted a cross-sectional investigation among 2324 children aged 12 years from 9 regions of Jilin in 2017. Caries was evaluated with the decayed-missing-filled teeth index and the significant caries index. The rate of pit and fissure closure, education level of patients, brushing habits, and sugar consumption were evaluated in a structured questionnaire. The associated risk indicators of caries were also assessed through logistic regression analysis.
The prevalence of dental caries is 56.11%, and the value of decayed-missing-filled teeth was 1.53. More dental caries was found in students living in high-fluorine areas (P < .01). The results of logistic regression analysis show that females, poor self-assessment of oral health, toothache experience, dental visits, and education levels of parents are risk indicators for caries (P < .01).
Regarding the current status of DC among 12-year-old students in Jilin Province, (1) The high-fluorine areas have lower DC prevalence than the non-high fluorine areas, (2) Female students have higher DC prevalence than male students, (3) Poor self-assessment of dental health, toothache experience, dental visits, and low education levels of parents can increase the risk of dental caries.
1. Introduction
Dental caries (DC) is a widespread, chronic, cumulative, and oral bacterial disease that affects 60% to 90% of school-age children and almost 100% adults worldwide.[1–9] It can continue to deteriorate if there is no timely management, thus leading to pain and infection,[10] affecting students’ school performance, attendance, and even their quality of life.[11,12] Moreover, the treatment of oral diseases is costly and may pose a tremendous financial burden on individuals and national health care systems.[13] DC is a dynamic process of dental damage caused by a combination of multiple pathological factors,[10] such as bacteria, fungal species, eating habits, oral hygiene habits, education background of parents.[2,8,14–22] The pathogenesis of DC is inorganic demineralization and decomposition of organic matters on the tooth surface.[23] Many scholars have reported that protective factors, including fluoride level of drinking water, a healthy diet, good oral habits, the pit and fissure sealing, can inhibit or even reverse demineralization.[2,14,16–18,20,24,25] Therefore, reducing risk factors and increasing protective factors may be an effective way to prevent DC.[26]
Over the past 3 decades, DC experience among children worldwide has decreased significantly.[27] Nevertheless, the prevalence of DC varies considerably between urban and rural areas and between genders. The latest data were achieved in 2005. They are not sufficient as a baseline for provincial oral health. Moreover, in the past 20 years, with the rapid development of China's economy, the investment in dental medical facilities has increased and the citizens’ awareness of oral health care has enhanced. These factors may affect the incidence of DC. Consequently, specific, detailed, and renovated data focused on the prevalence of DC and related risk factors are crucial to the development of effective prevention programs for oral diseases. Therefore, the objective of the present study is to determine the prevalence of DC, as well as to detect the risk factors associated with DC among 12-year-old students in Jilin Province.
2. Ethical approval
Ethical approval for the study was obtained from the Jilin University Stomatological Hospital. Review No. (54) In 2019. Informed consent to examine the children was obtained from parents, and assent was obtained from children before examination.
3. Methods
We conducted a cross-sectional investigation among 2324 children aged 12 years from 9 regions of Jilin in 2017. Multi-stage, stratified, random sampling was used to select respondents of 12-year-old students in 9 regions.
3.1. Sample size evaluation
We measure the sample size using the following formula:
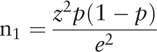 |
In the formula, n1 is a simple size; z was the level of confidence, and when the confidence was 95%, z was 1.96; p is the prevalence of DC (28.9% as reported by the Third National Oral Survey); e is the margin of error. The nonresponse rate was 5%. The final sample size in our study was 2324.
3.2. Sampling design
By using a simple random sampling technique, 9 areas in Jilin Province were investigated (Fig. 1), and then 4 school in every region was also selected by a simple random sampling technique. The simple allocated size in every school was according to the total sample size and the percentage of the 12-year-old students of every school in all the 9 schools. Finally, the participants were selected by a simple random sampling method according to the name lists in every school.
Figure 1.
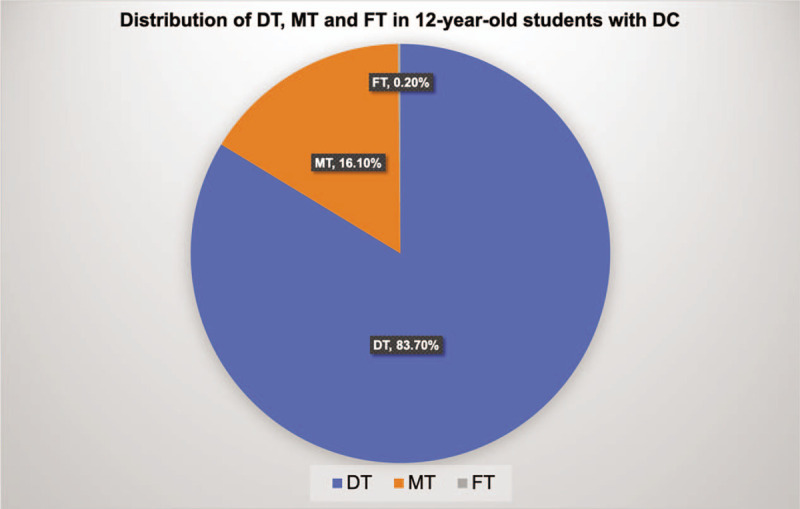
Distribution ofnnnnnnnnnnn and FT in 12-yr-old students with DC. DT = decayed teeth, FT = filled teeth, MT = missing teeth.
3.3. Oral examination and data collection
Three certified dentists with clinical experience performed an oral examination for more than 3 years. Before the survey, they received theoretical and clinical training again, and the Kappa value (SPSS 23.0 software, IBM Corp., Armonk NY) of the standard consistency test was more significant than 0.8. The evaluation criteria of kappa value are as follows: Kappa ≥ 0.75 indicates that the diagnostic results of the 2 methods are in good consistency; 0.4 ≤ kappa < 0.75 indicates that the diagnostic results of the 2 methods are in general consistency; kappa < 0.4 indicates that the diagnostic results of the 2 methods are in poor consistency. During the study, 5% of the respondents were randomly selected for re-examination, and the Kappa values calculated were still higher than 0.8. The clinical assessment of the students was according to the methods and criteria provided by the World Health Organization Oral Health Surveys.[28]
Disposable plane mouth mirrors under a portable light. Community periodontal index probes were used to perform the examination, and the participants were in a supine position in mobile dental chairs. The decayed-missing-filled teeth (DMFT) indexes evaluated the status of DC.
After the oral examination, all the participants were asked to complete a structured questionnaire (Attachment 1), which covered family background (single child or not, whether parents’ education level are higher than junior college; oral habits (frequency of tooth brushing a day); dietary habits (frequency of eating desserts and candies, frequency of carbonated drinks, frequency of drinking sugared beverages (milk, yogurt, milk tea, soy milk or coffee with sugar); Self-assessment of teeth (Excellent, Good, Fair or Poor); Experience of toothache (Often, Occasional, Rare, Never); Visit to dentist (Yes or No) and Frequency of dentist visit (Once a year or 2–4 times a year); Tooth injury (Yes, Not or Unknown).
SPSS Statistics (SPSS, Version 23.0, IBM Corp.) was used to analyze the data. Descriptive statistics and Chi-square tests were performed to assess the relationship between DC and related variables. Further research on the association between DC prevalence and caries risk factors were also revealed by logistic regression analysis. A P-value of less than .05 was defined as statistically significant.
4. Results and Discussion
A total of 2324 students aged 12-year-old were involved in this study, and all the participants finished the oral examination. However, only 2317 questionnaires were collected. The prevalence of DC in Jilin Province was 56.11%, and the results of the DC examination in 9 regions are shown in Table 1.
Table 1.
Caries of 12-yr-old children in 9 regions of Jilin.
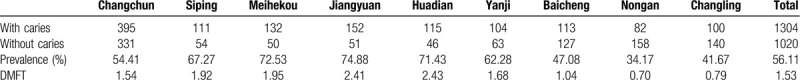
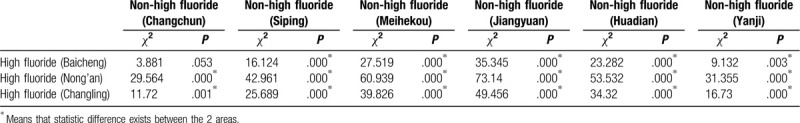
Of the 9 regions, Baicheng, Changling, and Nongan are high fluoride areas. When compared to the non-fluoride areas (the other 6 regions) respectively, we found that the prevalence of DC in the 3 high fluoride regions was significant lower than that of non-fluoride areas (P < .01) (Table 1), except that between Baicheng and Changchun (Table 2).
Table 2.
The prevalence of caries in the high fluoride areas and the non-high fluoride areas.
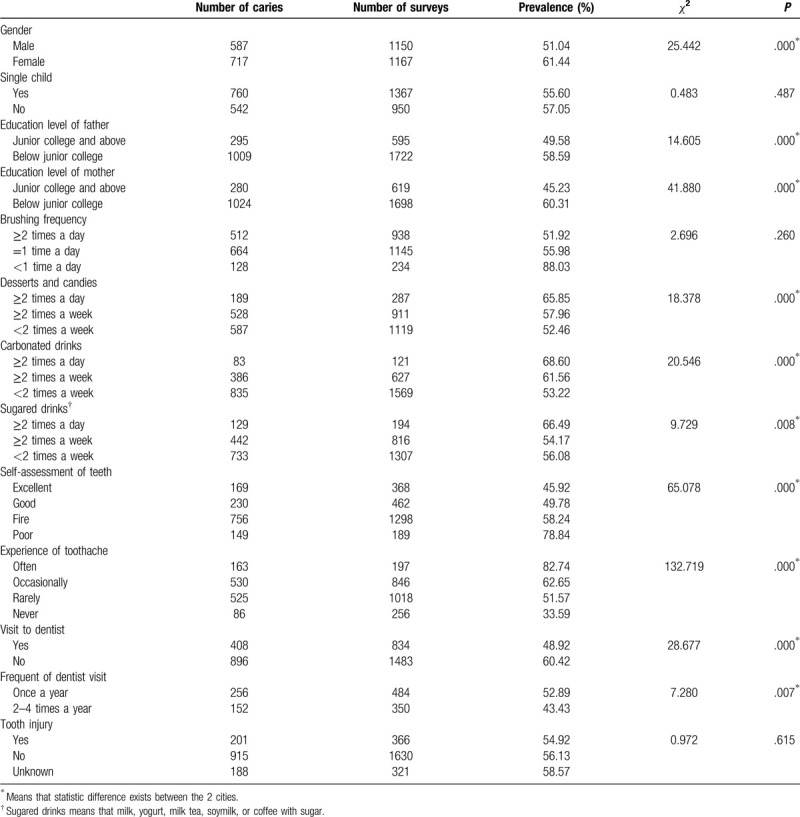
Many differences were revealed between DC and related variables (Table 3), and the differences were demonstrated to be statistically significant (P < .05). Among children in Jilin, the prevalence of DC in females was 61.44%, which was higher than 51.04% in males (P < .001). However, whether the student was a single child seems not to be a related variable for the prevalence of DC (P > .05). The education level of the parent has a significantly influence on the prevalence of DC (P < .001). Interestingly, it seems that brushing frequency has no obvious influence on the effect on the prevalence of DC (P > .05). Not surprisingly, the frequency of having desserts and candies, carbonated drinks, and sugared drinks can affect the prevalence of DC. The self-assessment of teeth was also proved to be a related variable; the prevalence of DC could up to be 78.84% when the self-assessment was “poor.” The experience of toothache could be a warning sign in predicting the occurrence of DC, in the students who often experienced a toothache, the prevalence of DC was up to 82.74%. Dentist visits can affect the prevalence of DC (P < .01). The injury of the tooth does not influence the prevalence of DC (P > .05).
Table 3.
Prevalence of dental caries associated risk factors according to the questionnaire.
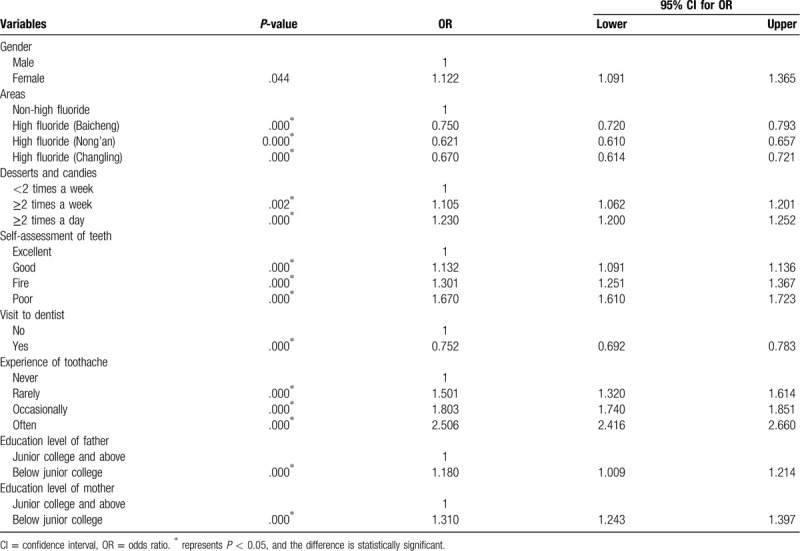
Logistic regression analysis of potential explanatory factors of DC (Table 4) revealed the association between the prevalence of DC and the 8 related risk indicators. Gender is one of the factors related to DC, and the odds ratio of females was 1.122 than males, the difference was significant. The prevalence of DC in high fluoride areas was lower than that in non-high fluoride areas, and the odds ratios of DR in Baicheng, Nong’an, Changling were 0.750, 0.621, 0.670, respectively. Regression analysis of DC with the frequency of eating desserts and candies “≥2 times a week” and “≥2 times a day” showed significant odds ratio (1.105 and 1.230) when compared to “<2 times a week.” Significant differences were also shown in the “self-assessment of teeth,” the odds ratios were 1.132 (good), 1.301 (fair) and 1.670 (poor), and the P-values were all <.001. Whether going to see a dentist also has an influence on the prevalence of DC, the odds ratio was 0.692 to 0.783 of “Yes” and “No.” More experience of toothache was also a risk factor. Regression analysis of DC with the education level of the parent, both father and mother, shows a significant odds ratio, which means that the education level of the parent (both father and mother) has an influence on the prevalence of DC.
Table 4.
Logistic regression of dental caries and its potential explanatory variables.
DC is the most common oral disease. More than 2.4 billion people globally were affected by DC in 2010.[29] In addition, it has a relatively high incidence in China, resulting in a heavy burden on the Chinese national healthcare system and also a more substantial economic burden on the general citizens.[30,31] Stomatology doctors should understand the current prevalence of DC to identify related risk factors and solve the troubles induced by DC. However, the epidemiological data on DC in Jilin Province is outdated and insufficient. Thus, we carried this study to investigate DC status, to learn precisely about the oral health conditions of the population as an attempt to make prevention strategies, as well as to determine medical requires.
Following the criteria emphasized by the World Health Organization, we selected 12-year-old students as the respondents[4,32] and performed a cross-sectional study. On one hand, at the age of 12, students will experience the eruption of all permanent teeth except the third molar; on the other hand, school-based data collection at this age is much easy.
With an overall prevalence of 56.11%, DC is a common oral disease among 12-year-old students in Jilin Province. It is significantly higher than the average level of China as reported by the 3rd National Oral Health Survey in 2005 (28.9%),[33] also that of some other developing countries including Tamil Nadu India (40%),[34] Nigeria (13.9%),[35] Kashmir (25%),[36] and even some developed countries such as Sudan (30.5%).[37] Various factors, including socio-economic factors, sample size, dietary behaviors, brushing habits, and cultural differences, can lead to different results.[2,3,8,14,15,24,25] Thus, it is necessary to carefully and reasonably interpret each result. We speculate that the high incidence of DC in Jilin Province may be attributed to the following 2 factors:
-
(1)
rapid economic growth in recent years, which has led to lifestyle changes, changes in eating habits, and an increase in the consumption of sweet snacks and soft drinks, as argued by Hu J and his colleagues[2];
-
(2)
the dental health resources in Jilin Province are rare, especially in grassroots health care institutions.
The high-fluorine areas have lower DC prevalence than the non-high fluorine areas. The incidence of DC in 9 areas of Jilin province ranged from 34.7% to 74.88%, and the difference was significant in different areas. Generally, children in rural areas have higher rates of DC due to risk factors such as low education level of parents and poor oral health care conditions.[2,7,18,19,24] Interestingly, Nong’an, a rural county of Jilin, has the lowest prevalence of DC (34.17%). This finding may be related to the location of Nong’an, which belongs to the high fluorine area. Children in high-fluoride areas have higher levels of fluoride in their drinking water, which inhibits the prevalence of DC.[6] Moreover, among the 9 areas surveyed in Jilin Province, Nong’an, Changling, and Baicheng are the high fluoride areas, while the other 6 regions are non-high fluoride areas. The results show that the prevalence of DC in high fluoride areas is significantly lower than that in non-high fluoride areas.
Female students have higher DC prevalence and filling rates than male students, even though male children have worse oral hygiene. This finding in our study is consistent with the results in the USA and other provinces of China.[2,38] Two possible explanations are that those female students are more likely to eat cariogenic foods, in addition to earlier tooth eruption in girls than boys.[39] It exposes their teeth to a cariogenic oral environment for a longer time compared to boys.
The total mean DMFT value is 1.53, which is lower than the number in the literature reported in Eritrea (2.5),[18] in Brazil (2.04),[40] and in Quito (1.6),[4] but higher than that of 0.14 in Nigeria,[41] 0.42 in Sudan,[42] and 0.42 in Kenya,[43] 1.4 in São Paulo.[44] Our result reflects that the dietary habits, application of dental care facilities, awareness, and dental care practice in Jilin Province are at the middle level in the world and further improvement is needed.
From the 1st Chinese National Oral Survey in 1983 to the 3rd Chinese National Oral Survey in 2005, the DMFT of China's 12-year-old students showed a favorable trend, decreased from 1.03 to 0.5.[45] However, the results of this study show adverse trends from 2009 to 2017, with the prevalence of DC increasing from 43.65% to 56.11%, and DMFT increasing from 1.07 to 1.53. Besides, significant statistical differences in DMFT score and DC prevalence were detected between urban and rural children, since urban students obtained a higher FT score and filling rate than rural students. This result may be attributed to China's unevenly distribution of medical resources between urban and rural areas. Therefore, urban students have more access to appropriate oral health education, dental care, and the oral health care system. Under the premise of rapid economic development, on the one hand, the investment in medical health care has been increased. On the other hand, cariogenic food for residents is more accessible. However, spending on oral health care is still low. Thus, considerable efforts in preventive oral health measures should be ready to face a predictable further increase in DC due to continuing social and economic development.
The dentist visit is an essential risk factor associated with DC.[2] In Nigeria, Eritrea, and Kenya respectively, 80%,[35] 69%,[18] and 46.7%[43] of the study participants did not report dental treatment. In this study, more than half (60.42%) of the participants said they had never visited a dentist. It was further found that 79% of students who had visited a dentist in Jilin Province had a toothache, similar to studies investigating Iraq (71.2%), Kenya (73.4%), and Eritrea (82%). Therefore, underutilization of dental care facilities is a potential factor contributing to the high incidence of DC. Also, the authors reported that children who went to a dentist more often had more frequent experience of toothache and DC.[46] In the past, the national strategy for healthcare was treatment-orientated care, rather than prevention-orientated care.[47] At the same time of treatment, patients got information about the approach to oral problem prevention. This may explain why students brushing their teeth twice or more a day have higher DC prevalence and DMFT scores.[2]
Toothbrush and toothpaste are the 2 most common and effective methods for promoting oral hygiene.[14,16,48,49] Furthermore, brushing teeth twice a day[14,16,48] and using fluoridated toothpaste at concentrations of 1,000 PPM or more have proven to benefit dental health.[50] However, some scholars believe that brushing will not prevent DC.[25] We found 51.92% of students brushing their teeth twice daily, which was significantly higher than the results of Eritrea (19.1%).[18] However, 73.7% of children did not know that brushing teeth could prevent periodontal disease, and many students brushed their teeth alone without help. As a result, their brushing might be ineffective. Thus, monitoring the frequency and effect of cleaning and strengthening the awareness of oral health care are essential measures to prevent DC in the future.
For sugar consumption, limiting sugars to 5% of energy intake is helpful to minimize the risk of DC.[51] In our study, we detected that eating dessert and drinking sweet drinks more than twice a day were risk factors for DC (P < .05), but sweetened milk, soy milk, and coffee did not increase the risk (P > .05). Peres et al[47] also agreed to the viewpoint that sugar consumption might lead to DC. Consequently, reasonable control of sugar intake is considered as an effective strategy to reduce or eliminate the causes of DC.
As for the pit and fissure sealing rate, scholars think it is a valid measure to prevent DC. However, the rate of pit and fissure sealing in Jilin Province is only 10%, lower than the result of 3.6% in Sichuan Province, China in 2016, and 6.9% in China in 2005. Therefore, this policy needs to be widely implemented in Jilin Province. For instance, Zhejiang Province in China extensively carries out the pit and fissure sealing for young people and obtains positive effect.[2]
Although we got a detailed, objective, and updated data of DC in the present study, there are still many limitations. First, in the assessment part of the questionnaire, students’ different awareness of bad habits and healthy habits may affect the assessment results. Secondly, there is a bias in the proportion of urban and rural students, which may cause the conclusion not to be available for the entire group of 12-year-old children in Jilin Province. Therefore, we should strictly control the inclusion criteria and exclusion criteria of the research objects, and collect the data objectively and uniformly. We should adopt blind method to collect the data and conduct hierarchical analysis and multivariate analysis. At last, no test–retest was performed in the present study, which can be regarded as a logical limitation.
5. Conclusions
Regarding the current status of DC among 12-year-old students in Jilin Province,
-
(1)
The high-fluorine areas have lower DC prevalence than the non-high fluorine areas,
-
(2)
Female students have higher DC prevalence than male students,
-
(3)
Poor self-assessment of dental health, toothache experience, dental visits, and low education levels of parents can increase the risk of DC.
Author contributions
Conceptualization: Rui Wang.
Data curation: Fenglan Zhang.
Investigation: Chong Chen.
Methodology: Fenglan Zhang.
Validation: Rui Wang.
Writing – original draft: Chong Chen, Fenglan Zhang.
Writing – review & editing: Rui Wang.
Supplementary Material
Footnotes
Abbreviations: DC = dental caries, DMFT = decayed-missing-filled teeth.
How to cite this article: Chen C, Zhang F, Wang R. Dental caries experience and related risk indicators of 12-year-old students in Jilin, China. Medicine. 2020;99:28(e20988).
Study was supported by the Scientific Research Project of Jilin Provincial Health Commission (2017W001).
The authors declare that they have no conflict of interest.
Supplemental Digital Content is available for this article.
The datasets generated during and/or analyzed during the current study are publicly available.
References
- [1].Du A, Zhang H, Chen C, et al. Oral health of 12-year-old children in Jilin province, China: a population-based epidemiological survey. Medicine (Baltimore) 2019;98:e18463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Hu J, Jiang W, Lin X, et al. Dental caries status and caries risk factors in students ages 12–14 years in Zhejiang, China. Med Sci Monit 2018;24:3670–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Navarro Azevedo de Azeredo F, Silva Guimaraes L, Azeredo AAL, et al. Global prevalence of dental caries in athletes with intellectual disabilities: an epidemiological systematic review and meta-analysis. Spec Care Dentist 2019;39:114–24. [DOI] [PubMed] [Google Scholar]
- [4].Michel-Crosato E, Raggio DP, Coloma-Valverde ANJ, et al. Oral health of 12-year-old children in Quito, Ecuador: a population-based epidemiological survey. BMC Oral Health 2019;19:184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Lima IFP, Nobrega DF, Cericato GO, et al. Prevalence of dental fluorosis in regions supplied with non-fluoridated water in the Brazilian territory: a systematic review and meta-analysis. Cien Saude Colet 2019;24:2909–22. [DOI] [PubMed] [Google Scholar]
- [6].Dalledone M, Cunha AS, Ramazzotto LA, et al. Estrogen receptor gene is associated with dental fluorosis in Brazilian children. Clin Oral Investig 2019;23:3565–70. [DOI] [PubMed] [Google Scholar]
- [7].Zhou Y, Chen D, Zhi Q, et al. Epidemiology and risk indicators of dental fluorosis in 12-year-old children in China. The 18th Annual Conference of Stomatological Preventive Medicine, Chinese Society of Stomatology. 2018. [Google Scholar]
- [8].Sun HY, Jiang H, Du MQ, et al. The prevalence and associated factors of periodontal disease among 35 to 44-year-old Chinese adults in the 4th National Oral Health Survey. Chin J Dent Res 2018;21:241–7. [DOI] [PubMed] [Google Scholar]
- [9].Petersen PE, Bourgeois D, Ogawa H, et al. The global burden of oral diseases and risks to oral health. Bull World Health Organ 2005;83:661–9. [PMC free article] [PubMed] [Google Scholar]
- [10].Selwitz RH, Ismail AI, Pitts NB. Dental caries. Lancet 2007;369:51–9. [DOI] [PubMed] [Google Scholar]
- [11].Krisdapong S, Prasertsom P, Rattanarangsima K, et al. Relationships between oral diseases and impacts on Thai schoolchildren's quality of life: evidence from a Thai national oral health survey of 12- and 15-year-olds. Community Dent Oral Epidemiol 2012;40:550–9. [DOI] [PubMed] [Google Scholar]
- [12].Montero J, Rosel E, Barrios R, et al. Oral health-related quality of life in 6- to 12-year-old schoolchildren in Spain. Int J Paediatr Dent 2016;26:220–30. [DOI] [PubMed] [Google Scholar]
- [13].Kassebaum NJ, Bernabe E, Dahiya M, et al. Global burden of untreated caries: a systematic review and metaregression. J Dent Res 2015;94:650–8. [DOI] [PubMed] [Google Scholar]
- [14].Boustedt K, Dahlgren J, Twetman S, et al. Tooth brushing habits and prevalence of early childhood caries: a prospective cohort study. Eur Arch Paediatr Dent 2020;21:155–9. [DOI] [PubMed] [Google Scholar]
- [15].Al-Rafee MA, AlShammery AR, AlRumikan AS, et al. A comparison of dental caries in urban and rural children of the Riyadh region of Saudi Arabia. Front Public Health 2019;7:195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Sun X, Bernabe E, Liu X, et al. Early life factors and dental caries in 5-year-old children in China. J Dent 2017;64:73–9. [DOI] [PubMed] [Google Scholar]
- [17].Han K, Park JB. Association between oral health behavior and periodontal disease among Korean adults: the Korea national health and nutrition examination survey. Medicine (Baltimore) 2017;96:e6176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Andegiorgish AK, Weldemariam BW, Kifle MM, et al. Prevalence of dental caries and associated factors among 12 years old students in Eritrea. BMC Oral Health 2017;17:169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Tasneem S, Sultan S, Gowhar O, et al. Prevalence of dental caries among 12 year old school children in Kashmir, India - a cross-sectional study. Int J Contemp Med Res 2016;3:2156–9. [Google Scholar]
- [20].Paiva PCP, de Paiva HN, de Oliveira Filho PM, et al. Prevalence and risk factors associated with traumatic dental injury among 12-year-old schoolchildren in Montes Claros, MG, Brazil. Ciencia e Saude Coletiva 2015;20:1–0. [DOI] [PubMed] [Google Scholar]
- [21].Bowen WH, Burne RA, Wu H, et al. Oral biofilms: pathogens, matrix, and polymicrobial interactions in microenvironments. Trends Microbiol 2018;26:229–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Rodrigues ME, Gomes F, Rodrigues CF. Candida spp./bacteria mixed biofilms. J Fungi (Basel) 2020;6:1–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Featherstone JDB. The continuum of dental caries - evidence for a dynamic disease process. J Dent Res 2004;83((SPEC. ISS. C)):C39–42. [DOI] [PubMed] [Google Scholar]
- [24].Pham TAV, Nguyen PA. Factors related to dental caries in 10-year-old Vietnamese school children. Int Dent J 2019;69:214–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Nishide S, Yoshihara T, Hongou H, et al. Daily life habits associated with eveningness lead to a higher prevalence of dental caries in children. J Dent Sci 2019;14:302–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Featherstone JDB. The science and practice of caries prevention. J Am Dent Assoc 2000;131:887–99. [DOI] [PubMed] [Google Scholar]
- [27].Do LG. Distribution of caries in children: variations between and within populations. J Dent Res 2012;91:536–43. [DOI] [PubMed] [Google Scholar]
- [28].WHO. Oral Health Surveys: Basic Methods. 5th ed. Geneva: World Health Organization. 2013. [Google Scholar]
- [29].Marcenes W, Kassebaum NJ, Bernabe E, et al. Global burden of oral conditions in 1990-2010: a systematic analysis. J Dent Res 2013;92:592–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Zhang SS, Wang XZ, Liu XN, et al. Economic burden of oral disease in China. J Dent Res. 2016;95(Spec Iss B):1571. [Google Scholar]
- [31].Cheng ML, Xu MR, Xie YY, et al. Utilisation of oral health services and economic burden of oral diseases in China. Chin J Dent Res 2018;21:275–84. [DOI] [PubMed] [Google Scholar]
- [32].WHO. Oral Health Surveys: Basic Methods. World Health Organization. 2013. [Google Scholar]
- [33].Lu HX, Tao DY, Lo ECM, et al. The 4th National Oral Health Survey in the mainland of China: background and methodology. Chin J Dent Res 2018;21:161–5. [DOI] [PubMed] [Google Scholar]
- [34].Prabu JJ, Saravanan S. Impact of dental caries and dental fluorosis on the quality of life on 12 year old children in Tamil Nadu, India. Chettinad Health City Med J 2013;2:74–9. [Google Scholar]
- [35].Sofowora C, Nasir W, Oginni A, et al. Dental caries in 12 year old suburban Nigerian school children. Afr Health Sci 2006;6:145–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Tasneem S, Sultan S, Gowhar O, et al. Prevalence of dental caries among 12 year old school children in Kashmir, India-a crosssectional study. Int J Contemp Med Res 2016;3:2156–9. [Google Scholar]
- [37].Nurelhuda NM, Trovik TA, Ali RW, et al. Oral health status of 12-year-old school children in Khartoum state, the Sudan; a school-based survey. BMC Oral Health 2009;9:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Yin W, Yang YM, Chen H, et al. Oral health status in Sichuan province: findings from the oral health survey of Sichuan, 2015–2016. Int J Oral Sci 2017;9:10–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Lukacs JR, Largaespada LL. Explaining sex differences in dental caries prevalence: Saliva, hormones, and “life history” etiologies. Am J Hum Biol 2006;18:540–55. [DOI] [PubMed] [Google Scholar]
- [40].Freire Mdo C, Reis SC, Figueiredo N, et al. Individual and contextual determinants of dental caries in Brazilian 12-year-olds in 2010. Rev Saude Publica 2013;47: Suppl 3: 40–9. [DOI] [PubMed] [Google Scholar]
- [41].Adekoya-Sofowora CA, Nasir WO, Oginni AO, et al. Dental caries in 12-year-old suburban Nigerian school children. Afr Health Sci 2006;6:145–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Nurelhuda NM, Trovik TA, Ali RW, et al. Oral health status of 12-year-old school children in Khartoum state, the Sudan; a school-based survey. BMC Oral Health 2009;9:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Health KMo. Kenya National Oral Health Survey Report. Available at: www.health.go.ke. 2015;1–54. [Google Scholar]
- [44].Sousa Mda L, Rando-Meirelles MP, Torres LH, et al. Dental caries and treatment needs in adolescents from the state of Sao Paulo, Brazil. Rev Saude Publica 2013;47: Suppl 3: 50–8. [DOI] [PubMed] [Google Scholar]
- [45].Hu Dy, Hong X, Li X. Oral health in China – trends and challenges. Int J Oral Sci 2011;3:7–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Nomura LH, Bastos JL, Peres MA. Dental pain prevalence and association with dental caries and socioeconomic status in schoolchildren, Southern Brazil, 2002. Braz Oral Res 2004;18:134–40. [DOI] [PubMed] [Google Scholar]
- [47].Peres MA, Sheiham A, Liu P, et al. Sugar consumption and changes in dental caries from childhood to adolescence. J Dent Res 2016;95:388–94. [DOI] [PubMed] [Google Scholar]
- [48].ElSalhy M, Honkala S, Soderling E, et al. Relationship between daily habits, Streptococcus mutans, and caries among schoolboys. J Dent 2013;41:1000–6. [DOI] [PubMed] [Google Scholar]
- [49].Prasai Dixit L, Shakya A, Shrestha M, et al. Dental caries prevalence, oral health knowledge and practice among indigenous Chepang school children of Nepal. BMC Oral Health 2013;13:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Diehnelt DE, Asuman Kiyak H. Socioeconomic factors that affect international caries levels. Commun Dent Oral Epidemiol 2001;29:226–33. [DOI] [PubMed] [Google Scholar]
- [51].Moynihan PJ, Kelly SAM. Effect on caries of restricting sugars intake: systematic review to inform WHO guidelines. J Dent Res 2014;93:8–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


