Supplemental Digital Content is available in the text
Keywords: bladder, case report, mucosa-associated lymphoid tissue, transurethral resection of bladder tumors
Abstract
Introduction:
Primary bladder mucosa-associated lymphoid tissue (MALT) lymphoma is a rare tumor. To date, the PubMed database contains only 39 English articles covering 63 cases of primary bladder MALT lymphoma. Herein, we report a case of this disease and review the current literature.
Patient concerns:
A 77-year-old woman presented with frequent urination, urinary urgency, and dysuria for 3 years. In the past 3 years, the patient's symptoms recurred and progressively worsened, and she was admitted to the hospital.
Diagnosis:
A histopathological examination revealed the bladder mass as a tumor with high proliferation of atypical B-lymphocytes. Immunohistochemistry showed positive results for CD20, PAX-5, Ki-67, BCL-2, and CD21 and negative results for CD10, MUM1, TDT, and cyclin D1. These data supported the diagnosis of primary bladder MALT lymphoma.
Interventions:
A transurethral resection of bladder tumor was performed to treat the disease.
Outcomes:
The patient was alive and healthy at the 15-month follow-up.
Conclusion:
Primary bladder MALT lymphoma is a rare disease and can be easily missed or misdiagnosed before achieving a histological confirmation. Surgery may be the best choice for both diagnosis and treatment.
1. Introduction
Mucosa-associated lymphoid tissue (MALT) is a unique subtype of B-cell non-Hodgkin's lymphoma, and is a low-grade malignant tumor.[1] Primary MALT lymphoma of the bladder is rare. To date, the PubMed database contains only 39 English articles covering 63 cases of primary bladder MALT lymphoma, of which only 38 include description on clinical manifestations, treatments, and outcomes.[2–40] The cause of this disease is unknown, and there is no consensus on treatment approach. Herein, we report and discuss a case of primary bladder MALT lymphoma and its treatment. We also analyze the clinical characteristics, diagnosis, and treatment of this disease by reviewing the current literature.
2. Case report
A 77-year-old woman presented with frequent urination, urinary urgency, and dysuria for 3 years. She had pain after urination, without gross hematuria, and the symptoms had improved after anti-inflammatory treatment. In the past 3 years, the patient's symptoms recurred and progressively worsened, and she was admitted to the hospital on December 1, 2017. She reported no history of smoking, hepatitis, tuberculosis, connective tissue disease, drug or food allergies, or chronic cystitis. The superficial lymph nodes were not tender or swollen, and there was no ulcer in the mouth. No abnormalities were detected in the heart or abdomen. B-scan ultrasonography of the urinary system showed roughness in the inner walls of the bladder, and pelvic contrast-enhanced computed tomography (CT) showed multiple nodules in the bladder wall (Fig. 1A, 1B). CT of the chest and abdomen showed no swelling on lymph nodes. Bone marrow biopsy, gastrointestinal endoscopy, and abdominal color Doppler ultrasonography showed no abnormalities. Further cystoscopy improved the relevant findings by showing a “bladder occupying” tumor (Fig. 2).
Figure 1.
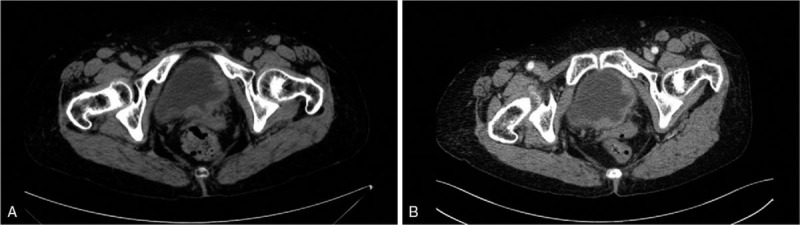
(A-B): Pelvic contrast-enhanced computed tomography (CT) showed multiple nodules in the bladder wall.
Figure 2.
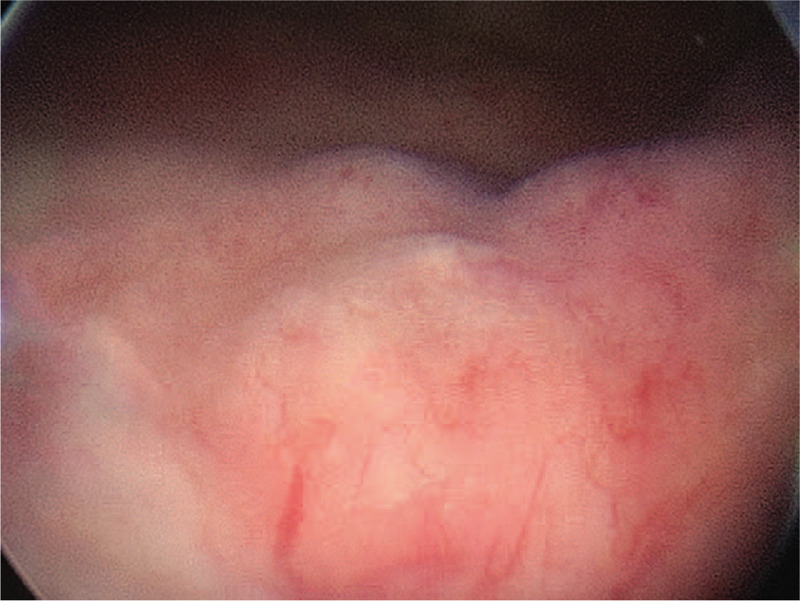
Cystoscopy showed “bladder occupancy”.
Histopathology of the bladder tumor revealed a “bladder occupying”, high proliferation of lymphatic tissue. Immunohistochemistry showed positive results for CD20, PAX-5, Ki-67, BCL-2, and CD21, but negative results for CD10, MUM1, TDT, and cyclin D1. The pathological diagnosis of the “bladder occupying” tumor was consistent with MALT lymphoma (Fig. 3).
Figure 3.
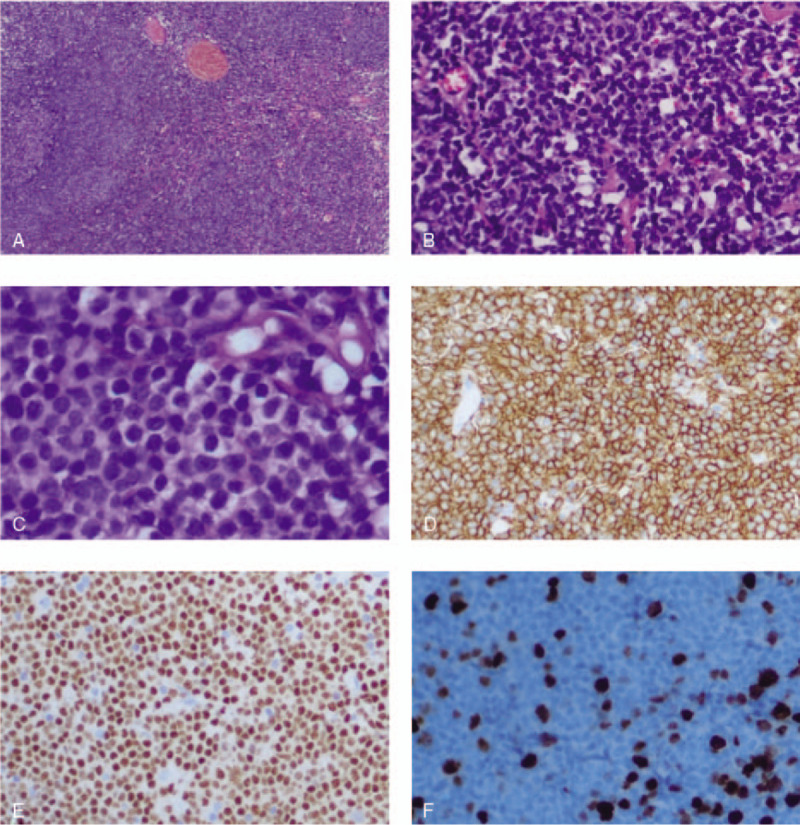
Characteristics of histological examination. The lesion consisted of dense lymphocyte infiltration with some lymphoid follicles (A, Hematoxylin and Eosin, HE 40x magnification). Small-to middle-sized, centrocyte-like lymphoid cell population were diffusely infiltrated with lymphoepithelial lesions of bladder (B, HE 200x magnification and C, HE 400x magnification). And lymphocytes were diffusely positive for CD20 (D 200x magnification) and pax-5 (E 200x magnification) antibodies. Ki67 labeling index was in a low level (F 200x magnification).
The patient underwent cystoscopy and transurethral resection of bladder tumors (TURBT) under general anesthesia using a laryngeal mask to excise the tumor. The clinical stage IE group A was confirmed based on the clinical and imaging examinations. According to the patient's condition, the patient was recommended radiotherapy and chemotherapy, which was rejected by the patient and family. Therefore, regular follow-up was performed. At the March 2019 follow-up, there were no abnormalities in the chest and abdominal CT, which was similar to the previous findings. Simultaneously, fluorodeoxyglucose-positron emission tomography/CT (FDG-PET/CT) showed no lesions other than those in the bladder.
3. Discussion
MALT lymphoma is a non-Hodgkin's lymphoma that causes B-cell proliferation in the mucosal margin. It is characterized by inert growth and a tendency to be localized in the primary area for a long time.[41] The concept of MALT lymphoma was first proposed by Isaacson and Wright in 1983.[42] MALT lymphoma invades many mucosal organs, of which stomach is the most common, followed by the lungs, while primary bladder MALT lymphoma is rare, accounting for approximately 0.2% of non-Hodgkin's lymphoma cases.[29,43,44] Kuhara et al[45] reported the first case of bladder MALT lymphoma in a woman in 1990. To date, the published literature on bladder MALT lymphoma consists mostly of case reports.
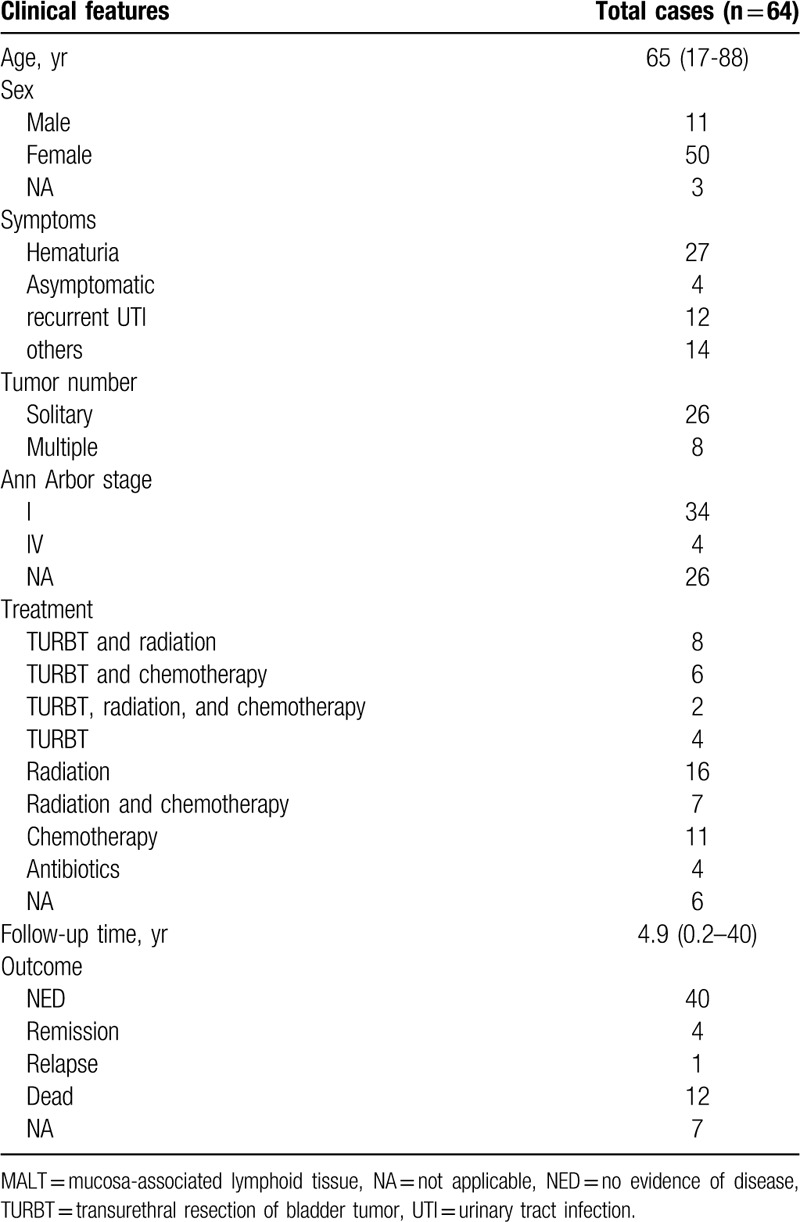
The clinical features and treatment of bladder MALT lymphoma are unclear. Table 1 summarizes the clinical features of the reported cases in a systematic review of the bladder MALT lymphoma, including the present case. We found that the average age of onset of the disease was 65 years (17–88 years). Women were more commonly affected, with the men/women ratio of about 1:5, which was consistent with previous literature.[34,46,47] The first symptom of the patient was mostly hematuria (50.9%). Most patients (76.5%) presented with a solitary mass. According to the Ann Arbor staging system, most patients (89.5%) belonged to stage IE.
Table 1.
Clinical features of the reported cases of primary bladder MALT lymphoma, including the present case.
The pathogenesis of primary bladder MALT lymphoma is unknown. At present, it is believed that bladder MALT lymphoma is caused by chronic inflammation. Chronic inflammation leads to the acquisition of MALT in the bladder mucosa, which progresses to lymphoma. Similar to the association between Helicobacter pylori and gastric MALT, Oscier et al reported that E coli is a common infectious agent for the pathogenesis of bladder MALT lymphoma, and patients can achieve complete remission after anti-infective treatment.[48] Bladder MALT lymphoma has also been reported in autoimmune interstitial cystitis, which is similar to the association between thyroid MALT lymphoma and chronic lymphocytic thyroiditis.[27] We analyzed the cases of a total of 64 patients with bladder MALT lymphoma, including the present case, of which 12 had recurrent urinary tract infection and 1 had interstitial cystitis. Four patients were treated with antibiotics; of them, 1 showed marked reduction in tumor size, and 3 had “no evidence of disease”. These results indicate that chronic inflammation and autoimmune disease may contribute to the development of primary bladder MALT lymphoma. However, further evidence is needed to reach a conclusion.
Most cases of primary bladder MALT lymphoma have a long disease course, insidious onset, and non-specific clinical manifestations. The most common clinical manifestation is gross hematuria, followed by dysuria, nocturia, frequent urination, urinary urgency, and painful urination. A few patients have complained of perineal pain and urinary incontinence. Only a few patients could locate the lower abdomen mass at presentation. Patients with this disease often receive delayed diagnosis and treatment due to the lack of specific symptoms and signs. The clinical manifestations in the present case were frequent urination, urinary urgency, and dysuria; thus, the diagnosis could not be made without pathological and immunohistochemical examinations. Typical MALT lymphoma cells often present as small to medium-sized lymphocytes with moderate cell mass and nuclear irregularities, similar to the follicular center cells, and are thus called “central cell-like cells.” In immunohistochemistry, MALT lymphoma is positive for CD20 and CD79a and negative for CD5, CD10, CD23, and cyclin D1. In addition, lymphoepithelial lesions, colonization of reactive follicles by monocytoid cells, and plasmacytic differentiation were observed in the transitional epithelium.[8,24] In this study, the clinical symptoms, pathological histomorphology, and immunophenotype of the patients were found to be consistent with MALT lymphoma.
To date, an optimal treatment strategy for primary bladder MALT lymphoma has not been determined because of the rarity of the disease. Of all the cases in this study, 89.5% of patients present of localized (stage I) disease. A wide variety of methods were treated and most cases had positive outcomes, with a mean follow-up duration of 4.9 years (range: 0.2–40 years) (Table 1). Combined with literature reports, we recommend that surgery like TURBT be tried first, followed by chemotherapy, or radiotherapy alone, or combination therapy. Radiotherapy alone proved effective in only 68.8% (11 of 16) patients. As for the chemotherapy regimen, rituximab (anti-CD20 monoclonal antibody) has been shown to be useful for MALT lymphoma, with a remission rate of 55% to 73%.[49] In the present case, the patient just underwent TURBT and She has remained disease-free without any additional treatment after the surgery (15-month follow-up). However, by accumulating more cases and long-term follow-up, the best treatment and prognosis of the disease can be better understood.
4. Conclusion
In summary, primary bladder MALT lymphoma is a rare tumor, which tends to be a solitary mass, most commonly occurring in the elderly women. Because of the lack of specific clinical symptoms, signs, and imaging findings, it is easily missed or misdiagnosed before achieving a histological confirmation. Surgery may be the best choice for both diagnosis and treatment. Primary bladder MALT lymphoma is an indolent tumor with a good overall prognosis. We need additional reports to improve our understanding of the disease and its management. Supplementary Table.
Author contributions
Dr. Baixin Shen and Dr. Zhongqing Wei contributed equally to the work.
Conceptualization: Zhongqing Wei, Baixin Shen.
Data curation: Zhongqing Wei, Baixin Shen.
Formal analysis: Hewei Xu.
Funding acquisition: Zhongqing Wei, Baixin Shen.
Investigation: Hewei Xu.
Methodology: Hewei Xu.
Software: Zhengsen Chen.
Supervision: Zhongqing Wei, Baixin Shen.
Writing – original draft: Hewei Xu.
Supplementary Material
Footnotes
Abbreviations: CT = computed tomography, MALT = mucosa-associated lymphoid tissue, TURBT = transurethral resection of bladder tumors.
How to cite this article: Xu H, Chen Z, Shen B, Wei Z. Primary bladder mucosa-associated lymphoid tissue lymphoma: A case report and literature review. Medicine. 2020;99:28(e20825).
Informed written consent was obtained from the patient for publication of this case report and accompanying images.
Grant support: This work was supported by grants from National Natural Science Foundation of China (No. 81400758).
The authors have no funding and conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
The datasets generated during and/or analyzed during the current study are publicly available.
References
- [1].Anderson J, Armitage J, Berger F. A clinical evaluation of the International Lymphoma Study Group classification of non-Hodgkin's lymphoma. The Non-Hodgkin's Lymphoma Classification Project. Blood 1997;89:3909–18. [PubMed] [Google Scholar]
- [2].Hajime K, Zyun T, Taizan S, et al. Primary malignant lymphoma of the urinary bladder. Acta Pathol Jpn 1990;40:764–9. [DOI] [PubMed] [Google Scholar]
- [3].Pawade J, Banerjee SS, Harris M, et al. Lymphomas of mucosa-associated lymphoid tissue arising in the urinary bladder. Histopathology 1993;23:147–51. [DOI] [PubMed] [Google Scholar]
- [4].Fernandez AM, Martin RC, Lopez GJ, et al. Primary malignant lymphoma of the bladder. Report of three cases. Pathol Res Pract 1996;192:160–3. 164-165. [DOI] [PubMed] [Google Scholar]
- [5].Kempton CL, Kurtin PJ, Inwards DJ, et al. Malignant lymphoma of the bladder: evidence from 36 cases that low-grade lymphoma of the MALT-type is the most common primary bladder lymphoma. Am J Surg Pathol 1997;21:1324–33. [DOI] [PubMed] [Google Scholar]
- [6].Gallardo J, Gamargo C, Fodor M, et al. [MALT lymphoma of the bladder: report of a case]. Rev Med Chil 1998;126:199–201. [PubMed] [Google Scholar]
- [7].Ando K, Matsuno Y, Kanai Y, et al. Primary low-grade lymphoma of mucosa-associated lymphoid tissue of the urinary bladder: a case report with special reference to the use of ancillary diagnostic studies. Jpn J Clin Oncol 1999;29:636–9. [DOI] [PubMed] [Google Scholar]
- [8].Bates AW, Norton AJ, Baithun SI. Malignant lymphoma of the urinary bladder: a clinicopathological study of 11 cases. J Clin Pathol 2000;53:458–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Kawakami K, Oka K, Kato M, et al. Whole-bladder irradiation and doxorubicin-containing chemotherapy as successful treatment for a primary mucosa-associated lymphoid tissue lymphoma of the bladder. Int J Hematol 2000;72:346–8. [PubMed] [Google Scholar]
- [10].Tasu JP, Geffroy D, Rocher L, et al. Primary malignant lymphoma of the urinary bladder: report of three cases and review of the literature. Eur Radiol 2000;10:1261–4. [DOI] [PubMed] [Google Scholar]
- [11].Al-Maghrabi J, Kamel-Reid S, Jewett M, et al. Primary low-grade B-cell lymphoma of mucosa-associated lymphoid tissue type arising in the urinary bladder: report of 4 cases with molecular genetic analysis. Arch Pathol Lab Med 2001;125:332–6. [DOI] [PubMed] [Google Scholar]
- [12].Wazait HD, Chahal R, Sundurum SK, et al. MALT-type primary lymphoma of the urinary bladder: clinicopathological study of 2 cases and review of the literature. Urol Int 2001;66:220–4. [DOI] [PubMed] [Google Scholar]
- [13].Tsang RW, Gospodarowicz MK, Pintilie M, et al. Stage I and II MALT lymphoma: results of treatment with radiotherapy. Int J Radiat Oncol Biol Phys 2001;50:1258–64. [DOI] [PubMed] [Google Scholar]
- [14].van den Bosch J, Kropman RF, Blok P, et al. Disappearance of a mucosa-associated lymphoid tissue (MALT) lymphoma of the urinary bladder after treatment for Helicobacter pylori. Eur J Haematol 2002;68:187–8. [DOI] [PubMed] [Google Scholar]
- [15].Krober SM, Aepinus C, Ruck P, et al. Extranodal marginal zone B cell lymphoma of MALT type involving the mucosa of both the urinary bladder and stomach. J Clin Pathol 2002;55:554–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Hughes M, Morrison A, Jackson R. Primary bladder lymphoma: management and outcome of 12 patients with a review of the literature. Leukemia Lymphoma 2005;46:873–7. [DOI] [PubMed] [Google Scholar]
- [17].Takahara Y, Kawashima H, Han YS, et al. [Primary mucosa-associated lymphoid tissue (MALT) lymphoma of the urinary bladder]. Hinyokika Kiyo 2005;51:45–8. [PubMed] [Google Scholar]
- [18].Hatano K, Sato M, Tsujimoto Y, et al. [Primary mucosa-associated lymphoid tissue (MALT) lymphoma of the urinary bladder associated with left renal pelvic carcinoma: a case report]. Hinyokika Kiyo 2007;53:57–60. [PubMed] [Google Scholar]
- [19].Ueno Y, Sakai H, Tsuruta T, et al. Mucosa-associated lymphoma of the bladder with relapse in the stomach after successful local treatment. Hinyokika Kiyo 2007;53:575–9. [PubMed] [Google Scholar]
- [20].Fujimura M, Chin K, Sekita N, et al. Regression of mucosa-associated lymphoid tissue lymphoma of the bladder after antibiotic therapy: a case report. Hinyokika Kiyo 2008;54:783–6. [PubMed] [Google Scholar]
- [21].Schniederjan SD, Osunkoya AO. Lymphoid neoplasms of the urinary tract and male genital organs: a clinicopathological study of 40 cases. Modern Pathol 2009;22:1057–65. [DOI] [PubMed] [Google Scholar]
- [22].Sen S, Macaulay JH, Allford SL. A case of cerebral arteriovenous malformation in pregnancy associated with MALT lymphoma. J Obstet Gynaecol V 30 2010;308–10. [DOI] [PubMed] [Google Scholar]
- [23].Terada T. Primary CD5-positive mucosa-associated lymphoid tissue lymphoma of the urinary bladder. Ann Diagn Pathol 2011;15:382–4. [DOI] [PubMed] [Google Scholar]
- [24].Doglioni C, Ponzoni M, Ferreri AJ, et al. Gastric lymphoma: the histology report. Dig Liver Dis 2011;43: Suppl 4: S310–8. [DOI] [PubMed] [Google Scholar]
- [25].Maninderpal KG, Amir FH, Azad HA, et al. Imaging findings of a primary bladder maltoma. Br J Radiol 2011; 1005;84:e186–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Szopiński TR, Sudoł Szopińska I, Dzik T, et al. Incidental sonographic detection of mucosa-associated lymphoid tissue lymphoma of the urinary bladder found in a very young woman: report of a case. J Clin Ultrasound 2011;39:233–5. [DOI] [PubMed] [Google Scholar]
- [27].Morita K, Nakamura F, Nannya Y, et al. Primary MALT lymphoma of the urinary bladder in the background of interstitial cystitis. Ann Hematol 2012;91:1505–6. [DOI] [PubMed] [Google Scholar]
- [28].Mayer EK, Undre S, Cohen DC, et al. An unusual urological tumour: above the collar and below the belt. Case Rep Oncol Med 2012;2012:480826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Lucioni M, Nicola M, Riboni R, et al. Antibiotic therapy-induced remission of bladder mucosa-associated lymphoid tissue (MALT) lymphoma carrying t(11;18)(q21;q21) apoptosis inhibitor 2-MALT1. J Clin Oncol 2013;31:e304–6. [DOI] [PubMed] [Google Scholar]
- [30].Bacalja J, Ulamec M, Rako D, et al. Persistence of primary MALT lymphoma of the urinary bladder after rituximab with CHOP chemotherapy and radiotherapy. In vivo (Athens, Greece) 2013;27:545. [PubMed] [Google Scholar]
- [31].Takahashi H, Shimazaki H, Oda T, et al. Malignant lymphoma case with urinary cytology mimicking that of urothelial carcinoma. Cytopathology 2013;24:412–4. [DOI] [PubMed] [Google Scholar]
- [32].Mizuno K, Nakanishi S, Sakatani T, et al. A case of primary mucosa-associated lymphoid tissue-type lymphoma of the urinary bladder that progressed after antibiotic therapy. Hinyokika Kiyo 2013;59:239–42. [PubMed] [Google Scholar]
- [33].Haddad-Lacle JEM, Haddad CJ, Villas B. A rare urinary bladder tumour. Case Reports 2014;2014(may15 1):r2013202994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Matsuda I, Zozumi M, Tsuchida YA, et al. Primary extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue type with malakoplakia in the urinary bladder: a case report. Int J Clin Exp Pathol 2014;7:5280–4. [PMC free article] [PubMed] [Google Scholar]
- [35].Vedovo F, Pavan N, Liguori G, et al. Incidence and distribution of lymphoid neoplasm of the urinary tract and male genital organs in an urban area of northern italy in the last decade. Urologia Journal 2014;81: 23_suppl: S20–3. [DOI] [PubMed] [Google Scholar]
- [36].Vempati P, Knoll MA, Alqatari M, et al. MALT Lymphoma of the Bladder: a Case Report and Review of the Literature. Case Reports in Hematology 2015;2015:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Hsu J, Lin C, Chen Y, et al. Primary mucosa-associated lymphoid tissue lymphoma of the urinary bladder. Kaohsiung J Med Sci 2015;31:388–9. [DOI] [PubMed] [Google Scholar]
- [38].Simpson W, Lopez A, Babbar P, et al. Primary bladder lymphoma, diffuse large B-cell type: Case report and literature review of 26 cases. Urol Ann 2015;7:268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Isono M, Sato A, Kimura F, et al. A case of mucosa-associated lymphoid tissue lymphoma of the bladder successfully treated with radiotherapy. Urol Case Rep 2017;16:1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Kadam PD, Han HC, Kwok JL. An uncommon case of mucosa-associated lymphoid tissue (MALT) tumor of the bladder. Int Urogynecol J 2018;30:1017–8. [DOI] [PubMed] [Google Scholar]
- [41].Cohen SM, Petryk M, Varma M, et al. Non-Hodgkin's lymphoma of mucosa-associated lymphoid tissue. Oncologist 2006;11:1100–17. [DOI] [PubMed] [Google Scholar]
- [42].Isaacson P, Wright DH. Malignant lymphoma of mucosa-associated lymphoid tissue. A distinctive type of B-cell lymphoma. Cancer-Am Cancer Soc 1983;52:1410–6. [DOI] [PubMed] [Google Scholar]
- [43].Park JB, Koo JS. Helicobacter pylori infection in gastric mucosa-associated lymphoid tissue lymphoma. World J Gastroenterol 2014;20:2751–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Kiesewetter B, Raderer M. Antibiotic therapy in nongastrointestinal MALT lymphoma: a review of the literature. Blood 2013;122:1350–7. [DOI] [PubMed] [Google Scholar]
- [45].Kuhara H, Tamura Z, Suchi T, et al. Primary malignant lymphoma of the urinary bladder. A case report. Acta Pathol Jpn 1990;40:764–9. [DOI] [PubMed] [Google Scholar]
- [46].Venyo AK. Lymphoma of the urinary bladder. Adv Urol 2014;2014:327917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Chen YR, Hung LY, Chang KC. Mucosa-associated lymphoid tissue-type lymphoma presenting as a urethral caruncle with urinary bladder involvement. Int J Urol 2014;21:1073–4. [DOI] [PubMed] [Google Scholar]
- [48].Oscier D, Bramble J, Hodges E, et al. Regression of mucosa-associated lymphoid tissue lymphoma of the bladder after antibiotic therapy. J Clin Oncol 2002;20:882. [DOI] [PubMed] [Google Scholar]
- [49].Conconi A, Martinelli G, Thieblemont C, et al. Clinical activity ofrituximab in extranodal marginal zone B-cell lymphoma of MALT type. Blood 2003;102:2741–5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


