Abstract
The difference between the female and male immune response to COVID-19 infection, and infections in general, is multifactorial. The well-known determiners of the immune response, such as X and Y chromosomes, sex hormones, and microbiota, are functionally interconnected and influence each other in shaping the organism's immunity. We focus our commentary on the interplay between the genetic sex and mitochondria and how this may affect a sex-dependent immune response in COVID-19 infection. Realizing the existence of these interactions may help in designing novel methods or fine-tuning the existing and routine therapies to fight COVID-19 and other infections.
Keywords: COVID-19, SARS-CoV-2, Macrophages, Y chromosome, X chromosome, Immunity, Melatonin
Introduction
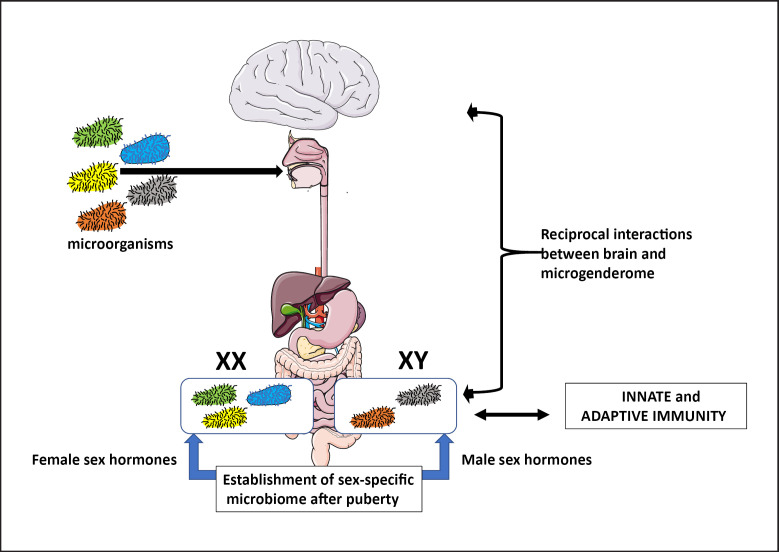
Research and clinical studies indicate that the genetic sex of patients influences the immune response, and the course, and prognosis of many common noninfectious and infectious diseases. A similar correlation has also been observed recently in COVID-19-infected patients; the worldwide statistical analyses of COVID-19 cases indicate that the rate of infection and the direness of the outcome are much higher and severe in males than in females. The most popular explanation for this phenomenon is “the immunocompetence handicap model” proposing that in males, the testosterone-dependent secondary male sex traits develop at the expense of the immune response. Sex hormones are known to affect the innate and adaptive immunological response with the androgens being anti-inflammatory, and the estrogens both pro-inflammatory and anti-inflammatory [1, 2]. However, the mechanisms of these sex-related differences are multifactorial and depend on very complex reciprocal interactions between sex chromosome-encoded and regulatory factors, hormones, and microbiota inhabiting the human body. In the last decade, it became clear that the microorganisms inhabiting the human gastrointestinal tract differ, in the type and abundance of species, between the sexes. This sex-dependent microbiome, called the microgenderome, develops after puberty when the sex hormones kick in and regulates local and systemic inflammation, and response to infection (Fig. 1) [1, 2, 3]. Recent studies also indicate that the sex-related difference in the immune response may depend on the sexually dimorphic populations of mitochondria. Below we give a short summary of how these different elements pitch in and shape the immune response to COVID-19 and other diseases.
Fig. 1.
Microgenderome effect on the immune system. The microorganisms acquired during birth, and from the environment (air and food) colonize the human body, especially the digestive system. After puberty, the sex hormones influence the abundance and variety of species inhabiting the male and female body; less variety in males than in females. The compounds produced by the microgendorome reciprocally influence the function of innate and adaptive immunity, and brain (adapted from Vemuri et al. [2]).
X and Y Chromosome Regulation of Immunity
Although some differences between the female and male immune response are directly related to the number of X chromosomes (2 X in females vs. 1 X in males), and the effect of sex hormones on the functions of immune cells, the studies of last decade indicate that both Y and X chromosomes regulate immune cell transcription and translation (transcriptome and proteome) profiles.
X Chromosome
The Archive.ensabl.org 2017: http://mar2017.archive.ensembl.org/Homo_sapiens/Location/Chromosome?r=X [4] indicate that the human chromosome X consists of over 150 million DNA base pairs and contains more than 800 protein-coding genes, which include the highest number of the innate and adaptive immunity-related genes of the whole human genome, and several hundred non-coding genes. The immune response genes include fraktaline receptor CXCR3 (C-X-C motif chemokine receptor 3) that directs immune cells, including macrophages, movement into inflamed tissues, and organs; the gene for CD80 ligand that binds to the CD40 receptor on antigen-presenting cells, B cells, monocytes/macrophages, and dendritic cells, and through interaction with CD154 transduces signals for T-dependent B-cell activation; and the interleukin-1 receptor-associated kinase 1 (IRAK1) gene. The X chromosome also contains 10% of all genomic microRNA (miRNA) genes that regulate expression and degradation of autosomal gene products [5, 6]. Studies showed that the absence of, or extensive deletions in one of the X chromosomes, lead to a variety of autoimmune diseases (Fig. 2) [5, 6].
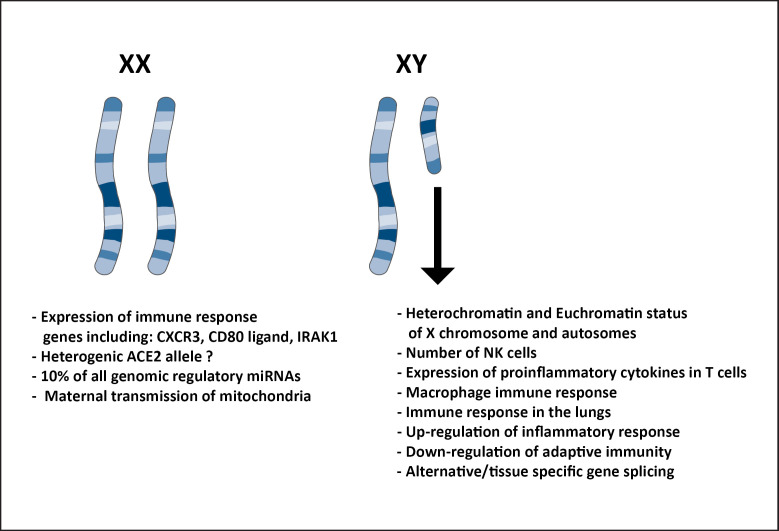
Fig. 2.
Effect of sex chromosomes on the immune-related functions. The X chromosome contains many immune response-related genes and 10% of all genomic miRNAs that regulate transcription, splicing, and degradation of many genes. It also, through the specification of female identity, directs maternal purging and transmission of mitochondria. Because in the female cells, the inactivation of one of the X chromosomes is random, the female body may contain different alleles of the same gene. For example, different alleles of viral receptor ACE2 may have a different affinity to the virus, which will affect the anti-viral immune response. The Y chromosome regulates many different immune-response functions, immune cell numbers, and immune cell phenotypes through the regulation of transcriptionally inert (heterochromatin) and active (euchromatin) status of X chromosome and autosomes.
A higher rate of COVID-19 infection in males may be, in part, influenced by the X chromosome mosaicism in the female cells, due to the stochastic X chromosome inactivation [7]. For example, the angiotensin-converting enzyme 2 (ACE2), the receptor for β-type coronaviruses SARS-CoV-1 and SARS-CoV-2, is encoded by the ACE2 gene located on the X chromosome. It is possible that some alleles of this gene may code for the receptors with different efficiency of recognizing and binding the virus. Male cells always express a single ACE2 allele because all cells contain an identical X chromosome. In contrast, a female has a heterogenic ACE2 allele because of the mosaicism of X chromosomes, which are stochastically distributed between the cells. Thus, in the female, a potentially more efficient form of ACE2 receptor would be present in only half of all cells. This may limit infectibility with SARS-CoV-1 and SARS-CoV-2 viruses and, to some extent, give females a relative resistance to the infection (Fig. 2). It has also been debated if such ACE2 polymorphism may have an impact on hypertension and other diseases [8, 9].
Y Chromosome
The human Y chromosome is much smaller than the X chromosome, consist of around 60 million DNA base pairs, and, in the majority of animals, its large portion is transcriptionally silent (heterochromatic). The Y chromosome is mainly composed of transposable elements, repeat sequences (comprising over 50% of its content), multicopy genes such as the polymorphic variants of the ribosomal genes, and a low number of protein-encoding genes, which are mainly male-specific and regulate sexual development, spermatogenesis, sex ratio, and fertility, and often evolved through the transposition/translocation from the autosomes. This male-specific region of the Y chromosome (MSY) does not recombine and, thus, remains unchanged between the consecutive male generations [10, 11, 12, 13]. Studies showed that Y chromosome can regulate the heterochromatin/euchromatin status of the autosomes and X chromosomes and, thus, affects silencing/expression of various genes, including the immune response genes, and regulate the tissue-/cell-specific alternative gene splicing [10, 14, 15, 16, 17, 18]. Although the mechanism by which the Y chromosome influences heterochromatin/euchromatin content and thus the transcription of the other genes is largely unknown, one of the hypotheses postulates that the Y chromosome sequesters heterochromatinization factors and another that it affects the architecture of cell nucleus, which makes specific genes inaccessible to the transcription factors [19, 20, 21, 22]. Phylogenetic studies showed that the males with the haplogroup I, which is one of the most popular European lineages of the Y chromosome, have upregulated inflammatory response, downregulated adaptive immunity, and a higher risk of coronary diseases [23, 24, 25]. In the murine models, Y chromosomes influence the number of natural killer T cells, the gene expression pattern in CD4+ T cells, the immune response of macrophages, and the mortality rate following the infection with coxsackievirus [26, 27, 28], which argues for the strong impact of the Y chromosome on a large variety of immune cells and immune processes. Studies of Case et al. [10] showed that the copy number of the Y chromosome gene Sly and RNA-binding motif gene Rbmy inversely regulates the susceptibility to autoimmune disease. Studies in mouse influenza model [29] showed that certain genetic variants of chromosome Y result in higher susceptibility to influenza A infection, activate pro-inflammatory cytokine expression in T cells, and increase pathogenic immune response in the lungs (Fig. 2).
Mitochondria
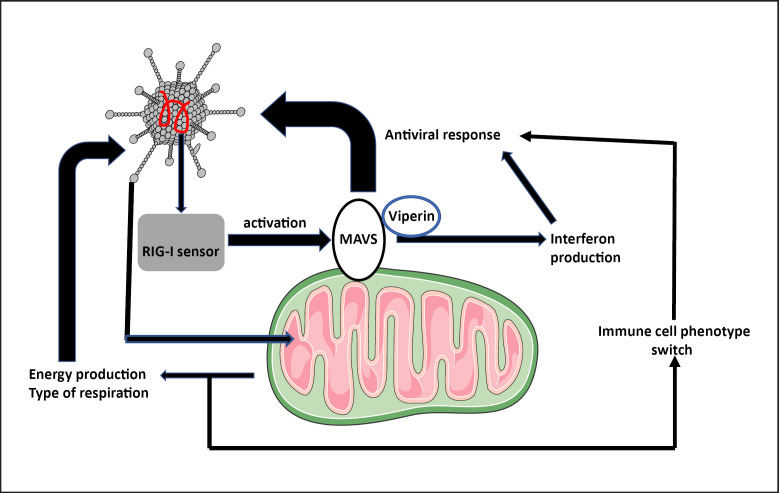
Studies of the past decades [30, 31] showed that mitochondria are not only the bioenergetic (they generate ATP) and biosynthetic (they generate components for the synthesis of various macromolecules) hubs but are also indispensable regulators of the innate and adaptive immune response, development, and maintenance/survival and activation of the specific phenotypes of immune cells. Mitochondria can also affect various signaling pathways and transcription in immune cells by changing the ATP level, alternating their metabolic pathways, and releasing the reactive oxygen species and mitochondrial DNA signals. By changing the type of respiration from the broken TCA cycle to β-Oxidation, the mitochondria can switch macrophage phenotype from the proinflammatory (M1) to the anti-inflammatory (M2). In addition, the localization of mitochondria in the proximity of endoplasmic reticulum membranes of the immune cells directly affects their metabolism and immune-related functions [30, 31]. Also, the outer membrane of mitochondria contains the mitochondrial antiviral signaling (MAVS) protein that is activated by the viral RNA sensor, the retinoic acid-inducible gene I (RIG-I) that senses the presence of viral RNA. MAVS can also act as an antiviral defense mechanism. In the macrophages infected with RNA viruses, MAVS interacts with the antiviral protein viperin, affecting the level of antiviral compound interferon (Fig. 3) [30, 32]. Proper functioning of mitochondrial MAVS response can be especially relevant and significant for COVID-19 infection where the SARS-CoV-2 virus directly infects alveolar macrophages inducing them to switch on the cytokine storm in the lungs [33]. Moreover, because the survival and replication of the virus depend on the energy produced by the host mitochondria, which in turn, are affected by the virus (Fig. 3); the novel antiviral strategies may include compounds that modulate mitochondrial bioenergetic functions [34].
Fig. 3.
Effect of mitochondria on the anti-viral immune response. The presence of the virus is sensed by the RIG-I that is a major sensor of viral RNA. This activates anti-viral MAVS protein present in the mitochondrial membrane. Activated MAVS, through the interaction with the virus inhibitory protein, viperin, affects the level of interferon, which in turn regulates virus replication. In addition, viruses can directly affect mitochondrial functions such as aerobic or anaerobic respiration, which in turn affect immune cell phenotypes and responses.
All these data indicate that the healthy and properly functioning mitochondria are indispensable for the adequacy of the immune response. Thus, it is not surprising that one of the theories explaining the higher infection rate and severity of infections, such as COVID-19, in males relates to the maternal transmission of mitochondria, and substandard quality of mitochondria in the males. In mammals, including humans, mitochondria are maternally transmitted in the egg cytoplasm. Following fertilization, during early embryogenesis, maternal mitochondria replicate and enter the prospective somatic and germ cells [20]. Although there are some, very rare, examples of paternal transmission of mitochondria in humans [35], the concept of maternal inheritance of mitochondrial DNA in humans remains valid. During the formation and maturation of the mammalian egg, the mitochondria undergo the quality control [36] and those which are defective, or contain, harmful for the female, mutations, are eliminated. Because this mitochondrial culling is female-biased, the mitochondria remaining in the egg cytoplasm may contain mutations harmful for the male. This so-called “mother curse” [20] may also influence the quality and caliber of a male immune response.
Recently, the melatonin was suggested as a potential adjuvant for COVID-19 treatment [37]. Melatonin has positive effects on mitochondrial homeostasis by scavenging toxic oxygen species and nitrogen-based reactants, enhancing anti-oxidative enzymes, facilitating the electron transport chain, limiting electron leakage, free radical generation, and stimulating ATP synthesis [38]. In light of our hypothesis that the quality of mitochondria may influence COVID-19 infection, the melatonin treatment of COVID-19 patients may be more beneficial for men than women. Although, at present, there is no proven effective remedy for the sex-biased outcome of COVID-19 and other microbial infections, the detailed knowledge of all mechanisms underlying the differences between female and male immune response should facilitate the development of new treatments and therapeutic approaches.
Disclosure Statement
Authors do not have conflict of interest and have nothing to disclose.
Funding Sources
Support from the Polish Ministry of National Defense project “Kościuszko” # 5508/2017/DA to J.Z.K.
Authors Contributions
Malgorzata Kloc: concept, writing, and figures. Jacek Z. Kubiak: concept, writing, editing, and figures. Rafik Mark Ghobrial: writing and editing.
Acknowledgements
We acknowledge that some of the images used to make figures were from the Servier Medical ART: SMART, smart.servier.com. We also acknowledge the support from the Polish Ministry of National Defense project “Kościuszko” # 5508/2017/DA to JZK.
References
- 1.Klein SL, Flanagan KL. Sex differences in immune responses. Nat Rev Immunol. 2016;16((10)):626–38. doi: 10.1038/nri.2016.90. [DOI] [PubMed] [Google Scholar]
- 2.Vemuri R, Sylvia KE, Klein SL, Forster SC, Plebanski M, Eri R, et al. The microgenderome revealed: sex differences in bidirectional interactions between the microbiota, hormones, immunity and disease susceptibility. Semin Immunopathol. 2019;41((2)):265–75. doi: 10.1007/s00281-018-0716-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Steegenga WT, Mischke M, Lute C, Boekschoten MV, Pruis MG, Lendvai A, et al. Sexually dimorphic characteristics of the small intestine and colon of prepubescent C57BL/6 mice. Biol Sex Differ. 2014;5:11. doi: 10.1186/s13293-014-0011-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Archive.ensembl.org/Homo_sapiensChromosome X: 1-1 − Chromosome summary − Homo sapiens. http://mar2017.archive.ensembl.org/Homo_sapiens/Location/Chromosome?r=X.
- 5.Bianchi I, Lleo A, Gershwin ME, Invernizzi P. The X chromosome and immune associated genes. J Autoimmun. 2012;38((2–3)):J187–92. doi: 10.1016/j.jaut.2011.11.012. [DOI] [PubMed] [Google Scholar]
- 6.Schurz H, Salie M, Tromp G, Hoal EG, Kinnear CJ, Möller M. The X chromosome and sex-specific effects in infectious disease susceptibility. Hum Genom. 2019;13((1)):2. doi: 10.1186/s40246-018-0185-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lyon MF. Gene action in the X-chromosome of the mouse (Mus musculus L.) Nature. 1961;190:372–3. doi: 10.1038/190372a0. [DOI] [PubMed] [Google Scholar]
- 8.Benjafield AV, Wang WY, Morris BJ. No association of angiotensin-converting enzyme 2 gene (ACE2) polymorphisms with essential hypertension. Am J Hypertens. 2004;17((7)):624–8. doi: 10.1016/j.amjhyper.2004.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pan Y, Wang T, Li Y, Guan T, Lai Y, Shen Y, et al. Association of ACE2 polymorphisms with susceptibility to essential hypertension and dyslipidemia in Xinjiang, China. Lipids Health Dis. 2018;17((1)):241. doi: 10.1186/s12944-018-0890-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Case LK, Wall EH, Dragon JA, Saligrama N, Krementsov DN, Moussawi M, et al. The Y chromosome as a regulatory element shaping immune cell transcriptomes and susceptibility to autoimmune disease. Genome Res. 2013;23((9)):1474–85. doi: 10.1101/gr.156703.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Koerich LB, Wang X, Clark AG, Carvalho AB. Low conservation of gene content in the Drosophila Y chromosome. Nature. 2008;456((7224)):949–51. doi: 10.1038/nature07463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Quintana-Murci L, Fellous M. The human Y chromosome: the biological role of a “functional Wasteland”. J Biomed Biotechnol. 2001;1((1)):18–24. doi: 10.1155/S1110724301000080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Skaletsky H, Kuroda-Kawaguchi T, Minx PJ, Cordum HS, Hillier L, Brown LG, et al. The male-specific region of the human Y chromosome is a mosaic of discrete sequence classes. Nature. 2003;423((6942)):825–37. doi: 10.1038/nature01722. [DOI] [PubMed] [Google Scholar]
- 14.Lemos B, Araripe LO, Hartl DL. Polymorphic Y chromosomes harbor cryptic variation with manifold functional consequences. Science. 2008;319((5859)):91–3. doi: 10.1126/science.1148861. [DOI] [PubMed] [Google Scholar]
- 15.Lemos B, Branco AT, Hartl DL. Epigenetic effects of polymorphic Y chromosomes modulate chromatin components, immune response, and sexual conflict. Proc Natl Acad Sci U S A. 2010;107((36)):15826–31. doi: 10.1073/pnas.1010383107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Paredes S, Branco AT, Hartl DL, Maggert KA, Lemos B. Ribosomal DNA deletions modulate genome-wide gene expression: “rDNA-sensitive” genes and natural variation. PLoS Genet. 2011;7((4)):e1001376. doi: 10.1371/journal.pgen.1001376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Piergentili R. Multiple roles of the Y chromosome in the biology of Drosophila melanogaster. ScientificWorldJournal. 2010;10:1749–67. doi: 10.1100/tsw.2010.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhou J, Sackton TB, Martinsen L, Lemos B, Eickbush TH, Hartl DL. Y chromosome mediates ribosomal DNA silencing and modulates the chromatin state in Drosophila. Proc Natl Acad Sci U S A. 2012;109((25)):9941–6. doi: 10.1073/pnas.1207367109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Francisco FO, Lemos B. How do Y-chromosomes modulate genome-wide epigenetic states: genome folding, chromatin sinks, and gene expression. J Genom. 2014;2:94–103. doi: 10.7150/jgen.8043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Silkaitis K, Lemos B. Sex-biased chromatin and regulatory cross-talk between sex chromosomes, autosomes, and mitochondria. Biol Sex Differ. 2014;5((1)):2. doi: 10.1186/2042-6410-5-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Taddei A, Hediger F, Neumann FR, Gasser SM. The function of nuclear architecture: a genetic approach. Annu Rev Genet. 2004;38:305–45. doi: 10.1146/annurev.genet.37.110801.142705. [DOI] [PubMed] [Google Scholar]
- 22.Ye Q, Worman HJ. Interaction between an integral protein of the nuclear envelope inner membrane and human chromodomain proteins homologous to Drosophila HP1. J Biol Chem. 1996;271((25)):14653–6. doi: 10.1074/jbc.271.25.14653. [DOI] [PubMed] [Google Scholar]
- 23.Charchar FJ, Bloomer LD, Barnes TA, Cowley MJ, Nelson CP, Wang Y, et al. Inheritance of coronary artery disease in men: an analysis of the role of the Y chromosome. Lancet. 2012;379((9819)):915–22. doi: 10.1016/S0140-6736(11)61453-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Khan SI, Andrews KL, Jennings GL, Sampson AK, Chin-Dusting JPF. Y chromosome, hypertension and cardiovascular disease: is inflammation the answer? Int J Mol Sci. 2019;20((12)):2892. doi: 10.3390/ijms20122892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maan AA, Eales J, Akbarov A, Rowland J, Xu X, Jobling MA, et al. The Y chromosome: a blueprint for men's health? Eur J Hum Genet. 2017;25((11)):1181–8. doi: 10.1038/ejhg.2017.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Case LK, Toussaint L, Moussawi M, Roberts B, Saligrama N, Brossay L, et al. Chromosome Y regulates survival following murine coxsackievirus B3 infection. G3. 2012;2((1)):115–21. doi: 10.1534/g3.111.001610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Teuscher C, Noubade R, Spach K, McElvany B, Bunn JY, Fillmore PD, et al. Evidence that the Y chromosome influences autoimmune disease in male and female mice. Proc Natl Acad Sci U S A. 2006;103((21)):8024–9. doi: 10.1073/pnas.0600536103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Spach KM, Blake M, Bunn JY, McElvany B, Noubade R, Blankenhorn EP, et al. Cutting edge: the Y chromosome controls the age-dependent experimental allergic encephalomyelitis sexual dimorphism in SJL/J mice. J Immunol. 2009;182((4)):1789–93. doi: 10.4049/jimmunol.0803200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Krementsov DN, Case LK, Dienz O, Raza A, Fang Q, Ather JL, et al. Genetic variation in chromosome Y regulates susceptibility to influenza A virus infection. Proc Natl Acad Sci U S A. 2017;114((13)):3491–6. doi: 10.1073/pnas.1620889114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Angajala A, Lim S, Phillips JB, Kim J-H, Yates C, You Z. Diverse roles of mitochondria in immune responses: novel insights into immuno-metabolism. Front Immunol. 2018;9:1605. doi: 10.3389/fimmu.2018.01605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Weinberg SE, Sena LA, Chandel NS. Mitochondria in the regulation of innate and adaptive immunity. Immunity. 2015;42((3)):406–17. doi: 10.1016/j.immuni.2015.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hee JS, Cresswell P. Viperin interaction with mitochondrial antiviral signaling protein (MAVS) limits viperin-mediated inhibition of the interferon response in macrophages. PLoS One. 2017;12((2)):e0172236. doi: 10.1371/journal.pone.0172236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang C, Xie J, Zhao L, Fei X, Zhang H, Tan Y, et al. Alveolar macrophage activation and cytokine storm in the pathogenesis of severe COVID-19. 2020. www.researchsquare.com. [DOI] [PMC free article] [PubMed]
- 34.El-Bacha T, Da Poian AT. Virus-induced changes in mitochondrial bioenergetics as potential targets for therapy. Int J Biochem Cell Biol. 2013;45((1)):41–6. doi: 10.1016/j.biocel.2012.09.021. [DOI] [PubMed] [Google Scholar]
- 35.Luo S, Valencia CA, Zhang J, Lee N-C, Slone J, Gui B, et al. Biparental inheritance of mitochondrial DNA in humans. Proc Natl Acad Sci U S A. 2018;115((51)):13039–44. doi: 10.1073/pnas.1810946115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lieber T, Jeedigunta SP, Palozzi JM, Lehmann R, Hurd TR. Mitochondrial fragmentation drives selective removal of deleterious mtDNA in the germline. Nature. 2019;570((7761)):380–4. doi: 10.1038/s41586-019-1213-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhang R, Wang X, Ni L, Di X, Ma B, Niu S, et al. COVID-19: melatonin as a potential adjuvant treatment. Life Sci. 2020;250:117583. doi: 10.1016/j.lfs.2020.117583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Leon J, Acuña-Castroviejo D, Sainz RM, Mayo JC, Tan DX, Reiter RJ. Melatonin and mitochondrial function. Life Sci. 2004;75((7)):765–90. doi: 10.1016/j.lfs.2004.03.003. [DOI] [PubMed] [Google Scholar]