Abstract
Objective
Continuing to utilize healthcare as needed during an epidemic outbreak is significant, in general, and especially for cancer patients. Therefore, this study aimed to explore factors associated with health services utilization among breast cancer patients during the coronavirus disease (COVID-19) outbreak.
Method
A cross-sectional online survey was conducted among 151 women with breast cancer. Participants completed measures of perceived health status, perceived susceptibility to COVID-19, anxiety, coping resources, health services utilization (contact with healthcare professionals and cancellation of an appointment to the oncology/hematology clinic), and socio-demographic questionnaires. A multiple hierarchical regression was calculated; contact with healthcare professionals was the dependent variable. In addition, a logistic regression was calculated; cancellation of an appointment to the oncology/hematology clinic because of the COVID-19 was the dependent variable.
Results
Breast cancer patients’ contact with healthcare professionals was lower than their contact prior to the pandemic. A higher extent of contact with healthcare professionals was related to patients’ perception of health as bad/reasonable, lower perceived susceptibility, a lower sense of mastery, and higher social support. In addition, the odds of cancelling an appointment to the oncology/hematology clinic were higher in the presence of additional chronic illnesses and a higher sense of mastery.
Significance of results
The results could provide public health agencies with a more complete picture of the impact of the COVID-19 epidemic among breast cancer patients. This is significant because, in the event that COVID-19 re-emerges, the findings of the current study could help guide public health officials and possibly prevent the future avoidance of health services’ use among this high-risk population.
Key words: Anxiety, Breast cancer, Coping resources, COVID-19, Health services utilization, Perceived susceptibility
Background
Israel and the rest of the world are currently experiencing an outbreak of the novel coronavirus disease (COVID-19) (Guo et al., 2020). Accordingly, on January 30, 2020, the World Health Organization declared the outbreak of COVID-19 a Public Health Emergency of International Concern. The first Israeli person with COVID-19 was diagnosed on February 21, 2020. Since then, in Israel, thousands of individuals have been isolated in their homes, thousands have been diagnosed, and, as of May 7, 2020, 239 individuals have died from this virus.
Cumulative knowledge indicates that cancer patients are more susceptible to COVID-19 than individuals without cancer. This is due to these patients’ systemic immunosuppressive state, caused by the malignancy and anticancer treatments, such as chemotherapy or surgery (Liang et al., 2020; Porzio et al., 2020). Therefore, these patients are likely at increased risk of COVID-19 and have a poorer general prognosis (Liang et al., 2020). However, it should be noted that there is currently insufficient evidence to draw conclusive associations between cancer and COVID-19 (Xia et al., 2020). Nevertheless, this study is focused on breast cancer in the context of COVID-19, as breast cancer is the most common cancer and also the primary cause of mortality due to cancer in female around the World (Waks and Winer, 2019). More than 1.8 million new breast cancer cases are diagnosed every year worldwide (Tasnim et al., 2018).
Overall, it seems that one of the main risks for cancer patients, and among them breast cancer, is the inability to receive routine medical care in hospitals because of the urgency and priority to treat COVID-19 patients (Shankar et al., 2020; Xia et al., 2020). In addition, travel restrictions have made it difficult for some cancer patients to reach the hospital. Moreover, the fear of infection while visiting the hospital has caused many others to simply cancel their appointments (Curigliano et al., 2020). Consequently, patients with cancer might not be utilizing the health services they need, which might affect their health condition (Shankar et al., 2020). To understand this phenomenon, the current study attempts to explore factors associated with health services utilization among Israeli breast cancer patients during the COVID-19 outbreak.
This study is based on the Stress and Coping Model developed (Lazarus and Folkman, 1986), which proposes that the physical and psychological health outcomes of coping with chronic and intense stressors are affected by appraisals of the stressors and coping resources. In this study, perceived stressors were conceptualized as perceived susceptibility, as this factor may influence willingness and motivation to adopt health behavior (Shinan-Altman and Levkovich, 2020). Perceived susceptibility has been used to measure perceptions of the likelihood of experiencing a disease or a virus (Bolton et al., 2019). Overall, the COVID-19 pandemic has not only introduced the risk and susceptibility of becoming ill from the viral infection, but also led to unbearable psychological pressure (Duan and Zhu, 2020; Xiao, 2020). Indeed, previous research examining adverse psychological reactions to COVID-19 among the Israeli lay public reported high levels of stress, fear, and worry (Levkovich and Shinan-Altman, 2020). Therefore, breast cancer patients, who are at increased risk of infection from the virus, may also experience negative emotional responses. Previous research found that higher negative emotional responses during the COVID-19 outbreak were associated with higher health-promoting behavior (Shinan-Altman and Levkovich, 2020).
Coping resources, such as sense of mastery and social support, were shown to reduce negative psychological reactions. Coping resources are relatively stable characteristics of a person's disposition and the environment (Taylor and Stanton, 2007). They refer to the individual's available resources, which can be used to help cope with stressful events (Taylor and Stanton, 2007). In this study, we examined sense of mastery (an internal resource) and social support (an external resource), two coping resources that have consistently been found in the literature to be related to health services utilization (King et al., 2015; Gyasi et al., 2020). Sense of mastery refers to the perceived control of individuals over their future, their appreciation of cause–effect relationships, and their perceived ability to cope with life stressors (Pearlin and Schooler, 1978; Hobfoll and Walfisch, 1984). Social support is defined as the knowledge that one is cared for and respected, and is part of a social network of people who are concerned with one's safety (Sarason et al., 1983).
Both cognitive (perceived susceptibility) and emotional matters, together with coping resources, have an important bearing on handling health threats (Zhang et al., 2014). Yet, research literature regarding these concepts in the area of COVID-19 is only now beginning to emerge, and to our knowledge, no study to date has examined these factors among breast cancer patients during the COVID-19 outbreak. Therefore, the aim of the current study was to examine the associations linking perceived health status, perceived susceptibility of COVID-19, anxiety, and coping resources with health services utilization among breast cancer patients during the outbreak of COVID-19. This aim is especially important, given that the health services utilization of these patients may help improve their health indicators, especially during a virus outbreak.
Methods
Procedure
Prior to commencing the study, authorization was obtained from Bar-Ilan University's Ethics Committee (Authorization No. 032003). The study is a cross-sectional online survey. To minimize personal contact during the outbreak, the questionnaires were administered through the Qualtrics online platform. A total of 153 Israelis visited the online survey between April 5, 2020 and April 12, 2020. Inclusion criteria were persons who were diagnosed with breast cancer in the last 5 years, aged 18+; and Hebrew speakers. Exclusion criteria were responses to the items in a similar pattern or not completing the questionnaire in its entirety (n = 2).
Measures
Dependent variable
Health services utilization was measured using two dimensions:
-
1.
Contact with healthcare professionals: It was measured using a 6-item scale. Three items refer to the degree of contact with an oncologist/family physician/nurse prior to the COVID-19 outbreak; three additional items refer to the degree of contact with an oncologist/family physician/nurse during the COVID-19 outbreak. Participants were asked to indicate the extent of their contact with these healthcare professionals on a 5-point Likert scale ranging from 1 = not at all to 5 = very often (e.g., “To what extent were you in contact with your oncologist/family physician/nurse prior to the outbreak of COVID-19?”). Two composite indices were created: contact with healthcare professionals prior to the COVID-19 outbreak (α = 0.62) and contact with healthcare professionals during the COVID-19 outbreak (α = 0.66). A higher score in both indices indicates a higher frequency of contact with healthcare professionals.
-
2.
Cancelling an appointment to the oncology or hematology clinic: participants were asked to indicate whether they had cancelled an appointment because of the COVID-19 outbreak (no = 0, yes = 1).
Independent variables
Perceived susceptibility was assessed based on a previous study conducted among the general public during the COVID-19 outbreak (Shinan-Altman and Levkovich, 2020) using a one-item measure examining the extent to which the participant thinks he/she will contract the virus. “How likely do you think it is that you will contract COVID-19?” Answers were rated on a 5-point Likert-type scale, ranging from 1 = not at all likely to 5 = very likely.
Anxiety was measured based on The Brief Symptom Inventory; an 18-item measure consists of three subscales: somatization, depression, and anxiety (Derogatis and Savitz, 1999). In this study, only the anxiety subscale (six items) was used. Participants were asked to indicate to what extent they experienced each item in the last week on a 4-point Likert scale ranging from 0 = not at all to 3 = very often (e.g., “Suddenly scared for no reason”). The mean score was calculated; a high score indicated greater levels of anxiety (Cronbach's α = 0.91).
Sense of mastery was assessed by a 7-item scale measuring the ability to deal with or exert control over issues as they arise in people's lives (Pearlin and Schooler, 1978). Participants were asked to indicate the extent to which they agreed or disagreed with each item on a 5-point Likert scale ranging from 1 = strongly disagree to 5 = strongly agree (e.g., “What happens to me in the future mostly depends on me”). The mean score was calculated; a high score indicated greater levels of sense of mastery (Cronbach's α = 0.81).
Social support was assessed by the Multidimensional Scale of Perceived Social Support (Zimet et al., 1988), a 12-item scale. Participants were asked to indicate the extent to which they agreed or disagreed with each item on a 5-point Likert scale ranging from 1 = strongly disagree to 5 = strongly agree (e.g., “My family really tries to help me”). The mean score was calculated; a high score indicated greater levels of perceived social support (Cronbach's α = 0.94).
Socio-demographic variables included gender, age, years of education, marital status, number of children, and home isolation since the outbreak of COVID-19 (yes/no).
Health information included perceived health status (bad/reasonable/good) — recoded into bad and reasonable = 0 vs. good = 1, time since diagnosis, and other chronic diseases (yes/no).
Statistical analyses
Data were analyzed using SPSS version 25. Descriptive statistics were used to describe the participants’ demographic characteristics and the research variables. Pearson correlations were calculated to assess the associations between the research variables. A multiple hierarchical regression was calculated; contact with healthcare professionals was the dependent variable. Age and other chronic diseases (yes/no) were entered in the first step, perceived health in the second step, perceived susceptibility in the third step, anxiety in the fourth step, and coping resources (sense of mastery and social support) in the fifth and final steps. A logistic regression was similarly calculated; cancellation of an appointment to the oncology or hematology clinic because of the COVID-19 outbreak was the dependent variable.
Results
The study included 151 women with breast cancer. The mean age was about 51 years (range 23–86), and the average of education was approximately 15.4 years (range 10–25). Most were married (64%) with a mean of two children. About half of the participants reported being in isolation since the COVID-19 outbreak. In addition, the perceived health status of half of the participants was moderate, and 35% of the participants had other additional diseases. Among these, other additional diseases were 41.4% hypertension, 17.1% diabetes, 15.7% coronary heart disease, and 25.7% other diseases. In addition, 31% reported cancelling a health services appointment due to the COVID-19 outbreak.
According to Table 1, the mean score for contact with healthcare professionals during the COVID-19 outbreak was 2.08 (SD = 0.85, range 1–4.67), meaning that the contact with the healthcare professionals score was relatively low during the COVID-19 outbreak. A total of 30% of the participants cancelled an appointment to the oncology or hematology clinic because of the COVID-19 outbreak. Reasons for cancelling an appointment to the oncology or hematology clinics were fear to contract the virus (93%), forgetfulness (4%), and lack of urgency (3%). In addition, the mean score of perceived susceptibility was moderate, while the mean score for anxiety was relatively low. Sense of mastery and social support were relatively high.
Table 1.
Correlates, means, SDs, and ranges of study variables (n = 151)
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|
| 1. Contact with healthcare professionals | – | ||||||
| 2. Cancelling an appointment due to COVID-19 | 0.02 | – | |||||
| 3. Perceived health status | −0.18* | −0.10 | – | ||||
| 4. Perceived susceptibility | −0.02 | 0.18* | −0.24*** | – | |||
| 5. Anxiety | 0.16* | 0.20** | −0.31*** | 0.34*** | – | ||
| 6. Sense of mastery | −0.15* | −0.21** | 0.24*** | −0.20** | −0.56*** | – | |
| 7. Social support | 0.01 | −0.15* | 0.15* | −0.10 | −0.30*** | 0.38*** | – |
| Mean | 2.64 | 0.30 | 0.43 | 2.46 | 2.04 | 3.44 | 3.91 |
| SD | 0.77 | 0.46 | 0.50 | 0.95 | 0.67 | 0.69 | 0.88 |
| Possible range | 1–5 | 0–1 | 0–1 | 1–5 | 1–5 | 1–5 | 1–5 |
| Actual range | 1–5 | 0–1 | 0–1 | 1–5 | 1–4 | 1–5 | 1–5 |
p < 0.05.
p < 0.01.
p < 0.001.
Associations between the study variables
According to Table 1, negative associations were found linking perceived health status and sense of mastery with contact with healthcare professionals, while a positive association was found between anxiety and contact with healthcare professionals. In other words, participants with perceived bad to reasonable health status, a lower sense of mastery, and higher anxiety had more contact with healthcare professionals during the COVID-19 pandemic.
In addition, negative associations were found linking perceived health status, sense of mastery, and social support with cancelling an appointment to the oncology or hematology clinic because of the COVID-19 outbreak. This means that participants who did not cancel an appointment to the oncology or hematology clinic during the COVID-19 outbreak perceived their health status as being bad to reasonable and had a higher sense of mastery and higher levels of social support. In addition, participants who cancelled an appointment to the oncology or hematology clinic during the COVID-19 outbreak had higher perceived susceptibility and higher anxiety levels.
Contact with healthcare professionals
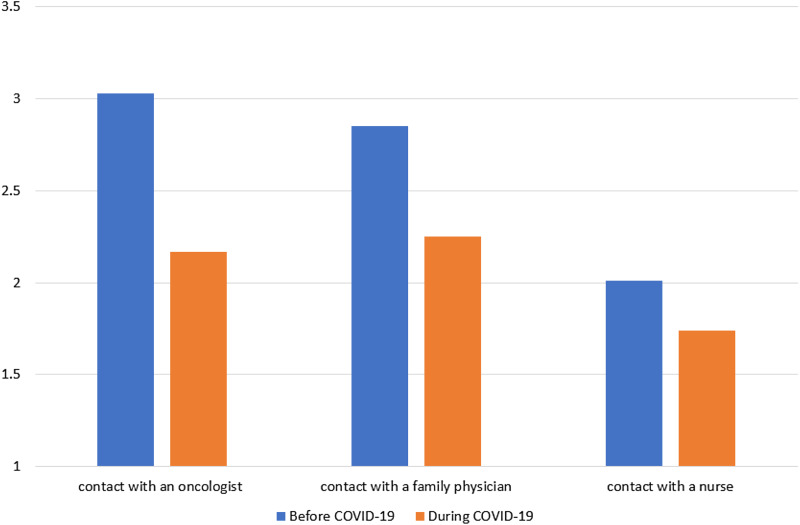
Four paired-samples t-tests were conducted separately to evaluate the changes in contact with healthcare professionals before and during the COVID-19 outbreak (Table 2). A statistically significant decrease was found in being in contact with an oncologist before the COVID-19 outbreak (M = 3.03, SD = 0.98) and during the COVID-19 outbreak (M = 2.17, SD = 1.15), t(146) = 10.60, p < 0.001 (Pair 1). In addition, a statistically significant decrease was found in being in contact with a family physician before the COVID-19 outbreak (M = 2.85, SD = 0.97) and during the COVID-19 outbreak (M = 2.25, SD = 1.12), t(148) = 7.65, p < 0.001 (Pair 2). Furthermore, a statistically significant decrease was found in being in contact with a nurse before the COVID-19 outbreak (M = 2.01, SD = 1.07) and during the COVID-19 outbreak (M = 1.74, SD = 1.01), t(147) = 4.65, p < 0.001 (Pair 3). Finally, a statistically significant decrease was found in the mean of all three pairs before the COVID-19 outbreak (M = 2.63, SD = 0.76) and during the COVID-19 outbreak (M = 2.07, SD = 0.85), t(148) = 10.65, p < 0.001 (Pair 4) (Figure 1).
Table 2.
Paired-samples t-test for contact with healthcare professionals before and during the COVID-19 outbreak (n = 151)
| 95% Confidence interval of the difference | ||||||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | SEM | Lower | Upper | t | df | Sig. | |
| Pair 1 | 0.85 | 1.11 | 0.08 | 0.69 | 1.01 | 10.60 | 189 | p < 0.001 |
| Pair 2 | 0.59 | 1.08 | 0.07 | 0.44 | 0.74 | 7.65 | 192 | p < 0.001 |
| Pair 3 | 0.27 | 0.79 | 0.05 | 0.15 | 0.38 | 4.65 | 188 | p < 0.001 |
| Total score | 0.57 | 0.74 | 0.05 | 0.46 | 0.67 | 10.74 | 196 | p < 0.001 |
Note: Pair 1 — contact with an oncologist; Pair 2 — contact with a family physician; Pair 3 — contact with a nurse.
Fig. 1.
Means of contact with healthcare professionals before and during the COVID-19 outbreak. Note: Possible range: 1 not at all to 5 very often 1–5; all three differences between “before COVID-19” and “during COVID-19” are statistically significant (p < 0.001).
Contact with healthcare professionals during the COVID-19 outbreak was marginally related to age (r = −0.13, p = 0.063), negatively related to years of education (r = −0.22, p = 0.003), and unrelated to the number of children (r = 0.05, p = 0.526). No differences were found between married and non-married participants (t(149) = 1.20, p = 0.231), and between participants with or without additional chronic illnesses (t(149) = 0.17, p = 0.868).
Cancelling an appointment to the oncology or hematology clinic was not associated with age (r = 0.04, p = 0.553), years of education (r = −0.01, p = 0.983), and number of children (r = −0.11, p = 0.130). In addition, no differences were found between married and non-married participants (χ2(1) = 0.44, p = 0.30). A significant difference was found between participants with and without additional chronic illnesses (χ2(1) = 20.60, p < 0.001).
Regression analysis for identifying contact with healthcare professionals correlation
Due to the correlations and differences noted above, the analyses were calculated while controlling for age and the presence of additional chronic illnesses (years of education was related to contact with healthcare professionals, but was excluded due to missing data. Its inclusion did not change the results).
The results in Table 3 show that the regression model for contact with healthcare professionals during the COVID-19 outbreak is significant, but the explained variance is low. It appears that a higher extent of contact with healthcare professionals was related to patients’ perception of their health as being bad or reasonable (but not good), lower perceived susceptibility, a lower sense of mastery, and higher social support.
Table 3.
Regression analysis for contact with healthcare professionals during the COVID-19 outbreak (n = 151)
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
|---|---|---|---|---|---|
| β | β | β | β | β | |
| Age | −0.12 | −0.12 | −0.14 | −0.14 | −0.13 |
| Other diseases | 0.03 | −0.02 | −0.01 | −0.02 | 0.01 |
| Perceived health status | −0.18* | −0.21** | −0.18* | −0.17* | |
| Perceived susceptibility | −0.13 | −0.17* | −0.18* | ||
| Anxiety | 0.16* | 0.09 | |||
| Sense of mastery | −0.20* | ||||
| Social support | 0.16* | ||||
| Adj. R2 | 0.002 | 0.028* | 0.038* | 0.053** | 0.079** |
p < 0.05.
p < 0.01.
The results in Table 4 show that the regression model for cancellation of an appointment to the oncology or hematology clinic is significant, with about 22% of explained variance. The odds of cancelling an appointment to the oncology or hematology clinic were higher in the presence of additional chronic illnesses and a higher sense of mastery.
Table 4.
Logistic regression analysis for appointment cancellation (n = 151)
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
|---|---|---|---|---|---|
| OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | |
| Age | 0.99 (0.96,1.02) | 0.99 (0.96,1.02) | 0.99 (0.97,1.03) | 0.99 (0.97,1.03) | 0.99 (0.97,1.03) |
| Additional diseases | 4.36** (2.23,8.54) | 4.27** (2.14,8.54) | 4.05** (2.01,8.17) | 3.90** (1.92,7.92) | 3.99** (1.92,8.27) |
| Perceived health status | 0.92 (0.46,1.83) | 1.06 (0.52,2.16) | 1.24 (0.59,2.59) | 1.38 (0.65,2.95) | |
| Perceived susceptibility | 1.39 (0.96,2.02) | 1.26 (0.86,1.85) | 1.24 (0.84,1.83) | ||
| Anxiety | 1.56 (0.91,2.68) | 1.06 (0.56,2.00) | |||
| Sense of mastery | 0.50* (0.26,0.93) | ||||
| Social support | 0.82 (0.55, 1.24) | ||||
| Nagelkerke R2 | 0.138** | 0.138** | 0.160** | 0.177** | 0.221** |
p < 0.05.
p < 0.001.
Discussion
This study represents an attempt to delineate the complex processes related to encouraging breast cancer patients who need treatments to take advantage of healthcare services during the COVID-19 outbreak. Therefore, the objective of the current study was to examine the association linking perceived health status, perceived susceptibility of COVID-19, anxiety, and coping resources (sense of mastery and social support) with health services utilization among patients with breast cancer during this outbreak.
Our findings indicate that breast cancer patients’ contact with healthcare professionals was less frequent during the COVID-19 outbreak, compared with prior to the pandemic. This finding is worrisome because reduced healthcare utilization (e.g., less contact with healthcare professionals) was found to be associated with lower health outcomes (Wang et al., 2012). Lower health services utilization was also found in 2003, during the Severe Acute Respiratory Syndrome (SARS) epidemic (Chang et al., 2004). Because of the rapid transmission of the virus and limited knowledge about it, people were afraid to seek healthcare services and preferred to avoid exposure to the disease (Lu et al., 2007).
In this study, a higher extent of contact with healthcare professionals was associated with the self-perception of one's health status as bad or reasonable and with low perceived susceptibility. It should be noted that one important factor affecting whether a patient decides to seek out medical advice is when the relative benefits outweigh the costs (Lu et al., 2007). According to the current study, for breast cancer patients, the benefits of going to healthcare providers were outweighed by the risk of being infected by COVID-19.
In this study, the bivariate associations revealed a significant association between anxiety and contact with healthcare professionals during the COVID-19 outbreak. However, in the regression analyses, controlling for background variables, the associations between anxiety and contact with healthcare professionals became non-significant. This suggests that the remaining significant factors examined in this study might account for the associations at the bivariate level. The insignificant association between anxiety and contact with healthcare professionals is in contrast to previous studies (e.g., Tremblay et al., 2018). There are two possible explanations for this finding in the current study. Firstly, the anxiety levels found among the current study's sample were relatively low, meaning anxiety did not have a major influence on the decision to utilize healthcare services during the virus outbreak. Secondly, it is possible that the findings in this study relate to the selected measure and/or the self-report nature of the study method. Therefore, it is recommended that future studies will examine whether anxiety among breast cancer patients may predict contact with healthcare professionals during a pandemic outbreak using a longitudinal design.
In contrast to the Stress and Coping Model's assumption (Lazarus and Folkman, 1986), a lower sense of mastery was associated with more frequent contact with healthcare professionals, meaning patients who feel they have less control prefer to put their health into the hands of healthcare professionals. These individuals seem to derive something reassuring from this, in addition to their continued relationship with their healthcare professionals, especially in a situation of uncertainty and lack of control such as that of the COVID-19 pandemic. This finding is in line with a previous study conducted among healthcare professionals of cancer patients, which found that the support of healthcare teams increases patients’ experience of certainty, safety, and dependability, which, in turn, strengthens their internal sense of control (Rohrmoser et al., 2017). In addition, this study indicates that the odds of cancelling an appointment to the oncology or hematology clinic were higher for participants with a higher sense of mastery. In other words, cancer patients who felt higher levels of control had a greater tendency to cancel appointments with their healthcare professionals. It is even possible that cancelling the appointment caused them to feel a greater sense of control over their situation.
In the current study, more frequent contact with healthcare professionals was related to higher social support. This finding is in line with the Stress and Coping model's assumption (Lazarus and Folkman, 1986), which argues that positive buffers such as social support may enable individuals to perform positive behaviors, such as seeking out medical services (Sellars et al., 2010). It seems that during a virus outbreak, when social distancing and social isolation requirements are established, the importance of social support increases. Accordingly, social support plays an important role as a gatekeeper for cancer patients’ health by supporting them to continue to utilize the health services they need, despite the epidemic.
Finally, our findings indicate that the odds of cancelling an appointment to the oncology or hematology clinic were higher among comorbidities patients. Indeed, it was found that the presence and number of comorbidities is associated with the poorer clinical outcome in patients with COVID-19 (Mao et al., 2020). In a recent study of 1,099 patients with laboratory-confirmed COVID-19, 23.7% of the patients with COVID-19 reported having at least one comorbidity, with hypertension, diabetes, and coronary heart disease being the most common (Porzio et al., 2020). These diseases were also the most common diseases in the current study.
Certain limitations in the current study deserve consideration. First, this is a cross-sectional study; therefore, causal interpretations cannot be made. Second, we used a correlational design, thereby limiting our capacity to demonstrate causal relationships. Finally, the variables examined in our study explained only a small proportion of the variance of the dependent variable — contact with healthcare professionals. This indicates the need to include additional variables in future studies in an attempt to better explain the complexity of contact with healthcare professionals during a pandemic crisis among cancer patients.
Despite these limitations, this study has important clinical implications. According to the study's results, clinical interventions targeting breast cancer patients’ perceived health status, perceived susceptibility of COVID-19, and coping resources may encourage breast cancer patients to utilize health services during an epidemic outbreak. For health professionals, this study is useful as it allows for a greater understanding of the profiles of those who chose to reduce/cancel their medical care appointments during the outbreak. In addition, the results could provide public health agencies with a more complete picture of the impact of the COVID-19 epidemic among breast cancer patients. This is especially important because, in the event that COVID-19 re-emerges, this study's findings could help guide health professionals and prevent the avoidance of health services utilization among this high-risk population. In addition, health services should be prepared accordingly to provide the necessary care breast cancer patients need during these types of crises, while reducing any possibility of them contracting the virus.
Conclusions
This study is the first to examine the influence of perceived health status, perceived susceptibility of COVID-19, anxiety, and coping resources on health services utilization among breast cancer patients during an epidemic outbreak. As such, this article represents a unique contribution to the existing literature, because it highlights the characteristics and factors that encourage/discourage breast cancer patients from seeing medical care professionals during a virus outbreak, such as the COVID-19 pandemic.
It is recommended to carry out future longitudinal studies, which will examine symptoms and other psychosocial factors that may affect health services utilization over longer periods and among larger samples, in order to build tailored intervention programs in the event of the recurrence of a virus outbreak, such as that of COVID-19.
Conflict of interest
The authors declare that there is no conflict of interest.
REFERENCES
- Bolton CD, Sunil TS, Hurd T, et al. (2019) Hispanic men and women's knowledge, beliefs, perceived susceptibility, and barriers to clinical breast examination and mammography practices in South Texas Colonias. Journal of Community Health 44(6), 1069–1075. [DOI] [PubMed] [Google Scholar]
- Chang HJ, Huang N, Lee CH, et al. (2004) The impact of the SARS epidemic on the utilization of medical services: SARS and the fear of SARS. American Journal of Public Health 94(4), 562–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curigliano G, Cardoso MJ, Poortmans P, et al. (2020) Recommendations for triage, prioritization and treatment of breast cancer patients during the COVID-19 pandemic. The Breast 52, 8–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis LR and Savitz KL (1999) The SCL-90-R, brief symptom inventory, and matching clinical rating scales In Maruish ME (ed.), The Use of Psychological Testing for Treatment Planning and Outcomes Assessment, 2nd ed., Mahwah, NJ: Lawrence Erlbaum Associates Publishers, pp. 679–724. [Google Scholar]
- Duan L and Zhu G (2020) Psychological interventions for people affected by the COVID-19 epidemic. The Lancet Psychiatry 7(4), 300–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo YR, Cao QD, Hong ZS, et al. (2020) The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak: An update on the status. Military Medical Research 7(1), 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gyasi RM, Phillips DR and Amoah PA (2020) Multidimensional social support and health services utilization among noninstitutionalized older persons in Ghana. Journal of Aging and Health 32(3-4), 227–239. [DOI] [PubMed] [Google Scholar]
- Hobfoll SE and Walfisch S (1984) Coping with a threat to life: A longitudinal study of self-concept, social support, and psychological distress. American Journal of Community Psychology 12(1), 87–100. [DOI] [PubMed] [Google Scholar]
- King A, Wardecker BM and Edelstein RS (2015) Personal mastery buffers the effects of childhood sexual abuse on women's health and family functioning. Journal of Family Violence 30(7), 887–897. [Google Scholar]
- Lazarus RS and Folkman S (1986) Cognitive theories of stress and the issue of circularity In Mortimer HA and Richard T (eds), Dynamics of Stress. Boston, MA: Springer, pp. 63–80. [Google Scholar]
- Levkovich I and Shinan-Altman S (2020). COVID-19—Stress and psychological impact among the Israeli public: A mixed-methods study. Submitted.
- Liang W, Guan W, Chen R, et al. (2020) Cancer patients in SARS-CoV-2 infection: A nationwide analysis in China. The Lancet Oncology 21(3), 335–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu TH, Chou YJ and Liou CS (2007) Impact of SARS on healthcare utilization by disease categories: Implications for delivery of healthcare services. Health Policy 83(2-3), 375–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mao R, Liang J, Shen J, et al. (2020) Implications of COVID-19 for patients with pre-existing digestive diseases. The Lancet Gastroenterology and Hepatology 5(5), 426–428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearlin LI and Schooler C (1978) The structure of coping. Journal of Health and Social Behavior 19(1), 2–21. [PubMed] [Google Scholar]
- Porzio G, Cortellini A, Bruera E, et al. (2020) Home care for cancer patients during COVID-19 pandemic: The “double triage” protocol. Journal of Pain and Symptom Management 60(1), 5–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohrmoser A, Preisler M, Bär K, et al. (2017) Early integration of palliative/supportive cancer care—Healthcare professionals’ perspectives on the support needs of cancer patients and their caregivers across the cancer treatment trajectory. Supportive Care in Cancer 25(5), 1621–1627. [DOI] [PubMed] [Google Scholar]
- Sarason IG, Levine HM, Basham RB, et al. (1983) Assessing social support: The social support questionnaire. Journal of Personality and Social Psychology 44(1), 127. [Google Scholar]
- Sellars B, Garza MA, Fryer CS, et al. (2010) Utilization of health care services and willingness to participate in future medical research: The role of race and social support. Journal of the National Medical Association 102(9), 776–786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shankar A, Saini D, Roy S, et al. (2020) Cancer care delivery challenges amidst coronavirus disease–19 (COVID-19) outbreak: Specific precautions for cancer patients and cancer care providers to prevent spread. Asian Pacific Journal of Cancer Prevention 21(3), 569–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shinan-Altman S and Levkovich I (2020) COVID-19 precautionary behavior: The Israeli case in the initial stage of the outbreak. Submitted. [DOI] [PMC free article] [PubMed]
- Tasnim F, Jannat F, Kibria S, et al. (2018) Electromagnetic performances analysis of a microwave imaging system (MIS) for breast tumor detection In 2018 International Conference on Innovations in Science, Engineering and Technology (ICISET). Chittagong, Bangladesh: IEEE, pp. 442–446. [Google Scholar]
- Taylor SE and Stanton AL (2007) Coping resources, coping processes, and mental health. Annual Review Clinical Psychology 3, 377–401. [DOI] [PubMed] [Google Scholar]
- Tremblay MA, Denis I, Turcotte S, et al. (2018) Heart-focused anxiety and health care seeking in patients with non-cardiac chest pain: A prospective study. General Hospital Psychiatry 50, 83–89. [DOI] [PubMed] [Google Scholar]
- Waks AG and Winer EP (2019) Breast cancer treatment: A review. JAMA 321(3), 288–300. [DOI] [PubMed] [Google Scholar]
- Wang SY, Chen LK, Hsu SH, et al. (2012) Health care utilization and health outcomes: A population study of Taiwan. Health Policy and Planning 27(7), 590–599. [DOI] [PubMed] [Google Scholar]
- Xia Y, Jin R, Zhao J, et al. (2020) Risk of COVID-19 for patients with cancer. The Lancet Oncology 21(4), e180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao C (2020) A novel approach of consultation on 2019 novel coronavirus (COVID-19)-related psychological and mental problems: Structured letter therapy. Psychiatry Investigation 17(2), 175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang JM, Zhang D and Chock TM (2014) Effects of HIV/AIDS public service announcements on attitude and behavior: Interplay of perceived threat and self-efficacy. Social Behavior and Personality: An International Journal 42(5), 799–809. [Google Scholar]
- Zimet GD, Dahlem NW, Zimet SG, et al. (1988) The multidimensional scale of perceived social support. Journal of Personality Assessment 52(1), 30–41. [Google Scholar]