Abstract
Background
The coronavirus 2019 (COVID-19) pandemic has changed the practice of neurosurgery. Significant resources have been dedicated to the disease. The pandemic in the Indian subcontinent, compared with the rest of the world, is relatively delayed. The neurosurgical practice cannot remain unaffected by hugely disruptive measures such as a lockdown. The inevitable increase in COVID infections with the gradual relaxation of lockdown continues to pose a risk for health care providers. Therefore, it is imperative to evaluate whether the pandemic has had a discernible effect on health care providers, especially in terms of practice modifications in private establishments and publicly funded hospitals, the emotional impact on the surgeon, and the influence of social media on the psyche of the surgeon.
Methods
An online questionnaire-based survey was prepared, with questions related to the COVID-specific themes of precautions taken in outpatient services and operating theaters, the influence of social media, the economic loss incurred, and the perceptible impact of telemedicine and webinars. The links to the survey were mailed to neurosurgeons in private and public practice countrywide. The responses were anonymized to ensure free and unbiased answers to the survey questions.
Results
A total of 176 responses were received from across the Indian subcontinent. The median age of respondents was 39 years (range, 32–70 years) and the postresidency experience was 7 years (range, 0–34 years). Respondents were an equitable mix of public and private practitioners. Of respondents, 46% were practicing restricted outpatient services, more in public institutions (P = 0.22) which also had a higher incidence of tele-outpatient services (26% vs. 17%). Wearing surgical masks, N95 masks, and gloves were the most commonly practiced precautionary measures in outpatient services (>60%). Although private practitioners were continuing elective cases (40%), public institutes were more cautious, with only emergency patients being operated on (29%). The greatest fear among all practitioners was passing the infection to their family (75%). Social media were helpful for brainstorming queries and updating practice modifications, but some surgeons admitted to receiving threats on social media platforms (37.5%). Depression and economic losses were palpable for approximately 30% neurosurgeons.
Conclusions
The survey highlights the perception of neurosurgeons toward the pandemic and the difference in public–private practice. Suspension of elective procedures, severe curtailment of regular outpatient appointments, drastic modifications of the normal outpatient department/operating room practices, and apprehensions related to inadequacy of safety provided by personal protective equipment use and financial losses of private establishments were some of the visible themes in our survey results. Although telemedicine has not been as widely adopted as expected, online education has been favorably received.
Key words: Coronavirus, COVID-19, Neurosurgery, Social media
Abbreviations and Acronyms: COVID-19, Coronavirus disease 2019; OPD, Outpatient department; PPE, Personal protective equipment
Introduction
I understand that it's hard for everyone, but one cannot give in to emotions... we'll have to draw lessons from the current crisis and now we'll have to work on overcoming it.
Boris Yeltsin
The coronavirus 2019 (COVID-19) pandemic has irrevocably challenged the traditional perspectives and practices of neurosurgery. Medical services have been heavily scaled down during the lockdown as a huge amount of resources have been deployed to face the emerging epidemic. Hospitals rapidly reduced scheduled clinical and surgical activities and were forced to postpone nonemergent procedures. During this period, a significant shrinkage in access to the emergency department for both minor and major diseases has been observed, together with a precipitous decline in outpatient appointments.1 Perhaps the fear of contagion prevented patients, even with severe symptoms, from seeking care. Alternatively, patients may also have experienced difficulties in accessing medical services given the extraordinary commitment to treating the new disease and curbs on mobility of people.2 The lockdown imposed to contain the contagion had some unavoidable adverse consequences for health care delivery.3
In this context, the effect of the disease and its influence on the health care system continue to be felt daily.4 , 5 Neurosurgical practice is not untouched by the situation. There are reports from various parts of the world including Europe and North America regarding the change in neurosurgical practice during the COVID pandemic.6, 7, 8, 9 Neurosurgical patients needing intensive care may have been affected because most of the resources such as intensive care unit beds, ventilators, and intensivists were diverted to the care of patients with COVID.10 However, there are some major differences in the developed and developing world (e.g., the Indian subcontinent): a large and dense population, limited resources, and already strained health infrastructure.11 , 12 Recently, a few reports from the developing world13, 14, 15, 16, 17 have described the perception of neurosurgeons about the pandemic and changes in neurosurgical practice in the pandemic but there have been none from the Indian subcontinent. Hence, there was a need to understand the effect of the COVID epidemic on neurosurgical practice in the Indian subcontinent. Moreover, there is a fear of an alarming increase in the number of cases of violence against medical personnel as a result of a fear of contagion or frustration with the increasingly hamstrung health care system in the Indian subcontinent.
We surveyed practicing neurosurgeons in the Indian subcontinent about changes in neurosurgical practice during this pandemic. We also discuss unconventional issues such as the loss of economic remuneration, mental health worries, the impact of social media, and the surge of surveys and webinars. Our primary intent was to explore the disparity, if any, between private and publicly funded institutions, concerning the patterns of clinical neurosurgical practice and the use of personal protective equipment (PPE) during direct patient exposure. We also discuss the use of telemedicine in the Indian subcontinent.
Methods
We prepared a comprehensive online questionnaire with 26 questions with multiple choice answers and circulated it in various social media groups, focused e-mail lists, and direct messaging platforms consisting of neurosurgeons from the Indian subcontinent (India, Pakistan, Bhutan, Bangladesh, Nepal, and Sri Lanka). The total number of recipients of the survey was approximately 1000. The respondents were anonymized concerning name, place of practice, sex, and country of origin to obtain an unbiased opinion. Data were collected using Google Forms (Google LLC, Mountain View, California, USA) software online. Questions were divided into 3 broad areas:
-
1)
The pattern of neurosurgical practice during the COVID-19 pandemic
-
2)
Influence of social media and electronic learning platforms on neurosurgeons and their mental health
-
3)
The financial and emotional impact of the epidemic on neurosurgeons.
The statistical analysis was primarily descriptive. Data compiled on the online Google spreadsheet were analyzed with R (R Foundation for Statistical Computing, Vienna, Austria). The categorical variables were examined using χ2 statistics and the continuous variables were compared using a Welch t test. The responses collected on Likert scale patterns were studied using nonparametric tests (Wilcoxon rank sum test and Kruskal-Wallis test). Statistically significant differences have been reported.
Results
Responses
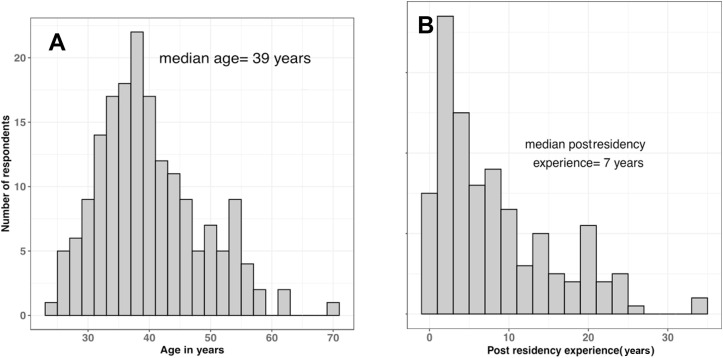
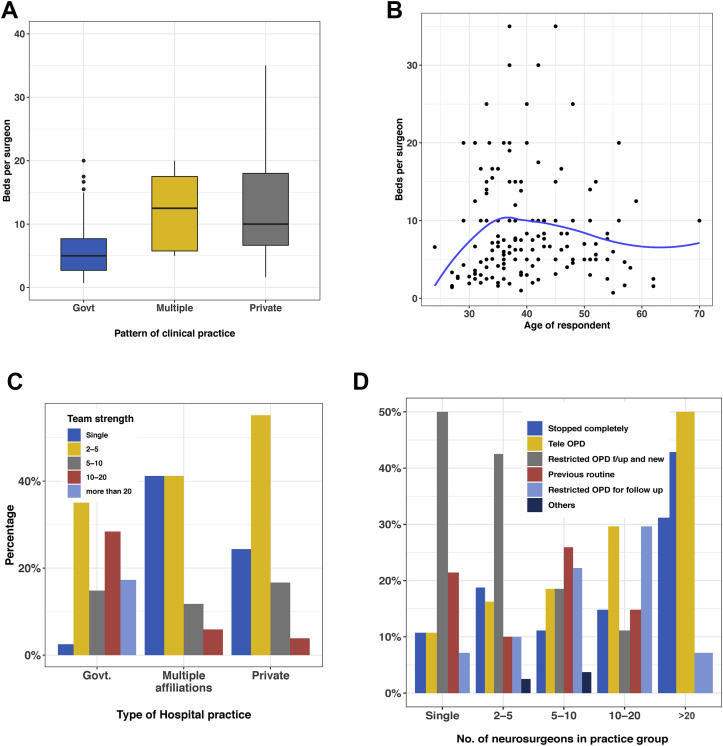
We received 176 responses from 1000 potential recipients (17.6% response rate) to the survey between May 1 and May 15, 2020. The respondents were equally distributed among government and private institutions (81 vs. 78 respondents, respectively) (Table 1 ) and had varying duration of experience after residency (Figure 1 ). The median age of the respondents was 39 years (range, 32–70 years) and the median postresidency experience was 7 years (range, 0–34 years). Most of the neurosurgeons had a median of approximately 7 beds (interquartile range, 9) to manage per head (Figure 2 ), with private neurosurgeons having more beds to manage per head than those in public institutions.
Table 1.
Characteristics of Respondents (N = 176)
| Type of Clinical Practice | n (%) |
|---|---|
| Government academic institute/teaching hospital | 77 (43.8) |
| Government nonacademic hospital | 4 (2.3) |
| Multiple affiliations | 17 (9.7) |
| Private academic institute | 33 (18.8) |
| Private nonacademic hospital | 45 (25.6) |
| Postresidency practice experience | |
| <3 years | 40 (23.3) |
| 3–6 years | 37 (21.5) |
| 6–10 years | 34 (19.8) |
| >10 years | 61 (35.5) |
| Strength of Neurosurgical Team | Type of Practice, n (%) |
||
|---|---|---|---|
| Government | Multiple Affiliations | Private | |
| Single | 2 (2.5) | 7 (41.2) | 19 (24.4) |
| 2–5 | 30 (37) | 7 (41.2) | 43 (55.1) |
| 5–10 | 12 (14.8) | 2 (11.8) | 13 (16.7) |
| 10–20 | 23 (28.4) | 1 (5.9) | 3 (3.8) |
| >20 | 14 (17.3) | ||
Figure 1.
(A) Age in years of respondents. (B) Postresidency experience in years.
Figure 2.
(A) Patterns of clinical practice of respondents. Govt, government. (B) Scatter plot of the inpatient bed strength per head in relation to the age of the respondent. (C) Team strength variations among public and private institutions. Govt, government. (D) Outpatient department (OPD) practice modifications compared across different team strengths.
Public–Private Disparity
There was a noticeable change in the outpatient department (OPD) practices of neurosurgeons, with most either restricting OPD (31.8%) or opting for tele-OPD (20.5%). Some stopped OPD services completely (17.6%). At the other end of the spectrum were a similar number of surgeons who continued their regular OPD practices (14.2%) (Table 2 ). The practice varied with the number of neurosurgeons in a group. Whereas single/sole practicing neurosurgeons opted for restriction of OPD numbers or follow-up cases or continued unchanged, groups with >10 neurosurgeons either stopped OPD completely or relied completely on tele-OPD. This difference can be attributed to the fact that most of the large neurosurgical practice groups belonged to public institutions and were obligated to close OPDs following government directives.
Table 2.
Changes in Outpatient Department Practices During COVID Epidemic (N=176)
| OPD Visit Patterns Across Practice Models | ||||
|---|---|---|---|---|
| OPD Practice | Government (n = 81), n (%) | Multiple Affiliations (n = 17), n (%) | Private (n = 78), n (%) | P Value |
| Stopped completely | 21 (25.9) | 3 (17.6) | 7 (9) | 0.001∗ |
| Tele-OPD | 21 (25.9) | 1 (5.9) | 14 (17.9) | |
| Restricted OPD follow-up and new | 11 (13.6) | 11 (64.7) | 34 (43.6) | |
| Previous routine | 8 (9.9) | 1 (5.9) | 16 (20.5) | |
| Restricted OPD for follow-up | 18 (22.2) | 1 (5.9) | 6 (7.7) | |
| Others | 2 (2.5) | 1 (1.3) | ||
| OPD Visit Patterns Compared Across Team Strength of Practicing Groups | ||||||
|---|---|---|---|---|---|---|
| OPD Practice | Single (n = 28) | 2–5 (n = 80) | 5–10 (n = 27) | 10–20 (n = 27) | >20 (n = 14) | P Value |
| Stopped completely | 3 (10.7) | 15 (18.8) | 3 (11.1) | 4 (14.8) | 6 (42.9) | 0.22 |
| Tele-OPD | 3 (10.7) | 13 (16.2) | 5 (18.5) | 8 (29.6) | 7 (50) | |
| Restricted OPD follow-up and new | 14 (50) | 34 (42.5) | 5 (18.5) | 3 (11.1) | ||
| Previous routine | 6 (21.4) | 8 (10) | 7 (25.9) | 4 (14.8) | ||
| Restricted OPD for follow-up | 2 (7.1) | 8 (10) | 6 (22.2) | 8 (29.6) | 1 (7.1) | |
| Personal Protective Equipment Use/Preventive Strategies Across Practice Groups | ||||
|---|---|---|---|---|
| Personal Protective Equipment/Strategies | Government (n = 81) | Multiple Affiliations (n = 17) | Private (n = 78) | P Value |
| Face shield | 1 (1.2) | 2 (11.8) | 6 (7.7) | 0.07 |
| Full personal protective equipment kit | 9 (11.1) | 2 (11.8) | 6 (7.7) | |
| Glass barrier | 9 (11.1) | 3 (17.6) | 10 (12.8) | |
| Gown/gloves | 20 (24.7) | 7 (41.2) | 26 (33.3) | |
| N95 mask | 17 (21) | 5 (29.4) | 29 (37.2) | |
| Prior screening | 0 (0) | 0 (0) | 4 (5.1) | |
| Surgical mask | 50 (61.7) | 11 (64.7) | 45 (57.7) | |
OPD, outpatient department.
Significant.
This theory is corroborated by observations comparing the OPD practices of private and public institutions. Of the government/public practitioners, 26% had stopped OPD completely and the same proportion had opted for tele-OPD services. In contrast, only 9% of private practitioners had found it feasible to suspend their OPDs; 17.9% had started tele-OPD (Table 2). These differences in the changing patterns of outpatient services were significant (P < 0.001) when compared across groups. This finding needs to be interpreted in the context that most respondents (61.3%) worked in smaller (<5 surgeons) groups. It is reflective of the type of neurosurgery practice in our subcontinent, which is still considerably individualized in the private sector. Although government institutions had an almost equitable distribution of the number of neurosurgeons between >10 and <10 groups (37 vs. 44), private practice was dominated by teams comprising 2–5 neurosurgeons per team (Figure 2D, Table 2).
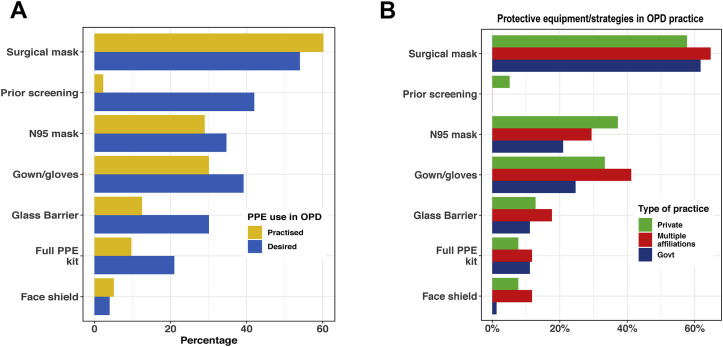
Personal Protective Precautions and Strategies
In outpatient clinics, ordinary surgical masks were used primarily, although the respondents believed that ideally N95 masks with gown/gloves and prior screening of cases should be adopted (Figure 3 ). Many neurosurgeons even expected glass barriers to be erected between them and their patients or even the use of full PPE kits in OPD for maximal protection. However, these protective measures were implemented sparingly when examined against the expectation of the clinicians (Figure 3, Table 2). Face shields were not popular either in use or in expectations in OPD probably because their prolonged use was considered to be cumbersome, even although face shields were made with surgical sterilization wraps to meet the Food and Drug Administration criterion of a bacterial filtration efficacy of 98.9%–99.9%. Apart from this finding, practice more or less matched expectations both in public and in private practice.
Figure 3.
(A) Personal protective equipment (PPE)/protection strategies used in outpatient department (OPD). (B) Personal protective equipment use/protection strategies used by different practice groups.
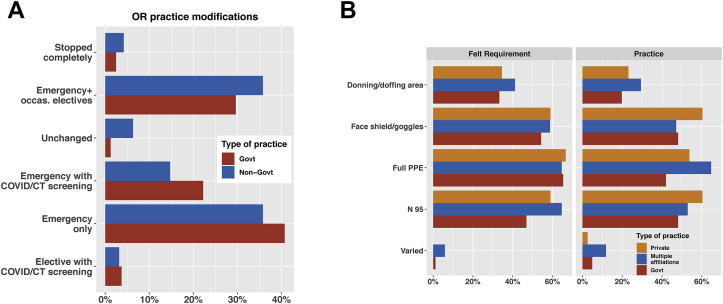
In operating theaters, too, the operative strategy shifted from elective and emergencies to mainly emergencies and occasional elective cases during the pandemic (Figure 4 , Table 4). Although government hospitals treated either only emergencies or emergencies with COVID testing, nongovernment organizations continued to perform occasional elective procedures or had their practice unchanged (i.e., they continued to perform occasional elective procedures) (Table 3 ). There was no difference in terms of the expectation of operating theater precautions with donning/doffing area, full PPE use, and face shields/goggles being expected by both private and government institutions (Figure 4, Table 4). However, in terms of practice, the private practitioner was more careful and had higher use of donning/doffing area (23.1% vs. 19.8%), full PPE use (53.8% vs. 42%), and face shields/goggles (60.3% vs. 48.1%) compared with government institutions.
Figure 4.
(A) Personal protective equipment use in operating theater. CT, computed tomography; Govt, government; occas, occasional; OR, operating room. (B) Felt need versus personal protective equipment use.
Table 4.
Emotional Aspects, Resumption of Practice, Social Media Use, and e-Learning
| Government (n = 81), n (%) | Multiple Affiliations (n = 17), n (%) | Private (n = 78), n (%) | |
|---|---|---|---|
| Biggest Fear During the Epidemic | |||
| Passing infection to family | 59 (72.8) | 13 (76.5) | 60 (76.9) |
| Hospital being sealed/taken over | 5 (6.2) | 2 (2.6) | |
| Becoming infected | 10 (12.3) | 1 (5.9) | 9 (11.5) |
| Financial | 7 (8.6) | 2 (11.8) | 5 (6.4) |
| All the above | 1 (5.9) | 2 (2.6) | |
| When Will You Restart Practice? | Pattern of Foreseeable Practice on Resumption | ||
|---|---|---|---|
| Don't know | 46 (26.1) | Continue semielective and elective with testing | 82 (46.6) |
| Financial obligation to restart | 14 (8) | Normal practice | 13 (7.4) |
| Post antiviral | 6 (3.4) | Only emergencies and that too with testing | 19 (10.8) |
| Post vaccine | 31 (17.6) | Very restricted practice (only emergency cases) | 51 (29) |
| Restricted for foreseeable future | 77 (43.8) | Miscellaneous | 11 (6.2) |
| Resumed with personal protective equipment | 2 (1.1) | ||
| Frequency of Receiving Threatening Messages on Social Media | |||
|---|---|---|---|
| Every day | 11 (13.6) | 1 (5.9) | 4 (5.1) |
| Once a month | 7 (8.6) | 1 (5.9) | 4 (5.1) |
| Once in 3 months | 4 (4.9) | 2 (2.6) | |
| Rarely if ever | 15 (18.5) | 3 (17.6) | 14 (17.9) |
| Never | 44 (54.3) | 12 (70.6) | 54 (69.2) |
| Do You Find Webinars Useful? | Usefulness of Telemedicine in Post-COVID Practice | ||
|---|---|---|---|
| Yes | 85 (48.3) | Not useful | 58 (33) |
| Maybe | 54 (30.7) | Undecided | 54 (30.7) |
| No | 19 (10.8) | Useful | 64 (36.4) |
| Can't exactly say | 18 (10.2) | Not useful | 58 (33) |
Table 3.
Changes in Neurosurgical Operating Room Practice During COVID Epidemic (N = 176)
| OR Practice | Public/Teaching Hospital (n = 81) | Multiple Affiliations (n = 17) | Private (n = 78) |
|---|---|---|---|
| OR practice changes across practice models | |||
| Elective with COVID/CT screening | 3 (3.7) | 3 (3.8) | |
| Emergency only | 33 (40.7) | 11 (64.7) | 23 (29.5) |
| Emergency with COVID/CT screening | 18 (22.2) | 14 (17.9) | |
| Unchanged | 1 (1.2) | 2 (11.8) | 4 (5.1) |
| Emergency + occasional electives | 24 (29.6) | 4 (23.5) | 30 (38.5) |
| Stopped completely | 2 (2.5) | 4 (5.1) | |
| PPE Desirability and Use Across Practice Models | ||||||
|---|---|---|---|---|---|---|
| PPE Strategies | Felt Requirement | Practiced | Felt Requirement | Practiced | Felt Requirement | Practiced |
| Donning/doffing area | 27 (33.3) | 16 (19.8) | 7 (41.2) | 5 (29.4) | 27 (34.6) | 18 (23.1) |
| Face shield/googles | 44 (54.3) | 39 (48.1) | 10 (58.8) | 8 (47.1) | 46 (59) | 47 (60.3) |
| Full PPE | 53 (65.4) | 34 (42) | 11 (64.7) | 11 (64.7) | 52 (66.7) | 42 (53.8) |
| N95 masks | 38 (46.9) | 39 (48.1) | 11 (64.7) | 9 (52.9) | 46 (59) | 47 (60.3) |
| Varied | 1 (1.2) | 4 (4.9) | 1 (5.9) | 2 (11.8) | 0 (0) | 2 (2.6) |
OR, operating room; CT, computed tomography; PPE, personal protective equipment.
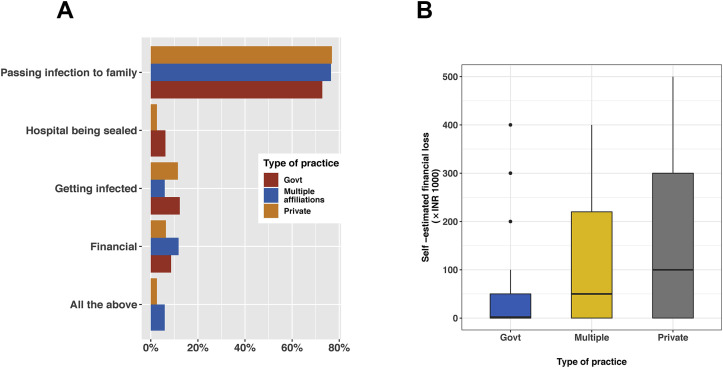
One of the biggest concerns among practitioners during this time was passing the infection to family members, with >70% of all respondents wanting to prevent this occurrence (Figure 5 ). This concern was greater than the fear of becoming infected and financial losses (Table 4). Regarding their outlook toward the resumption of clinical practice, many believed that this situation would be restricted for the foreseeable future (43.8%), whereas many were uncertain (26.1%). In the absence of government regulations, most wanted to continue semielective and elective cases with testing for COVID (46.6%) or perform only restricted practice such as emergency cases only (29%) (Table 4).
Figure 5.
(A) The greatest fear of respondents. (B) Amount of financial loss in Indian rupees (INR) compared across practice patterns. Govt, government.
Social Media Role and Mental Health
About a quarter of the respondents had been mentally depressed during the past 6 weeks of the lockdown period after the declaration of the COVID pandemic measures.
Social media were rife with fake news claiming false treatments and >80% of respondents seem to have encountered such news daily (Table 4). However, PPEs and prophylactic medications such as hydroxychloroquine were also discussed frequently by neurosurgeons on social media as the pandemic struck the subcontinent. Most respondents (>60%) found social media to be useful in deciding workflow and planning during the pandemic (Table 5 ). Most respondents denied facing any threats from the community during the COVID pandemic, in contrast to the social media stories. However, 30% of the respondents admitted that they felt discriminated against or encountered hostility on social media during the pandemic, with 61% reporting never having experienced these feelings and 9% choosing not to respond to the question. Most respondents (78.2%) believed that an “infodemic” of articles and surveys on COVID-19 had accompanied the pandemic, perhaps more than can be humanly absorbed.
Table 5.
Queries Regarding Social Media Use and Awareness of Neurologic Manifestations of COVID-19
| Encountered False Information on Social Media, n (%) | Discussed COVID Prophylaxis on Social Media, n (%) | ||
|---|---|---|---|
| Daily | 142 (81.1) | Daily | 68 (38.8) |
| Rarely | 18 (10.3) | Rarely if ever | 47 (26.9) |
| Once a month | 11 (6.3) | Never | 30 (17.1) |
| Never | 3 (1.7) | Once a month | 21 (12) |
| Once a week | 1 (0.6) | Occasionally | 9 (5.1) |
| Awareness of Neurologic Manifestations, n (%) | Usefulness of Social Media in Deciding Workflow, n (%) | ||
|---|---|---|---|
| Yes | 113 (64.2) | Somewhat useful | 78 (44.6) |
| No | 38 (21.6) | Very useful | 32 (18.3) |
| Maybe | 25 (14.2) | Rarely useful | 49 (28) |
| Not useful | 16 (9.1) | ||
Telemedicine, Webinars, and Journals
About two thirds of the respondents expected a greater role in telemedicine in the post-COVID era. Most respondents were aware of the neurologic manifestations of COVID-19 (64.2%) and recounted names of reputed journals (New England Journal of Medicine, Lancet, Journal of the American Medical Association, and Nature) as their popular sources of scientific information on the pandemic. Almost 47.2% of respondents remarked that webinars were a good source of learning during this phase of social distancing (Table 5).
Economic Loss
Most of the neurosurgeons reported economic losses during this period, with only 17.3% reporting no loss. The salaried surgeons face a deduction in salary ranging from 20% to 30% and private practitioners face setbacks because they need to meet the running cost of their infrastructure. The estimated losses ranged from U.S. $700 to $4000 (50,000 to 300,000 rupees per month). The average monthly salary of a neurosurgeon in India has been estimated to be U.S. $4000 (range, $2600–$10,000).6 This figure should be interpreted carefully because the losses not only meant salaries but erosion of savings and investment valuations.
Discussion
COVID-19 has infected almost 9,825,000 people worldwide as of this writing and has spread to >200 countries across the globe.13 , 14 India has >508,000 cases and is just behind the United States, Brazil, and Russia in terms of caseload. The surge of cases in India has been delayed perhaps because of the strict lockdown implemented by the government in the initial period, which was inevitably lifted because of socioeconomic compulsions. This strategy was important to collect and streamline the resources and increase public awareness necessary to counter the epidemic. The relaxation of the lockdown and increased COVID testing have led to an expected recent increase in the number of cases in India.
The experience from most countries, including India, Brazil, and Russia, shows that the pandemic has been disproportionately severe in densely populated metropolitan centers. High population density is one of the most important factors responsible for the uncontrolled spread of the virus, with a maximum number of cases seen in metropolitan cities with populations >20 million (e.g., Mumbai and New Delhi). Similarly, St. Petersburg in Russia and Rio De Janeiro and Sao Paulo in Brazil have borne the brunt of disease. This situation is probably attributable to prolonged and close contact between the infected and susceptible populations, occasioned by the crowded nature of these urban centers. Thus, a short-term dispersion of the population outside crowded urban centers may be a useful middle path strategy vis à vis an absolute lockdown.
Comparison of India with Russia and Brazil
Although most of the developed nations in Europe and scores of U.S. states have seen enough progress in their strategy against the virus to focus on how best to reopen their economies, the developing nations of Brazil, India, and Russia have seen a surge in cases and are placed second to fourth in the list of number of cases overall. However, the response in all these nations has been different. Whereas India initiated an early lockdown and had a spike of cases later, Brazil had a partial lockdown and later lifted it. Russia, on the other hand, had a partial economic shutdown imposed in late March, which helped slow the outbreak and prevent the nation's health care system from being overwhelmed. A nationwide lockdown was later needed and provincial governors were encouraged to consider reopening industries and construction sites. One of the common factors in all these nations is the incapability to sustain long periods of lockdown because of economic factors, which has led to a late increase in cases. Developed nations, on the other hand, have had resources to sustain a lockdown and thus have been able to contain the spread and reopen early (United States, Italy, and Spain).
Impact on Medical Practice
Given the serious public health risk, medical practice has changed remarkably during this pandemic. Although the virus primarily affects the respiratory system, the neurologic manifestations of COVID are well recognized.18 Although neurosurgery is not at the forefront of the medical response to this pandemic, neurosurgical practice and training are not insulated from this epidemic. Many organizations have advocated against operating on elective cases during this time,7 , 8 as increasingly more resources are being claimed by the response to the pandemic. We sought to highlight a seldom explored disparity between the response of private establishments and public hospitals offering neurosurgical services as they manage this pandemic. We also intended to examine the effect of social media, the economic losses incurred, and the most effective sources of information for a neurosurgeon in the Indian subcontinent during this pandemic.
All neurosurgical societies worldwide, including Indian societies, have responded to the pandemic by making changes in existing protocols and reorganizing neurosurgical activities.7 , 9 , 10 The focus has been shifted to triaging patients on the basis of disease into those needing emergent or elective care, although in neurosurgery, not many diseases are amenable to elective management. A scoring system for triaging patients for spine surgery in the setting of limited resources has also been developed.11 Our survey similarly reflected the global trend toward postponing nonemergent surgeries.
Precautions
There was a noticeable difference between the outpatient practices in private and government institutions. Neurosurgeons in larger practice groups (>10 neurosurgeons) experienced a stricter closure of normal outpatient services. This situation may be because most of these large practice groups belonged to public institutions and were obligated to close OPDs following government directives. Many government hospitals were declared COVID centers by the government and even the specialists were kept ready to take care of patients admitted with a diagnosis of COVID. This policy resulted from the strategy of preserving the workforce for the worst.
The operative strategy in government hospitals was adapted to the directions issued by the Neurological Society of India and other organizations.7 , 12 Private practitioners too scaled down their operation to occasional electives, with few continuing unchanged. These policy decisions are not insulated from the financial implications being faced by the respondents. Private practitioners needed to continue practice to remain financially viable and government institutions needed to balance the risk of operating emergencies with the high risk of iatrogenic transmission, given the larger caseload and active COVID-19 cases being treated at most of the public hospitals.
Neurosurgeons were most anxious about passing the infection to their families. However, this anxiety does not mean that the neurosurgeons were not worried about their safety. Even in the immediate future, most envisage performing only emergence procedures and semielective procedures with COVID testing, implying their commitment toward preventing transmission of the virus and keeping themselves safe (Table 4). These concerns were also reflected when we enquired about practice outside the regulation umbrella.
Telemedicine
Eight hundred million Indians have limited access to secondary and tertiary care, having to travel mostly to metropolitan centers for superspecialty care.13 Telemedicine provides a potential solution to mitigate this deficiency, more so, during the mobility restrictions caused by the COVID pandemic. Telemedicine has been the predominant mode of patient follow-up and has significantly replaced outdoor visits to neurosurgery departments in most of the developed world.14 One major center from the United States reported that 60% of visits to neurosurgery departments were deferred to a later date and >80% of the remaining visits were successfully converted to virtual.8 Another center reported a 40-fold increase in the use of telemedicine after the shelter-in-place measures were initiated, with a significant increase in the mean number of patients evaluated via telemedicine per week across all divisions of neurosurgery (4.5 to 180.4 patients/week).15 That center reported that both established patient visits and new patient visits increased significantly.
However, telemedicine services were offered by only 16.7% of neurosurgeons in our survey, which is low. There are many reasons responsible for this low figure. First, not many Indian patients have access to the Internet at home except for smartphones and are uncomfortable with various platforms such as Zoom and Webex for telemedicine. Second, telemedicine facilities were practically nonexistent in India before the COVID pandemic began and it is difficult to ensure rapid adoption of a relatively new service for both patients and doctors. Third, most patients do not have any medical insurance and few of those who have it are covered under various schemes run by the government. In both scenarios, there is no remuneration for the physician, which leads to low initiative on the part of the neurosurgeons to offer tele-OPD services. The increased risk of malpractice suits with tele-OPD and undefined regulations further discourage remote consultations.
PPE Use
Use of PPE has been recommended during interaction and transfer of patients presenting with neurosurgical emergencies as well as during neurosurgical surgeries and procedures for patients with confirmed and suspected COVID-19. Most respondents across different setups felt the need to use PPE during patient encounters in OPD as well as during surgery in the operating theater. However, there was a difference in the felt need and practice regarding the use of PPE among the respondents of our survey (Tables 2 and 3).
There might be several reasons for this observation. The supply of PPE was initially erratic because of disruption of global supply chains. The ordinary PPE suits often become uncomfortable for the surgeon during involved and prolonged neurosurgical procedures, discouraging its use.
Private practitioners were more punctilious in terms of PPE use. These observations may be attributed to diversion of PPEs in large public hospitals to other departments that were facing higher caseloads of patients with COVID or suspected COVID.
Mental Health
Mental health has been an often-neglected issue among neurosurgeons. Physicians and medical students had higher rates of burnout and depression than did the general population.16 Before the COVID pandemic, physicians were able to mitigate their stress levels with social and familial interactions. The stress extends outside the realm of health care facilities. Physicians worrying about infecting their families and contaminating their homes may choose to self-isolate or face the guilt of potentially infecting a family member. This worry was reflected in our survey too, with the primary concern being not spreading the infection to families and around 27% neurosurgeons feeling depressed during this time. A recent survey involving 375 respondents from 52 countries found that 34% of the respondents felt tense, 32.5% were unhappy, 25% experienced insomnia, almost 20% had headaches, and 5% had suicidal ideation during the pandemic.17 Of the respondents, 14% were found to have scores consistent with depression on Self-Reporting Questionnaire-20. Various factors identified by this study to be associated with higher risk of depression included those who did not receive guidance about self-protection, those who did not feel safe with provided PPE, and those whose families considered their workplace unsafe.
Violence Against Doctors
A recent report from China18 has highlighted a welcome response that there was no ripple effect or violence against doctors when they started resuming their routine neurosurgical outpatient clinics after lockdown of 3 months. In contrast, ≥30% of the respondents in our survey admitted to receiving unwelcome and intimidatory messages via social media during this pandemic, although it is difficult to ascribe all this to the COVID pandemic. Most of these threats specific to the COVID pandemic resulted from misplaced apprehension of the general public that health care workers could carry the infection into the neighborhood. The other reasons for hostility could be the delay in the treatment of patients who require neurosurgical attention because of the difficulties posed by suspension of regular services,
Limitations of Our Survey
Any survey has many limitations, with the foremost being selection bias. This was not an epidemiologic study and does not allow conclusions to be made about the prevalence and incidence of the variables investigated. However, it does allow us to draw conclusions about the perception of neurosurgeons of the COVID-19 health emergency concerning epidemiologic data. Another shortcoming is that perceptions are likely to change over time as the pandemic evolves and no survey can possibly surmount this limitation. However, we do not expect major changes in surgeons' perception and practices because the risk of catching the disease remains high until the pandemic is over. In an area with >3500 neurosurgeons, we were able to generate only 176 respondents. Despite this response, this is the first survey to analyze seldom-asked questions on mental health, social media impact, and differences among private and public centers, which may have been lost in this pandemic.
Conclusions
The neurosurgical community in developing countries cannot insulate itself from the implications of the COVID pandemic and must adapt rapidly to the changed scenario in health care delivery. Suspension of elective procedures, severe curtailment of regular outpatient appointments, drastic modifications of the normal OPD/operating room practices and apprehensions related to inadequacy of safety provided by PPE use and financial losses of private establishments were some of the visible themes in our survey results. Although telemedicine has not been as widely adopted as expected, online education has been favorably received.
CRediT authorship contribution statement
Harsh Deora: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing - original draft, Writing - review & editing. Shashwat Mishra: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing - original draft, Writing - review & editing. Manjul Tripathi: Writing - original draft, Writing - review & editing. Kanwaljeet Garg: Writing - original draft, Writing - review & editing. Vivek Tandon: Project administration. Sachin Borkar: Project administration. Nagesh Varshney: Project administration. Rupesh Raut: Project administration. Bipin Chaurasia: Resources, Software, Supervision, Validation. P. Sarat Chandra: Validation. Shashank Sharad Kale: Resources, Software, Supervision, Validation.
Footnotes
Conflict of interest statement: The authors declare that the article content was composed in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Harsh Deora and Shashwat Mishra contributed equally to this study and share equal first authorship,
References
- 1.Cenzato M., DiMeco F., Fontanella M., Locatelli D., Servadei F. Editorial. Neurosurgery in the storm of COVID-19: suggestions from the Lombardy region, Italy (ex malobonum) [e-pub ahead of print] https://doi.org/10.3171/2020.3.JNS20960 J Neurosurg. accessed July 31, 2020. [DOI] [PMC free article] [PubMed]
- 2.Tartara F., Cofano F., Zenga F., Boeris D., Garbossa D., Cenzato M. Are we forgetting non-COVID-19-related diseases during lockdown? Acta Neurochir (Wien) 2020;162:1501. doi: 10.1007/s00701-020-04385-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kissler S.M., Tedijanto C., Goldstein E., Grad Y.H., Lipsitch M. Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science. 2020;368:860–868. doi: 10.1126/science.abb5793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fontanella M.M., De Maria L., Zanin L. Neurosurgical practice during the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic: a worldwide survey. World Neurosurg. 2020;139:e818–e826. doi: 10.1016/j.wneu.2020.04.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sahu D., Agrawal T., Rathod V., Bagaria V. Impact of COVID 19 lockdown on orthopaedic surgeons in India: a survey. J Clin Orthop Trauma. 2020;11:S283–S290. doi: 10.1016/j.jcot.2020.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Neurosurgeon Salary in India/PayScale. https://www.payscale.com/research/IN/Job=Neurosurgeon/Salary Available at:
- 7.Gupta P., Muthukumar N., Rajshekhar V. Neurosurgery and neurology practices during the novel COVID-19 pandemic: a consensus statement from India. Neurol India. 2020;68:246–254. doi: 10.4103/0028-3886.283130. [DOI] [PubMed] [Google Scholar]
- 8.Arnaout O., Patel A., Carter B., Chiocca E.A. Letter: Adaptation under fire: two Harvard neurosurgical services during the COVID-19 pandemic. Neurosurgery. 2020;87:E173–E177. doi: 10.1093/neuros/nyaa146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ansari A., Kato Y., Tang J. Letter to the editor: neurosurgical practice in COVID-19 pandemic: from the view of academic departments in India, Japan and China. Br J Neurosurg. 2020;34:355–356. doi: 10.1080/02688697.2020.1759784. [DOI] [PubMed] [Google Scholar]
- 10.Bray D.P., Stricsek G.P., Malcolm J. Letter: maintaining neurosurgical resident education and safety during the COVID-19 pandemic. https://doi.org/10.1093/neuros/nyaa164 Neurosurgery. [DOI] [PMC free article] [PubMed]
- 11.Sciubba D.M., Ehresman J., Pennington Z. Scoring system to triage patients for spine surgery in the setting of limited resources: application to the coronavirus disease 2019 (COVID-19) pandemic and beyond [e-pub ahead of print] https://doi.org/10.1016/j.wneu.2020.05.233 World Neurosurg. accessed July 31, 2020. [DOI] [PMC free article] [PubMed]
- 12.Centers for Disease Control and Prevention Information for Laboratories about Coronavirus (COVID-19) https://www.cdc.gov/coronavirus/2019-ncov/lab/guidelines-clinical-specimens.html Available at:
- 13.Ganapathy K. Telemedicine in the Indian context: an overview. Stud Health Technol Inform. 2004;104:178–181. [PubMed] [Google Scholar]
- 14.Rahman M.M., Azam M.G., Bohorquez-Rivero J., Garcia-Ballestas E., Agrawal A., Moscote-Salazar L.R. Telehealth and telemedicine in the COVID-19 era: a world of opportunities for the neurosurgeons [e-pub ahead of print] https://doi.org/10.1016/j.wneu.2020.06.064 World Neurosurg. accessed July 31, 2020. [DOI] [PMC free article] [PubMed]
- 15.Mouchtouris N., Lavergne P., Montenegro T.S. Telemedicine in neurosurgery: lessons learned and transformation of care during the COVID-19 pandemic [e-pub ahead of print] https://doi.org/10.1016/j.wneu.2020.05.251 World Neurosurg. accessed July 31, 2020. [DOI] [PMC free article] [PubMed]
- 16.Dyrbye L.N., West C.P., Satele D. Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population. Acad Med. 2014;89:443–451. doi: 10.1097/ACM.0000000000000134. [DOI] [PubMed] [Google Scholar]
- 17.Sharif S., Amin F., Hafiz M. COVID 19-depression and neurosurgeons [e-pub ahead of print] https://doi.org/10.1016/j.wneu.2020.06.007 World Neurosurg. accessed July 31, 2020. [DOI] [PMC free article] [PubMed]
- 18.Xu X.-W., Wu X.-X., Jiang X.-G. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: retrospective case series. BMJ. 2020;368:m606. doi: 10.1136/bmj.m606. [DOI] [PMC free article] [PubMed] [Google Scholar]