To the Editor
With great interest, we have read the publication of Vitullo et al., regarding the use of simulation-CT’s as an opportunistic coronavirus disease 2019 screening tool during the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic [1]. Within the Iridium Network, a radiation therapy (RT) department consisting of 10 linear accelerators, a very similar approach (Fig. 1 ) was adopted. In this short communication, we want to describe our methodology and report the outcome in a population of 724 patients. Sharing approaches and outcome of measurements taken in RT departments during the COVID outbreak, might help us to tackle the challenges of future outbreaks in a more uniform way.
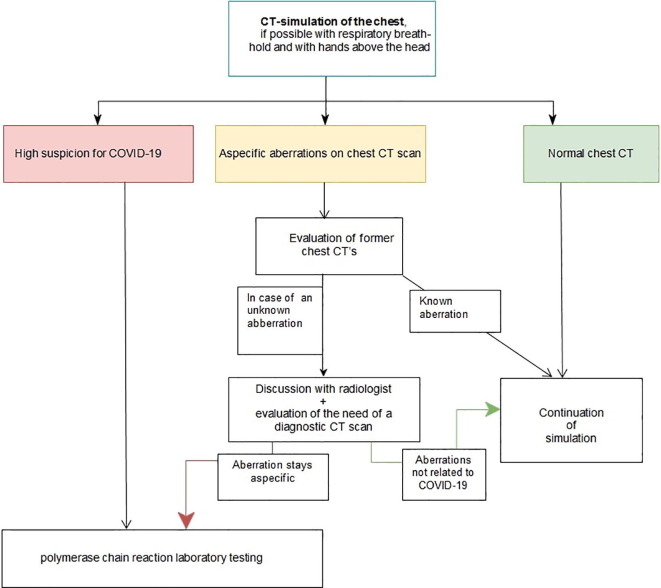
Fig. 1.
CT simulation workflow.
At the entrance of our RT department, all patients were screened for an elevated body temperature and symptoms related to COVID-19. At simulation, following oral informed consent, a chest CT scan was taken, preferably with the hands above the head and with a respiratory breath hold technique. Each chest CT was then analysed by at least one radiation oncologist. In case of high suspicion for COVID-19, the patient was immediately referred for laboratory testing. In case of aspecific aberrations on chest CT scan, previous imaging was analysed to see if this was a preexisting condition or not. In the case of newly found aberrations, the findings were discussed with a dedicated radiologist (Fig. 1) to assess the probability of COVID-19.
This approach was initiated at 29th of March 2020 for a two-month period till 29th of May 2020. In total, 724 patients were referred for simulation in that period. Temperature measurement upon arrival for simulation at our department resulted in 3/724 patients with an above-normal temperature. One of these patients had several non-COVID related infections. Two patients were known with tumor fever for several days or weeks; one of them developed a COVID infection at a later time-point during radiation treatment.
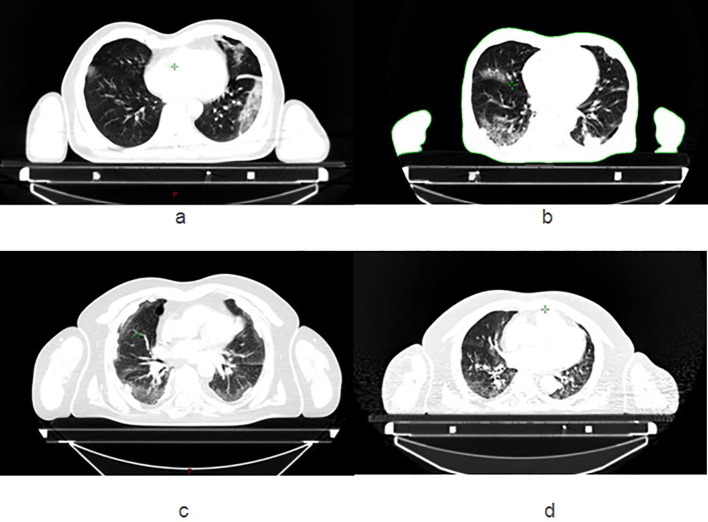
In total, 724 patients underwent simulation, including thoracic imaging, with a treatment-planning CT using 1–3 mm slice thickness depending on the primary tumor site. In 4/724 scans, new abnormalities were found on chest CT. Two cases with lung patterns highly suspicious for COVID were observed (Fig. 2 a and b), interestingly, these asymptomatic patients tested both positive for SARS-CoV-2 on polymerase chain reaction (PCR) laboratory testing. The other two CT scans showed new lung abnormalities that were however less typical for COVID-19 (Fig. 2c and d). These cases were discussed with a radiologist, who could not rule out COVID-19 infection in both cases. Therefore, these patients were referred for PCR-testing and tested both negative for SARS-CoV-2. Both PCR-confirmed positive patients were seen in the first half of April. None of the four patients who were send for PCR-testing had respiratory symptoms or fever.
Fig. 2.
Chest CT scans of the four patients that were referred for polymerase chain reaction laboratory testing.
Similar to Vitullo et al., our RT department developed a COVID-19 screening protocol for oncologic patients consisting of both temperature checks and chest CT at simulation [1]. This approach is based on the results of Ai et al., showing a sensitivity of 97%, to find COVID-19 with a chest CT scan in their cohort of 1014 patients [2]. In the (n = 101) patient cohort of Vitullo et al., no diagnosis of COVID-19 was found using a chest CT at simulation [1]. In our larger dataset, 2 out of 4 asymptomatic patients with suspicious CT scan tested positive for SARS-CoV-2. Therefore we believe that thoracic CT screening allows early diagnosis of COVID-19, when patients are still in the asymptomatic phase. Identifying these patients is important, especially since it is known that patients with cancer have an excess mortality risk from COVID-19 [3]. Secondly, the presence of asymptomatic COVID-19 patients at the RT department may cause cross infection towards other frail oncologic patients as well as staff [4].
However, as CT abnormalities were seen in only four cases out of 724 (0.5%), resulting in two PCR-confirmed diagnoses, every department has to outweigh the advantages of this screening against the extra workload and radiation dose.
To put things in perspective, in our patient cohort, only 3/724 patients with fever were retained during the same period using systematic body temperature measurement, while the temperature check is performed worldwide as a screening tool [4]. Furthermore, it seems feasible to only perform this approach with chest CT around the peak of an outbreak, since in our patient population, we did not find any new cases in the last five weeks of performing this approach, when infection numbers in Belgium were dropping.
Interestingly, the cumulative incidence for SARS-CoV-2 positivity in the general population in Belgium is 0.5% (58.615/11.000.000 on 2/6/2020) [5]. It seems that in our patient population of 724 cancer patients without severe immunosuppression, we observe similar SARS-CoV-2 positivity rates.
In conclusion, imaging techniques used in RT are a potential screening opportunity [6] and may be an added value to identify asymptomatic COVID-19 patients that are not identified by standard screening in hospitals (e.g. temperature screening and questions regarding COVID-19 related symptoms).
Footnotes
The Editors of the Journal, the Publisher and the European Society for Radiotherapy and Oncology (ESTRO) cannot take responsibility for the statements or opinions expressed by the authors of these articles. Practitioners and researchers must always rely on their own experience and knowledge in evaluating and using any information, methods, compounds or experiments described herein. Because of rapid advances in the medical sciences, in particular, independent verification of diagnoses and drug dosages should be made. For more information see the editorial “Radiotherapy & Oncology during the COVID-19 pandemic”, Vol. 146, 2020.
References
- 1.Vitullo A., De Santis M.C., Marchianò A., Valdagni R., Lozza L. The simulation-CT: radiotherapy’s useful tool in the race against COVID-19 pandemic. A serendipity approach. Radiother Oncol. 2020;147:151–152. doi: 10.1016/j.radonc.2020.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ai T., Yang Z., Hou H., et al. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 2020;26 doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gosain R., Abdou Y., Singh A., et al. COVID-19 and cancer: a comprehensive review. Curr Oncol Rep. 2020;5:53. doi: 10.1007/s11912-020-00934-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wei W., Jiang H., Chen W., Zhou Y., Guo S., Zhong G. How should we implement radiotherapy for cancer patients in China during the endemic period of COVID-19? Radiother Oncol. 2020;147:100–102. doi: 10.1016/j.radonc.2020.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.https://covid-19.sciensano.be/sites/default/files/Covid19/Meest%20recente%20update.pdf. Consulted on 2/6/2020.
- 6.Boldrini L., Dinapoli N., Valentini V. Radiotherapy imaging: an unexpected ally in fighting COVID 19 pandemic. Radiother Oncol. 2020;148:223–224. doi: 10.1016/j.radonc.2020.04.036. [DOI] [PMC free article] [PubMed] [Google Scholar]