Abstract
During novel coronavirus 2019 (COVID-19) pandemic, patients usually present with several reports showing symptoms of severe systemic or respiratory illness and, although rare, some genital complaints such as scrotal discomfort can be seen. In the majority of patients, however, genital complaints seem not to be the initial or sole symptoms. In this article, we report an unusual presentation of a male case with severe external genital pain which was suspected to be the first clinical sign of COVID-19.
Keywords: COVID19, Male genitalia, Testis
Introduction
After the first report of SARS-CoV-2 (severe acute respiratory syndrome coronavirus-2; COVID-19) infection in late December 2019, the scientific community diverted its attention to impact of this virulent virus on the whole organ systems.1 Involvement of male genitourinary system as a potential target was also reported in the literature.2
There is a very limited number of data regarding effect of COVID-19 on fertility. Nonetheless, patients with COVID-19 are recommended to be followed in the long-term to reveal any deleterious effects of this infection on male reproductive system, which is also an interesting topic to be debated for many researchers. In this article, we report an unusual presentation of a male case with severe external genital pain which was suspected to be the first clinical sign of COVID-19.
Case presentation
A 49-year-old, single male patient was admitted to our urology outpatient clinic with swelling sensation and pain in his left groin and testicle. His symptoms started early on the day of hospital admission. He had intermittent pain initially; however, its severity increased over time within three to 4 h before his admission to hospital, radiating to his left inguinal area and reaching up to the left flank region. The patient had no lower urinary tract symptoms. His medical history revealed hyperlipidemia and insulin resistance without any previous surgery. Physical examination showed normal vital signs at the time of presentation. Genital examination revealed left spermatic cord tenderness and pain on palpation without any abnormality overlying scrotal skin. After a suspicious contact history in emergency department two days ago, he was screened for COVID-19 and a pharyngeal swab sample was taken for quantitative reverse transcriptase polymerase chain reaction (qRT-PCR) analysis. The patient was sent home and self-isolation was instructed until test results were obtained. The result was reported positive on the day of admission to our urology outpatient clinic.
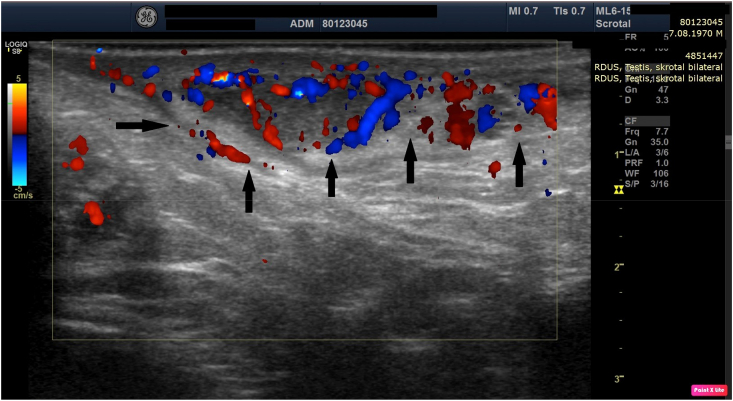
Laboratory analysis showed mild leukopenia (3970/mm3) and anemia (hemoglobin 12.8 g/dL) with normal D-dimer and increased ferritin levels. Thoracic computed tomography revealed no findings of COVID-19. Abdominal ultrasound revealed small simple cysts in both kidneys. Scrotal ultrasound showed slightly increased vascularity, suggesting spermatic cord inflammation with no testicular finding compatible with orchitis (Fig. 1). Urinalysis result was negative with non-specific urine cultures. The cultures were collected for sexually transmitted diseases including RT-PCR analysis for Chlamydia trachomatis, Ureaplasma urealyticum, and parvum, Neisseria gonorrhoeae, Herpes genitalis (type 1 and type 2), Mycoplasma genitalium, Trichomonas vaginalis, and Gardnerella vaginalis and all were negative. In addition, the Venereal Disease Research Laboratory (VDRL), Brucella agglutination tests, and Mumps antibodies were negative. Semen analysis using RT-PCR also produced negative results. Due to his high concern on fertility, semen analysis was performed, and sperm count analysis revealed no abnormality according to 2010 World Health Organization criteria for semen analysis.
Fig. 1.
Ultrasound image showing increased vascularity (black arrows) suggesting inflammation along the spermatic cord.
The patient was hospitalized for COVID-19 treatment and was given a standard 5-day regimen of hydroxychloroquine 200 mg twice a day, azithromycin 250 mg once daily, and imipenem cilastatin 500 mg four times a day for seven days. The hospital course went uneventful with full recovery from his genital complaints after the second day of treatment. The two subsequent RT-PCR tests were positive on Days 8 and 13 after the first positive PCR. The results were found to be negative in the fourth test on Day 18. However, on Days 19 and 20, the test results were positive again. We finally obtained two consecutive negative RT-PCR results on Days 22 and 24, indicating that the viral shedding took longer than three weeks.
A written informed consent was obtained from the patient for all the diagnostic and therapeutic procedures performed.
Discussion
Based on current body of scientific knowledge with diverse case studies on COVID-19, it becomes clear that the virus can express itself differently on a case by case basis. In its nature, the COVID-19 is a viral infection which predominantly attacks respiratory organs. However, as in our case, patients can exhibit various symptoms in organs other than the lungs, such as in genitals. The presence of ACE2 in testes, Leydig, and Sertoli cells, receptor for entry into target cells by SARS-CoV-2,3 suggests a high suspicion of involvement of male gonads, although there is no clinical evidence available to date. One recent study reported that COVID-19 could induce damage to male reproductive system hormones.4 In this study, the authors compared sex-related hormones between 81 reproductive-aged men with SARS-CoV-2 infection and 100 age-matched healthy men, and found that serum luteinizing hormone (LH) significantly increased, while testosterone-to-LH ratio and follicle-stimulating hormone-to-LH ratio significantly decreased in males with COVID-19. This finding provides a good evidence on the influence of medical condition of COVID-19 on male sex hormones, taking more attention to gonadal function of patients recovered from SARS-CoV-2 infection, particularly for reproductive-aged men. Although these findings are preliminary, urogenital system may be in a potential risk to be infected by SARS-CoV-2 infection.
Genital complaints such as scrotal discomfort were reported in 19% of patients around time of their COVID-19 confirmation in the Pan et al.‘s study.5 In our case, the patient had no other systemic or urinary symptoms in addition to testicular/spermatic cord pain and swelling sensation. Furthermore, viral clearance took longer than the mean clearance time of pneumonia. Any illness with fever may have deleterious effects on spermatogenesis temporarily, as it was shown in previous studies. On the other hand, we cannot be sure that COVID-19 would follow the same pattern. Therefore, the case study reflects that COVID-19 would be a potential target to male genitalia directly without affecting any other organ systems and systemic symptoms and should be closely followed. Although listed symptoms and concerns do not fit the mold of COVID-19 symptoms, our case suggests that it is possible for patients with genital pain and discomfort to be infected with the virus.
Conclusion
In conclusion, patients with isolated genital symptoms such as testicular/spermatic cord pain and discomfort without other systemic symptoms should be closely followed for COVID-19 and clinicians should be alert for this unusual presentation of the virus during pandemic.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
The authors declare that there is no conflict of interest regarding the publication of this article.
Acknowledgements
We wish to acknowledge the help provided by Şenay Cankut who is a chief of staff in our Andrology Lab in IVF department for her assistance handling of semen analysis and semen sample for PCR analysis and Prof.Canan Külah, MD from Microbiology Department for her PCR work in semen and Ms. Merve Revna Ozdamar from Columbia University, Department of Social Work for proof-editing of the paper.
References
- 1.Chen N., Zhou M., Dong X. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zou X., Chen K., Zou J., Han P., Hao J., Han Z. Single-cell RNA-seq data analysis on the receptor ACE2 expression reveals the potential risk of different human organs vulnerable to 2019-nCoV infection. Front Med. 2020 Apr;14(2):185–192. doi: 10.1007/s11684-020-0754-0. Epub 2020 Mar 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang Z., Xu X. Spermatogonia, Leydig and Sertoli Cells. medRxviv; 2020. scRNA-seq profiling of human testes reveals the presence of ACE2receptor, a target for SARS-Cov-2, infection. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ma L., Xie W., Li D. Effect of SARS-CoV-2 infection upon male gonadal function: a single center-based study. medRxiv. 2020 doi: 10.1101/2020.03.21.20037267. [DOI] [Google Scholar]
- 5.Pan F., Xiao X., Guo J. No evidence of SARS-CoV-2 in semen of males recovering from COVID-19. Fertil Steril. 2020 doi: 10.1016/j.fertnstert.2020.04.024. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]