Highlights
-
•
In an emergency situation it is possible to put in place a remote MT support intervention.
-
•
Clinical Staff define this structured intervention as empathic, supportive and professional.
-
•
MTps were able to create a remote therapeutic relationship with Clinical staff (CS).
-
•
Self-administration of music by CS would not have been enough to achieve the objective of the present study.
-
•
Few studies have been conducted so far with a focus on MT support to CS assisting COVID patients.
Keywords: Music therapy, Covid-19, Support, Clinical staff, Stress
Abstract
The influence of music therapy (MT) as a support intervention to reduce stress and improve wellbeing in Clinical Staff (CS) working with COVID-19 patients was evaluated. Participants were enrolled as a result of spontaneous agreement (n = 34) and were given remote receptive MT intervention over a 5-week period. Their levels of tiredness, sadness, fear and worry were measured with MTC-Q1 before and after MT intervention. An immediate significant variation in the CS emotional status was observed. The results seem to confirm that in an emergency situation, it is possible to put in place a remote MT support intervention for CS exposed to highly stressful situations.
Introduction
The 2019 novel coronavirus disease (COVID-19), caused by the virus officially named SARS-CoV-2, appeared in Wuhan, Hubei Province, China at the end of 2019, not only caused great public concern, (Wang, Horby, & Hayden, 2020), but also brought about huge psychological distress, especially for Clinical Staff (CS) (Zhang et al., 2020). Due to the rapid increase in the number of cases from December 2019, the outbreak was classified by the World Health Organization (WHO) as a pandemic on March 11, 2020. In Europe, Spain, UK and Italy have recently reported the highest numbers of cases (https://covid19.who.int/) and deaths (as of 11 May 2020; WHO, 2020).
The North of Italy has been the most affected area of the country (Motta Zanin, Gentile, Parisi, & Spasiano, 2020). As a result, like in many other countries, the Italian National Health Service has been overwhelmed and has struggled to give an effective and timely response to the needs of the large number of infected patients. This situation had a significant impact on the physical and mental wellbeing of frontline healthcare workers, who were under increasing daily pressure for prolonged work shifts, scarcity of personal protective equipment, fear of being infected and of infecting their own family members (Lancet, 2020), and for the stress associated with the loss of many patients, colleagues and in some cases of their loved ones (Zaka, Shamloo, Fiorente, & Tafuri, 2020). Some studies have shown that, when in close contact with patients with emerging infectious disease, including SARS (Chung, Wong, Suen, & Chung, 2005), MERS-Cov (Kim, 2018), Ebola (Van Bortel, Basnayake, & Wurie, 2016) (Liu, Wang, & Zhou, 2019), H1N1 (Honey & Wang, 2013), Clinical Staff (CS) can suffer from loneliness, anxiety, fear, fatigue, sleep disorders, which are likely to result in a poorer quality of healthcare for patients (Su, Weng, & Tsang, 2009). What is more, long-term psychological consequences are also likely to be brought about, including higher levels of burnout, psychological distress and post-traumatic stress disorder. In addition, the newly recruited CS for the Covid Hospitals were usually without any adequate psychological training to cope with stressful work conditions (Zaka et al., 2020). Recent studies have focused on the severity of the psychological problems observed in CS (Kang, Li, & Hu, 2020), and on the urgency of providing them with psychological assistance (Xiang, Yang, & Li, 2020) and help to reduce their of levels tiredness sadness, fear and worry.
Music therapy (MT) has been shown to play an important role in helping address physical symptoms and psychological distress (Fallek et al., 2019). MT involves the systematic use of musical experiences aimed at achieving therapeutic goals by a trained music therapist (MTp). It also implies the establishment of a relationship between patient, music and MTp (Bradt, Dileo, & Shim, 2013), (Giordano et al., 2020). MT has been shown by some systematic reviews to reduce pain, improve sleep quality, decrease anxiety and tiredness and induce a relaxation response without the use of medication (Mofredj, Alaya, & Tassaioust, 2016) (Bradt, Dileo, & Magill, 2016) (Tan, Lester, & Lin, 2020). Among palliative care patients, MT has been observed to produce positive changes in pain, anxiety, physical comfort, emotional state, social interaction, and spiritual wellbeing (McConnell & Porter, 2017) (Schmid, Rosland, & von Hofacker, 2018). Through dopamine production (Ferreri et al., 2019), MT can induce pleasure, relaxing conditions, reduce cortisol levels and therefore stress levels (van der Steen, Smaling, & van der Wouden, 2018). As reported in the literature, MT is also used to reduce distress at work, to improve mood, performance, attention and concentration (Raglio, Imbriani, & Oddone, 2017). However, no studies have been conducted so far with a focus on MT support intervention administered to CS assisting COVID patients.
The aim of this preliminary study was to investigate the influence of MT as a support intervention to reduce stress and improve wellbeing in a sample of CS assisting patients with COVID-19.
Materials and methods
Participants
Over a 5-week period (from 1 April 2020 to 6 May 2020), emergency recruited CS to assist COVID-19 patients at the newly designated Coronavirus Unit of the University Hospital of Bari – Italy-, were invited to participate in this study.
Inclusion criteria were (a) age ≥ 18 years, (b) work at the Covid Unit, (c) willingness to cooperate. Exclusion criteria were (a) severe physical, neurological or psychiatric conditions in the previous twelve months, (b) refusal to participate in the study.
During these weeks the School of Medicine of the University of Bari made available single room hotel accommodation to each newly recruited CS, to prevent the risk of contagion in their families and also to help them find an appropriate accommodation. All CS staying at the hotel in question were informed about and asked to participate in this study by the Unit Coordinator on the basis of the above inclusion/exclusion criteria. Enrolment took place on the basis of participant agreement.
Receptive music therapy
An interactive relational approach of receptive MT (Bruscia, 1998a) (Grocke & Wigram, 2007), supplemented by Guided Imagery and Music (Bruscia & Grocke, 2002) was used. Some specific playlists (PLs) were created to favor relaxation and reduce anxiety and stress (Breathing PL), to recover energy and support concentration (Energy PL), to release tension and instill calm and peace of mind (Serenity PL).
In the relaxation PL (Breathing) music tracks were selected on the basis of the following elements: steady pulse; quiet mood; predictable melodic lines; little dynamic change; supportive bass line; stability in volume, timbre, rhythm, harmony and pitch; simple structure; clear form. The Breathing PL was structured by selections from classical music of the Western tradition and modern selections with similar features (Bonny, 2002, p. 301-324).
By contrast, in the “stimulating” PLs (Energy and Serenity) music tracks were more changeable in instrumentation and in dynamic flow, unpredictable in melodic lines, volume, timbre, rhythm, harmony, pitch, loose structure and unclear form. Bass line could range from supportive to non-supportive (Grocke & Wigram, 2007) (Wigram & Bonde, 2019).
The Energy PL and Serenity PL were arranged on the basis of selections from pop, rock and jazz music.
All playlists length was from 15−20 min.
A listening guideline was created for all the PLs ("Find a quiet and comfortable space", "close your eyes", "focus on an image or a colour", "breathe slowly" etc.). The MTps tailored music to each CS based on the results of their weekly feedback assessment (Robb & Burns, 2011).
Design and procedure
After Board Institutional review approval and after obtaining informed consent, 34 CS were included in this preliminary study.
In the first week CS received MT contents on their mobile phones from a MTp clinician:
-
1
2 Playlists (PLs) - Breathing and Energy – were prepared by three trained MTps;
-
2
a listening guide tailored to the playlist mood;
-
3
a short questionnaire (MTC-Q1) to fill before and after each listening.
At the end of week 1, two researcher MTps interviewed CS on the phone to assess their listening experience. On the basis of the feedback collected the two MTps prepared 2 customized playlists for each CS to listen to during the next week. All CS received their customized playlists, listening guide and MTC-Q1.
This procedure was repeated for four weeks. CS were let free to decide when and how to listen to their PL during the weeks.
At the end of the study, an MTC-Q2 questionnaire was administered to assess the MT intervention.
Measures
The MusicTeamCare-Q1 (MTC-Q1) was used to investigate the effects of receptive MT intervention to reduce stress and improve wellbeing of CS. The MTC-Q1 is a self-assessment questionnaire, in the form of a Likert Scale, whereby a subject evaluates in a scale from 0 to 10 (with 0 = not at all and 10 = very much so) how much he/she feels tired, sad, fear and worried.
MTC-Q1 was administered by a link via mobile phones. CS were invited to fill it at 2 time points: before listening to PL (T0) and within one hour after the end of listening (T1).
Once a week a researcher MTp interviewed the CS on the phone about their listening experience to assess the relevance of the playlist proposed to the potential needs of participants. At the end of the study an MTC-Q2 was used. The MTC-Q2 self-assessment questionnaire, was designed by 24 closed-ended questions, with the exception of a few specific cases, in order to investigate some aspects as perceived through the MT intervention. In this preliminary study the analysis of the questionnaire was limited to 3 questions only (n.11 how useful was the the Listening Guide prepared by MTp, n.14 How useful was weekly assessment?, n.16 What did you feel through weekly feedback by MtP?)
Data collection was made by a psychology researcher.
Statistical analysis
Statistical analysis was performed using IBM SPSS Statistics software, version 21. Firstly, descriptive statistics were computed (mean scores (M), frequencies, standard deviations (SD). Secondly, a paired-samples t-test was used to compare the MTC-Q1 scores at T0 and T1. For all statistical tests a p-value lower than 0.05 was considered statistically significant.
Results
This study involved 34 CS (14 doctors, 20 nurses). The sample included 22 women and 12 men. The age range of participants was 22–59 (Mage = 31,8, SD = 8,33). The participants were enrolled from the Covid Unit of the University Hospital of Bari. All the participants subscribed to a written informed consent form. 5 subjects dropped out after week 2.
1st week Playlist
Breathing
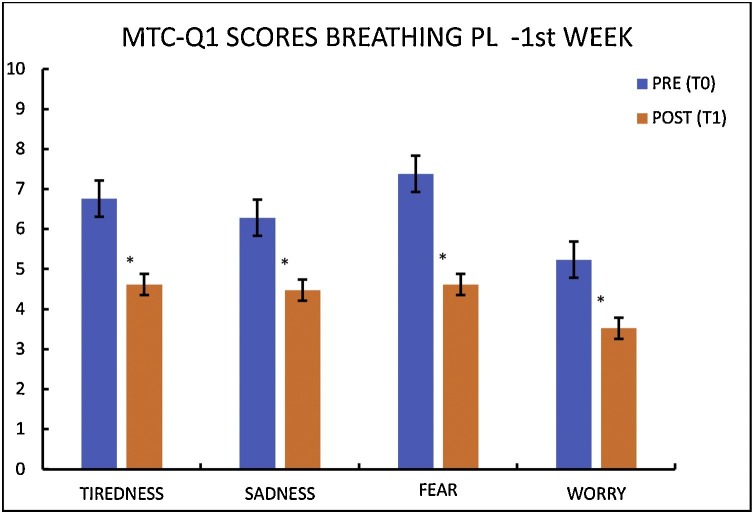
The variations in the emotional status of CS in the first week before and after listening to the breathing playlist are reported in Fig. 1 .
Fig. 1.
Descriptive analysis of MTC-Q1 scores for the 1 st week BREATHING PL.
Results of IBM SPSS as factor *p < 0,05.
The Breathing Playlist elicited a significant variation in the emotional status of CS. In more detail, in terms of the difference in tiredness perceived between T0 and T1, the test revealed a statistically significant result (t = 7,695, df = 20, p < 0,05). Moreover, there was a significant decrease in the intensity of perceived sadness (t = 6,432, df = 20, p < 0,05) and fear (t = 9,735, df = 20, p < 0,05) between T0 and T1. Finally, the results indicated a significant reduction in worry intensity between T0 and T1 (t = 5,056, df = 20, p < 0,05).
Energy
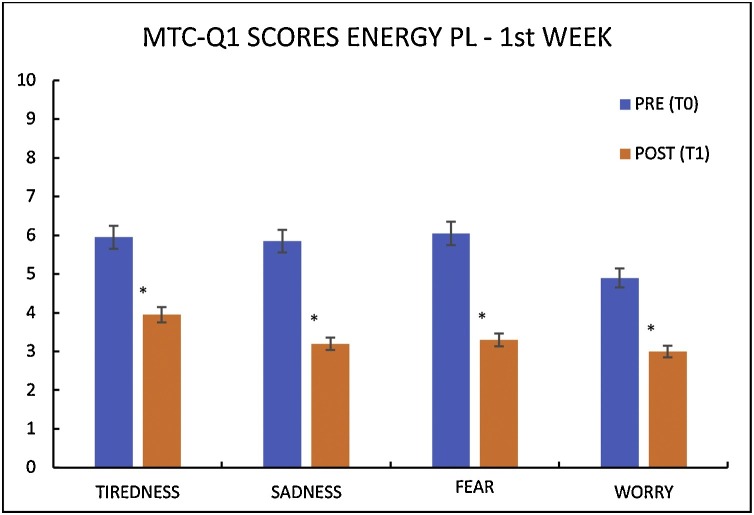
The variations in the CS emotional status in week 1 before and after listening to the Energy playlist are reported in Fig. 2 . In particular, paired-samples t-test results indicated a significant decrease in tiredness (t = 4,873, df = 20, p < 0,05), sadness (t = 8,545, df = 20, p < 0,05), fear (t = 6,419, df = 20, p < 0,05), and worry (t = 6,190, df = 20, p < 0,05) between T0 and T1.
Fig. 2.
Descriptive analysis of MTC-Q1 scores for the 1 st week ENERGY PL.
Results of IBM SPSS as factor *p < 0,05.
Customized playlists
Breathing
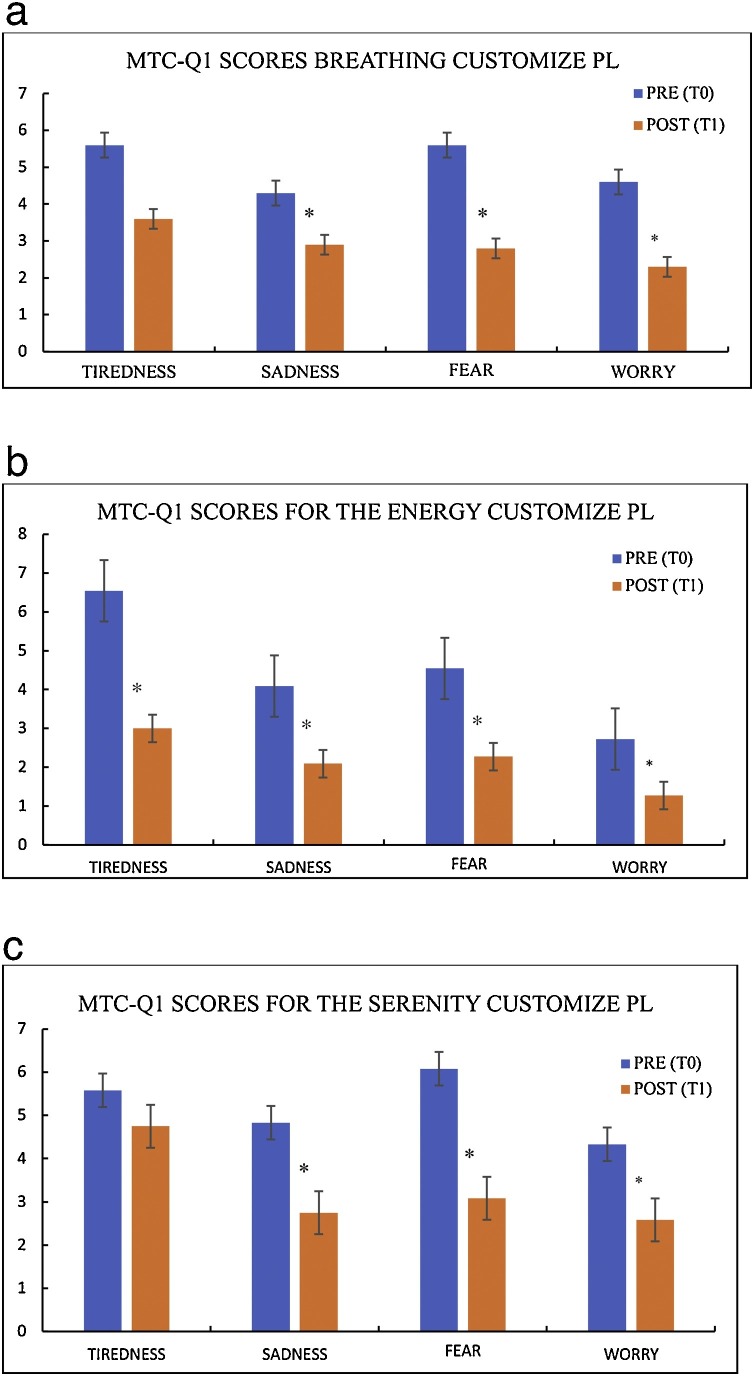
The variations in the emotional status of CS in the following week before and after listening to the customized personalized PL are reported in Fig. 3 a.
Fig. 3.
a) Descriptive analysis of MTC-Q1 scores for the Breathing Customize PL. b) Descriptive analysis of MTC-Q1 scores for the Energy Customize PL. c) Descriptive analysis of MTC-Q1 scores for the Serenity Customize PL.
Results of IBM SPSS as factor *p < 0,05 pre-post.
The customized Breathing Playlist generated a significant variation in the emotional status of CS. More specifically, the paired sample t-test indicated a significant decrease in the intensity of perceived sadness (t = 2,492, df = 9, p = 0,034), fear (t = 5,056, df = 9, p = 0,001), and worry (t = 3,535, df = 9, p = 0,006) after listening.
Energy
The variations in the emotional status of CS in following week before and after listening to the customized energy playlist are reported in Fig. 3b.
The customized Energy playlist generated a significant variation in the emotional status of healthcare workers, as indicated by the results of the paired-samples t-test. More specifically, there was a significant decrease in the intensity of perceived tiredness (t = 10,423, df = 10, p = 0,000), sadness (t = 4,282, df = 10, p = 0,002), fear (t = 3,858, df = 10, p = 0,003), and worry (t = 2,334, df = 10, p = 0,042) intensity after listening.
Serenity
The variations in the emotional status of CS before and after listening to the customized Serenity playlist are reported in Fig. 3c.
The customized Serenity playlist generated a significant variation in the emotional status of MP, as highlighted by the paired-samples t-test results. Specifically, there was a significant decrease in the intensity of sadness (t = 4,614, df = 11, p = 0,001), fright (t = 7,707, df = 11, p = 0,000), and worry (t = 2,956, df = 11, p = 0,013) after the listening of the playlist.
At the end of the study, CS were asked by MTC-Q2 how useful the Listening Guide prepared by MTp had been for them. Using a Likert Scale (with 0 = not at all and 10 = very much so) CS replied as follows:3,6% 6, 17,9%7, 28,6% 8, 14,3% 9, 32,1% 10, 3,6% 0. Moreover, CS were asked in the same way how useful the weekly assessment had been for them. Again, using a Likert Scale (with 0 = not at all and 10 = very much so) CS replied as reported in Table 1 .
Table 1.
Table describing how useful the weekly assessment had been for CS, using a Likert Scale (with 0 = not at all and 10 = very much so).
| MT | MUSIC THERAPY |
| CS | CLINICAL STAFF |
| MTp | MUSIC THERAPIST |
| MTC-Q1 | MUSIC TEAM CARE QUESTIONNAIRE 1 |
| PL | PLAY LIST |
Discussion
The aim of this study was to verify the effectiveness of receptive MT as a support intervention to reduce stress and improve wellbeing in CS assisting COVID-19 patients.
The findings indicate a significant decrease in the intensity of tiredness, sadness, fear and worry, as reported by CS after receptive MT intervention. Recent studies have shown that the most common stress-reducing strategies (Trifiletti, Di Bernardo, & Falvo, 2014) cannot be used in such extreme circumstances, as CS are more likely to be emotionally involved while feeling the duty and being asked to keep going. According to the literature, the important psycho-biological effects of music on stress conditions are ascribable to a reduced activity of the hypothalamus–pituitary–adrenal axis and hence to decreased cortisol production (Chanda & Levitin, 2013).
MT seems to favor the expression of emotions, strengthen self-awareness, social connection, and sense of personal support (Fallek et al., 2019), while having a positive effect on anxiety as a potential tool to mitigate stressful environmental factors (Geipel, Koenig, Resch, & Kaess, 2018) (Pfeifer, Fiedler, & Wittmann, 2019)
In the first week, PLs were prepared by three Mtps, using a methodology focused on the therapeutic features of music as described in 2.3, irrespective of the music participants were familiar with, and irrespective of their preferred music genre (Grocke & Wigram, 2007).
The data collected on first week PL (pre- and post-listening) highlighted significant decreases in tiredness, sadness, fear and worry.
PLs were also prepared considering to what extent music can involve the physical, emotional and mental spheres and the sphere of thought in a targeted manner without causing side effects, including overstimulation and loss of contact with reality.
All the above aspects have been assessed by means of the weekly assessment to measure, adapt and customize the PLs for the following weeks.
For a successful on-site receptive MT session the MTp is tasked with monitoring many factors, including making available to the client the most comfortable setting in terms of lights, spaces, as well as music reproduction and voice quality to favor a state of relaxation (Grocke & Wigram, 2007). Due to the Covid-19 restrictions the MTp was not able to monitor in person all the above factors. For this reason all the PLs were accompanied by a written Listening Guide with some indications on how to get prepared to listen (“take a quiet space, find a comfortable position, close your eyes, breathe slowly, focus your attention on…”, etc).
Through weekly assessments MTps were able to create a remote therapeutic relationship with CS; to identify their requests and take care of their needs, comments and specific experiences; to define and set up a music selection on the basis of some specific musical features; to take into consideration the level of energy, the state of physical health and mood, the preferred genre and style of music of participants and to customize the PLs to each one of them (Grocke & Wigram, 2007).
The data obtained have highlighted that customized PLs had a greater impact on specific markers, as they were able to respond to the specific needs emerged during the weekly assessments.
In addition, the data derived from MTC-Q2 (n.11 and n.14) seem to suggest that even though CS often use pre-recorded music through personal listening devices or through free field to enhance their concentration and focus, reduce their tension and /or promote their efficiency as they engage in every-day life, or in medical procedures -most typically surgery (George, 2011) (Allen & Blascovich, 1994), the presence of a MTp was perceived as being of greater help and support.
CS defined this structured intervention (weekly assessment, listening guidelines, personalization of PLs) as empathic, supportive and professional (n.16 MTC-Q2). However, this remote MT intervention has required more involvement on the part of the MTp due to the lack of a direct personal contact that could not be completely replaced just by getting feedbacks on the phone and because MTps were a part of a broader community involved in the pandemic.
On the basis of these considerations it seems to be sensible and reasonable that direct use of music (self-administration) by CS would not have been enough to achieve the objective of the present study.
Stress management studies in a non-clinical population have shown significant changes between MT intervention versus no treatment according to self-reported measures such as mood and anxiety (STAI and non-STAI), and physiological measures such as blood pressure, respiration rate, Immunoglobulin A and heart rate/pulse (Dileo & Bradt, 2007).
What is more, MT intervention is cost-effective and non-invasive (Chlan, Heiderscheit, Skaar, & Neidecker, 2018).
Implications
This study has highlighted to what extent it has been possible to use a minimally invasive and sustainable cost-effective resource to remotely support frontline Clinical Staff during the COVID-19 pandemic. Extreme speed and flexibility were required to cope with the challenges of an extreme and difficult working environment. Clearly enough, further studies and research efforts are required to understand how MT can be used as a resource for self-care and work-related stress prevention in different types of professionals involved in maxi-emergency or high-risk situations.
Further studies are needed to explore and enhance the methodologies and techniques underlying remote receptive MT interventions.
Limitations
The present study is a preliminary, pilot study and therefore it is not intended to produce conclusive evidence. Future research efforts will require a larger sample of participants and different study settings. It was not possible to use randomization procedures due to the nature of the treatment in question and to the situation of emergency.
However, further research is required to determine the full efficacy of this intervention in terms of providing support to CS and prevent burn-out in situations other than health emergencies.
Qualitative Data from MTC-Q2, including phone feedback topics, specific aspects of the music used for the playlists, personal experiences with music listening, etc. are currently being investigated and studied for future publication.
Conclusions
In conclusion, this study seems to confirm that in an emergency situation it is possible to put in place a remote MT support intervention targeted to CS exposed to highly stressful situations.
Thanks to the music and the presence of a certified MTp, MT can become an important form of support provided, even indirectly, by means of the non-invasive but constant presence of a professional music therapist who guides the CS in listening and taking care of themselves in unexpected and unpredictable extreme situations.
Declaration of Competing Interest
Nothing to declare.
References
- Allen K., Blascovich J. Effects of music on cardiovascular reactivity among surgeons. JAM. 1994;272(22):1724. [PubMed] [Google Scholar]
- Bonny H. In: Music & consciousness. Barcelona Publishers, editor. Barcelona Publisher; Ghilsum, NH: 2002. [Google Scholar]
- Bradt J., Dileo C., Shim M. Music interventions for preoperative anxiety. The Cochrane Database of Systematic Reviews. 2013;6 doi: 10.1002/14651858.CD006908.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradt J., Dileo C., Magill L. Music interventions for improving psychological and physical outcomes in cancer patients. The Cochrane Database of Systematic Reviews. 2016;8 doi: 10.1002/14651858.CD006911.pub3. [DOI] [PubMed] [Google Scholar]
- Bruscia K. 2nd ed. Barcelona Publisher; Gilsum, NH: 1998. Defining music therapy. [Google Scholar]
- Bruscia K., Grocke D. Barcelona Publisher; Gilsum, NH: 2002. Guided imagery and mUsic: The bonny method and beyond. [Google Scholar]
- Chanda M., Levitin D. The neurochemistry of music. Trends in Cognitive Sciences. 2013;17(4):179–193. doi: 10.1016/j.tics.2013.02.007. [DOI] [PubMed] [Google Scholar]
- Chlan L., Heiderscheit A., Skaar D., Neidecker M. Conomic evaluation of a patient-directed music intervention for ICU patients receiving mechanical ventilatory support. Critical Care Medicine. 2018;46(9):1430–1435. doi: 10.1097/CCM.0000000000003199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung B., Wong T., Suen E., Chung J. SARS: Caring for patients in Hong Kong. Journal of Clinical Nursing. 2005;14:510–517. doi: 10.1111/j.1365-2702.2004.01072.x. [DOI] [PubMed] [Google Scholar]
- Dileo C., Bradt J. Music therapy - Applications to stress management. In: Lehrer, Woolfolk, Sinne, editors. Principles and practices of stress management. Guilford Press; New York: 2007. pp. 519–544. [Google Scholar]
- Fallek R., Kristen Corey K., Aamna Qamar A., Vernisie S., Hoberman A., Selwyn P., Lounsbury D. Soothing the heart with music: A feasibility study of a bedside music therapy intervention for critically ill patients in an urban hospital setting. Palliative & Supportive Care. 2019:1–8. doi: 10.1017/S1478951519000294. [DOI] [PubMed] [Google Scholar]
- Ferreri L., Mas-Herrero E., Zatorre R., Ripollés P., Gomez-Andres A., Alicart H., Fornells A. Dopamine modulates the reward experiences elicited by music. Proceedings of the National Academy of Sciences. 2019;116(9):3793–3798. doi: 10.1073/pnas.1811878116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geipel J., Koenig J.H., Resch F., Kaess M. Music-based interventions to reduce internalizing symptoms in children and adolescent: A meta-analysis. Journal of Affective Disorders. 2018;225:647–656. doi: 10.1016/j.jad.20. [DOI] [PubMed] [Google Scholar]
- George S.A.S. Influence of music on operation theatre staff. Journal of Anaesthesiology, Clinical Pharmacology. 2011 doi: 10.4103/0970-9185.83681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giordano F., Zanchi B., De Leonardis F., Rutigliano C., Esposito F., Brienza N.…Santoro N. The influence of music therapy on preoperative anxiety in pediatric oncology patients undergoing invasive procedures. The Arts in Psycotherapy. 2020;68(101649) ISSN 0197-4556. [Google Scholar]
- Grocke D., Wigram T. Jessica Kingsley Publishers; London and Philadelphia: 2007. Receptive methods in music therapy. Techniques and clinical applications for music therapy clinicians, educators and students. (ISBN978 1 84310 4131 ed.) [Google Scholar]
- Honey M., Wang W.Y. New Zealand nurses perceptions of caring for patients with influenza A (H1N1) Nursing in Critical Care. 2013;18:63–69. doi: 10.1111/j.1478-5153.2012.00520.x. [DOI] [PubMed] [Google Scholar]
- Kang L., Li Y., Hu S. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. The Lancet Psychiatry. 2020;2020 doi: 10.1016/S2215-0366(20)30047-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim Y. Nurses’ experiences of care for patients with Middle East respiratory syndrome-coronavirus in South Korea. American Journal of Infection Control. 2018;46(7):781–787. doi: 10.1016/j.ajic.2018.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lancet T. Protecting healthcare workers. The Lancet (2020) COVID-19. 2020;395(10228):922. doi: 10.1016/S0140-6736(20)30644-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu C., Wang H., Zhou L. Sources and symptoms of stress among nurses in the first Chinese anti-Ebola medical team dur ing the Sierra Leone aid mission: A qualitative study. International Journal of Nursing Sciences. 2019;6(2):187–191. doi: 10.1016/j.ijnss.2019.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McConnell T., Porter S. Music therapy for palliative care: A realist review. Palliative & Supportive Care. 2017;15:454–464. doi: 10.1017/S1478951516000663. [DOI] [PubMed] [Google Scholar]
- Mofredj A., Alaya S., Tassaioust K. Music therapy, a review of the potential therapeutic benefits for the critically ill. Journal of Critical Care. 2016;35:195–199. doi: 10.1016/j.jcrc.2016.05.021. [DOI] [PubMed] [Google Scholar]
- Motta Zanin G., Gentile E., Parisi A., Spasiano D. A preliminary evaluation of the public risk perception related to the COVID-19 health emergency in Italy. International Journal of Environmental Research and Public Health. 2020;17:3024. doi: 10.3390/ijerph17093024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfeifer E., Fiedler H., Wittmann M. Enhanced relaxation in students after combined depth relaxation music therapy and silence in a natural setting. The Arts in Psychotherapy. 2019 doi: 10.1016/j.aip.2019.02.006. [DOI] [Google Scholar]
- Raglio A., Imbriani C., Oddone E. Music therapy and Occupational medicine. Giornale Italiano Di Medicina Del Lavoro Ed Ergonomia. 2017;38:257–260. [PubMed] [Google Scholar]
- Robb S., Burns D.C. Reporting guidelines for musicbased interventions. Journal of Health Psychology. 2011;16(2):342–352. doi: 10.1177/1359105310374781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmid W., Rosland J., von Hofacker S. Patient’s and health care provider’s perspectives on music therapy in palliative care - an integrative review. BMC Palliative Care. 2018;17:32. doi: 10.1186/s12904-018-0286-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su J., Weng H., Tsang H. Mental health and quality of life among doctors, nurses and other hospital staff. Stress and Health: Journal of the International Society for the Investigation of Stress. 2009;25(5):423–430. [Google Scholar]
- Tan P., Lester L., Lin A. Music therapy treatments in an inpatient Setting-A randomized pilot study. The Arts in Psychotherapy. 2020 101660. [Google Scholar]
- Trifiletti E., Di Bernardo G., Falvo R. Patients are not fully human: A nurse’s coping response to stress. Journal of Applied Social Psychology. 2014;44(12):768–777. [Google Scholar]
- Van Bortel T., Basnayake A., Wurie F. Psychosocial effects of an Ebola outbreak at individual, community and international levels. Bulletin of the World Health Organization. 2016;94(3):210–214. doi: 10.2471/BLT.15.158543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Steen J., Smaling H., van der Wouden J. Musicbased therapeutic interventions for people with dementia. The Cochrane Database of Systematic Reviews. 2018;7 doi: 10.1002/14651858.CD003477.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Horby P.W., Hayden F.G. A novel coronavirus outbreak of global health concern. Lancet. 2020;395(10223):470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . 2020. World Health Organization. Tratto da Rolling updates on coronavirus disease (COVID-19)https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen [Google Scholar]
- Wigram T., Bonde L. Psycological reactions to music. In: Jacobsen S., IN P., Bonde L., editors. A comprehensive guide to music therapy. Jessica Kingsley Publishers; London: 2019. pp. 204–208. [Google Scholar]
- Xiang Y.T., Yang Y., Li V. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. The Lancet Psychiatry. 2020 doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaka A., Shamloo S., Fiorente P., Tafuri A. COVID-19 pandemic as a watershed moment: A call for systematic psychological health care for frontline medical staff. Journal of Health Psychology. 2020 doi: 10.1177/1359105320925148. [DOI] [PubMed] [Google Scholar]
- Zhang C., Yang L., Liu S., Ma S., Wang Y., Cai Z.…Zhang B. Survey of insomnia and related social psychological factors among medical staff involved in the 2019 novel coronavirus disease outbreak. Frontiers in Psychiatry. 2020;11:306. doi: 10.3389/fpsyt.2020.00306. [DOI] [PMC free article] [PubMed] [Google Scholar]