Abstract
Background
during the COVID-19 pandemic, the number of Acute Care Surgery procedures performed in Spanish hospitals decreased significantly. The aim of this study was to compare Acute Care Surgery activity during the COVID-19 pandemic and during a control period.
Material and methods
a multicenter retrospective cohort study was performed including patients who underwent Acute Care Surgery in three tertiary care hospitals in Spain during a control (11th March 2019 to 21st April 2019) and a pandemic (16th March 2020 to 26th April 2020) period. Type of surgical procedures, patients' features and postoperative complications were compared.
Results
two hundred and eighty-five and 117 patients were included in each group. Mean number of patients who underwent Acute Care Surgery during the control and pandemic periods was 2.3 and 0.9 patients per day and hospital (p < 0.001), representing a 58.9% decrease in Acute Care Surgery activity. Time from symptoms onset to patient arrival at the Emergency Department was longer during the pandemic (44.6 vs. 71.0 h, p < 0.001). Surgeries due to acute cholecystitis and complications from previous elective procedures decreased (26.7% vs. 9.4%) during the pandemic, while bowel obstructions and abdominal wall hernia surgeries increased (12.3% vs. 22.2%) (p = 0.001). Morbidity was higher during pandemic period (34.7% vs. 47.1%, p = 0.022), although this difference was not statistically significant in the multivariate analysis. Reoperation rate (17.9% vs. 12.8%, p = 0.212) and mortality (6.7% vs. 4.3%, p = 0.358) were similar in both groups.
Conclusion
during the COVID-19 pandemic, a significant reduction in the performance of Acute Care Surgery procedures was observed. Moreso, a longer time from symptoms onset to patient arrival at the Emergency Department was noted. Higher morbidity was observed in patients undergoing Acute Care Surgery during the pandemic period, although there was not any difference in mortality or reoperation rate.
Keywords: Acute care surgery, Emergency surgery, COVID-19, SARS-CoV-2, Pandemic
Highlights
-
•
Acute Care Surgery Activity was decreased during the COVID-19 pandemic.
-
•
A higher delay of the patients presenting in the Emergency Department was observed during the pandemic period.
-
•
During the COVID-19 pandemic, a higher morbidity rate was found in patients undergoing Acute Care Surgery.
1. Introduction
In late December 2019, 7 patients presenting unusual pneumonia were detected in Wuhan (China) and reported to the Chinese Center for Disease Control and Prevention [1]. Since then, the disease, called COVID-19, has spread all around the world; and is considered a pandemic since 11 March 2020 according to the World Health Organization [2].
During the pandemic, health care systems and hospitals had to adapt their structures to this new scenario. Intensive care capacity had to be increased, transforming recovery facilities and even waiting rooms into ICU beds. Medical and nursing staff were redistributed and outpatient clinic visits were cancelled or conducted online or by phone [3,4]. Departments of Surgery were, for sure, affected by these changes; elective procedures were delayed, staff members were allocated to reinforce the ICU and surgeons were reorganized in closed working groups to avoid infections between them [5,6]. Certainly, another one of these changes was a reduction in Acute Care Surgery Activity (ACSA).
Reduction in ACSA was clearly observed in Spanish hospitals [7], taking into account that Spain was one of the most affected countries by COVID-19. However, this has also been observed in other territories seriously hit by the pandemic, such as Italy [8].
The aim of this study was to analyze the reduction in ACSA. ACSA during COVID-19 pandemic was compared with a control period to quantify this reduction. Also, the main causes and consequences of this change in ACSA were studied.
2. MATERIAL and METHODS
A multicenter, retrospective and analytic cohort study was performed. Patients were included if they underwent Acute Care Surgery (ACS) in the Department of Surgery of one of the hospitals included in the study (three tertiary care hospitals in Spain, two of them in Madrid and the third one in Barcelona) during the study periods. Patients who underwent minor surgical procedures were excluded.
Two different periods of study were selected. Pandemic period included patients who underwent ACS from the 16th of March 2020 to the 26th of April 2020, because at that time the pandemic was well stablished, both in Madrid and in Barcelona. For the control period the dates ranging from the 11th of March 2019 up to the 21st of April 2019 were selected, in order to include a similar number of days in the same season of the year, though before the pandemic started.
Medical records were reviewed to fill in a database including demographic features of the patients, diagnoses, delay of the patient to present at the Emergency Department, SOFA score at the Emergency Department, delay of the surgical procedure, COVID status of the patient at the time of surgery, surgical technical details, length of stay, morbidity analyzed according to Clavien-Dindo classification and mortality. Most common diagnoses were assessed independently, while all other medical conditions (such as contaminated cases or trauma patients, for instance) were included as “other diagnoses”.
Delay of the patient to present at the Emergency Department was considered as the time between onset of symptoms and the arrival of the patient to the Emergency Department. Delay of the surgical procedure was considered as the lapse of time between the patient's arrival and the beginning of the surgery itself. COVID status of the patient was classified as negative (Reverse transcription polymerase chain reaction (RT-PCR) for SARS-CoV-2 negative), not-suspected (not tested for SARS-CoV-2 and no clinical symptoms), suspected (clinical symptoms of COVID without SARS-CoV-2 test or with negative RT-PCR) and positive (RT-PCR for SARS-CoV-2 positive).
Stata® 13.1 (StataCorp, Texas, USA) was used for statistical analysis. Differences with p < 0.05 were considered statistically significant. Quantitative variables were expressed as mean (95% confidence interval (CI)) and categorical ones as number of patients (percentage). Univariate analysis was performed with Fisher, X2, and Student-T tests, as appropriate.
The possible relationship between the study period and the morbidity was analyzed using a logistic regression model. Variables that were statistically or clinically (Odds Ratio (OR) > 1.5, OR<0.67, Pearson correlation coefficient>0.1 or Pearson correlation coefficient<0.1) associated with both the study period and the morbidity were included as possible confounding variables. Those model with a change in less than 10% the OR for period were studied in order to choose the final regression model.
Authors declare that they have no conflict of interest. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required. This research was approved by the Institutional Review Board (Code: 20/282-E_COVID). Research is being reported in line with the STROCCS criteria [9]. This study was registered in the Chinese Clinical Trial Registry (Code: ChiCTR2000033052).
3. RESULTS
Four hundred and two patients were included in the study. Two hundred and eighty-five (70.90%) underwent surgery during the control period; one hundred and seventeen (29.10%) during the pandemic. Mean age was 54.3 (95% CI 52.3–56.3) and 184 (45.77%) of the patients were female. Hypertension, dyslipidemia, diabetes mellitus and ischemic heart disease were present in 132 (32.84%), 88 (21.89%), 43 (10.70%) and 34 (8.46%) patients respectively. According to the American Society of Anesthesiology Classification (ASA) 150 (37.31%) patients were ASA I, 156 (38.81%) ASA II, 79 (19.65%) ASA III and 17 (4.23%) ASA IV or V.
The most common diagnoses were acute appendicitis (128 patients, 31.84%), anorectal abscess (53 patients, 13.18%), complications of a previous elective procedure (49 patients, 12.19%), acute cholecystitis (38 patients, 9.45%), bowel obstruction (34 patients 8.46%) and abdominal wall hernia reparation (27 patients, 6.72%).
Mean delay of the patient to present at the Emergency Department and mean delay of the surgical procedure were 52.7 (95% CI 45.5–59.8) and 12.4 (95% CI 10.9–13.9) hours respectively. Mean SOFA score was 1.2 (95% CI 0.9–1.5), with 129 (36.24%) patients with a SOFA score higher than 0.
Three hundred and sixty-four (90.55%) patients were not suspected for COVID, 31 (7.71%) were COVID negative, 4 (1.00%) were suspected for COVID and 3 (0.75%) were COVID positive.
Laparoscopy was performed in 196 (57.82%) patients, but 8 (4.08%) of them required conversion to an open approach.
Mean length of hospital stay was 11.1 (95% CI 8.6–13.6) days. Eighty-five patients (21.14%) were admitted to Intensive Care (Unit), with a mean length of stay in this unit of 11.0 (95% CI 6.3–15.7) days. One-hundred and fifty-four (38.31%) patients suffered at least one procedural complication during the postoperative course and these were classified as Clavien-Dindo I or II, III, IV and V in 58 (37.66%), 41 (26.62%), 38 (24.68%) and 17 (11.04%) patients respectively. Five (4.55%) patients developed COVID-19 during the postoperative course. Intrabdominal sepsis, surgical site infection, respiratory complications, postoperative ileus and bleeding were observed in 76 (18.91%), 49 (12.19%), 43 (10.70%), 39 (9.70%) and 26 (6.47%) patients respectively. Sixty-six (16.42%) patients required reintervention and 24 (5.97%) died during the postoperative course.
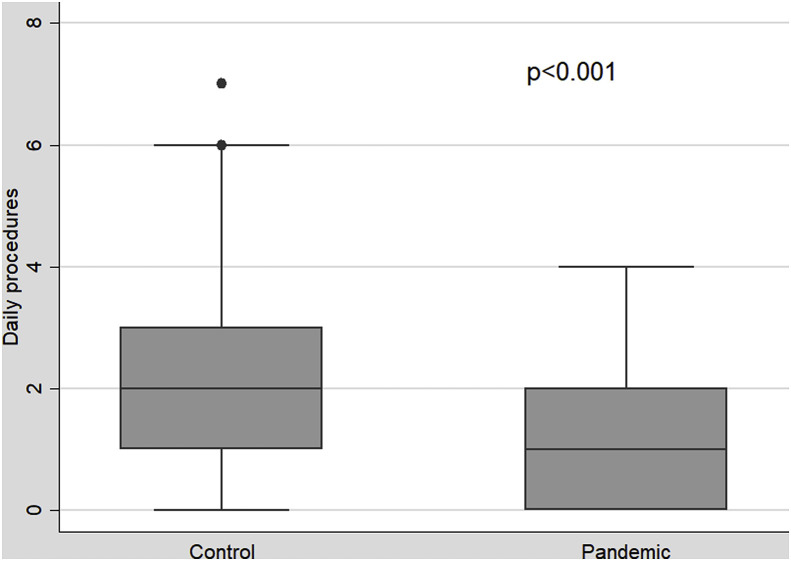
Mean number of patients who underwent ACS during the control and pandemic periods was 2.3 and 0.9 patients per day per hospital respectively (difference 1.3 patients per day, CI 1.0–1.7, p < 0.001) (Fig. 1 ) and this implies a 58.95% decrease in the ACSA during the pandemic period.
Fig. 1.
Box plot comparing the number of daily procedures during the Control and Pandemic Period.
Table 1 compares the patient's characteristics in both periods of time. A statistically significant increase was observed on the delay of the patient to present at the Emergency Department (44.6 vs. 71.0 h, p < 0.001). Also, a non-statistically significant increase in the SOFA score was observed during the pandemic period (SOFA score higher than 0 in 33.87% vs. 41.67% patients respectively, p = 0.160). Laparoscopic approach was more frequently performed in the control period (63.64%, vs. 43.30%, p < 0.001). This difference persisted even when the variable laparoscopic approach was adjusted with the variable diagnoses using a logistic regression (OR = 3.4, p = 0.001).
Table 1.
Comparison of patients undergoing Acute Care Surgery in the Control and Pandemic Period. Quantitative variables are expressed as mean (95% Confidence interval) and qualitative ones as number of patients (percentage).
| Control | Pandemic | p | |
|---|---|---|---|
| Mean age (years) | 55.0 (52.7–57.3) | 52.6 (48.7–56.5) | 0.276 |
| Gender (% female) | 145 (50.88%) | 39 (33.38%) | 0.001 |
| High blood pressure (% patients) | 89 (31.23%) | 43 (36.75%) | 0.284 |
| Dyslipidemia (% patients) | 66 (23.16%) | 22 (18.80%) | 0.338 |
| Diabetes Mellitus (% patients) | 36 (12.63%) | 7 (5.98%) | 0.050 |
| Ischemic Heart Disease (% patients) | 26 (9.12%) | 8 (6.84%) | 0.454 |
| American Society of Anesthesiology Classification (% III-IV-V) | 69 (24.21%) | 27 (23.08%) | 0.809 |
| Mean delay of the patient to present in the Emergency Department (hours) | 44.6 (36.6–52.7) | 71.0 (56.9–85.0) | <0.001 |
| Mean delay of the surgery (hours) | 12.4 (10.5–14.4) | 12.3 (10.0–14.6) | 0.930 |
| SOFA score (% patients with SOFA>0) | 84 (33.87%) | 45 (41.67%) | 0.160 |
| Laparoscopic approach (% patients) | 154 (63.64%) | 42 (43.30%) | 0.001 |
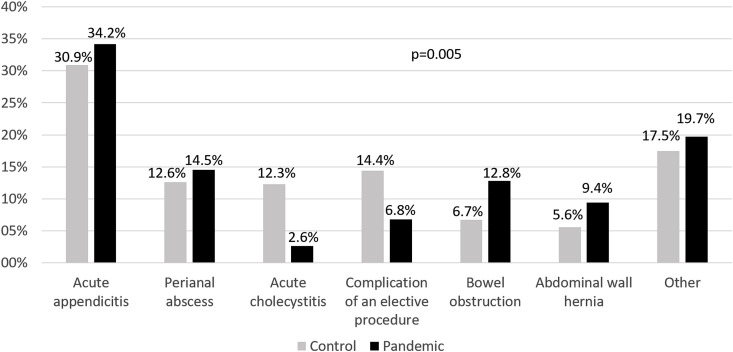
A change in the medical conditions that required surgery took during the pandemic (Fig. 2 ). Even though the percentage of patients who underwent ACS due to acute appendicitis or anorectal abscess were similar in both periods, acute cholecystitis and surgeries required for treating complications of previous elective procedures decreased (26.67% vs. 9.40%) and at the same time, surgical interventions due to intestinal obstruction and reparation of abdominal wall hernia increased (12.28% vs. 22.22%). Interestingly, in the group of patients diagnosed with acute appendicitis, a significant increase in the rate of complicated appendicitis was observed during the pandemic period (7.95% vs. 42.50%, p < 0.001).
Fig. 2.
Bart chart comparing the diagnoses during the control and pandemic periods.
Table 2 compares the postoperative evolution during both periods. Length of hospital stay was longer in the control period, although this difference was not statistically significant (12.2 vs. 8.5 days, 0 = 0.182). Morbidity was higher in the pandemic period (34.74% vs. 47.01%, p = 0.022) but reintervention rates (17.89% vs. 12.82%, 0.212) and mortality (6.67% vs. 4.27%, p = 0.358) were similar.
Table 2.
Comparison of postoperative results in both periods.
| Control | Pandemic | P | |
|---|---|---|---|
| Mean length of stay (days) | 12.2 (8.8–15.6) | 8.5 (6.6–10.3) | 0.182 |
| Intensive Care Unit admission (%) | 65 (22.81%) | 20 (17.09%) | 0.203 |
| Complications (%) | 99 (34.74%) | 55 (47.01%) | 0.022 |
| Clavien-Dindo classification (% Clavien-Dindo III-V) | 68 (68.69%) | 28 (50.91%) | 0.029 |
| Intrabdominal sepsis (%) | 51 (17.89%) | 25 (21.37%) | 0.419 |
| Respiratory complication (%) | 29 (10.18%) | 14 (11.97%) | 0.598 |
| Surgical site infection (%) | 39 (13.68%) | 10 (8.55%) | 0.153 |
| Postoperative ileus (%) | 21 (7.37%) | 18 (15.38%) | 0.014 |
| Bleeding (%) | 12 (4.21%) | 14 (11.97%) | 0.004 |
| Reoperation (%) | 51 (17.89%) | 15 (12.82%) | 0.212 |
| Exitus (%) | 19 (6.67%) | 5 (4.27%) | 0.358 |
Quantitative variables are expressed as mean (95% Confidence interval) and qualitative ones as number of patients (percentage).
After performing the multivariate analysis, which included both delay of the patient to present at the Emergency Department and laparoscopic approach as confounding variables, pandemic period was not statistically associated with morbidity (OR = 1.2, 95% CI 0.7–2.2, p = 0.501).
4. Discussion
With the development of the COVID-19 pandemic, some authors have published their surgical experience during the pandemic [6,10,11] or have reported their protocol to treat surgical patients with COVID-19 [[12], [13], [14], [15], [16], [17], [18]]. Nevertheless, as far as we know, the reduction of ACSA observed during this pandemic has never been properly reported. Only two letters to the editor have been published [7,8]. The first one reports the initial experience of our group [7]; the second one recalls the experience of italian colleagues [8]. Furthermore, we have not found reports that study ACSA at any other pandemic throughout time. Nevertheless, two studies reported a decrease in surgical activity during Ebola pandemic [19,20].
During the pandemic the daily number of ACS procedures decreased from 2.3 to 0.9, cutting in half the activity that took place during the control period. This decline in the activity should be carefully taken into account in those regions where the pandemic is still developing, as well as if a new outbreak takes place. The resources usually assigned to ACS could then be reoriented to attend patients with COVID-19, increasing the potential resources of the health systems by for example shutting down operating rooms and using anaesthesia machinery as mechanical ventilators in the Intensive Care Units.
Several factors could explain the reduction in ACS procedures. First of all, patients could be delaying attending the Emergency Departments to avoid being infected with the SARS-CoV-2 [8,21]. In our series, a statistically significant increase in the time between symptoms onset and patient's arrival at the Emergency Department was observed. This delay has also been noted in other Emergency Departments; for example, Lazzerini et al. reported a case series of children that delayed their visit to the Emergency Department due to fear of infection or collapse of the health system. Clinical outcome of these paediatric patients was discouraging [22]. It has been seen that that this delay could result in more advanced diseases [23]. And in accordance with this finding, in our series a higher proportion of patients who underwent appendectomy presented complicated appendicitis (8.0% vs. 42.5%, p < 0.001). The increase in severity was also observed with SOFA scale, although this difference was not statistically significant.
The reduction in ACSA could also be explained by modifications in lifestyle habits. For instance, changes in dietary fat quantity and quality could decrease the incidence of biliary complications, such as acute cholecystitis. And this reduction was in fact observed in our series. However, treating these conditions medically, rather than surgically could be another plausible explanation and could even demonstrate a trend in choosing more conservative therapies in order to avoid hospitalization. This strategy has been proposed by some authors, for example, to treat acute appendicitis [24]. This hypothesis could then explain why certain procedures that do not count with alternative treatments, such as incarcerated abdominal wall hernia reparation or bowel obstruction, were increased during the pandemic period, while surgical procedures such as appendicectomy or anorectal abscess drainage remained stable, and cholecystectomy was less frequently performed.
Finally, another important circumstance that could explain the reduction in ACSA could be the fact that lots of scheduled surgeries were delayed or even cancelled during the pandemic period. This way, postoperative patients that required reintervention decreased, contributing to the global drop of surgical activity.
When analysing the surgical procedures performed during the pandemic period, we also observed a reduction in the proportion of patients undergoing a laparoscopic approach (63.6%, vs. 43.3%, p < 0.001). This difference remained even when it was adjusted with diagnoses. The raise in performing an open surgical approach could be related to having more patients with a complicated course, but fear of spreading COVID-19 infection with laparoscopic aerosols could also explain this shift [25].
Finally, we also compared the postoperative course in both groups of patients. Mean length of hospital stay was shorter during the pandemic period. Probably, this finding is due to early discharge implemented during the COVID-19 pandemic to decrease the risk of nosocomial infection.
Complications were more common during the pandemic period. Greater severity of the patients could be the most plausible explanation for the higher morbidity we experienced, as the complication rate was not statistically associated to the pandemic period when a multivariate analysis was performed. Moreover, although morbidity was higher in the pandemic period, reoperation rate and mortality were similar in both groups; at the same time the percentage of severe complications was higher in the control period group. These findings suggest that minor complications were more common during the pandemic because delayed and more severe patients underwent surgery, but severe complications were probably similar in both groups.
Regarding post-surgery complications, only bleeding and postoperative ileus were statistically increased during the pandemic period. It is noteworthy the fact that 4.6% of the patients in the pandemic period group developed COVID-19 during the recovery. COVID-19 during postoperative stay could either represent nosocomial infection or a delayed presentation of a preoperative infection. It would be interesting to analyze if patients developing COVID-19 during the postoperative course have higher morbidity than patients without this disease. In any case, more patients would be needed to perform this particular analysis.
The main limitation of this study was that patients undergoing non-operative treatment could not be studied. The retrospective design of the project could also be considered a weakness. To avoid this limitation, data from both periods were collected using the same methodology. The main strengths of our paper were that a significant number of patients were included and that it was performed in three tertiary care hospitals located in Spain, where the pandemic has been really severe.
5. Conclusions
During the COVID-19 pandemic period a significant reduction was observed in the number of ACS procedures performed. ACSA during this period was reduced to half the activity in the control period. A significant delay of the patients’ arrival at the Emergency Department was also observed. Diagnoses changed during the pandemic period; acute appendicitis and anorectal abscess were similar in both periods, acute cholecystitis and complications from previous elective procedures decreased and bowel obstruction and abdominal wall hernia reparation increased during the pandemic. A higher morbidity was observed in the patients undergoing ACS during the pandemic period, although mortality and reoperation rate did not change.
Funding
No funding was needed to perform this study.
Ethical approval
This research was approved by the Institutional Review Board (Code: 20/282-E_COVID).
Research registration Unique Identifying number (UIN)
-
1.
Name of the registry: Chinese Clinical Trial Registry
-
2.
Unique Identifying number or registration ID: ChiCTR2000033052
-
3.
Hyperlink to your specific registration (must be publicly accessible and will be checked): http://www.chictr.org.cn/showprojen.aspx?proj=53892
Guarantor
The Guarantor is the one or more people who accept full responsibility for the work and/or the conduct of the study, had access to the data, and controlled the decision to publish. Please note that providing a guarantor is compulsory.
Oscar Cano-Valderrama.
Data statement
Data from this study has been considered confidential and are not available.
Provenance and peer review
Not commissioned, externally peer-reviewed.
CRediT authorship contribution statement
Oscar Cano-Valderrama: Conceptualization, Methodology, Formal analysis, Investigation, Data curation, Writing - original draft. Xavier Morales: Methodology, Formal analysis, Investigation, Data curation, Writing - original draft. Carlos J. Ferrigni: Methodology, Formal analysis, Investigation, Data curation, Writing - original draft. Esteban Martín-Antona: Conceptualization, Methodology, Investigation, Writing - review & editing. Victor Turrado: Conceptualization, Methodology, Formal analysis, Investigation, Data curation, Writing - original draft, Writing - review & editing. Alejandro García: Methodology, Formal analysis, Data curation, Writing - review & editing. Yolanda Cuñarro-López: Conceptualization, Methodology, Formal analysis, Writing - original draft. Leire Zarain-Obrador: Methodology, Formal analysis, Data curation, Writing - review & editing. Manuel Duran-Poveda: Conceptualization, Methodology, Writing - review & editing, Supervision. José M. Balibrea: Conceptualization, Methodology, Formal analysis, Writing - review & editing, Supervision. Antonio J. Torres: Conceptualization, Methodology, Formal analysis, Writing - review & editing, Supervision.
Declaration of competing interest
None. No financial support was needed to perform this study.
Acknowledgements
Authors would like to Dr. Marinero for English grammar review.
References
- 1.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese center for disease control and prevention. J. Am. Med. Assoc. 2020 doi: 10.1001/jama.2020.2648. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization . 11th March 2020. Coronavirus Disease 2019 (COVID-19). Situation Report – 51. [Google Scholar]
- 3.Wr Smith AJ Atala, Terlecki R.P., Kelly E.E., Matthews C.A. Implementation guide for rapid integration of an outpatient telemedicine program during the COVID-19 pandemic. J. Am. Coll. Surg. 2020 doi: 10.1016/j.jamcollsurg.2020.04.030. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gagliano A., Villani P.G., Co F.M. COVID-19 epidemic in the middle province of northern Italy: impact, logistics, and strategy in the first line hospital. Disaster Med. Public Health Prep. 2020 doi: 10.1017/dmp.2020.51. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liu Z., Ding Z., Guan X., Zhang Y., Wang X., Khan J. Optimizing response in surgical systems during and after COVID-19 pandemic: lessons from China and the UK – Perspective. Int. J. Surg. 2020;78:156–159. doi: 10.1016/j.ijsu.2020.04.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alvarez Gallego M., Gortázar de Las Casas S., Pascual Migueláñez I. SARS-CoV-2 pandemic on the activity and professional of a General and Digestive Surgery Service in a tertiary hospital. Cir. Esp. 2020 doi: 10.1016/j.ciresp.2020.05.001. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cano-Valderrama O., Morales X., Ferrigni C.J. Reduction in emergency surgery activity during COVID-19 pandemic in three Spanish hospitals. BJS. 2020 doi: 10.1002/bjs.11667. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Patriti A., Eugeni E., Guerra F. What happened to surgical emergencies in the era of COVID-19 outbreak? Considerations of surgeons working in an Italian COVID-19 zone. Updates Surg. 2020 doi: 10.1007/s13304-020-00779-6. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Agha R.A., Abdall-Razak A., Crossley E., Dowlut N., Iosifidis C., Mathew G. The STROCSS 2019 guideline: strengthening the reporting of cohort studies in surgery. Int. J. Surg. 2019;72:156–165. doi: 10.1016/j.ijsu.2017.08.586. [DOI] [PubMed] [Google Scholar]
- 10.Chew M.H., Koh F.H., Ng K.H. A call to arms: a perspective of safe general surgery in Singapore during the COVID-19 pandemic. Singap. Med. J. 2020 doi: 10.11622/smedj.2020049. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aminian A., Safari S., Razeghian-Jahromi A., Ghorbani M., Delaney C.P. COVID-19 outbreak and surgical practice: unexpected fatality in perioperative period. Ann. Surg. 2020 doi: 10.1097/SLA.0000000000003925. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ngoi N., Lim J., Ow S. A segregated-team model to maintain cancer care during the COVID-19 outbreak at an academic center in Singapore. Ann. Oncol. 2020 doi: 10.1016/j.annonc.2020.03.306. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Di Saverio S., Pata F., Gallo G. Coronavirus pandemic and Colorectal surgery: practical advice based on the Italian experience. Colorectal Dis. 2020 doi: 10.1111/codi.15056. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 14.Balibrea J.M., Badia J.M., Rubio Pérez I. Surgical management of patients with COVID-19 infection. Recommend. Spanish Assoc. Surg. Cir. Esp. 2020 doi: 10.1016/j.ciresp.2020.03.001. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Coimbra R., Edwards S., Kurihara H. European Society of Trauma and Emergency Surgery (ESTES) recommendations for trauma and emergency surgery preparation during times of COVID-19 infection. Eur. J. Trauma Emerg. Surg. 2020 doi: 10.1007/s00068-020-01364-7. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Orthopoulos G., Fernandez G.L., Dahle J.L., Casey E., Jabbour N. Perioperative considerations during emergency general surgery in the era of COVID-19: a U.S. Experience. J. Laparoendosc. Adv. Surg. Tech. A. 2020 doi: 10.1089/lap.2020.0266. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 17.De Simone B., Chouillard E., Di Saveiro S. Emergency surgery during the COVID-19 pandemic: what you need to know for practice. Ann. R. Coll. Surg. Engl. 2020 doi: 10.1308/rcsann.2020.0097. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zizzo M., Bollino R., Castro Ruiz C. Surgical management of suspected or confirmed SARS-CoV-2 (COVID-19)-positive patients: a model stemming from the experience at Level III Hospital in Emilia-Romagna. Italy Eur. J. Trauma Emerg. Surg. 2020 doi: 10.1007/s00068-020-01377-2. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bundu I., Patel A., Mansaray A., Kamara T.B., Hunt L.M. Surgery in the time of Ebola: how events impacted on a single surgical institution in Sierra Leone. J. Roy. Army Med. Corps. 2016;162:212–216. doi: 10.1136/jramc-2015-000582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bolkan H.A., Da Bash-Taqi, M Samai, M Gerdin, Jv Schreeb Ebola and indirect effects on health service function in Sierra Leone. PLoS Curr. 2014;19:6. doi: 10.1371/currents.outbreaks.0307d588df619f9c9447f8ead5b72b2d. DOI: 10.1371currents.outbreaks.0307d588df619f9c9447f8ead5b72b2d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Slim K., Veziant J. Urgent digestive surgery, a collateral victim of the COVID-19 crisis? J. Vis. Surg. 2020 doi: 10.1016/j.jviscsurg.2020.04.001. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lazzerini M., Barbi E., Apicella A., Marchetti F., Cardinale F., Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child. Adolesc. Health. 2020 doi: 10.1016/S2352-4642(20)30108-5. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Garcia Virosta M., Ortega I., Ferrero E., AL Picardo. Diagnostic delay during the COIVD-19: liver abscess secondary to acute lithiasic cholecystitis. Cir. Esp. 2020 doi: 10.1016/j.ciresp.2020.04.010. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Collard M., Lakkis Z., Loriau J. Antibiotics alone as an alternative to appendectomy for uncomplicated acute appendicitis in adults: changes in treatment modalities related to the COVID-19 health crisis. J. Vis. Surg. 2020 doi: 10.1016/j.jviscsurg.2020.04.014. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Veziant J., Bourdel N., Slim K. Risks of viral contamination in healthcare professionals during laparoscopy in the Covid-19 pandemic. J. Vis. Surg. 2020 doi: 10.1016/j.jviscsurg.2020.04.010. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]