Abstract
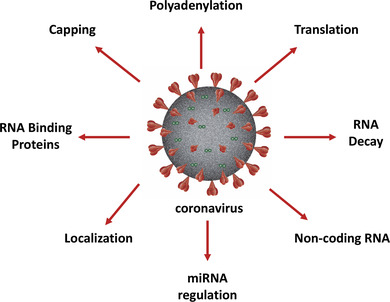
Coronaviruses, including SARS‐Cov‐2, are RNA‐based pathogens that interface with a large variety of RNA‐related cellular processes during infection. These processes include capping, polyadenylation, localization, RNA stability, translation, and regulation by RNA binding proteins or noncoding RNA effectors. The goal of this article is to provide an in‐depth perspective on the current state of knowledge of how various coronaviruses interact with, usurp, and/or avoid aspects of these cellular RNA biology machineries. A thorough understanding of how coronaviruses interact with RNA‐related posttranscriptional processes in the cell should allow for new insights into aspects of viral pathogenesis as well as identify new potential avenues for the development of anti‐coronaviral therapeutics.
This article is categorized under:
RNA in Disease and Development > RNA in Disease
Keywords: coronavirus, miRNA, polyadenylation, RNA stability, translation
Coronavirus interplay with mechanisms associated with the RNA biology of the host cell play a key role in numerous aspects of virus replication and pathogenesis.
1. INTRODUCTION
Coronaviruses, members of the family Coronaviridae in the order Nidovirales, are RNA viruses that represent an important class of human and animal pathogens. Human CoV‐229, NL63, OC43, and HKU1 viruses are endemic in the human population and represent major causes of the common cold in humans (Corman, Muth, Niemeyer, & Drosten, 2018). SARS‐CoV, MERS‐CoV, and now SARS‐CoV‐2 have emerged this century and cause major life‐threatening respiratory infections (Paules, Marston, & Fauci, 2020). Major animal coronavirus pathogens include porcine deltacoronavirus, porcine epidemic diarrhea virus (PEDV), and porcine hemagglutinating encephalomyocarditis virus (PHEV) (Wang, Vlasova, Kenney, & Saif, 2019). Several coronaviruses have served as laboratory models for the group, including mouse hepatitis virus (MHV), infectious bronchitis virus (IBV), and transmissible gastroenteritis virus (TGEV). Collectively these viruses exhibit numerous interesting strategies for viral replication and cellular pathogenesis that result in significant economic and clinical impact around the globe (Cui, Li, & Shi, 2019).
The coronavirus genome consists of a very large 26–32 kb positive‐sense linear RNA fragment that is transcribed into numerous subgenomic mRNAs via a unique discontinuous mechanism that involves priming by a small (65–98 base) leader RNA at intergenic regions to initiate transcription (Sola, Almazán, Zúñiga, & Enjuanes, 2015). While the subgenomic mRNAs encode various proteins, the positive‐sense genomic RNA itself is translated into two large polyproteins (pp1a and pp1ab) from a long open reading frame (ORF) situated at the 5′ half of the genome. Interestingly, the pp1ab protein is generated from a programmed −1 frameshift of the ribosome (Plant & Dinman, 2008). Depending on the individual coronavirus strain, a variable number of structural and accessory proteins are generated from the subgenomic mRNAs produced from the 3′ half of the genome. Numerous RNA elements and structures that have been identified in the genomic RNA are associated with functional and regulatory roles in infection (Madhugiri, Fricke, Marz, & Ziebuhr, 2016). Collectively these viral regulatory elements and proteins generate an effective molecular arsenal that results in the effective replication of the virus as well as usurping numerous aspects of host cell biology.
As a pathogen that possesses an RNA genome, coronavirus transcripts must actively and effectively interface with numerous aspects of the RNA biology of the infected cell (see graphical abstract). These virus–host molecular interactions can potentially have major influences on cellular RNA processing, transport, translation, stability, and RNA‐associated regulatory processes. This virus–host interface may include relatively straightforward aspects such as the direct commandeering of cellular RNA binding proteins (RBPs) and RNA machineries for use in viral replication and packaging. However, the virus–host RNA interface can also dramatically impact pathogenesis and cytopathology as coronaviruses disrupt these essential posttranscriptional processes in the host cell. This latter impact has been relatively understudied in the field to date. The purpose of this review is thus to provide an in‐depth overview of coronavirus interactions with cellular posttranscriptional machinery and RNA regulatory mechanisms to provide insight into this important area of virus–host interactions.
2. CORONAVIRUS CAPPING AND POLYADENYLATION
Coronaviruses possess a conventional 7meGppp cap at the 5′ end of their positive‐sense genomic and mRNAs and also contain 2′O‐methylations at their 5′ terminal nucleotides (Chen & Guo, 2016). These 5′ terminal 2′O‐methylations are important for viral evasion of cellular innate antiviral effectors as the host IFIT1 (interferon‐induced protein with tetratricopeptide repeats 1) protein will recognize versions of viral caps that lack these modifications and activate a robust interferon response (Abbas et al., 2017; Daffis et al., 2010). A complex of viral nonstructural (nsp) proteins, including, nsp13 (RNA triphosphatase), nsp14 (N7‐methyltransferase), and nsp16 (2′O‐methyltransferase), is responsible for capping of the 5′ end of coronavirus transcripts (Chen & Guo, 2016). Curiously, the viral capping enzyme or guanylyltransferase has not been identified to date. Thus, although there a few short KxDG amino acid motifs in the nsp1ab polyprotein that have been noted to represent a conserved motif of viral capping enzymes (Li, Rahmeh, Morelli, & Whelan, 2008), one cannot formally rule out the possibility that a cellular factor provides guanylyltransferase activity. If this were the case, we speculate due to the cytoplasmic nature of the event that perhaps this might be a cellular enzyme associated with cytoplasmic recapping of cellular mRNAs (Trotman & Schoenberg, 2019). Finally, all of the genomic and subgenomic mRNAs of SARS‐CoV start with a transcribed A residue instead of a G residue that is found at the 5′ terminus in the majority of cellular mRNAs. Interestingly, essentially all cellular mRNAs that start with a transcribed A residue get modified with an m6A modification by the CAPAM protein (Cowling, 2019). It will be interesting to investigate whether or not coronavirus genomic RNA and mRNAs have a similar m7G(5′)ppp(5′)m6Am 5′ end structure or not, and implications thereof to virus–host interactions.
Coronaviruses contain a poly(A) tail at the 3′ end of their positive‐sense RNAs, but it is not clear how the adenylate stretch is added. Recent studies have demonstrated that the viral nsp8 protein contains terminal adenylase activity that may be directed by the short oligo U tract found on the 5′ end of (−) strand viral RNA replication intermediates (Hofmann & Brian, 1991; Imbert et al., 2006; Tvarogová et al., 2019). Interestingly, poly(A) tail length appears to be differentially regulated at different times postinfection, ranging from 45 to 65 nucleotides in length (Peng et al., 2016; Shien, Su, & Wu, 2014; Wu, Ke, Liao, & Chang, 2013). While this change in poly(A) tail length could simply reflect viral RNA dependent RNA polymerase slippage on the terminal homopolymer during the production of the termini of (−) strand templates or viral mRNAs, it could also potentially influence the assembly of RBPs on the poly(A) tail that promote translation or replication. The coronavirus poly(A) tail binds the cellular poly(A) binding protein (PABP) to promote the translation of viral mRNAs (Spagnolo & Hogue, 2001). The bovine coronavirus nucleocapsid N protein has also been shown to be able to bind to the poly(A) tail of viral RNAs. N protein binding to the poly(A) tail represses translation of the viral RNA and may recruit viral replication complexes through an interaction with nsp9 (Tsai, Lin, Lin, Lo, & Wu, 2018). It is important to note, however, that N protein is not innately a translational repressor as binding to the 5′ UTR has been shown to increase viral mRNA translation (Nelson, Stohlman, & Tahara, 2000; Tahara, Dietlin, Nelson, Stohlman, & Manno, 1998), perhaps by disrupting repressive RNA structures or protein–RNA interactions.
While it is clear that the terminal cap and poly(A) tails play vital roles in the life cycle of coronaviruses, we currently have relatively little insight into the enzymes and detailed mechanisms of how they are generated. Additional studies in this area, therefore, would be fruitful in advancing our molecular understanding of viral terminal RNA modifications. Since (based on studies with other cytoplasmic RNA viruses) these terminal RNA modifications are likely one of the few aspects of coronavirus RNA biology that do not usurp host cell enzymes, it may be an area for the development of broad‐spectrum anti‐coronavirus drugs. For example, a better understanding of the coronavirus nsp interactome and the molecular description of enzymatic functions in capping may provide insight into a novel avenue of coronaviral therapeutic targets as has been proposed for other virus families (Issur, Picard‐Jean, & Bisaillon, 2011). The viral nsp14 MTase activity, for example, is known to have a unique structure that significantly differs from canonical MTases (Ferron et al., 2018), making it an attractive target for small molecule inhibitors. Finally, one of the speculated targets of the FDA‐approved antiviral drug ribavirin is the viral RNA capping reaction (Ogino & Ogino, 2017). This adds some support for the validity of this aspect of viral RNA biology for drug targeting.
3. CORONAVIRUS mRNA TRANSLATION
The translation of most coronavirus mRNAs is cap‐dependent (Cencic et al., 2011) and, as outlined below, arguably represents a goldmine for studying unconventional aspects of regulated protein synthesis. Interestingly, coronavirus mRNAs use many of the previously described noncanonical mechanisms to regulate protein production and gain access to ORFs (Rodnina et al., 2020). Well‐conserved upstream ORFs are located in genomic (but not subgenomic) coronavirus mRNAs and downregulate translation as a result of the pausing of scanning ribosomes on these upstream AUG start codons (C. H. Wu, Chen, & Yeh, 2014). A programmed −1 frameshift is used on viral genomic mRNAs to generate the ORF1ab polyprotein. The frameshifting signal consists of a slippery site (UUUAAAC) followed by a dynamic RNA pseudoknot structure (Caliskan, Katunin, Belardinelli, Peske, & Rodnina, 2014; Cho, Lin, Chou, Hsu, & Chang, 2013; Giedroc, Theimer, & Nixon, 2000; Napthine, Liphardt, Bloys, Routledge, & Brierley, 1999; Ritchie, Foster, & Woodside, 2012). Curiously, ribosomal profiling studies have not observed the substantial ribosome pause in this region as one might expect (Irigoyen et al., 2016). The phenomenon of leaky scanning, or the occasional bypassing of the first AUG by the ribosome, is observed on the coronavirus N mRNA (Senanayake & Brian, 1997). This leaky scanning generates a small protein called the I protein (or nsp9b) that has been shown to play a role in evading innate immunity and causes enhanced cytopathicity (Shi et al., 2014). Ribosome shunting, a phenomenon that involves discontinuous scanning by the assembled ribosome on the mRNA, has been inferred in the translation of the TGEV 3b protein (O'Connor & Brian, 2000). Finally, IRES elements, structured RNA domains that mediate cap‐independent loading of ribosomes, have been identified in mRNA 3 of IBV and MHV (Liu & Inglis, 1992; Thiel & Siddell, 1994). Collectively, coronavirus mRNAs use many tricks to regulate their gene expression at the level of protein synthesis to achieve maximal gene expression, RNA replication and pathogenesis. Understanding the RNA structural basis for these various forms of translational regulation, therefore, may be an interesting avenue for broad‐spectrum anti‐coronaviral drug development. Virtual screening for small molecules that will interfere with coronavirus genomic RNA pseudoknot formation, for example, has identified an inhibitor that will block the −1 frameshifting from SARS‐CoV mRNA (Hermann, 2016; Park, Kim, & Park, 2011).
MHV, MERS‐CoV, and SARS‐CoV, and likely all coronaviruses, repress host cell translation during infection. While this may simply occur as part of an integrated stress response to infection (Raaben, Groot Koerkamp, Rottier, & de Haan, 2007), there appear to be several virus‐specific effectors at play as well. Coronavirus infection affects the translation of host cell mRNAs, largely shifting the transcripts from polysomes to 80S monosomes, through multiple possible mechanisms. MHV infection has been shown to induce 28S rRNA cleavage via the induction of RNAse L, likely resulting in a reduction in the number of active ribosomes (Banerjee, An, Zhou, Silverman, & Makino, 2000). The SARS‐CoV (but interestingly not the MERS‐CoV) nsp1 protein has been shown to bind to 40S ribosomal subunits and likely interfere with their function (Kamitani, Huang, Narayanan, Lokugamage, & Makino, 2009) as there is clear evidence that translation initiation is repressed during SARS‐CoV infections (Lokugamage, Narayanan, Huang, & Makino, 2012). A recent structural study has indicated that the C‐terminus of the SARS‐CoV‐2 nsp1 protein binds to the ribosome and directly obstructs the mRNA entry tunnel (Thoms et al., 2020). Interestingly, three other coronaviral proteins have been demonstrated to interface with components of the protein synthesis machinery. The N‐terminal region of the spike protein (S) of SARS‐CoV and IBV bind to eIF3F, a factor that promotes the interaction between the 43S preinitiation complex and the mRNA (Xiao, Xu, Yamada, & Liu, 2008). The nucleocapsid (N) protein can bind and induce the aggregation of eIF1‐a, a GTP/GDP‐regulated protein that helps to guide the charged tRNA to the ribosome (Zhou et al., 2008). Finally, the small 122 amino acid, membrane‐associated SARS‐CoV 7a protein will inhibit cellular protein synthesis when transfected into cells (Kopecky‐Bromberg, Martinez‐Sobrido, & Palese, 2006). In summary, coronaviruses appear to use a variety of strategies to commandeer cellular protein synthesis during infection. These complementary mechanisms have likely resulted from the natural pressures on the virus to effectively usurp this key part of the cytoplasmic RNA machinery to generate the array of viral proteins needed for the effective production of progeny virions.
A final aspect of coronavirus translation to consider is the potential impact of codon optimality, the relationship of codon usage on an mRNA to the availability of the cognate tRNA in the cell (Hanson & Coller, 2018). Codon optimality influences the rate of protein synthesis, and thus ribosome movement, along the mRNA. The rate of ribosome movement also influences the rate of decay of the mRNA, perhaps through the CCR4‐Not complex (Buschauer et al., 2020; Hia et al., 2019). Interestingly, SARS‐CoV and the novel SARS‐CoV‐2 viruses contain a higher level of optimal codons relative to other coronaviruses, indicating that these pathogens may have adapted for highly efficient protein synthesis and mRNA stability in human cells (Yang & Chen, 2020).
There are several key knowledge gaps remaining in our understanding between coronaviruses and the cellular protein synthesis machinery. A more precise understanding of the mechanistic underpinnings of how coronaviruses repress the translation of cellular mRNAs could help focus drug discovery efforts towards viral‐specific aspects and avoid affecting global cellular protein synthesis. Additional insight into RNA structural elements that impact frameshifting and other ribosomal gymnastics on the viral mRNA could yield novel targets for therapeutics. Finally, characterizing the impact of viral codon optimality in relation to the efficiency of coronavirus infection could provide insights into host range adaptations that could help predict the likelihood and severity of future emerging members of this virus family.
4. CORONAVIRUSES AND NUCLEAR‐CYTOPLASMIC SHUTTLING
As noted above, several RBPs relocalize from the nucleus to the cytoplasm during coronavirus infections (Shi, Yu, & Lai, 2003; Sola, Galán, et al., 2011; Li et al., 2018). This phenomenon is likely attributable to a combination of virus‐induced alterations in the export/import machinery associated with the nuclear pore as well as active sequestration of these proteins in the cytoplasm by viral RNAs. Viral repression of nuclear pore activity is a common strategy used by many RNA viruses to handicap cellular gene expression (Yarbrough, Mata, Sakthivel, & Fontoura, 2014). SARS‐CoV nsp1 protein has been shown to interact with Nup93, a protein of the nuclear pore complex that impacts gene expression in multiple ways (i.e., Gozalo et al., 2020). Through this interaction, nsp1 induces alterations in the nucleo‐cytoplasmic distribution of nucleolin (Gomez, Abrar, Dodhia, Gonzalez, & Nag, 2019). The small (63 amino acid) SARS ORF6 protein interacts with karyopherin α2 (aka importin α) (Frieman et al., 2007) and has a significant effect on the import of numerous key cellular transcription factors and other nuclear proteins (Sims et al., 2013).
Overall, the influence of coronavirus infections on cellular nuclear pore functions is an interesting area of host–virus interplay that warrants further exploration. It is interesting to note that other RNA viruses interact with or proteolytically cleave various Nups and affect nucleo‐cytoplasmic transport during infection (Yarbrough et al., 2014). Thus, it seems likely that the described CoV nsp1 and ORF6 interactions, as well as potentially other coronaviral proteins (Gordon et al., 2020), could be significantly contributing to cytopathology via this mechanism.
5. CORONAVIRUSES AND THE CELLULAR RNA DECAY MACHINERY
The general RNA decay machinery of the cell primarily targets mRNAs for degradation via deadenylation of the poly(A) tail followed by decapping and exonucleolytic decay of the body of the transcript (Schoenberg & Maquat, 2012). RNA decay represents a major player in cellular mRNA expression and mRNA quality control (Wolin & Maquat, 2019)—and thus is often targeted by cytoplasmic RNA viruses to enhance viral RNA stability, replication, translation, and pathogenesis (Moon & Wilusz, 2013). One approach a virus can use to influence this machinery is to change the playing field—in this case encode its own ribonuclease which trumps the natural regulation of mRNA turnover and likely creates havoc with the cellular RNA decay machinery.
The conserved coronavirus nsp1 protein has endoribonuclease activity that selectively targets cellular mRNAs for degradation (Kamitani et al., 2006; Tohya et al., 2009). The massive degradation of cellular mRNAs enhances the formation of stress granules and P bodies (retaining sites for downregulated mRNAs) during the infection (Raaben et al., 2007). SARS‐CoV and MERS‐CoV nsp1 associate with the stem loop (SL) SL1 hairpin in the 5′ UTR of coronaviral mRNAs. The presence of the SL1 element in the 5′ UTR of viral mRNAs helps to protect these transcripts from nsp1‐directed cleavage (Huang et al., 2011; Tanaka, Kamitani, DeDiego, Enjuanes, & Matsuura, 2012; Terada, Kawachi, Matsuura, & Kamitani, 2017). Curiously, the SARS‐CoV nsp1 is a 179 amino acid protein with an irregular beta‐barrel fold and lacks an obvious signature of a ribonuclease domain (Almeida, Johnson, Herrmann, Geralt, & Wüthrich, 2007). There is circumstantial evidence that the nsp1 protein coordinates its endonuclease activity with other aspects of RNA biology in the cell. While the SARS‐CoV nsp1 interfaces with translation via an interaction with the 40S ribosome, the MERS‐CoV nsp1 protein instead shuttles between the nucleus and cytoplasm and selectively targets mRNAs with a nuclear experience (i.e., all cellular mRNAs) for cleavage (Huang et al., 2011). Mutational analyses indicate that nsp1 and its endoribonucleolytic activity play an important role in dampening the innate immune response of the cell to viral infection (Narayanan et al., 2008). A recent study also associates the endoribonuclease activity with efficient coronaviral virion assembly or budding (Nakagawa et al., 2018). Therefore, this novel viral ribonuclease is clearly a major player in viral infections.
Coronaviruses also code for their own 3′–5′ exonuclease—a novelty among RNA viruses. The viral nsp14 protein (also called nsp‐14‐ExoN) is a 3′–5′ exoribonuclease classified as part of the DE‐D‐Dh family of exonucleases that influences the fidelity of CoV replication through a proofreading activity (Graepel et al., 2017). This function makes nsp14‐ExoN the first RNA proofreading enzyme to be described. Given the large 26–32 kb size of the coronavirus RNA genome and its surprisingly low mutation rate, nsp14‐ExoN contributes in a major way to maintaining fidelity during replication (e.g., Ferron et al., 2018). Mutation of the active site of nsp14‐ExoN results in up to a 20× decrease in fidelity (Eckerle et al., 2010; Graepel et al., 2017). As discussed above, nsp14 also contains MTase activity for the RNA capping process (Case, Ashbrook, Dermody, & Denison, 2016) and nsp14 is found in complex with the viral nsp10 protein that upregulates the ExoN and MTase activities (Chen et al., 2011). Thus nsp10 appears to be a broad‐based regulator of CoV RNA modification and quality control. Given the havoc that an unregulated 3′–5′ exoribonuclease can play during viral infection, nsp14 is clearly carefully controlled by protein–protein complexes and does not appear to significantly impact the overall degradation of RNAs in the infected cell.
Nonsense‐mediated decay (NMD) is a quality control mechanism that coordinates the translation and decay of a subset of cellular mRNAs (Kishor, Fritz, & Hogg, 2019). NMD targets mRNAs with premature termination codons and long 3′ untranslated regions for decay following assembly of a surveillance complex via the UPF1 protein (Kurosaki, Popp, & Maquat, 2019). Interestingly, the NMD pathway was recently shown to impact MHV coronavirus infections by degrading viral mRNAs early in infection. As soon as the viral nucleocapsid (N) accumulates, it specifically inhibits the NMD pathway (Wada, Lokugamage, Nakagawa, & Narayanan, 2018). The underlying mechanism for the repression of NMD by the viral N protein remains to be elucidated. The NMD pathway has been shown to impact a variety of RNA viruses (Balistreri, Bognanni, & Mühlemann, 2017) and, interestingly, the capsid protein of Zika virus has been shown to repress NMD by lowering UPF1 levels (Fontaine et al., 2018). Thus, a pattern of viral nucleic acid assembly proteins moonlighting as protectors of viral transcripts from NMD may be emerging.
While there is clearly interplay between coronaviruses and the cellular RNA decay machinery, there are many pressing knowledge gaps that remain to be addressed. First, how do coronavirus mRNAs maintain their stability during infection—not just from the effects of the viral nsp1 endoribonuclease and the NMD machinery—but also from other cellular factors that target mRNAs for decay? Coronaviral transcripts, like other viral RNAs, are likely recognized as foreign invaders and targeted by multiple mechanisms for removal in this RNA decay molecular arms race. Second, what is the mechanism used by CoV and the CoV N protein to repress the NMD machinery? Third, do coronaviruses alter other components of the cellular RNA decay machinery as is done by other positive‐sense viruses (Kishor et al., 2019) to gain an advantage over cellular gene expression during infection? Along these lines, it is not clear what the impact of the endonucleolytic cleavage of the mass of cellular RNA has on the ability of the cellular exonucleases to continue to rapidly remove transcripts that have been targeted for removal. Finally, there is a growing appreciation of a connection and crosstalk between nuclear transcription rates and cytoplasmic RNA decay rates (El‐Brolosy et al., 2019; Gilbertson, Federspiel, Hartenian, Cristea, & Glaunsinger, 2018). Whether or not coronaviruses interfere with this communication network remains to be determined.
6. CORONAVIRUSES AND HOST miRNAs
Host micro RNAs (miRNAs) are small transcripts that downregulate mRNAs generally through binding in their 3′ UTRs using the cell's RNA interference machinery (Gutbrod & Martienssen, 2020). miRNA–mRNA interactions are initiated by a short seed sequence at the 5′ end of the miRNA, resulting in the ability of one miRNA to regulate many different mRNAs, perhaps in a coordinated fashion. Thus miRNAs play a major role in fine tuning cellular gene expression, allowing for proper cellular differentiation, growth and environmental responses (Gebert & MacRae, 2019). It is not surprising, therefore, that miRNA expression is altered during coronavirus expression as both a cellular response to the infection and by viral‐based manipulation of the biogenesis and sequestration of miRNAs. Differential miRNA expression analyses have demonstrated 10s to 100s of miRNAs whose levels are altered by a variety of coronaviruses. Infections with TGEV (X. Ma, Zhao, et al., 2018), IBV (Kemp et al., 2020; Lin, Wang, Wang, & Yang, 2019), and SARS‐CoV (Mallick, Ghosh, & Chakrabarti, 2009; Peng et al., 2011), for example, were shown by next generation sequencing (NGS) to differentially express scores of miRNAs with both increases and decreases seen in expression profiles. A growing number of the changes in the expression of select miRNAs have also been shown to be functionally relevant for a variety of coronaviruses. The goal of this section is to provide an organized overview of these observations.
Changes in miRNA expression can enhance viral pathogenesis and cytopathology. An increase in miR‐4331 during TGEV infection has been shown to the associated with mitochondrial damage via the targeting and repression of RB1 expression (Zhao et al., 2018). TGEV infection also disrupts ER membranes resulting in the activation of the cellular endonuclease IRE1. IRE1 has been shown to decrease miR‐30a‐5p, a negative regulator of two inhibitors of the IFN pathway, SOCS1 and SOCS3. This increase in SOCS1/3 expression helps to promote TGEV infection (Y. Ma, Wang, et al., 2018). Studies with the human SARS coronavirus in bronchoalveolar stem cells (BASC) have demonstrated an interplay between viral manipulation of several miRNAs and immune evasion during BASC differentiation (Mallick et al., 2009). Finally, the downregulation of angiotensin converting enzyme ACE2 by the activation of miR‐200c‐3p that targets the 3′ UTR of the cellular ACE2 mRNA during infection by SARS and other pneumonias promotes acute respiratory syndromes (Liu et al., 2017).
The miRNAs that are targeted for dysregulation in coronavirus infections can be either antiviral or proviral. Antiviral miRNAs can function through at least two mechanisms. The first mechanism is via the downregulation of cellular factors that create an optimal environment for viral replication in the cell. The miR30a‐5p noted above that is downregulated in TGEV infections is a good example of an antiviral miRNA that works through this mechanism (Y. Ma, Wang, et al., 2018). Another example is the chicken miRNA gga‐30d that is antiviral for IBV and is downregulated by the virus during infection (Li et al., 2020). The miR gga‐30d naturally downregulates a deubiquitinating enzyme, USP47. Thus, the downregulation of this small RNA by IBV can have dramatic effects on the cellular proteome. Finally, PHEV infection increases miR‐10a‐5p, resulting in a decrease in the host protein syndecan (SDC1)—a transmembrane protein involved in aspects of cell signaling, proliferation and cytoskeletal organization—and a concomitant decrease in PHEV replication (Hu et al., 2020). The second mechanism by which miRNAs can be antiviral to coronaviruses is via direct targeting of the viral RNA. The miRNA‐221‐5p, for example, directly targets the 3′ UTR of PEDV to decrease viral replication, augmenting this antiviral state by also targeting inhibitors of NF‐KB signaling (Zheng et al., 2018). Additional studies will likely lead to more examples of active targeting of antiviral miRNAs by coronaviruses during infection.
Proviral miRNAs that are induced in coronavirus infections have been somewhat better characterized to date and generally work by downregulating the expression of specific negative regulators of viral replication. IBV induces miR‐146a‐5p during infection which subsequently targets and downregulates IRAK2 (which influences NF‐KB induction) and TNFRSF18 (a member of the TNF receptor superfamily (Liu, Yang, Zhang, Zou, & Wang, 2018)). PHEV upregulates miR‐142‐5p (which targets ULK1) (Li et al., 2017), miR‐142a‐3p (which targets the RAB GTPase Rab3a) (Fan et al., 2020), and miR‐21a‐5p (which targets CASKIN1, a neuronal intracellular signaling factor) to promote increased viral replication (Lv et al., 2017). Finally, human coronaviruses also take advantage of several proviral miRNAs during infection. The nucleocapsid protein of CoV‐OC43 binds to and sequesters miR‐9, resulting in an increase in negative regulators of the NF‐KB pathway (Lai, Stephenson, Mahony, & Lichty, 2014). Finally, mouse experiments have shown that miR‐155 is a key enhancer of T cell responses that can alter the pathogenic profile of the MHV coronavirus (Dickey, Worne, Glover, Lane, & O'Connell, 2016). Overall, one gets the impression that these examples are just the tip of the iceberg and that more proviral miRNAs will undoubtedly be discovered as researchers sort through the many miRNAs whose expression is dysregulated during infections.
Collectively, these data indicate that the strategy of manipulation of cellular miRNA expression is a conserved part of the interplay between animal coronaviruses and their hosts. Numerous key questions remain in this area. First, the virus‐specific, host‐specific, and cell type‐specific dysregulation of miRNA expression during coronavirus infections need to be carefully catalogued. This may lead to the identification of preferred small RNA targets as well as cellular pathways/regulons that coronaviruses target for their replication and pathogenesis. Second, the use of miRNAs and miRNA mimics that target conserved regions of medically important coronaviruses—or key cellular factors that promote infection—can be used to downregulate coronavirus replication/gene expression and thus are a potential broad anti‐coronavirus therapeutic strategy. Finally, the underlying mechanism(s) for the dysregulation of host miRNAs during coronavirus infections needs to be explored. Elaborating the possible direct effects of coronaviral factors on miRNAs, miRNA genes, and miRNA clusters may provide many new paradigms in host–viral interactions.
7. THE INTERPLAY OF CORONAVIRUSES WITH LONG NONCODING RNAs AND CIRCULAR RNAs
Long noncoding RNAs (lncRNAs), many undetected before the advent of advanced sequencing techniques, make up the lion's share of transcripts generated from the host genome (Ransohoff, Wei, & Khavari, 2018; Tsagakis, Douka, Birds, & Aspden, 2020). Another recently expanded class of cellular transcripts are circular RNAs (circRNAs) that arise from backsplicing of linear pre‐mRNAs (Pandey et al., 2020; Wilusz, 2018). While the functional roles of the vast majority of these transcripts are unknown, some have been implicated in regulating a variety of cellular processes including transcription, RNA processing, translation and miRNA accessibility (Pandey et al., 2020).
The influence of viral factors with these less‐characterized noncoding transcripts may provide insight into both viral–host interactions and cellular biology. Though in its relative infancy, there have been several reports of coronavirus infections on the differential expression of several of these non‐coding transcripts. CircRNA expression can be dysregulated in a variety of coronavirus infections. TGEV infection of porcine intestinal epithelial cells, for example, causes the differential expression of over 120 circRNAs (X. Ma, Zhao, et al., 2018) and affects over 100 lncRNAs (Ma et al., 2019). A recent similar NGS study of PEDV infection of porcine epithelial cells revealed many hundreds of potential alterations in circRNA expression, eight of which were independently validated (Chen et al., 2019). A study in PDCV infection of neonatal piglets revealed 30–100 lncRNAs to be differentially expressed at different times post infection (Tang et al., 2019). In terms of human coronaviruses, there have only been a few studies to date in this area. Early NGS analysis of SARS‐CoV infections suggested the dysregulation of many lncRNAs during infections of mice (Peng et al., 2011). MERS‐CoV infection of Calu‐3 epithelial cells demonstrated differences in the expression of over 3% of identified circRNAs at 24 hr postinfection (Zhang et al., 2020). Interestingly, this study of MERS‐CoV infections of lung adenocarcinoma epithelial cells revealed two circRNAs that are upregulated 2–3× during infection (Zhang et al., 2020). Both of these circRNAs—circFNDC3B and circCNOT1—were hypothesized to sponge/sequester miR1275 and miR‐2392 respectively, a model supported by circRNA knockdown data that resulted in a decrease in mRNA targets of the miRNAs.
Overall, the influence of lncRNAs and circRNAs on coronavirus biology is an underexplored area that may yield novel insights into virus–host interactions. It is not yet clear from a mechanistic perspective how coronavirus infections mediate these changes in noncoding RNA gene expression. The NGS studies to date have laid a promising foundation for additional growth in this area, and it will be interesting to see what the future may hold.
8. CORONAVIRUS INTERACTIONS WITH CELLULAR RBPs
Given the abundance of RBPs in a host cell (Hentze, Castello, Schwarzl, & Preiss, 2018), many cellular RBPs are likely to interact with coronavirus transcripts during infection, many with possible functional implications to virus replication and pathogenesis. While the host interactome of SARS‐CoV proteins has been described (Srinivasan et al., 2020), the description of the coronavirus RNA host interactome is still to be determined. Several RBPs, however, have been described over the years to interact specifically with coronavirus RNA regulatory elements. The goal of this section is to provide an overview of these interactions which we believe may set the stage for additional insight into host interactions with viral RNAs in the future.
The best described interaction of an RBP with coronavirus RNAs is the host hnRNP A1 protein. hnRNP A1 is an abundant nucleo‐cytoplasmic shuttling protein that contains tandem RNA binding domains that possess significant binding plasticity at its N‐terminus followed by a largely disordered C‐terminal portion (Levengood & Tolbert, 2019). hnRNP A1 binds a wide range of RNA substrates and can play a role in alternative RNA splicing, nuclear export, and translation. hnRNP A1 protein interacts with MHV coronavirus RNAs at the UTR regions of the genome ([−] sense leader and 3′ UTR) as well as at intergenic regions (Li, Zhang, Duncan, Comai, & Lai, 1997; Shi et al., 2003). Evidence suggests that hnRNP A1 binding at these sites could stimulate complex formation between the viral RNA, polymerase, and nucleocapsid protein (Shi, Huang, Li, & Lai, 2000; Zhang, Li, Xue, & Lai, 1999), although the mechanistic implications of these complexes are not clear. Overexpression of hnRNP A1 in cells has been shown to increase MHV replication kinetics in a fashion that required the C‐terminal disordered portion of the hnRNP protein (Shi et al., 2000). hnRNP A1 and hnRNP A2/B1 proteins have been shown to relocalize to the cytoplasm during coronavirus infections (Li et al., 2018; Shi et al., 2003), perhaps providing a readily available source of the factor for the cytoplasmic replication of the virus. While some reports using hnRNP A1 depletion have demonstrated that the protein is proviral for coronavirus replication (Li et al., 2018), one report demonstrated no effect of A1 knockouts in mouse cells (Shen & Masters, 2001). This apparent discrepancy might be explained by the apparent ability of close relatives of hnRNP A1 protein (hnRNP A2/B1, A/B, and A3) to substitute for hnRNP A1 during infection (Shi et al., 2003).
Interestingly, hnRNP A1 has been shown to interact with the nucleocapsid protein of MHV (Wang & Zhang, 1999), PEDV (Li et al., 2018), IBV (Emmott et al., 2013), and SARS (Luo et al., 2005). The putative RNA helicase DDX1 also interacts with N protein and is thought to play a role in coronavirus transcription (H. Y. Wu, Guan, Su, Fan, & Brian, 2014). Coronavirus nucleocapsid proteins on their own have been shown to promote ER stress, prolong the cellular S phase, and inhibit interferon production (Ding et al., 2014; Xu et al., 2013). In addition, the viral nucleocapsid proteins appear to be active substrates for a variety of proteases during infection (Jaru‐Ampornpan, Jengarn, Wanitchang, & Jongkaewwattana, 2017). It will be interesting to assess in the future whether these interactions between hnRNP A1 protein and coronavirus N protein (or proteolytic fragments) are responsible for aspects of cytopathology and alterations in gene expression in the host cell.
Another host protein that interacts with UTR and intergenic regulatory elements of coronaviruses is polypyrimidine tract binding protein (PTB). PTB was shown to bind to MHV leader RNAs as well as the 3′ UTR where it was argued to induce conformational changes (Li, Huang, Park, & Lai, 1999; Huang & Lai, 1999; Sola, Mateos‐Gomez, Almazan, Zuñiga, & Enjuanes, 2011). Experiments using mutations of the UCUAA pentanucleotide PTB binding site, as well as through the use of over‐expression of dominant negative variants, argue for a role for PTB in MHV transcription. Similar binding of PTB to transcriptional elements was observed in TGEV (Galán et al., 2009; Sola, Galán, et al., 2011). During TGEV infection, PTB was observed to shuttle out of the nucleus and accumulate in the cytoplasm—including in stress‐granule‐like structures (Sola, Galán, et al., 2011). Finally, it has been speculated that PTB and hnRNP A1 may interact while binding to the coronavirus genome, promoting interactions between the termini of the viral RNA that may have regulatory implications (Huang & Lai, 2001).
Several additional cellular proteins have been shown to interact with coronavirus RNAs. The 3′ untranslated region of TGEV RNA interacts with PABP, hnRNP Q, and the glutamyl‐prolyl tRNA synthetase, three factors that appear to be proviral for RNA replication based on a 2–3× increase in RNA synthesis in knockdown experiments (Galán et al., 2009). Interestingly, hnRNP Q (also called synaptotagmin‐binding cytoplasmic interacting protein), which has also been shown to interact with MHV untranslated regions (Choi, Mizutani, & Lai, 2004), is a factor that has been shown to be part of RNA editing complexes and plays a role in the survival of motor neurons complex. Finally, the 3′ 42 nucleotides of MHV have been shown to interact with mitochondrial aconitase as well as mitochondrial HSP70, HSP60 and HSP40.
Given the impact that cellular RBPs have on all aspects of RNA processing/RNA biology, as well as the plasticity of many of their RNA binding domains, it is imperative that a more complete understanding of the RBP interactome of coronavirus RNAs be obtained and the functional implications of those interactions both to the virus as well as cellular RNA biology be uncovered. For example, the relocation of hnRNP A1 and PTB to the cytoplasm as well their sequestration of coronavirus RNAs may not only affect viral RNA replication, but could also have dramatic effect on the appearance and relative amounts of alternative mRNA isoforms in the infected cell since the two proteins are known regulators of splicing (Kafasla et al., 2012; Roy, Huang, Seckl, & Pardo, 2017). Such alterations of the cellular splicing code during infection could have dramatic implications on cellular gene expression and cytopathology (Boudreault, Roy, Lemay, & Bisaillon, 2019). Finally, the application of cutting‐edge approaches such as VIR‐CLASP (Kim et al., 2020) to uncover viral RNA interactions with host cell proteins should be very fruitful in expanding our understanding of this important virus–host interface.
9. CONCLUSION
Coronaviruses interface in a significant way with every aspect of the post‐transcriptional RNA biological mechanisms of the infected cell. Thus, in order to fully appreciate the molecular basis of the pathogenesis of this viral pathogen, additional work is needed to elucidate the extent, mechanisms, and functional consequences of this viral–cell biology interface. We hope that the detailed descriptions and insights that we provide in this overview will stimulate additional focused and productive work in this area with the goal of revealing additional targets for effective, possibly broad anti‐coronaviral therapeutic intervention.
CONFLICT OF INTEREST
The authors have declared no conflicts of interest for this article.
AUTHOR CONTRIBUTIONS
David Maranon: Writing‐review and editing. John Anderson: Writing‐review and editing. Abril Maranon: Writing‐review and editing. Jeff Wilusz: Conceptualization; formal analysis; funding acquisition; writing‐original draft; writing‐review and editing.
RELATED WIREs ARTICLES
Small molecules targeting viral RNA
RNA regulatory processes in RNA virus biology.
Nonsense‐mediated mRNA decay: The challenge of telling right from wrong in a complex transcriptome
ACKNOWLEDGMENTS
We wish to thank all of the first responders, health care workers, and researchers who are helping the planet to effectively deal with the 2020 COVID‐19 pandemic. Virology research in the Wilusz lab is supported by NIH grant award AI123136.
Maranon DG, Anderson JR, Maranon AG, Wilusz J. The interface between coronaviruses and host cell RNA biology: Novel potential insights for future therapeutic intervention. WIREs RNA. 2020;11:e1614. 10.1002/wrna.1614
Funding information National Institutes of Health, Grant/Award Number: AI123136
REFERENCES
- Abbas, Y. M. , Laudenbach, B. T. , Martínez‐Montero, S. , Cencic, R. , Habjan, M. , Pichlmair, A. , … Nagar, B. (2017). Structure of human IFIT1 with capped RNA reveals adaptable mRNA binding and mechanisms for sensing N1 and N2 ribose 2′‐O methylations. Proceedings of the National Academy of Sciences of the United States of America, 114(11), E2106–E2115. 10.1073/pnas.1612444114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almeida, M. S. , Johnson, M. A. , Herrmann, T. , Geralt, M. , & Wüthrich, K. (2007). Novel beta‐barrel fold in the nuclear magnetic resonance structure of the replicase nonstructural protein 1 from the severe acute respiratory syndrome coronavirus. Journal of Virology, 81(7), 3151–3161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balistreri, G. , Bognanni, C. , & Mühlemann, O. (2017). Virus escape and manipulation of cellular nonsense‐mediated mRNA decay. Viruses, 9(1), 24. 10.3390/v9010024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banerjee, S. , An, S. , Zhou, A. , Silverman, R. H. , & Makino, S. (2000). RNase L‐independent specific 28S rRNA cleavage in murine coronavirus‐infected cells. Journal of Virology, 74(19), 8793–8802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boudreault, S. , Roy, P. , Lemay, G. , & Bisaillon, M. (2019). Viral modulation of cellular RNA alternative splicing: A new key player in virus‐host interactions? WIREs RNA, 10(5), e1543. 10.1002/wrna.1543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buschauer, R. , Matsuo, Y. , Sugiyama, T. , Chen, Y. H. , Alhusaini, N. , Sweet, T. , … Beckmann, R. (2020). The Ccr4‐Not complex monitors the translating ribosome for codon optimality. Science, 368(6488), eaay6912. 10.1126/science.aay6912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caliskan, N. , Katunin, V. I. , Belardinelli, R. , Peske, F. , & Rodnina, M. V. (2014). Programmed −1 frameshifting by kinetic partitioning during impeded translocation. Cell, 157(7), 1619–1631. 10.1016/j.cell.2014.04.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Case, J. B. , Ashbrook, A. W. , Dermody, T. S. , & Denison, M. R. (2016). Mutagenesis of S‐adenosyl‐l‐methionine‐binding residues in coronavirus nsp14 N7‐methyltransferase demonstrates differing requirements for genome translation and resistance to innate immunity. Journal of Virology, 90(16), 7248–7256. 10.1128/JVI.00542-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cencic, R. , Desforges, M. , Hall, D. R. , Kozakov, D. , Du, Y. , Min, J. , … Pelletier, J. (2011). Blocking eIF4E‐eIF4G interaction as a strategy to impair coronavirus replication. Journal of Virology, 85(13), 6381–6389. 10.1128/JVI.00078-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, J. , Wang, H. , Jin, L. , Wang, L. , Huang, X. , Chen, W. , … Liu, G. (2019). Profile analysis of circRNAs induced by porcine endemic diarrhea virus infection in porcine intestinal epithelial cells. Virology, 527, 169–179. 10.1016/j.virol.2018.11.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, Y. , & Guo, D. (2016). Molecular mechanisms of coronavirus RNA capping and methylation. Virologica Sinica, 31(1), 3–11. 10.1007/s12250-016-3726-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, Y. , Su, C. , Ke, M. , Jin, X. , Xu, L. , Zhang, Z. , … Guo, D. (2011). Biochemical and structural insights into the mechanisms of SARS coronavirus RNA ribose 2′‐O‐methylation by nsp16/nsp10 protein complex. PLoS Pathogens, 7(10), e1002294. 10.1371/journal.ppat.1002294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho, C. P. , Lin, S. C. , Chou, M. Y. , Hsu, H. T. , & Chang, K. Y. (2013). Regulation of programmed ribosomal frameshifting by co‐translational refolding RNA hairpins. PLoS One, 8(4), e62283. 10.1371/journal.pone.0062283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi, K. S. , Mizutani, A. , & Lai, M. M. (2004). SYNCRIP, a member of the heterogeneous nuclear ribonucleoprotein family, is involved in mouse hepatitis virus RNA synthesis. Journal of Virology, 78(23), 13153–13162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corman, V. M. , Muth, D. , Niemeyer, D. , & Drosten, C. (2018). Hosts and sources of endemic human coronaviruses. Advances in Virus Research, 100, 163–188. 10.1016/bs.aivir.2018.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cowling, V. H. (2019). CAPAM: The mRNA cap adenosine N6‐methyltransferase. Trends in Biochemical Sciences, 44(3), 183–185. 10.1016/j.tibs.2019.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui, J. , Li, F. , & Shi, Z. L. (2019). Origin and evolution of pathogenic coronaviruses. Nature Reviews. Microbiology, 17(3), 181–192. 10.1038/s41579-018-0118-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daffis, S. , Szretter, K. J. , Schriewer, J. , Li, J. , Youn, S. , Errett, J. , … Diamond, M. S. (2010). 2′‐O methylation of the viral mRNA cap evades host restriction by IFIT family members. Nature, 468(7322), 452–456. 10.1038/nature09489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickey, L. L. , Worne, C. L. , Glover, J. L. , Lane, T. E. , & O'Connell, R. M. (2016). MicroRNA‐155 enhances T cell trafficking and antiviral effector function in a model of coronavirus‐induced neurologic disease. Neuroinflammation, 13(1), 240. 10.1186/s12974-016-0699-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding, Z. , Fang, L. , Jing, H. , Zeng, S. , Wang, D. , Liu, L. , … Xiao, S. (2014). Porcine epidemic diarrhea virus nucleocapsid protein antagonizes beta interferon production by sequestering the interaction between IRF3 and TBK1. Journal of Virology, 88(16), 8936–8945. 10.1128/JVI.00700-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eckerle, L. D. , Becker, M. M. , Halpin, R. A. , Li, K. , Venter, E. , Lu, X. , … Denison, M. R. (2010). Infidelity of SARS‐CoV Nsp14‐exonuclease mutant virus replication is revealed by complete genome sequencing. PLoS Pathogens, 6(5), e1000896. 10.1371/journal.ppat.1000896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- El‐Brolosy, M. A. , Kontarakis, Z. , Rossi, A. , Kuenne, C. , Günther, S. , Fukuda, N. , … Stainier, D. Y. R. (2019). Genetic compensation triggered by mutant mRNA degradation. Nature, 568(7751), 193–197. 10.1038/s41586-019-1064-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emmott, E. , Munday, D. , Bickerton, E. , Britton, P. , Rodgers, M. A. , Whitehouse, A. , … Hiscox, J. A. (2013). The cellular interactome of the coronavirus infectious bronchitis virus nucleocapsid protein and functional implications for virus biology. Journal of Virology, 87(17), 9486–9500. 10.1128/JVI.00321-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan, P. , Guan, J. , He, W. , Lv, X. , Hu, S. , Lan, Y. , … Li, Z. (2020). miR‐142a‐3p promotes the proliferation of porcine hemagglutinating encephalomyelitis virus by targeting Rab3a. Archives of Virology, 165(2), 345–354. 10.1007/s00705-019-04470-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferron, F. , Subissi, L. , Silveira De Morais, A. T. , Le, N. T. T. , Sevajol, M. , Gluais, L. , … Imbert, I. (2018). Structural and molecular basis of mismatch correction and ribavirin excision from coronavirus RNA. Proceedings of the National Academy of Sciences of the United States of America, 115(2), E162–E171. 10.1073/pnas.1718806115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fontaine, K. A. , Leon, K. E. , Khalid, M. M. , Tomar, S. , Jimenez‐Morales, D. , Dunlap, M. , … Ott, M. (2018). The cellular NMD pathway restricts Zika virus infection and is targeted by the viral capsid protein. mBio, 9(6), e02126‐18. 10.1128/mBio.02126-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frieman, M. , Yount, B. , Heise, M. , Kopecky‐Bromberg, S. A. , Palese, P. , & Baric, R. S. (2007). Severe acute respiratory syndrome coronavirus ORF6 antagonizes STAT1 function by sequestering nuclear import factors on the rough endoplasmic reticulum/Golgi membrane. Journal of Virology, 81(18), 9812–9824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galán, C. , Sola, I. , Nogales, A. , Thomas, B. , Akoulitchev, A. , Enjuanes, L. , & Almazán, F. (2009). Host cell proteins interacting with the 3′ end of TGEV coronavirus genome influence virus replication. Virology, 391(2), 304–314. 10.1016/j.virol.2009.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gebert, L. F. R. , & MacRae, I. J. (2019). Regulation of microRNA function in animals. Nature Reviews. Molecular Cell Biology, 20(1), 21–37. 10.1038/s41580-018-0045-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giedroc, D. P. , Theimer, C. A. , & Nixon, P. L. (2000). Structure, stability and function of RNA pseudoknots involved in stimulating ribosomal frameshifting. Journal of Molecular Biology, 298(2), 167–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbertson, S. , Federspiel, J. D. , Hartenian, E. , Cristea, I. M. , & Glaunsinger, B. (2018). Changes in mRNA abundance drive shuttling of RNA binding proteins, linking cytoplasmic RNA degradation to transcription. Elife, 7, e37663. 10.7554/eLife.37663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomez, G. N. , Abrar, F. , Dodhia, M. P. , Gonzalez, F. G. , & Nag, A. (2019). SARS coronavirus protein nsp1 disrupts localization of Nup93 from the nuclear pore complex. Biochemistry and Cell Biology, 97(6), 758–766. 10.1139/bcb-2018-0394 [DOI] [PubMed] [Google Scholar]
- Gordon, D. E. , Jang, G. M. , Bouhaddou, M. , Xu, J. , Obernier, K. , White, K. M. , … Krogan, N. J. (2020). A SARS‐CoV‐2 protein interaction map reveals targets for drug repurposing. Nature. 10.1038/s41586-020-2286-9 (Online ahead of print). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gozalo, A. , Duke, A. , Lan, Y. , Pascual‐Garcia, P. , Talamas, J. A. , Nguyen, S. C. , … Capelson, M. (2020. Jan 2). Core components of the nuclear pore bind distinct states of chromatin and contribute to polycomb repression. Molecular Cell, 77(1), 67–81.e7. 10.1016/j.molcel.2019.10.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graepel, K. W. , Lu, X. , Case, J. B. , Sexton, N. R. , Smith, E. C. , & Denison, M. R. (2017). Proofreading‐deficient coronaviruses adapt for increased fitness over long‐term passage without reversion of exoribonuclease‐inactivating mutations. mBio, 8(6), e01503‐17. 10.1128/mBio.01503-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gutbrod, M. J. , & Martienssen, R. A. (2020). Conserved chromosomal functions of RNA interference. Nature Reviews. Genetics, 21(5), 311–331. 10.1038/s41576-019-0203-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanson, G. , & Coller, J. (2018). Codon optimality, bias and usage in translation and mRNA decay. Nature Reviews. Molecular Cell Biology, 19(1), 20–30. 10.1038/nrm.2017.91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hentze, M. W. , Castello, A. , Schwarzl, T. , & Preiss, T. (2018). A brave new world of RNA‐binding proteins. Nature Reviews. Molecular Cell Biology, 19(5), 327–341. 10.1038/nrm.2017.130 [DOI] [PubMed] [Google Scholar]
- Hermann, T. (2016). Small molecules targeting viral RNA. WIREs RNA, 7(6), 726–743. 10.1002/wrna.1373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hia, F. , Yang, S. F. , Shichino, Y. , Yoshinaga, M. , Murakawa, Y. , Vandenbon, A. , … Takeuchi, O. (2019). Codon bias confers stability to human mRNAs. EMBO Reports, 20(11), e48220. 10.15252/embr.201948220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann, M. A. , & Brian, D. A. (1991). The 5′ end of coronavirus minus‐strand RNAs contains a short poly(U) tract. Journal of Virology, 65(11), 6331–6333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu, S. , Li, Z. , Lan, Y. , Guan, J. , Zhao, K. , Chu, D. , … He, W. (2020). MiR‐10a‐5p‐mediated syndecan 1 suppression restricts porcine hemagglutinating encephalomyelitis virus replication. Frontiers in Microbiology, 11, 105. 10.3389/fmicb.2020.00105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang, C. , Lokugamage, K. G. , Rozovics, J. M. , Narayanan, K. , Semler, B. L. , & Makino, S. (2011). SARS coronavirus nsp1 protein induces template‐dependent endonucleolytic cleavage of mRNAs: Viral mRNAs are resistant to nsp1‐induced RNA cleavage. PLoS Pathogens, 7(12), e1002433. 10.1371/journal.ppat.1002433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang, P. , & Lai, M. M. (1999). Polypyrimidine tract‐binding protein binds to the complementary strand of the mouse hepatitis virus 3′ untranslated region, thereby altering RNA conformation. Journal of Virology, 73(11), 9110–9116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang, P. , & Lai, M. M. (2001). Heterogeneous nuclear ribonucleoprotein a1 binds to the 3′‐untranslated region and mediates potential 5′–3′‐end cross talks of mouse hepatitis virus RNA. Journal of Virology, 75(11), 5009–5017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imbert, I. , Guillemot, J. C. , Bourhis, J. M. , Bussetta, C. , Coutard, B. , Egloff, M. P. , … Canard, B. (2006). A second, non‐canonical RNA‐dependent RNA polymerase in SARS coronavirus. The EMBO Journal, 25(20), 4933–4942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irigoyen, N. , Firth, A. E. , Jones, J. D. , Chung, B. Y. , Siddell, S. G. , & Brierley, I. (2016). High‐resolution analysis of coronavirus gene expression by RNA sequencing and ribosome profiling. PLoS Pathogens, 12(2), e1005473. 10.1371/journal.ppat.1005473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Issur, M. , Picard‐Jean, F. , & Bisaillon, M. (2011). The RNA capping machinery as an anti‐infective target. WIREs RNA, 2(2), 184–192. 10.1002/wrna.43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaru‐Ampornpan, P. , Jengarn, J. , Wanitchang, A. , & Jongkaewwattana, A. (2017). Porcine epidemic diarrhea virus 3C‐like protease‐mediated nucleocapsid processing: Possible link to viral cell culture adaptability. Journal of Virology, 91(2), e01660‐16. 10.1128/JVI.01660-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kafasla, P. , Mickleburgh, I. , Llorian, M. , Coelho, M. , Gooding, C. , Cherny, D. , … Smith, C. W. (2012). Defining the roles and interactions of PTB. Biochemical Society Transactions, 40(4), 815–820. 10.1042/BST20120044 [DOI] [PubMed] [Google Scholar]
- Kamitani, W. , Huang, C. , Narayanan, K. , Lokugamage, K. G. , & Makino, S. (2009). A two‐pronged strategy to suppress host protein synthesis by SARS coronavirus Nsp1 protein. Nature Structural & Molecular Biology, 16(11), 1134–1140. 10.1038/nsmb.1680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamitani, W. , Narayanan, K. , Huang, C. , Lokugamage, K. , Ikegami, T. , Ito, N. , … Makino, S. (2006). Severe acute respiratory syndrome coronavirus nsp1 protein suppresses host gene expression by promoting host mRNA degradation. Proceedings of the National Academy of Sciences of the United States of America, 103(34), 12885–12890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kemp, V. , Laconi, A. , Cocciolo, G. , Berends, A. J. , Breit, T. M. , & Verheije, M. H. (2020). miRNA repertoire and host immune factor regulation upon avian coronavirus infection in eggs. Archives of Virology, 165(4), 835–843. 10.1007/s00705-020-04527-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim, B. , Arcos, S. , Rothamel, K. , Rothamel, K. , Jian, J. , Rose, K. L. , … Ascano, M. (2020). Discovery of widespread host protein interactions with the pre‐replicated genome of CHIKV using VIR‐CLASP. Molecular Cell, 78(4), 624–640.e7. 10.1016/j.molcel.2020.04.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kishor, A. , Fritz, S. E. , & Hogg, J. R. (2019). Nonsense‐mediated mRNA decay: The challenge of telling right from wrong in a complex transcriptome. WIREs RNA, 10(6), e1548. 10.1002/wrna.1548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kopecky‐Bromberg, S. A. , Martinez‐Sobrido, L. , & Palese, P. (2006). 7a protein of severe acute respiratory syndrome coronavirus inhibits cellular protein synthesis and activates p38 mitogen‐activated protein kinase. Journal of Virology, 80(2), 785–793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurosaki, T. , Popp, M. W. , & Maquat, L. E. (2019). Quality and quantity control of gene expression by nonsense‐mediated mRNA decay. Nature Reviews. Molecular Cell Biology, 20(7), 406–420. 10.1038/s41580-019-0126-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai, F. W. , Stephenson, K. B. , Mahony, J. , & Lichty, B. D. (2014). Human coronavirus OC43 nucleocapsid protein binds microRNA 9 and potentiates NF‐κB activation. Journal of Virology, 88(1), 54–65. 10.1128/JVI.02678-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levengood, J. D. , & Tolbert, B. S. (2019). Idiosyncrasies of hnRNP A1‐RNA recognition: Can binding mode influence function. Seminars in Cell & Developmental Biology, 86, 150–161. 10.1016/j.semcdb.2018.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, H. , Li, J. , Zhai, Y. , Zhang, L. , Cui, P. , Feng, L. , … Yang, X. (2020). Gga‐miR‐30d regulates infectious bronchitis virus infection by targeting USP47 in HD11 cells. Microbial Pathogenesis, 141, 103998. 10.1016/j.micpath.2020.103998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, H. P. , Huang, P. , Park, S. , & Lai, M. M. (1999). Polypyrimidine tract‐binding protein binds to the leader RNA of mouse hepatitis virus and serves as a regulator of viral transcription. Journal of Virology, 73(1), 772–777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, H. P. , Zhang, X. , Duncan, R. , Comai, L. , & Lai, M. M. (1997). Heterogeneous nuclear ribonucleoprotein A1 binds to the transcription‐regulatory region of mouse hepatitis virus RNA. Proceedings of the National Academy of Sciences of the United States of America, 94(18), 9544–9549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, J. , Rahmeh, A. , Morelli, M. , & Whelan, S. P. (2008). A conserved motif in region v of the large polymerase proteins of nonsegmented negative‐sense RNA viruses that is essential for mRNA capping. Journal of Virology, 82(2), 775–784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, Z. , Lan, Y. , Zhao, K. , Lv, X. , Ding, N. , Lu, H. , … He, W. (2017). miR‐142‐5p disrupts neuronal morphogenesis underlying porcine hemagglutinating encephalomyelitis virus infection by targeting Ulk1. Frontiers in Cellular and Infection Microbiology, 7, 155. 10.3389/fcimb.2017.00155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, Z. , Zeng, W. , Ye, S. , Lv, J. , Nie, A. , Zhang, B. , … He, Q. (2018). Cellular hnRNP A1 interacts with nucleocapsid protein of porcine epidemic diarrhea virus and impairs viral replication. Viruses, 10(3), E127. 10.3390/v10030127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin, J. , Wang, Z. , Wang, J. , & Yang, Q. (2019). Microarray analysis of infectious bronchitis virus infection of chicken primary dendritic cells. BMC Genomics, 20(1), 557. 10.1186/s12864-019-5940-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, D. X. , & Inglis, S. C. (1992). Internal entry of ribosomes on a tricistronic mRNA encoded by infectious bronchitis virus. Journal of Virology, 66(10), 6143–6154 Erratum in: J Virol 1992 Nov;66(11):6840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, H. , Yang, X. , Zhang, Z. K. , Zou, W. C. , & Wang, H. N. (2018). miR‐146a‐5p promotes replication of infectious bronchitis virus by targeting IRAK2 and TNFRSF18. Microbial Pathogenesis, 120, 32–36. 10.1016/j.micpath.2018.04.046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, Q. , Du, J. , Yu, X. , Xu, J. , Huang, F. , Li, X. , … Jiang, C. (2017. Jun 27). miRNA‐200c‐3p is crucial in acute respiratory distress syndrome. Cell Discovery, 3, 17021. 10.1038/celldisc.2017.21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lokugamage, K. G. , Narayanan, K. , Huang, C. , & Makino, S. (2012). Severe acute respiratory syndrome coronavirus protein nsp1 is a novel eukaryotic translation inhibitor that represses multiple steps of translation initiation. Journal of Virology, 86(24), 13598–13608. 10.1128/JVI.01958-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo, H. , Chen, Q. , Chen, J. , Chen, K. , Shen, X. , & Jiang, H. (2005). The nucleocapsid protein of SARS coronavirus has a high binding affinity to the human cellular heterogeneous nuclear ribonucleoprotein A1. FEBS Letters, 579(12), 2623–2628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lv, X. , Zhao, K. , Lan, Y. , Li, Z. , Ding, N. , Su, J. , … He, W. (2017). miR‐21a‐5p contributes to porcine hemagglutinating encephalomyelitis virus proliferation via targeting CASK‐interactive protein1 in vivo and vitro. Frontiers in Microbiology, 8, 304. 10.3389/fmicb.2017.00304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma, X. , Zhao, X. , Wang, K. , Tang, X. , Guo, J. , Mi, M. , … Tong, D. (2019). Identification and analysis of long non‐coding RNAs that are involved in inflammatory process in response to transmissible gastroenteritis virus infection. BMC Genomics, 20(1), 806. 10.1186/s12864-019-6156-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma, X. , Zhao, X. , Zhang, Z. , Guo, J. , Guan, L. , Li, J. , … Tong, D. (2018). Differentially expressed non‐coding RNAs induced by transmissible gastroenteritis virus potentially regulate inflammation and NF‐κB pathway in porcine intestinal epithelial cell line. BMC Genomics, 19(1), 747. 10.1186/s12864-018-5128-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma, Y. , Wang, C. , Xue, M. , Fu, F. , Zhang, X. , Li, L. , … Liu, P. (2018). The coronavirus transmissible gastroenteritis virus evades the type I interferon response through IRE1α‐mediated manipulation of the microRNA miR‐30a‐5p/SOCS1/3 axis. Journal of Virology, 92(22), e00728‐18. 10.1128/JVI.00728-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madhugiri, R. , Fricke, M. , Marz, M. , & Ziebuhr, J. (2016). Coronavirus cis‐acting RNA elements. Advances in Virus Research, 96, 127–163. 10.1016/bs.aivir.2016.08.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mallick, B. , Ghosh, Z. , & Chakrabarti, J. (2009). MicroRNome analysis unravels the molecular basis of SARS infection in bronchoalveolar stem cells. PLoS One, 4(11), e7837. 10.1371/journal.pone.0007837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moon, S. L. , & Wilusz, J. (2013). Cytoplasmic viruses: Rage against the (cellular RNA decay) machine. PLoS Pathogens, 9(12), e1003762. 10.1371/journal.ppat.1003762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakagawa, K. , Narayanan, K. , Wada, M. , Popov, V. L. , Cajimat, M. , Baric, R. S. , & Makino, S. (2018). The endonucleolytic RNA cleavage function of nsp1 of Middle East respiratory syndrome coronavirus promotes the production of infectious virus particles in specific human cell lines. Journal of Virology, 92(21), e01157‐18. 10.1128/JVI.01157-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Napthine, S. , Liphardt, J. , Bloys, A. , Routledge, S. , & Brierley, I. (1999). The role of RNA pseudoknot stem 1 length in the promotion of efficient −1 ribosomal frameshifting. Journal of Molecular Biology, 288(3), 305–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narayanan, K. , Huang, C. , Lokugamage, K. , Kamitani, W. , Ikegami, T. , Tseng, C. T. , & Makino, S. (2008). Severe acute respiratory syndrome coronavirus nsp1 suppresses host gene expression, including that of type I interferon, in infected cells. Journal of Virology, 82(9), 4471–4479. 10.1128/JVI.02472-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson, G. W. , Stohlman, S. A. , & Tahara, S. M. (2000). High affinity interaction between nucleocapsid protein and leader/intergenic sequence of mouse hepatitis virus RNA. The Journal of General Virology, 81(Pt 1), 181–188. [DOI] [PubMed] [Google Scholar]
- O'Connor, J. B. , & Brian, D. A. (2000). Downstream ribosomal entry for translation of coronavirus TGEV gene 3b. Virology, 269(1), 172–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogino, M. , & Ogino, T. (2017). 5′‐Phospho‐RNA acceptor specificity of GDP polyribonucleotidyltransferase of vesicular stomatitis virus in mRNA capping. Journal of Virology, 91(6), e02322‐16. 10.1128/JVI.02322-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pandey, P. R. , Munk, R. , Kundu, G. , De, S. , Abdelmohsen, K. , & Gorospe, M. (2020). Methods for analysis of circular RNAs. WIREs RNA, 11(1), e1566. 10.1002/wrna.1566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park, S. J. , Kim, Y. G. , & Park, H. J. (2011). Identification of RNA pseudoknot‐binding ligand that inhibits the −1 ribosomal frameshifting of SARS‐coronavirus by structure‐based virtual screening. Journal of the American Chemical Society, 133(26), 10094–10100. 10.1021/ja1098325 [DOI] [PubMed] [Google Scholar]
- Paules, C. I. , Marston, H. D. , & Fauci, A. S. (2020). Coronavirus infections‐more than just the common cold. Journal of the American Medical Association, 323, 707. 10.1001/jama.2020.0757 [DOI] [PubMed] [Google Scholar]
- Peng, X. , Gralinski, L. , Ferris, M. T. , Frieman, M. B. , Thomas, M. J. , Proll, S. , … Katze, M. G. (2011). Integrative deep sequencing of the mouse lung transcriptome reveals differential expression of diverse classes of small RNAs in response to respiratory virus infection. mBio, 2(6), e00198‐11. 10.1128/mBio.00198-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peng, Y. H. , Lin, C. H. , Lin, C. N. , Lo, C. Y. , Tsai, T. L. , & Wu, H. Y. (2016). Characterization of the role of hexamer AGUAAA and poly(A) tail in coronavirus polyadenylation. PLoS One, 11(10), e0165077. 10.1371/journal.pone.0165077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plant, E. P. , & Dinman, J. D. (2008). The role of programmed‐1 ribosomal frameshifting in coronavirus propagation. Frontiers in Bioscience, 13, 4873–4881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raaben, M. , Groot Koerkamp, M. J. , Rottier, P. J. , & de Haan, C. A. (2007). Mouse hepatitis coronavirus replication induces host translational shutoff and mRNA decay, with concomitant formation of stress granules and processing bodies. Cellular Microbiology, 9(9), 2218–2229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ransohoff, J. D. , Wei, Y. , & Khavari, P. A. (2018). The functions and unique features of long intergenic non‐coding RNA. Nature Reviews. Molecular Cell Biology, 19(3), 143–157. 10.1038/nrm.2017.104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritchie, D. B. , Foster, D. A. , & Woodside, M. T. (2012). Programmed −1 frameshifting efficiency correlates with RNA pseudoknot conformational plasticity, not resistance to mechanical unfolding. Proceedings of the National Academy of Sciences of the United States of America, 109(40), 16167–16172. 10.1073/pnas.1204114109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodnina, M. V. , Korniy, N. , Klimova, M. , Karki, P. , Peng, B. Z. , Senyushkina, T. , … Peske, F. (2020). Translational recoding: Canonical translation mechanisms reinterpreted. Nucleic Acids Research, 48(3), 1056–1067. 10.1093/nar/gkz783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy, R. , Huang, Y. , Seckl, M. J. , & Pardo, O. E. (2017). Emerging roles of hnRNPA1 in modulating malignant transformation. WIREs RNA, 8(6), e1431. 10.1002/wrna.1431 [DOI] [PubMed] [Google Scholar]
- Schoenberg, D. R. , & Maquat, L. E. (2012). Regulation of cytoplasmic mRNA decay. Nature Reviews Genetics, 13(4), 246–259. 10.1038/nrg3160 Review. Erratum in: Nat Rev Genet. 2012 Jun;13(6):448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senanayake, S. D. , & Brian, D. A. (1997). Bovine coronavirus I protein synthesis follows ribosomal scanning on the bicistronic N mRNA. Virus Research, 48(1), 101–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen, X. , & Masters, P. S. (2001). Evaluation of the role of heterogeneous nuclear ribonucleoprotein A1 as a host factor in murine coronavirus discontinuous transcription and genome replication. Proceedings of the National Academy of Sciences of the United States of America, 98(5), 2717–2722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi, C. S. , Qi, H. Y. , Boularan, C. , Huang, N. N. , Abu‐Asab, M. , Shelhamer, J. H. , & Kehrl, J. H. (2014). SARS‐coronavirus open reading frame‐9b suppresses innate immunity by targeting mitochondria and the MAVS/TRAF3/TRAF6 signalosome. Journal of Immunology, 193(6), 3080–3089. 10.4049/jimmunol.1303196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi, S. T. , Huang, P. , Li, H. P. , & Lai, M. M. (2000). Heterogeneous nuclear ribonucleoprotein A1 regulates RNA synthesis of a cytoplasmic virus. The EMBO Journal, 19(17), 4701–4711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi, S. T. , Yu, G. Y. , & Lai, M. M. (2003). Multiple type A/B heterogeneous nuclear ribonucleoproteins (hnRNPs) can replace hnRNP A1 in mouse hepatitis virus RNA synthesis. Journal of Virology, 77(19), 10584–10593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shien, J. H. , Su, Y. D. , & Wu, H. Y. (2014). Regulation of coronaviral poly(A) tail length during infection is not coronavirus species‐ or host cell‐specific. Virus Genes, 49(3), 383–392. 10.1007/s11262-014-1103-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sims, A. C. , Tilton, S. C. , Menachery, V. D. , Gralinski, L. E. , Schäfer, A. , Matzke, M. M. , … Baric, R. S. (2013). Release of severe acute respiratory syndrome coronavirus nuclear import block enhances host transcription in human lung cells. Journal of Virology, 87(7), 3885–3902. 10.1128/JVI.02520-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sola, I. , Almazán, F. , Zúñiga, S. , & Enjuanes, L. (2015). Continuous and discontinuous RNA synthesis in coronaviruses. Annual Review of Virology, 2(1), 265–288. 10.1146/annurev-virology-100114-055218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sola, I. , Galán, C. , Mateos‐Gómez, P. A. , Palacio, L. , Zúñiga, S. , Cruz, J. L. , … Enjuanes, L. (2011). The polypyrimidine tract‐binding protein affects coronavirus RNA accumulation levels and relocalizes viral RNAs to novel cytoplasmic domains different from replication‐transcription sites. Journal of Virology, 85(10), 5136–5149. 10.1128/JVI.00195-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sola, I. , Mateos‐Gomez, P. A. , Almazan, F. , Zuñiga, S. , & Enjuanes, L. (2011). RNA‐RNA and RNA–protein interactions in coronavirus replication and transcription. RNA Biology, 8(2), 237–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spagnolo, J. F. , & Hogue, B. G. (2001). Requirement of the poly(A) tail in coronavirus genome replication. Advances in Experimental Medicine and Biology, 494, 467–474. [DOI] [PubMed] [Google Scholar]
- Srinivasan, S. , Cui, H. , Gao, Z. , Liu, M. , Lu, S. , Mkandawire, W. , … Korkin, D. (2020). Structural genomics of SARS‐CoV‐2 indicates evolutionary conserved functional regions of viral proteins. Viruses, 12(4), E360. 10.3390/v12040360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tahara, S. M. , Dietlin, T. A. , Nelson, G. W. , Stohlman, S. A. , & Manno, D. J. (1998). Mouse hepatitis virus nucleocapsid protein as a translational effector of viral mRNAs. Advances in Experimental Medicine and Biology, 440, 313–318. [DOI] [PubMed] [Google Scholar]
- Tanaka, T. , Kamitani, W. , DeDiego, M. L. , Enjuanes, L. , & Matsuura, Y. (2012). Severe acute respiratory syndrome coronavirus nsp1 facilitates efficient propagation in cells through a specific translational shutoff of host mRNA. Journal of Virology, 86(20), 11128–11137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang, X. , Lan, T. , Wu, R. , Zhou, Z. , Chen, Y. , Sun, Y. , … Ma, J. (2019). Analysis of long non‐coding RNAs in neonatal piglets at different stages of porcine deltacoronavirus infection. BMC Veterinary Research, 15(1), 111. 10.1186/s12917-019-1862-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terada, Y. , Kawachi, K. , Matsuura, Y. , & Kamitani, W. (2017). MERS coronavirus nsp1 participates in an efficient propagation through a specific interaction with viral RNA. Virology, 511, 95–105. 10.1016/j.virol.2017.08.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thiel, V. , & Siddell, S. G. (1994). Internal ribosome entry in the coding region of murine hepatitis virus mRNA 5. The Journal of General Virology, 75(Pt 11), 3041–3046. [DOI] [PubMed] [Google Scholar]
- Thoms, M. , Buschauer, R. , Ameismeier, M. , Koepke, L. , Denk, T. , Hirschenberger, M. , … Beckmann, R. (2020). Structural basis for the translational shutdown and immune evasion by the Nsp1 protein of SARS‐CoV‐2. BioRxiv. 10.1101/2020.05.18.102467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tohya, Y. , Narayanan, K. , Kamitani, W. , Huang, C. , Lokugamage, K. , & Makino, S. (2009). Suppression of host gene expression by nsp1 proteins of group 2 bat coronaviruses. Journal of Virology, 83(10), 5282–5288. 10.1128/JVI.02485-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trotman, J. B. , & Schoenberg, D. R. (2019). A recap of RNA recapping. WIREs RNA, 10(1), e1504. 10.1002/wrna.1504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsagakis, I. , Douka, K. , Birds, I. , & Aspden, J. L. (2020). Long non‐coding RNAs in development and disease: Conservation to mechanisms. The Journal of Pathology, 250, 480–495. 10.1002/path.5405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai, T. L. , Lin, C. H. , Lin, C. N. , Lo, C. Y. , & Wu, H. Y. (2018). Interplay between the poly(A) tail, poly(A)‐binding protein, and coronavirus nucleocapsid protein regulates gene expression of coronavirus and the host cell. Journal of Virology, 92(23), e01162‐18. 10.1128/JVI.01162-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tvarogová, J. , Madhugiri, R. , Bylapudi, G. , Ferguson, L. J. , Karl, N. , & Ziebuhr, J. (2019). Identification and characterization of a human coronavirus 229E nonstructural protein 8‐associated RNA 3′‐terminal adenylyltransferase activity. Journal of Virology, 93(12), e00291‐19. 10.1128/JVI.00291-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wada, M. , Lokugamage, K. G. , Nakagawa, K. , & Narayanan, K. (2018). Makino S interplay between coronavirus, a cytoplasmic RNA virus, and nonsense‐mediated mRNA decay pathway. Proceedings of the National Academy of Sciences of the United States of America, 115(43), E10157–E10166. 10.1073/pnas.1811675115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, Q. , Vlasova, A. N. , Kenney, S. P. , & Saif, L. J. (2019). Emerging and re‐emerging coronaviruses in pigs. Current Opinion in Virology, 34, 39–49. 10.1016/j.coviro.2018.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, Y. , & Zhang, X. (1999). The nucleocapsid protein of coronavirus mouse hepatitis virus interacts with the cellular heterogeneous nuclear ribonucleoprotein A1 in vitro and in vivo. Virology, 265(1), 96–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilusz, J. E. (2018). A 360° view of circular RNAs: From biogenesis to functions. WIREs RNA, 9(4), e1478. 10.1002/wrna.1478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolin, S. L. , & Maquat, L. E. (2019). Cellular RNA surveillance in health and disease. Science, 366(6467), 822–827. 10.1126/science.aax2957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu, C. H. , Chen, P. J. , & Yeh, S. H. (2014). Nucleocapsid phosphorylation and RNA helicase DDX1 recruitment enables coronavirus transition from discontinuous to continuous transcription. Cell Host & Microbe, 16(4), 462–472. 10.1016/j.chom.2014.09.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu, H. Y. , Guan, B. J. , Su, Y. P. , Fan, Y. H. , & Brian, D. A. (2014). Reselection of a genomic upstream open reading frame in mouse hepatitis coronavirus 5′‐untranslated‐region mutants. Journal of Virology, 88(2), 846–858. 10.1128/JVI.02831-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu, H. Y. , Ke, T. Y. , Liao, W. Y. , & Chang, N. Y. (2013). Regulation of coronaviral poly(A) tail length during infection. PLoS One, 8(7), e70548. 10.1371/journal.pone.0070548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao, H. , Xu, L. H. , Yamada, Y. , & Liu, D. X. (2008). Coronavirus spike protein inhibits host cell translation by interaction with eIF3f. PLoS One, 3(1), e1494. 10.1371/journal.pone.0001494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu, X. , Zhang, H. , Zhang, Q. , Huang, Y. , Dong, J. , Liang, Y. , … Tong, D. (2013). Porcine epidemic diarrhea virus N protein prolongs S‐phase cell cycle, induces endoplasmic reticulum stress, and up‐regulates interleukin‐8 expression. Veterinary Microbiology, 164(3–4), 212–221. 10.1016/j.vetmic.2013.01.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang, C. W. , & Chen, M. F. (2020). Composition of human‐specific slow codons and slow di‐codons in SARS‐CoV and 2019‐nCoV are lower than other coronaviruses suggesting a faster protein synthesis rate of SARS‐CoV and 2019‐nCoV. Journal of Microbiology, Immunology and Infection. 2020;53(3):419–424. 10.1016/j.jmii.2020.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yarbrough, M. L. , Mata, M. A. , Sakthivel, R. , & Fontoura, B. M. (2014). Viral subversion of nucleocytoplasmic trafficking. Traffic, 15(2), 127–140. 10.1111/tra.12137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, X. , Chu, H. , Wen, L. , Shuai, H. , Yang, D. , Wang, Y. , … Yuen, K. Y. (2020). Competing endogenous RNA network profiling reveals novel host dependency factors required for MERS‐CoV propagation. Emerging Microbes & Infections, 9(1), 733–746. 10.1080/22221751.2020.1738277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, X. , Li, H. P. , Xue, W. , & Lai, M. M. (1999). Formation of a ribonucleoprotein complex of mouse hepatitis virus involving heterogeneous nuclear ribonucleoprotein A1 and transcription‐regulatory elements of viral RNA. Virology, 264(1), 115–124. [DOI] [PubMed] [Google Scholar]
- Zhao, X. , Bai, X. , Guan, L. , Li, J. , Song, X. , Ma, X. , … Tong, D. (2018). microRNA‐4331 promotes transmissible gastroenteritis virus (TGEV)‐induced mitochondrial damage via targeting RB1, upregulating interleukin‐1 receptor accessory protein (IL1RAP), and activating p38 MAPK pathway in vitro. Molecular & Cellular Proteomics, 17(2), 190–204. 10.1074/mcp.RA117.000432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng, H. , Xu, L. , Liu, Y. , Li, C. , Zhang, L. , Wang, T. , … Zhang, Y. (2018). MicroRNA‐221‐5p inhibits porcine epidemic diarrhea virus replication by targeting genomic viral RNA and activating the NF‐κB pathway. International Journal of Molecular Sciences, 19(11), E3381. 10.3390/ijms19113381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou, B. , Liu, J. , Wang, Q. , Liu, X. , Li, X. , Li, P. , … Cao, C. (2008). The nucleocapsid protein of severe acute respiratory syndrome coronavirus inhibits cell cytokinesis and proliferation by interacting with translation elongation factor 1alpha. Journal of Virology, 82(14), 6962–6971. 10.1128/JVI.00133-08 [DOI] [PMC free article] [PubMed] [Google Scholar]


