Abstract
Objective
This study aimed to examine the impact of the coronavirus disease (COVID‐19) pandemic on patronage to unhealthy eating establishments in populations with obesity.
Methods
Anonymized movement data accounting for roughly 10% of devices in the United States at 138,989 unhealthy eating locations from December 1, 2019, through April 2020 and the percentage of adults with obesity, the poverty rate, and the food environment index in 65% of United States counties were collected and merged. A cluster corrected Poisson spline regression was performed predicting patronage by day, the percentage of adults with obesity in the establishment’s county, the county’s poverty rate, and its food environment index, as well as their interactions.
Results
Patronage to unhealthy eating establishments was higher where there was a higher percentage of the adult population with obesity. A similar pattern was observed for counties with a lower food environment index. These disparities appear to have increased as the COVID‐19 pandemic spread.
Conclusions
These results suggest unhealthy eating patterns during the COVID‐19 pandemic are higher in already at‐risk populations. Policy makers can use these findings to motivate interventions and programs aimed at increasing healthy food intake in at‐risk communities during crises.
Study Importance.
What is already known?
-
►
Obesity is linked to complications from coronavirus disease (COVID‐19).
-
►
The COVID‐19 pandemic has increased unhealthy eating in children.
What does this study add?
-
►
The percentage of adults suffering from obesity in a population is related to differential patronage patterns at unhealthy eating establishments during the pandemic.
How might these results change the direction of research or the focus of clinical practice?
-
►
They provide foresight into health problems likely to be complicated by the current pandemic, allowing for practitioners and policy makers to prepare.
-
►
Policy makers can use these findings to institute policies aimed at increasing healthy food intake in at‐risk populations during crises.
Introduction
The coronavirus disease 2019 (COVID‐19) has been shown to have both direct and indirect effects on at‐risk populations. First, individuals with obesity appear to be more adversely impacted if they contract the virus (1). Secondly, the eating habits of children have shifted toward less healthy foods (2). Given widespread anxiety (3, 4) and shortages of fresh foods at grocery stores (5), this shift to less healthy eating during the pandemic is likely to extend to adult populations already suffering from higher rates of obesity. Notably, these changes might also push other segments of society, such as those living in poverty and/or in “food deserts,” to cheaper and more readily available unhealthy foods as well.
Many individuals with obesity suffer from disordered eating driven in part by emotions (6). A variety of research has indicated that a contributing factor to weight gain is emotional eating (7). For example, negative emotions have been found to lead to consumption of less healthy foods (8). The COVID‐19 pandemic has produced negative emotions such as anxiety and panic in the US population according to an analysis of social media (4). Given this, it is predicted that the COVID‐19 pandemic will lead to differential consumption of unhealthy foods (e.g., fast food) in populations with higher rates of obesity.
Methods
Data acquisition
The number of patrons going to 141,833 eating establishments categorized as serving unhealthy foods (i.e., “fast food,” “ice cream,” “donut,” “snack,” or “dessert”) across 89% of counties in the United States from December 1, 2019, to April 30, 2020, were obtained from anonymized geographical positioning system data made available by SafeGraph in response to the COVID‐19 pandemic (9). Data are reported to represent ~10% of mobile devices used in the United States (10). Each establishment was merged with an estimate of the percentage of the adult population with obesity (measured in 2016) in the county it resided in (11), the percentage of the county’s population living in poverty in 2018 (12), and its estimated food environment index (data from 2015 and 2017) (11). Missing demographic data led to a loss of 773 counties. Many of the counties not accounted for in the GPS data and/or demographic data were sparsely populated areas. A total of 17,234,452 observations from 138,989 establishments representing 65% of United States counties were ultimately included in the analysis.
Analysis
Given the nature of the data (i.e., counts), a Poisson spline regression was performed predicting the number of patrons at an establishment by day, the percentage of the adult population with obesity (standardized), the county’s food environment index (standardized), the percentage of the population in poverty (standardized), and their respective interactions. Three splines were created by setting knots at February 29th and March 31st. To account for repeated sampling, robust standard errors were calculated by clustering on the level of the county (13). All data manipulation and analyses were performed using Stata Software version 13 SE (College Station, Texas), and statistical significance was declared if a two‐sided P value was less than 0.05.
Results
Table 1 reports the analysis and indicates support for the prediction that counties with a higher percentage of adults with obesity would show differential patronage to unhealthy eating establishments during the pandemic. In all cases, it appears populations with a higher percentage of adults with obesity showed higher patronage to unhealthy eating establishments. Figure 1 illustrates these results, showing that the 10% of counties with the highest percentage of the adult population with obesity showed higher patronage to unhealthy establishments compared with the lowest 10% of counties. This difference increased from December 2019 through February 2020 as the COVID‐19 pandemic spread. As the pandemic took hold in March, patronage decreased rapidly but was lessened in those counties with the highest percentage of the adult population with obesity. In April, when most states had issued stay at home orders, a steady resumption of patronage to unhealthy eating establishments occurred, a rebound that appears to be occurring faster in those counties with the highest percentage of the adult population with obesity.
TABLE 1.
Poisson regression results for main effects and interactions over splines
| Main Effects | β | 95% CI | z | P |
|---|---|---|---|---|
| Poverty rate (PR) | −0.0377 | −0.0835 to 0.0080 | −1.62 | 0.106 |
| Food environment index (FEI) | −0.1059 | −0.1472 to −0.0646 | −5.03 | 0.000 |
| Obesity rate (OR) | 0.0460 | 0.0194 to 0.0725 | 3.39 | 0.001 |
| PR × FEI | 0.0153 | −0.0036 to 0.0342 | 1.59 | 0.113 |
| PR × OR | −0.0311 | −0.0720 to 0.0099 | −1.49 | 0.137 |
| FEI × OR | −0.0308 | −0.0719 to 0.0104 | −1.47 | 0.142 |
| PR × FEI × OR | 0.0061 | −0.0048 to 0.0170 | 1.11 | 0.269 |
| Constant | 2.8626 | 2.8351 to 2.8901 | 203.94 | 0.000 |
| December 1, 2019, to February 29, 2020 | ||||
| Day | 0.0010 | 0.0008 to 0.0011 | 13.26 | 0.000 |
| PR × Day | 0.0002 | 0.0000 to 0.0004 | 2.26 | 0.024 |
| FEI × Day | −0.0003 | −0.0005 to 0.0000 | −2.42 | 0.015 |
| OR × Day | 0.0004 | 0.0002 to 0.0005 | 5.53 | 0.000 |
| PR × FEI × Day | −0.0002 | −0.0003 to −0.0002 | −5.41 | 0.000 |
| PR × OR × Day | 0.0001 | −0.0001 to 0.0003 | 1.13 | 0.260 |
| FEI × OR × Day | 0.0003 | 0.0002 to 0.0005 | 3.75 | 0.000 |
| PR × FEI × OR × Day | 0.0001 | 0.0001 to 0.0002 | 4.02 | 0.000 |
| March 2020 | ||||
| Day | −0.0250 | −0.0258 to −0.0243 | −68.11 | 0.000 |
| PR × Day | −0.0028 | −0.0037 to −0.0018 | −5.60 | 0.000 |
| FEI × Day | −0.0011 | −0.0020 to −0.0002 | −2.36 | 0.018 |
| OR × Day | 0.0044 | 0.0036 to 0.0052 | 11.15 | 0.000 |
| PR × FEI × Day | 0.0009 | 0.0004 to 0.0015 | 3.19 | 0.001 |
| PR × OR × Day | 0.0019 | 0.0009 to 0.0029 | 3.70 | 0.000 |
| FEI × OR × Day | 0.0016 | 0.0007 to 0.0025 | 3.33 | 0.001 |
| PR × FEI × OR × Day | −0.0005 | −0.0008 to −0.0002 | −3.30 | 0.001 |
| April 2020 | ||||
| Day | 0.0111 | 0.0108 to 0.0114 | 65.81 | 0.000 |
| PR × Day | −0.0008 | −0.0013 to −0.0004 | −3.67 | 0.000 |
| FEI × Day | −0.0013 | −0.0017 to −0.0008 | −5.63 | 0.000 |
| OR × Day | 0.0016 | 0.0013 to 0.0019 | 10.49 | 0.000 |
| PR × FEI × Day | −0.0005 | −0.0008 to −0.0001 | −2.89 | 0.004 |
| PR × OR × Day | 0.0003 | 0.0000 to 0.0007 | 1.73 | 0.083 |
| FEI × OR × Day | 0.0008 | 0.0004 to 0.0011 | 4.62 | 0.000 |
| PR × FEI × OR × Day | 0.0003 | 0.0001 to 0.0004 | 3.11 | 0.002 |
Hypothesized effects are bold and italicized.
Figure 1.
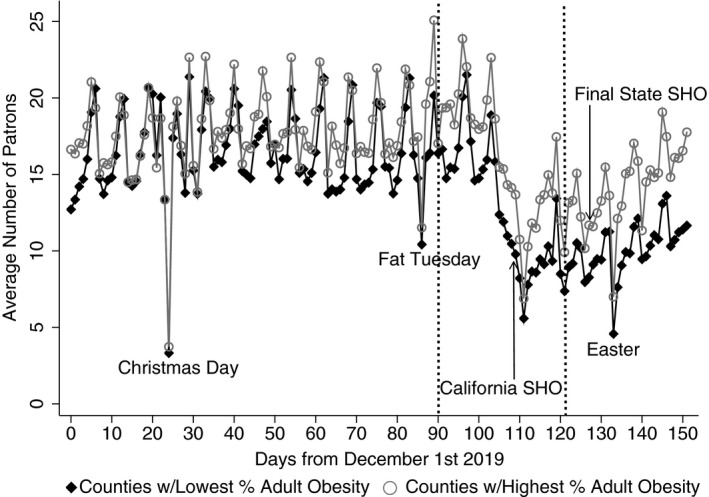
Average number of patrons at unhealthy eating establishments in the United States from December 1, 2019, through April 30, 2020. Plotted separately for the 10% of counties with the lowest/highest percentage of the adult population with obesity. Knots used in the analysis indicated by dashed lines and selected holidays and state‐issued stay home orders (SHO) marked.
The food environment index was found to be a significant predictor with a higher index (i.e., lower food insecurity) predicting lower rates of patronage at unhealthy eating establishments overall. The COVID‐19 pandemic appears to have boosted this difference, with counties having a higher index showing lower patronage across all splines. The poverty rate had no main effect but did interact with day. From December through February, populations with a higher rate of poverty showed increased patronage to unhealthy eating establishments. In contrast, during March, there was a steeper decrease in patronage followed by a slower recovery in April in those counties with higher poverty rates.
Discussion
While society struggles with COVID‐19, we must consider the indirect impacts the pandemic will have on those already at risk (1). One of those indirect impacts appears to be changes in eating behaviors (2). The current research indicates that while unhealthy eating declined overall during the pandemic, declines were less steep and appeared to be recovering faster in populations with a higher percentage of adults with obesity. In addition, the results suggest those living in areas with less access to quality foods are being similarly impacted. These changes in eating behaviors are likely to impact existing health issues.
One limitation of the current study is the use of anonymized county‐level data. While it is likely that patrons of an establishment reflect the demographics of the surrounding area, this cannot be guaranteed. As such, one must exercise extreme caution in interpreting the current results as evidence that individuals with obesity are driving the current patterns. To address this, future research must directly survey individuals about changes to their eating resulting from the COVID‐19 pandemic. In a similar vein, roughly 25% of the counties in the United States are not included in the current analysis because of missing points of demographic observation. Those counties not included are primarily sparsely inhabited rural areas. These geographically based missing data point to potential broader limitations in ascertaining measures of the nation’s health. As there is no easy remedy to this issue, one should remain cognizant that many areas are not represented in the current analysis and might therefore be impacted far differently by the pandemic.
Another limitation is the inability for the current data to estimate the unique contribution of all variables potentially affecting unhealthy food intake in populations with obesity. While the observed patterns align with the motivating theory of this investigation (6, 7, 8), that increased anxiety brought on by the pandemic (4) is leading to changes in disordered eating in populations with higher rates of obesity, the significant three‐ and four‐way interactions observed with poverty and the food environment index indicate the story is not that simple. The observed patterns are likely the result of multiple interacting factors beyond those that can be readily modeled in the current analysis (e.g., relationships, housing situations, job loss, school closures). Direct inquiry of those impacted is needed to determine the underlying causal factors.
There is also the inherent assumption that all counties experienced similar effects from the COVID‐19 pandemic in the current analysis. This is certainly a false assumption, as several states have not issued stay at home orders (e.g., Nebraska, Utah, Wyoming) and those that have did at different times (e.g., California was the first on March 19, whereas Missouri was the last on April 6). Unfortunately, the degree to which such differences are influencing the current results cannot be (readily) accounted for. Future research might remedy this by focusing on smaller subsets of the population where information can be gathered with more precision.
In sum, the current findings support suggestions that the COVID‐19 pandemic is exacerbating issues related to healthy eating (2, 14). By examining the potential indirect effects of the pandemic, practitioners and policy makers will be cognizant of the likely long‐term consequences that will result from the current pandemic and be able to better prepare at‐risk populations for future crises.
Disclosure
The author declared no conflict of interest.
See Commentary, pg. 1796.
References
- 1. Kalligeros M, Shehadeh F, Mylona EK, et al. Association of obesity with disease severity among patients with COVID‐19. Obesity (Silver Spring) 2020;28:1200–1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Pietrobelli A, Pecoraro L, Ferruzzi A, et al. Effects of COVID‐19 lockdown on lifestyle behaviors in children with obesity living in Verona, Italy: a longitudinal study. Obesity (Silver Spring) 2020;28:382–1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Depoux A, Martin S, Karafillakis E, Preet R, Wilder‐Smith A, Larson H. The pandemic of social media panic travels faster than the COVID‐19 outbreak. J Travel Med 2020;27:taaa031. doi:10.1093/jtm/taaa031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. CognoviLabs . Crisis monitor: coronavirus. https://coronavirus.cognovilabs.com/dashboard/Coronavirus%20Emotional%20Impact%20Index?key=countries/us/us‐all. Accessed May 2, 2020.
- 5. Hobbs JE. Food supply chains during the COVID‐19 pandemic. Canadian Journal of Agricultural Economics 2020;68:171–176. [Google Scholar]
- 6. Ganley RM. Emotion and eating in obesity: a review of the literature. Int J Eat Disord 1989;8:343‐361. [Google Scholar]
- 7. Frayn M, Knäuper B. Emotional eating and weight in adults: a review. Curr Psychol 2018;37:924‐933. [Google Scholar]
- 8. Patel KA, Schlundt DG. Impact of moods and social context on eating behavior. Appetite 2001;36:111‐118. [DOI] [PubMed] [Google Scholar]
- 9. SafeGraph . COVID‐19 Data Consortium. https://www.safegraph.com/covid‐19‐data‐consortium. Published 2020. Accessed April 1, 2020.
- 10. Fox RF. What about bias in the SafeGraph dataset? Safe Graph: Ideas of Interest blog. October 17, 2019. https://www.safegraph.com/blog/what‐about‐bias‐in‐the‐safegraph‐dataset. Accessed May 16, 2020. [Google Scholar]
- 11. Robert Wood Johnson Foundation and the University of Wisconsin Population Health Institute . County Health Rankings & Roadmaps. https://www.countyhealthrankings.org/. Accessed April 1, 2020.
- 12. U.S. Census Bureau . Small area income and poverty estimates. https://www.census.gov/data‐tools/demo/saipe/#/?map_geoSelector=aa_c. Accessed May 14, 2020
- 13. Rogers WH. sg17: regression standard errors in clustered samples. Stata J 1993;13:19‐23. [Google Scholar]
- 14. Rundle AG, Park Y, Herbstman JB, Kinsey EW, Wang YC. COVID‐19 related school closings and risk of weight gain among children. Obesity (Silver Spring) 2020;28:1008‐1009. doi:10.1002/oby.22813 [DOI] [PMC free article] [PubMed] [Google Scholar]


